Challenges in the Management of Non-Alcoholic Fatty Liver Disease (NAFLD): Towards a Compassionate Approach
Abstract
:1. Introduction
2. Methods
3. Historical Perspectives
4. Management of NAFLD
4.1. Role of Primary Care
4.2. Lifestyle Modification
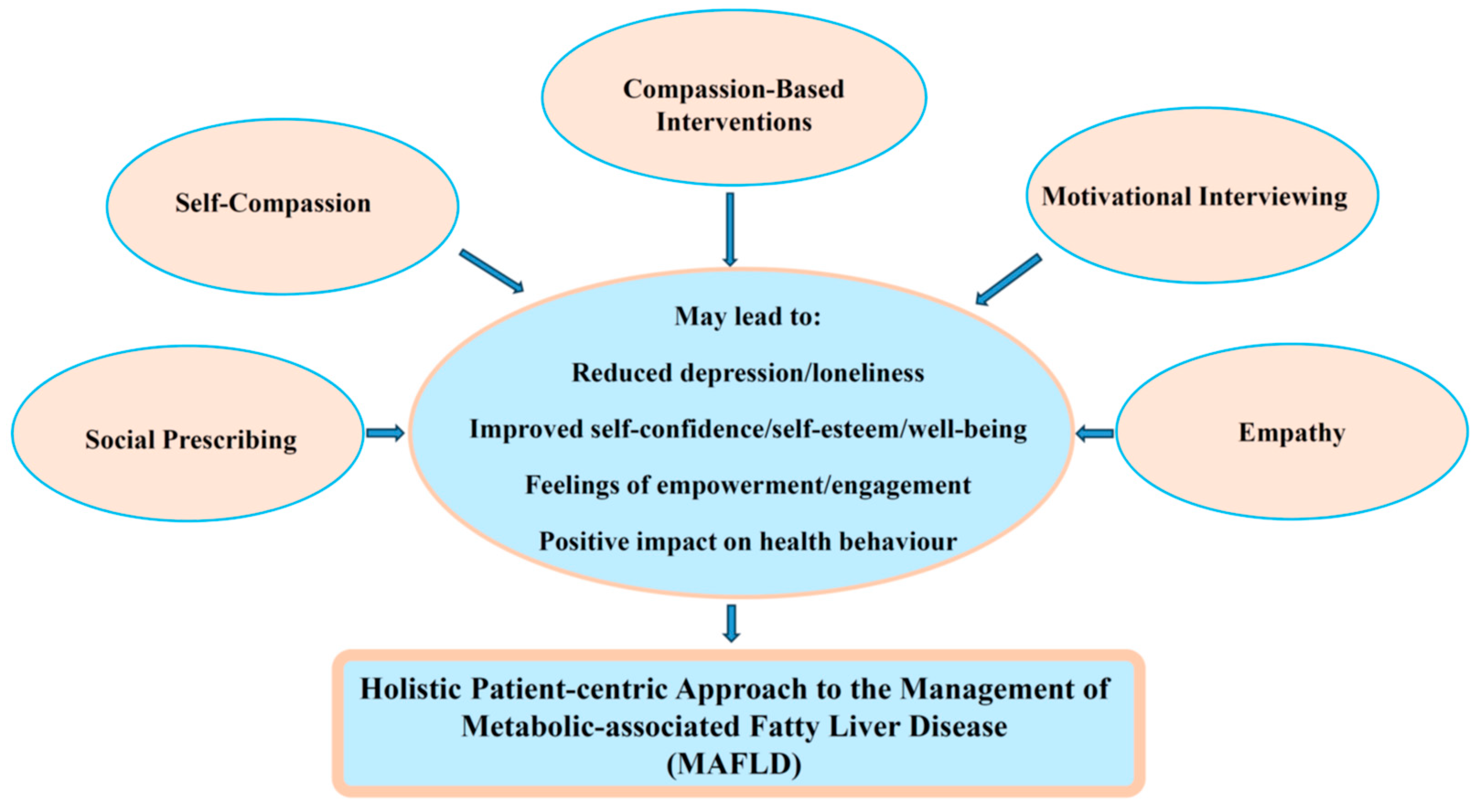
5. Compassionate Approaches
5.1. Compassion-Based Interventions
5.2. Self-Compassion
5.3. Motivational Interviewing
5.4. Social Prescribing
5.5. Empathy
6. Concluding Remarks
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Godoy-Matos, A.F.; Júnior, W.S.S.; Valerio, C.M. NAFLD as a continuum: From obesity to metabolic syndrome and diabetes. Diabetol. Metab. Syndr. 2020, 12, 60. [Google Scholar] [CrossRef]
- Katsiki, N.; Perez-Martinez, P.; Anagnostis, P.; Mikhailidis, D.P.; Karagiannis, A. Is Nonalcoholic Fatty Liver Disease Indeed the Hepatic Manifestation of Metabolic Syndrome? Curr. Vasc. Pharmacol. 2018, 16, 219–227. [Google Scholar] [CrossRef]
- Kyrou, I.; Randeva, H.S.; Tsigos, C.; Kaltsas, G.; Weickert, M.O. Clinical Problems Caused by Obesity. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2018. [Google Scholar]
- Younossi, Z.M.; Marchesini, G.; Pinto-Cortez, H.; Petta, S. Epidemiology of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis: Implications for Liver Transplantation. Transplantation 2019, 103, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Asrih, M.; Jornayvaz, F.R. Metabolic syndrome and nonalcoholic fatty liver disease: Is insulin resistance the link? Mol. Cell. Endocrinol. 2015, 418 Pt 1, 55–65. [Google Scholar] [CrossRef]
- Estes, C.; Anstee, Q.M.; Arias-Loste, M.T.; Bantel, H.; Bellentani, S.; Caballeria, J.; Colombo, M.; Craxi, A.; Crespo, J.; Day, C.P.; et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J. Hepatol. 2018, 69, 896–904. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Colombo, M.; Cortez-Pinto, H.; Huang, T.T.; Miller, V.; Ninburg, M.; Schattenberg, J.M.; Seim, L.; Wong, V.W.S.; Zelber-Sagi, S. NAFLD—Sounding the alarm on a silent epidemic. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 377–379. [Google Scholar] [CrossRef] [PubMed]
- Murag, S.; Ahmed, A.; Kim, D. Recent Epidemiology of Nonalcoholic Fatty Liver Disease. Gut Liver 2021, 15, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Noureddin, M.; Clark, J.M. Nonalcoholic Fatty Liver Disease: Review of Management for Primary Care Providers. Mayo Clin. Proc. 2022, 97, 1700–1716. [Google Scholar] [CrossRef]
- Paternostro, R.; Trauner, M. Current treatment of non-alcoholic fatty liver disease. J. Intern. Med. 2022, 292, 190–204. [Google Scholar] [CrossRef]
- Anstee, Q.M.; Hallsworth, K.; Lynch, N.; Hauvespre, A.; Mansour, E.; Kozma, S.; Marino, J.-P.; Bottomley, J.; Piercy, J.; Higgins, V. Real-world management of non-alcoholic steatohepatitis differs from clinical practice guideline recommendations and across regions. JHEP Rep. 2022, 4, 100411. [Google Scholar] [CrossRef]
- Berry, P.; Kotha, S. The Challenging Ethical Landscape of Non-alcoholic Fatty Liver Disease. Hepatology 2022. Available online: https://www.emjreviews.com/hepatology/article/the-challenging-ethical-landscape-of-non-alcoholic-fatty-liver-disease/ (accessed on 20 June 2023). [CrossRef]
- Dokmak, A.; Lizaola-Mayo, B.; Trivedi, H.D. The Impact of Nonalcoholic Fatty Liver Disease in Primary Care: A Population Health Perspective. Am. J. Med. 2021, 134, 23–29. [Google Scholar] [CrossRef]
- Pouwels, S.; Sakran, N.; Graham, Y.; Leal, A.; Pintar, T.; Yang, W.; Kassir, R.; Singhal, R.; Mahawar, K.; Ramnarain, D. Non-alcoholic fatty liver disease (NAFLD): A review of pathophysiology, clinical management and effects of weight loss. BMC Endocr. Disord. 2022, 22, 63. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Dalbeni, A.; Beatrice, G.; Cappelli, D.; Gomez-Peralta, F. Non-Alcoholic Fatty Liver Disease and Risk of Macro- and Microvascular Complications in Patients with Type 2 Diabetes. J. Clin. Med. 2022, 11, 968. [Google Scholar] [CrossRef] [PubMed]
- Shea, S.; Lionis, C.; Kite, C.; Atkinson, L.; Chaggar, S.S.; Randeva, H.S.; Kyrou, I. Non-Alcoholic Fatty Liver Disease (NAFLD) and Potential Links to Depression, Anxiety, and Chronic Stress. Biomedicines 2021, 9, 1697. [Google Scholar] [CrossRef]
- Shea, S.; Lionis, C.; Atkinson, L.; Kite, C.; Lagojda, L.; Chaggar, S.S.; Kyrou, I.; Randeva, H.S. Support Needs and Coping Strategies in Non-Alcoholic Fatty Liver Disease (NAFLD): A Multidisciplinary Approach to Potential Unmet Challenges Beyond Pharmacological Treatment. Livers 2023, 3, 1–20. [Google Scholar] [CrossRef]
- Orlandi, R.; Cianci, N.; Invernizzi, P.; Cesana, G.; Riva, M.A. “I Miss My Liver.” Nonmedical Sources in the History of Hepatocentrism. Hepatol. Commun. 2018, 2, 982–989. [Google Scholar] [CrossRef]
- Papavramidou, N. Hepatic regeneration in Greek mythology. World J. Meta Anal. 2019, 7, 77–79. [Google Scholar] [CrossRef]
- Riva, M.A.; Riva, E.; Spicci, M.; Strazzabosco, M.; Giovannini, M.; Cesana, G. “The city of Hepar”: Rituals, gastronomy, and politics at the origins of the modern names for the liver. J. Hepatol. 2011, 55, 1132–1136. [Google Scholar] [CrossRef]
- Lonardo, A.; Leoni, S.; Alswat, K.A.; Fouad, Y. History of Nonalcoholic Fatty Liver Disease. Int. J. Mol. Sci. 2020, 21, 5888. [Google Scholar] [CrossRef]
- Ayonrinde, O.T. Historical narrative from fatty liver in the nineteenth century to contemporary NAFLD—Reconciling the present with the past. JHEP Rep. 2021, 3, 100261. [Google Scholar] [CrossRef]
- Eslam, M.; Sanyal, A.J.; George, J.; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020, 158, 1999–2014.e1. [Google Scholar] [CrossRef]
- Fouad, Y.; Waked, I.; Bollipo, S.; Gomaa, A.; Ajlouni, Y.; Attia, D. What’s in a name? Renaming ‘NAFLD’ to ‘MAFLD’. Liver Int. 2020, 40, 1254–1261. [Google Scholar] [CrossRef] [PubMed]
- Francque, S.M.; Marchesini, G.; Kautz, A.; Walmsley, M.; Dorner, R.; Lazarus, J.V.; Zelber-Sagi, S.; Hallsworth, K.; Busetto, L.; Frühbeck, G.; et al. Non-alcoholic fatty liver disease: A patient guideline. JHEP Rep. 2021, 3, 100322. [Google Scholar] [CrossRef]
- Papadakis, S.; Anastasaki, M.; Gergianaki, I.; Koek, G.; Mendive, J.; Anastasiou, F.; Heyens, L.; Garcia-Retortillo, M.; Muris, J.; Lionis, C. Development and implementation of a continuing medical education program on non-alcoholic fatty liver disease for primary care practitioners in Europe. Front. Med. 2023, 10, 1034626. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.W.; Zelber-Sagi, S.; Cusi, K.; Carrieri, P.; Wright, E.; Crespo, J.; Lazarus, J.V. Management of NAFLD in primary care settings. Liver Int. 2022, 42, 2377–2389. [Google Scholar] [CrossRef] [PubMed]
- Islam, K.B.; Brandman, D.; Chu, J.N.; Goldman, M.L.; Fox, R.K. Primary Care Providers and Nonalcoholic Fatty Liver Disease: A Needs Assessment Survey. Dig. Dis. Sci. 2023, 68, 434–438. [Google Scholar] [CrossRef]
- Said, A.; Gagovic, V.; Malecki, K.; Givens, M.L.; Nieto, F.J. Primary care practitioners survey of non-alcoholic fatty liver disease. Ann. Hepatol. 2013, 12, 758–765. [Google Scholar] [CrossRef]
- Kanwal, F.; Shubrook, J.H.; Adams, L.A.; Pfotenhauer, K.; Wong, V.W.-S.; Wright, E.; Abdelmalek, M.F.; Harrison, S.A.; Loomba, R.; Mantzoros, C.S.; et al. Clinical Care Pathway for the Risk Stratification and Management of Patients with Nonalcoholic Fatty Liver Disease. Gastroenterology 2021, 161, 1657–1669. [Google Scholar] [CrossRef]
- Neilson, L.J.; Macdougall, L.; Lee, P.S.; Hardy, T.; Beaton, D.; Chandrapalan, S.; Ebraheem, A.; Hussien, M.; Galbraith, S.; Looi, S.; et al. Implementation of a care bundle improves the management of patients with non-alcoholic fatty liver disease. Front. Gastroenterol. 2021, 12, 578–585. [Google Scholar] [CrossRef]
- Kwak, M.S.; Kim, D. Non-alcoholic fatty liver disease and lifestyle modifications, focusing on physical activity. Korean J. Intern. Med. 2018, 33, 64–74. [Google Scholar] [CrossRef]
- Fogarty, L.A.; Curbow, B.A.; Wingard, J.R.; McDonnell, K.; Summerfield, M.R. Can 40 seconds of compassion reduce patient anxiety? J. Clin. Oncol. 1999, 17, 371. [Google Scholar] [CrossRef]
- Shaltout, H.A.; Tooze, J.A.; Rosenberger, E.; Kemper, K.J. Time, Touch, and Compassion: Effects on Autonomic Nervous System and Well-Being. Explore 2012, 8, 177–184. [Google Scholar] [CrossRef]
- Youngson, R. Time to Care: How to Love Your Patients and Your Job; Rebelheart Publishers: Hamilton, New Zealand, 2012. [Google Scholar]
- Goetz, J.L.; Keltner, D.; Simon-Thomas, E. Compassion: An evolutionary analysis and empirical review. Psychol. Bull. 2010, 136, 351–374. [Google Scholar] [CrossRef] [PubMed]
- Niño de Guzmán Quispe, E.; Martínez García, L.; Orrego Villagrán, C.; Heijmans, M.; Sunol, R.; Fraile-Navarro, D.; Pérez-Bracchiglione, J.; Ninov, L.; Salas-Gama, K.; García, A.V.; et al. The Perspectives of Patients with Chronic Diseases and Their Caregivers on Self-Management Interventions: A Scoping Review of Reviews. Patient 2021, 14, 719–740. [Google Scholar] [CrossRef]
- Austin, J.; Drossaert, C.H.C.; Schroevers, M.J.; Sanderman, R.; Kirby, J.N.; Bohlmeijer, E.T. Compassion-based interventions for people with long-term physical conditions: A mixed methods systematic review. Psychol. Health 2021, 36, 16–42. [Google Scholar] [CrossRef]
- Gilbert, J.; Stubbs, R.J.; Gale, C.; Gilbert, P.; Dunk, L.; Thomson, L. A qualitative study of the understanding and use of ‘compassion focused coping strategies’ in people who suffer from serious weight difficulties. J. Compassionate Health Care 2014, 1, 9. [Google Scholar] [CrossRef]
- Brenton-Peters, J.; Consedine, N.S.; Boggiss, A.; Wallace-Boyd, K.; Roy, R.; Serlachius, A. Self-compassion in weight management: A systematic review. J. Psychosom. Res. 2021, 150, 110617. [Google Scholar] [CrossRef] [PubMed]
- Friis, A.M.; Consedine, N.S.; Johnson, M.H. Does Kindness Matter? Diabetes, Depression, and Self-Compassion: A Selective Review and Research Agenda. Diabetes Spectr. 2015, 28, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Mantzios, M.; Egan, H.H. On the Role of Self-compassion and Self-kindness in Weight Regulation and Health Behavior Change. Front. Psychol. 2017, 8, 229. [Google Scholar] [CrossRef]
- Kilic, A.; Hudson, J.; McCracken, L.M.; Ruparelia, R.; Fawson, S.; Hughes, L.D. A Systematic Review of the Effectiveness of Self-Compassion-Related Interventions for Individuals with Chronic Physical Health Conditions. Behav. Ther. 2021, 52, 607–625. [Google Scholar] [CrossRef]
- Morrison, A.E.; Zaccardi, F.; Chatterjee, S.; Brady, E.; Doherty, Y.; Robertson, N.; Hadjiconstantinou, M.; Daniels, L.; Hall, A.; Khunti, K.; et al. Self-Compassion, Metabolic Control and Health Status in Individuals with Type 2 Diabetes: A UK Observational Study. Exp. Clin. Endocrinol. Diabetes 2021, 129, 413–419. [Google Scholar] [CrossRef]
- Sandham, C.; Deacon, E. The role of self-compassion in diabetes management: A rapid review. Front. Psychol. 2023, 14, 1123157. [Google Scholar] [CrossRef] [PubMed]
- Hunt, C.M.; Turner, M.J.; Gifford, E.J.; Britt, R.B.; Su, G.L. Identifying and Treating Nonalcoholic Fatty Liver Disease. Fed. Pract. 2019, 36, 20–29. [Google Scholar] [PubMed]
- Pollak, K.I.; Ostbye, T.; Alexander, S.C.; Gradison, M.; Bastian, L.A.; Brouwer, R.J. Empathy goes a long way in weight loss discussions. J. Fam. Pract. 2007, 56, 1031–1036. [Google Scholar]
- Steffen, P.L.S.; Mendonca, C.S.; Meyer, E.; Faustino-Silva, D.D. Motivational Interviewing in the Management of Type 2 Diabetes Mellitus and Arterial Hypertension in Primary Health Care: An RCT. Am. J. Prev. Med. 2021, 60, e203–e212. [Google Scholar] [CrossRef]
- Lee, W.W.; Choi, K.C.; Yum, R.W.; Yu, D.S.; Chair, S.Y. Effectiveness of motivational interviewing on lifestyle modification and health outcomes of clients at risk or diagnosed with cardiovascular diseases: A systematic review. Int. J. Nurs. Stud. 2015, 53, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Mifsud, J.L.; Galea, J.; Garside, J.; Stephenson, J.; Astin, F. Motivational interviewing to support modifiable risk factor change in individuals at increased risk of cardiovascular disease: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0241193. [Google Scholar] [CrossRef] [PubMed]
- Moffatt, S.; Steer, M.; Lawson, S.; Penn, L.; O’brien, N. Link Worker social prescribing to improve health and well-being for people with long-term conditions: Qualitative study of service user perceptions. BMJ Open 2017, 7, e015203. [Google Scholar] [CrossRef]
- Sharman, L.S.; McNamara, N.; Hayes, S.; Dingle, G.A. Social prescribing link workers-A qualitative Australian perspective. Health Soc. Care Commun. 2022, 30, e6376–e6385. [Google Scholar] [CrossRef]
- NHS (England). Social Prescribing: Reference Guide and Technical Annex for Primary Care Networks. Available online: https://www.england.nhs.uk/publication/social-prescribing-reference-guide-and-technical-annex-for-primary-care-networks/ (accessed on 25 June 2023).
- Sandhu, S.; Lian, T.; Drake, C.; Moffatt, S.; Wildman, J.; Wildman, J. Intervention components of link worker social prescribing programmes: A scoping review. Health Soc. Care Commun. 2022, 30, e3761–e3774. [Google Scholar] [CrossRef]
- Hassan, S.M.; Giebel, C.; Morasae, E.K.; Rotheram, C.; Mathieson, V.; Ward, D.; Reynolds, V.; Price, A.; Bristow, K.; Kullu, C. Social prescribing for people with mental health needs living in disadvantaged communities: The Life Rooms model. BMC Health Serv. Res. 2020, 20, 19. [Google Scholar] [CrossRef] [PubMed]
- Morse, D.F.; Sandhu, S.; Mulligan, K.; Tierney, S.; Polley, M.; Chiva Giurca, B.; Slade, S.; Dias, S.; Mahtani, K.R.; Wells, L.; et al. Global developments in social prescribing. BMJ Glob. Health 2022, 7, e008524. [Google Scholar] [CrossRef] [PubMed]
- Wildman, J.M.; Moffatt, S.; Steer, M.; Laing, K.; Penn, L.; O’brien, N. Service-users’ perspectives of link worker social prescribing: A qualitative follow-up study. BMC Public Health 2019, 19, 98. [Google Scholar] [CrossRef] [PubMed]
- Reinhardt, G.; Vidovic, D.; Hammerton, C. Understanding loneliness: A systematic review of the impact of social prescribing initiatives on loneliness. Perspect. Public Health 2021, 141, 204–213. [Google Scholar] [CrossRef]
- Baska, A.; Kurpas, D.; Kenkre, J.; Vidal-Alaball, J.; Petrazzuoli, F.; Dolan, M.; Śliż, D.; Robins, J. Social Prescribing and Lifestyle Medicine-A Remedy to Chronic Health Problems? Int. J. Environ. Res. Public Health 2021, 18, 10096. [Google Scholar] [CrossRef]
- Jayakrishnan, B.J.; Kesavadev, J.; Shrivastava, A.; Banshi, S.; Brij, M.M. Evolving Scope of Clinical Empathy in the Current Era of Medical Practice. Cureus 2023, 15, e40041. [Google Scholar]
- Kourakos, M.I.; Vlachou, E.D.; Kelesi, M.N. Empathy in the health professions: An ally in the care of patients with chronic diseases. Int. J. Health Sci. Res. 2018, 8, 233–240. [Google Scholar]
- Moudatsou, M.; Stavropoulou, A.; Philalithis, A.; Koukouli, S. The Role of Empathy in Health and Social Care Professionals. Healthcare 2020, 8, 26. [Google Scholar] [CrossRef]
- Canovas, L.; Carrascosa, A.J.; Garcia, M.; Fernandez, M.; Calvo, A.; Monsalve, V.; Soriano, J.-F.; Empathy Study Group. Impact of Empathy in the Patient-Doctor Relationship on Chronic Pain Relief and Quality of Life: A Prospective Study in Spanish Pain Clinics. Pain Med. 2018, 19, 1304–1314. [Google Scholar] [CrossRef]
- Barry, M.J.; Edgman-Levitan, S. Shared decision making--pinnacle of patient-centered care. N. Engl. J. Med. 2012, 366, 780–781. [Google Scholar] [CrossRef] [PubMed]
- Shea, S.; Lionis, C. Compassion in healthcare. In The Oxford Handbook of Compassion Science; Seppala, E., Simon-Thomas, E., Brown, S.L., Worline, M.C., Cameron, D.D., Doty, J.R., Eds.; Oxford University Press: New York, NY, USA, 2017; pp. 457–475. [Google Scholar]
- Lazarus, J.V.; Mark, H.E.; Allen, A.M.; Arab, J.P.; Carrieri, P.; Noureddin, M.; Alazawi, W.; Alkhouri, N.; Alqahtani, S.A.; Arrese, M.; et al. A global research priority agenda to advance public health responses to fatty liver disease. J. Hepatol. 2023, 79, 618–634. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shea, S.; Lionis, C.; Kite, C.; Atkinson, L.; Lagojda, L.; Chaggar, S.S.; Kyrou, I.; Randeva, H.S. Challenges in the Management of Non-Alcoholic Fatty Liver Disease (NAFLD): Towards a Compassionate Approach. Livers 2023, 3, 434-447. https://doi.org/10.3390/livers3030031
Shea S, Lionis C, Kite C, Atkinson L, Lagojda L, Chaggar SS, Kyrou I, Randeva HS. Challenges in the Management of Non-Alcoholic Fatty Liver Disease (NAFLD): Towards a Compassionate Approach. Livers. 2023; 3(3):434-447. https://doi.org/10.3390/livers3030031
Chicago/Turabian StyleShea, Sue, Christos Lionis, Chris Kite, Lou Atkinson, Lukasz Lagojda, Surinderjeet S. Chaggar, Ioannis Kyrou, and Harpal S. Randeva. 2023. "Challenges in the Management of Non-Alcoholic Fatty Liver Disease (NAFLD): Towards a Compassionate Approach" Livers 3, no. 3: 434-447. https://doi.org/10.3390/livers3030031
APA StyleShea, S., Lionis, C., Kite, C., Atkinson, L., Lagojda, L., Chaggar, S. S., Kyrou, I., & Randeva, H. S. (2023). Challenges in the Management of Non-Alcoholic Fatty Liver Disease (NAFLD): Towards a Compassionate Approach. Livers, 3(3), 434-447. https://doi.org/10.3390/livers3030031









