Abstract
Human milk is recognized as the optimal nutrition for infants, with evidence showing it can prevent childhood death. While there are approximately 756 milk banks worldwide, predominantly located in high-income countries, human milk banking remains limited in Africa, where infant mortality rates are highest. The purpose of this review was to examine the current landscape of human milk banking in Africa, analyzing its potential to decrease infant mortality and enhance neonatal health outcomes. We explore implementation challenges, opportunities for expansion, and strategies for establishing sustainable milk banking systems across the continent. Following Arksey and O’Malley’s scoping review framework, we conducted a comprehensive analysis of peer-reviewed literature, case studies, and reports from the PubMed, Google Scholar, and African Journals Online databases through 2024. Results: South Africa leads the continent, with over 20 milk banks, while countries like Kenya, Nigeria, and Uganda have recently established programs. Significant challenges include cultural barriers and a lack of infrastructure and funding. Despite current limitations, evidence supports the significant potential of human milk banking to reduce infant mortality in Africa. Success requires addressing cultural barriers, strengthening healthcare infrastructure, and developing sustainable funding models by integrating existing maternal and child health services.
1. Introduction
Scholarship on human milk indicates several benefits to newborn development, and it is acknowledged as optimal for infant nutrition in the first six months [1,2]. It provides essential nutrients, such as antibodies and bioactive factors that support childhood growth [3,4]. Additionally, infants exclusively fed human milk are reported to have fewer hospitalizations and the highest survival rate [4,5,6]. Due to its nutritional values, the World Health Organization (WHO) and several health organizations, such as the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN) and the Academy of Breastfeeding Medicine (ABM) [7], recommend that babies be fed exclusively human milk for their first six months, with subsequent continual breastfeeding and nutritious complementary foods for up to two years or more.
Furthermore, existing scholarship indicates that breastfeeding is vital for maternal and infant health and that about 820,000 childhood deaths could be prevented by the use of human milk [4,8,9]. When a mother’s milk is unavailable or insufficient due to illness, disability, or medication, numerous health professionals agree that human donor milk is the best option for baby feeding [10,11]. Human milk banking plays a vital role and has a long history of helping at-risk infants and vulnerable infants, such as those born preterm or with a low birth weight [12,13,14].
Additionally, several studies indicate the critical role of donors’ human milk and human milk banks in supporting mothers and their infants [15]. When a family needs supplementation for their infant, human milk from a donor is considered appropriate for the child [16,17,18,19]. Donors’ human milk is considered more compositionally similar to raw mothers’ milk than formula is [20,21]. Donor human milk could also be offered to an infant during the postpartum hospitalization of the mother to ensure continued exclusive human milk feeding [22,23].
Human milk banking involves the collection of surplus milk from breastfeeding mothers for pasteurization and the distribution of donated breast milk to infants in need [24]. Worldwide, it is estimated that there are about 756 human milk banks [25].
While these milk banks are predominantly located in high-income North American and European countries, where infant mortality rates are low [3], Africa faces a stark disparity. Despite having some of the highest infant mortality rates globally, the continent only has eight operational milk banks as of 2025, with facilities limited to South Africa, Kenya, Nigeria, Angola, Cameroon, Mozambique, Uganda, and Cape Verde [26]. The lack of human milk banking system and infrastructure in Africa demonstrates the existence of a serious gap in the availability of sufficient and optimal nutrition for vulnerable infants.
2. Results
The results consist of information about four key areas. One relates to current distribution and operational status, another to health outcomes, and another to implementation models and resource utilization. The results are organized into four main areas: current distribution and operational status, health outcomes, implementation models, and resource utilization (see Table 1 for a comprehensive summary of milk banks in Africa). Current distribution and status analysis revealed that formal human milk banking in Africa remains limited, with only eight countries having milk banks as of 2025. South Africa leads the continent, with the most developed network, operating over 20 milk banks integrated within its healthcare system since establishing its first bank in 2003. More recent implementations include Nigeria’s milk bank (2022) [27], and Uganda’s milk bank at St. Francis Hospital Nsambya (2021) [28].

Table 1.
Summary of existing human milk banks in Africa.
Table 2 highlights the reported benefits of utilizing donor human milk in African contexts. The key advantages of donor human milk include a reduced incidence of necrotizing enterocolitis (NEC), improved survival rates among vulnerable infants, enhanced immunological protection due to antibodies and bioactive components, better neurodevelopmental outcomes for low-birth-weight infants, and its critical role as an alternative feeding option for HIV-exposed infants in regions with high HIV prevalence [6]. These findings emphasize the importance of donor human milk in improving infant health outcomes.

Table 2.
Reported benefits of donor human milk in African contexts.
Human Milk Banks Implementation
South Africa is at the forefront of milk banking, opening the continent’s first human milk bank in 2003. Since then, South Africa has expanded its network to over 20 milk banks, serving neonatal units nationwide [44]. The Human Milk Banking Association of South Africa (HMBASA) has played a crucial role in establishing guidelines and promoting best practices for milk banking in the country [45].
Cameroon has at least six human milk banks [10], with one opening as early as 2006 at Bamenda Regional Hospital (Maternal & Child Health Advocacy International).
Cape Verde opened its first human milk bank in 2011 at Agostinho Neto Hospital in Praia, with support from the Brazilian government. In October 2018, Central Hospital Maputo in Mozambique opened its first human milk bank as part of a partnership between the Mozambique Ministry of Health, Brazil Ministry of Health, Fundação Oswaldo Cruz, and the Brazilian Cooperation Agency. The hospital follows the Brazilian human milk bank model as part of the Community of Portuguese-Speaking Countries Breast Milk Banks Network (Camera, 2018) [32]. Nigeria has also made strides in milk banking, with the first bank established in 2022 [27]. In 2019, Kenya launched its first public human milk bank at Pumwani Maternity Hospital in Nairobi as part of a pilot project supported by PATH and the Ministry of Health [45]. This initiative aims to provide donor milk to preterm and low-birth-weight infants in the neonatal intensive care unit [33]. In November 2019, the first human milk bank opened at the Lucrécia Paím Maternity Hospital in Luanda, Angola, as part of another partnership with Brazil’s Ministry of Health, Fundação Oswaldo Cruz, the Brazilian Cooperation Agency, and the Community of Portuguese Speaking Countries Breast Milk Banks Network [37].
In 2021, the first human milk bank was established in Kampala, Uganda, at St. Francis Hospital Nsambya [28]. By visiting and reviewing Pumwani Hospital’s human milk bank in Kenya, using the PATH Toolkit, assessing local needs, and working with a consultant expert in human milk banking, the project team was able to obtain the necessary resources and equipment, provide training and mentorship to healthcare workers, and begin the human milk bank.
Health outcomes studies from operational milk banks demonstrated significant positive health impacts. In South Africa, research by Coutsoudis et al. (2011 [46]) showed that donor milk implementation reduced necrotizing enterocolitis rates from 5.8% to 1.5% among very low-birth-weight infants [29]. Follow-up studies by Patra et al. (2017) [41] documented improved neurodevelopmental outcomes at 18 months for infants receiving donor milk compared to formula-fed counterparts, particularly in cognitive and motor development scores.
Implementation models and acceptance rates for donor milk showed regional variation but demonstrated an overall positive trend [41]. Recent studies in Ghana and Uganda reported that approximately 77% of surveyed women expressed willingness to donate milk, a significant improvement from earlier studies [38,39]. The South African model, operating under the Human Milk Banking Association of South Africa (HMBASA), emerged as the most comprehensive implementation framework, providing guidelines that other African nations have adopted. Despite these milk bank developments in recent years, several challenges exist (see Table 3).

Table 3.
Key barriers and challenges to human milk banking in Africa.
Table 3 displays Africa’s key barriers and challenges to human milk banking.
Resource utilization and sustainability analysis of operational costs and resource requirements revealed that while initial establishment costs were substantial, ongoing operations could be sustainable when integrated into existing healthcare systems (Table 4).

Table 4.
Strategies and opportunities for expanding human milk banking.
We found that wide accessibility and implementation disparities exist, even with the expansion of human milk banking in Africa. We identified countries with effective models; however, several factors continue to impact overall implementation and outcomes (See Figure 1).
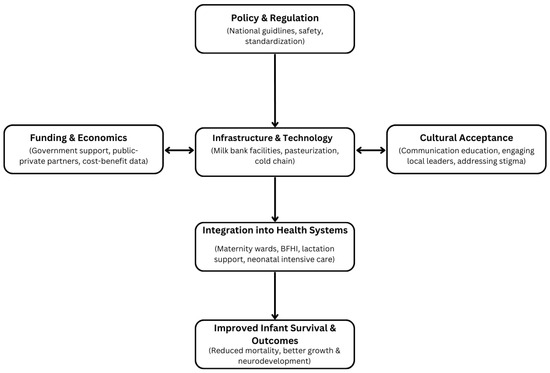
Figure 1.
Framework for human milk banking implementation in Africa, highlighting key components, challenges, and their interconnections to improve infant health outcomes.
3. Discussion
3.1. Infant Mortality Rates and the Need for Intervention
Whereas high-income countries experience 3 infant deaths per 1000 live births, Africa averages around 27 [47], typically due to premature birth, low birth weight, infection, and/or insufficient nutrition [48]. Many infants may have to rely on formula for their nourishment due to their mother being ill, dying, or not producing sufficient milk. Human milk contains more protective factors than formula, which can also be unsafe in areas with fewer resources [16]. Human milk must be made widely available, as it contains essential nutrients, antibodies, and bioactive compounds for vulnerable infants [16].
3.2. Advantages of Human Milk Banking
Donor milk is a safe alternative for infants of HIV-positive mothers, helping to avoid the risks associated with mixed feeding and the contaminated water used for formula preparation, particularly in regions with high HIV prevalence [52].
3.3. Utilizing Human Milk Banks to Reduce Disparities
Human milk bank expansion in Africa can narrow infant mortality disparities between African and high-income countries [53]. In order to expand milk banks and ensure their sustainability and reach, they must be integrated into existing maternal and child health programs [54]. One feasible example would be the inclusion of a human milk banks into the operation of neonatal care programs, even if limited in terms of resources.
Community outreach and engagement can also help with expansion, especially with the cultural stigma against receiving donor milk in many contexts [55]. Engaging with key partners may help to decrease community perceptions and misconceptions about donor milk. Additionally, innovation is important in reducing milk bank disparities, including involving technologies related to mobile milk banks and affordable pasteurization methods, decreasing the need for costly brick-and-mortar facilities in resource-limited areas [56]. Policy is another critical factor, as clear and evidence-based national guidelines regarding the recruitment of donors, the screening of donors, and milk pasteurization provide safety and efficacy measures. One model framework that other African countries could adopt is the Human Milk Banking Association of South Africa (HMBASA) [46]. Also, funding sustainability is critical, and some recommended funding models involve milk banks being integrated into national healthcare budgets and partnerships between the public and private sectors. These approaches outline strategies for expanding milk bank capacity to enhance and improve the continent’s infant and neonatal health outcomes.
3.4. Current Status of Human Milk Banking in Africa
Recently, human milk banks have been established on the continent [44] of Africa. Despite these positive developments in recent years, most African countries still lack formal milk banking systems. This leaves a critical gap in care for vulnerable infants who cannot access their mother’s milk. Informal milk-sharing practices exist in some communities, but these carry risks of disease transmission without proper screening and processing [39].
The scarcity of human milk banking systems in Africa highlights a critical need and gap in neonatal healthcare. Preterm or very-low-birth-weight infants face an increased risk of morbidity and mortality when maternal milk is inaccessible. In these situations, donor human milk can be life-saving to the infant, enriching them with essential nourishment for disease protection [4,8,9].
The sharing of milk in an informal manner, albeit necessary in some instances, carries great risks [48]. Unpasteurized milk, undergoing improper screening or none poses, infectious disease risks, such as HIV, hepatitis, and bacterial infections [55]. Thus, establishing formal milk banks that abide by rigorous safety protocols and standards ensures the safety and health of milk donors and recipients.
3.5. Potential Impact on Infant Mortality
The potential impact of expanded access to safe donor human milk on infant mortality in Africa is substantial, as studies indicate that positive maternal and infant health benefits are derived from using human milk, particularly by preterm and low-birth-weight infants [8,9]. These vulnerable newborns face high risks of life-threatening conditions, like necrotizing enterocolitis (NEC), when not fed human milk [4,8,9]. Studies from other regions have consistently shown that donor milk can significantly improve infant health and reduce NEC incidence compared to nonhuman milk [4,8,9].
A study by Coutsoudis et al. (2011) in South Africa found that introducing donor milk for infants of very low birth weight was associated with a significant reduction in NEC rates, from 5.8% to 1.5% [29]. This reduction in NEC incidence has important implications for survival, as NEC is a leading cause of mortality in preterm infants.
Beyond NEC prevention, human milk provides critical immunological and nutritional benefits that can improve outcomes for sick and premature infants [4,8,9,40,57]. The bioactive components in breast milk support gut health and brain development, and also provide protection against infections—factors which are crucial for survival and thriving in early life [4,8,9,16,40,57]. A case series by Reimers et al. [42] in South Africa documented the protective effects of donor human milk for abandoned and orphaned infants against failure to thrive, diarrhea, atopic dermatitis, and opportunistic infections. It is key to note that these infants had been exposed to or were positive for HIV.
Human milk banks provide safe nourishment for infants who may have mothers living with HIV who are unable to breastfeed. This helps to decrease the risks related to mixed feeding and the issues of safe formula accessibility in low-resource areas.
Beyond immediate survival, human milk feeding has significant implications for long-term neurodevelopmental outcomes, which is particularly relevant in the African context where follow-up care and early intervention services may be limited. A study by Patra et al. (2017) [41] in South Africa found that very low-birth-weight infants who received predominantly human milk during their NICU stay showed better neurodevelopmental outcomes at 18 months’ corrected age compared to those fed predominantly formula [4,16,40,57]. Specifically, they demonstrated higher cognitive and motor scores on the Bayley Scales of Infant Development. This aligns with findings from high-income countries, which show that human milk feeding is associated with improved cognitive outcomes, better development of white matter, and lower likelihood of cerebral palsy in preterm infants [4,16,40,57]. In low-resource areas with few options for neonatal care, providing essential nutrition through donor milk can be a practical, low-cost approach to achieving better health outcomes for vulnerable infants.
3.6. Challenges and Barriers
Although there are several potential benefits in the establishment and expansion of human milk banks in Africa, there are a variety of challenges.
3.6.1. Awareness and Cultural Acceptance
In many African communities, the concepts of milk banking and feeding an infant with another mother’s milk are unfamiliar and may face cultural barriers [39]. A study by Ighogboja Nigeria found that 71% of mothers would not accept donor milk for their babies [47]. However, significant education and awareness-raising efforts are still needed in many communities to initiate and operate human milk banks. Addressing these cultural concerns requires engagement with community leaders, healthcare providers, and religious figures to build trust and understanding about the safety and benefits of donor milk.
Religious beliefs as related to breast milk, particularly in Muslim-majority societies, can act as significant barriers to milk banking due to the concept of milk kinship. In Islam, infants who receive breastmilk from the same woman are considered milk siblings, establishing a kinship bond that prohibits future marriage [58,59]. This belief complicates both the donation and reception of human milk, as milk from multiple pooled donors makes kinship tracing impossible.
Despite these concerns, Islamic law does allow the use of donor milk under specific conditions. Some religious scholars have proposed milk banking models that align with Islamic guidelines, such as limiting milk pooling to three known donors or maintaining donor–recipient identity records [60]. However, past attempts to introduce formal milk banks in Muslim-majority countries were discontinued due to religious opposition, while small-scale milk exchange initiatives have seen limited expansion [47,61,62,63].
Addressing these religious concerns requires active engagement with religious leaders and scholars in order to develop milk banking models that are culturally and religiously acceptable. The proposed Conditional Identified Milk Banking System (CIMBS), which ensures traceability between donors and recipients, may provide a viable alternative [64]. Future milk banking initiatives in Muslim communities must integrate community education, religious discourse, and culturally tailored policies to increase acceptance and accessibility.
3.6.2. Infrastructure and Resource Limitations
Proper milk banking requires dedicated space, equipment for pasteurization and storage, reliable power, and cold chain systems—factors which can be lacking in resource-limited settings. It is very expensive to establish and operate milk banks, as evidenced by Tran. A study on the first human milk bank in Vietnam demonstrated the significant costs associated with establishment, ongoing operation, equipment fees, personnel training, and facility and operational costs [12]. In countries with limited resources, like those in Africa, these challenges are exacerbated by factors like resource accessibility and allocation and healthcare infrastructure. To help alleviate these issues, innovations involving technologies like mobile milk banks and affordable pasteurization are beneficial.
3.6.3. Screening and Safety Concerns
Although difficult to implement in laboratories with limited resources, the comprehensive and thorough screening of donors and testing of milk is vital to assure donor milk safety. Despite HIV and other pathogens being inactivated through the pasteurization process, trepidation about infections and HIV transmission remains. This creates a major barrier to establishing and running a milk bank in Africa.
Research by Naicker et al. (2015) [48] in South Africa demonstrated flash-heat pasteurization and its effectiveness in neutralizing bacteria in donor milk [48]. There must be a strong screening and pasteurization process to assure continual and effective safety and quality control standards and their maintenance.
3.6.4. Funding and Sustainability
Establishing sustainable funding sources remains a challenge in many African countries. While international donors or NGOs often support the establishment of milk banks, long-term sustainability requires integration into national health systems and budgets. Taylor et al. (2018) [49] conducted an economic analysis of donor milk allocation in South Africa, highlighting the cost-effectiveness of donor milk compared to formula but noting the need for the careful prioritization of limited donor milk supplies [49]. Human milk banks are vital, and governments must recognize this and develop systems for their proper funding. Additional funding frameworks that could provide financial stability and security may involve public and private partnerships and social impact bonds.
3.6.5. Policy and Regulatory Frameworks
Policies and guidelines on human milk banks are lacking throughout Africa, leading to varied and questionable quality control measures and practices. To increase the safety and efficacy of milk banks in Africa, following policies created by model programs, such as HMBASA in South Africa, is a recommendation. Comprehensive policies involve recruiting donors, screening donors, the pasteurization process, and storing and distributing milk. For policy adaptation, the WHO provides evidence-based approaches and best practices.
3.6.6. Competition with the Formula Industry
The widespread marketing and promotion of infant formula, particularly through campaigns targeting healthcare providers and mothers in Africa, can create challenges for breastfeeding, despite existing regulatory measures. Strengthening regulations and the enforcement of formula marketing policies is essential to ensuring informed feeding choices. Rather than framing it as competition, efforts should focus on complementary approaches that support breastfeeding while recognizing the role of both donor milk and infant formula in infant nutrition. Public health campaigns and health education messaging should emphasize the benefits of breastfeeding and donor milk, particularly for vulnerable infants. Improving infant and neonatal health will require a balanced approach, combining strong regulatory frameworks, public health initiatives, and education to support optimal feeding practices across diverse contexts.
3.7. Opportunities and Strategies for Expansion
Although there are significant challenges in Africa regarding milk bank establishment and expansion, opportunities do exist if hospitals collaborate. Bringing resources together help hospitals to share the funding burden.
3.7.1. Integration with Maternal and Newborn Health Programs
An integrative process of incorporating a milk bank within breastfeeding support and neonatal care offers a comprehensive approach to maternal and newborn health. Pumwani Maternity Hospital in Kenya is a prime example, with the milk bank integrated into the overall care improvement plan for newborns. This model ensures maternal and child health and increases milk bank sustainability.
3.7.2. Innovative Low-Resource Models
Low-cost and affordable pasteurization methods and mobile milk bank units are being developed for low-resource settings. For example, the FoneAstra pasteurization monitoring system, evaluated by Naicker et al. (2015) [48] in South Africa, provides a low-cost solution, using smartphones to guarantee safety during pasteurization for areas with limited access to resources [48]. Innovative solutions in African areas with few resources have the potential to overcome infrastructure and cost barriers in milk bank establishment.
3.7.3. Community Engagement and Education
Practicing cultural sensitivity and humility during outreach can enhance the acceptance of milk donations. Studies by Kimani-Murage et al. (2019) [11] and Magowan et al. (2020) [51] in Uganda highlighted the importance of community education in improving attitudes towards donor milk. Engaging religious leaders, traditional birth attendants, and other community influencers is especially important in milk bank promotion and acceptance [11,51].
3.7.4. Regional Cooperation
Cooperation and collaboration between countries are critical in establishing safe and effective milk bank systems in Africa, as seen in the partnership between Cape Verde and Brazil. Credible and trustworthy associations and networks, such as HMBASA in South Africa, are integral to promoting and establishing standardized milk bank practices and policies throughout Africa.
3.7.5. Policy Development
Safe and effective human milk banks require clear, evidence-based national guidelines and policies. The recent WHO initiative to develop global guidance on human milk banking, as described by Tyebally Fang et al. (2021), could provide a valuable framework for African countries to adapt to their specific contexts [25].
3.7.6. Partnerships
Engagement with NGOs, professional associations, and the private sector can provide technical and fiscal support for milk bank establishment and maintenance. The partnering between PATH, South Africa, and Kenya demonstrates the importance of community and organizational engagement and connection in successfully operating human milk banks.
3.8. Current Human Milk Bank Practices in Africa, Europe, and the Americas
Excluding South Africa, most other African countries are still in the infancy stages of developing structured and organized human milk bank systems that employ standardized and evidence-based practices. However, one particular program in Kenya, the mother–baby-friendly initiative, is particularly effective due to its systematic and step-by-step framework. It involves key public health partners in planning, implementation, and evaluation [25]. Although Uganda managed to establish its first human milk bank recently, challenges arose in the beginning phase due to the absence of national human milk bank guidelines [28].
In Europe, there is a well-established network of human milk banks, with at least 282 currently active and at least 18 in the planning phase [58]. Italy has the highest number of human milk banks in Europe, and in 2023, it developed comprehensive guidelines for establishing and operating human milk banks and all evidence-based practices involved [59]. Interestingly, the regulation of donor human milk varies throughout Europe, as it can be considered a tissue (the most regulated), a food, or a health product [60].
In North America, there are more than 30 human milk banks [61], and the HMBANA publishes guidelines for human milk banking and handling. The latest guidelines are comprehensive and include information on establishing clear protocols for handling milk safely in various settings, providing evidence-based approaches for milk storage and disposal, demonstrating the best methods for expressing milk in various settings, the proper sanitizing of equipment, milk transportation, training staff, and quality control approaches and procedures [62].
Of the South American countries, Brazil is recognized as a world leader in human milk banking, with 227 milk banks and 234 collection points connected via the Brazilian Network of Human Milk Banks [63]. Although not a high-income country, Brazil provides a global model for human milk banking, with a framework that is integrated into the country’s healthcare system. It is simplified and requires less expensive resources while still providing proper staff training and maternal and infant care, support, and education. Additionally, the model extends to dozens of other countries, including those in Africa [25].
3.9. Limitations
The main limitation is the paucity of published research on African human milk banks. Most existing studies are concentrated in just a few countries—South Africa, Ghana, and Nigeria—limiting the generalizability of findings across the diverse African continent. Additionally, although short-term studies have been documented, there is a notable lack of long-term follow-up studies of infant health outcomes after receiving donor milk in settings in African contexts. Outcomes for infants receiving donor milk in African settings are unstudied, although short-term benefits are well-documented. Additionally, standardized policies and guidelines on human milk banking do not exist in Africa, leading to a wide variety of practices and measures related to quality control. This hinders the ability to compare outcomes and establish best practices.
Considerable resource limitations exist throughout the continent, especially in terms of specialized equipment availability, power supply reliability, and correctly and adequately trained workers. Cost can also be a limiting factor, as establishing and maintaining a milk bank is costly without a sustainable funding source. These cost factors can hinder the operation of the milk bank and limit research opportunities.
Cultural and social misconceptions and beliefs also hinder the acceptance of donor milk, even with growing awareness campaigns in some areas.
These factors and limitations demonstrate that some research examines these issues throughout Africa, that standardized and clear guidelines are being developed, and that cultural humility and sensitivity are utilized in human milk bank establishment and implementation.
3.10. Future Directions
The future development of human milk banking in Africa requires a multifaceted approach centered on research expansion and infrastructure development. Priority should be given to conducting comprehensive studies across diverse African contexts that examine both the immediate and long-term outcomes of donor milk programs, with a special emphasis on infant growth, development, and health outcomes. Working in concert with this research is the construction and development of sound and clear policies and guidelines that follow WHO frameworks and that are adaptable to different contexts. Innovation in low-resource areas, such as mobile milk banks and more affordable pasteurization technology options, will fulfill the final necessity of expanding milk banks to areas with the highest needs.
Program sustainability largely depends on community engagement and support by key partners and leaders, as well as dependable funding sources.
Additionally, educational campaigns must address cultural barriers, provide health education, and promote the benefits of milk banks for vulnerable infants. Also, establishing funding sustainability is critical. This primarily occurs through partnerships between public and private sectors and integration into the national healthcare budgets of countries. Utilizing model frameworks, like that of South Africa, and connecting regions of the continent in milk bank operations will help to strengthen the capacity to develop these life-saving systems. Evaluation is also critical, as consistent and accurate data collection and surveillance will provide key information to assure continual improvement and quality.
4. Materials and Methods
This literature review was part of a human milk banking population needs assessment approved by the Indiana University Institutional Review Board (IRB). We based our review on Arksey and O’Malley’s (2005) framework, a mapping process suitable for broad topics when available research is limited [65]. Given the emerging nature of human milk banking in Africa, this approach allowed for a comprehensive examination of formal research and gray literature while maintaining methodological rigor.
The review began with the development of our primary research question: “What is the current state of human milk banking in Africa, and how can expanding access to donor milk reduce infant mortality and improve neonatal health outcomes on the continent?” This question was deliberately structured to encompass current practices and future potential, including infrastructure, implementation strategies, health outcomes, and barriers to expansion.
We performed a comprehensive literature review using multiple databases, including Pub Med, Google Scholar, and African Journals Online, covering publications through January 2024. Additional sources included WHO and UNICEF databases and national health ministry repositories. We combined search terms using Boolean operators and included variations of “human milk banking,” “donor milk,” and “breast milk bank,” along with geographic terms specific to Africa and individual country names. We also included outcome-related terms such as “infant mortality” and “neonatal health” and implementation-specific terms like “milk bank establishment” and “donor screening.”
We used the following inclusion criteria for study selection: original research on human milk banking in African contexts, policy documents and guidelines from recognized organizations, case studies of existing African milk banks, and studies addressing cultural, technical, or operational aspects of milk banking. We excluded studies focused solely on breastfeeding without milk banking components, research conducted outside of Africa or without an African context, and non-peer-reviewed publications. Data extraction focused on key themes, including milk banking infrastructure, health outcomes, cultural factors, implementation challenges, policy frameworks, and resource requirements.
Quality assurance measures included an independent review of selected studies by multiple researchers and cross-verification with existing systematic reviews. Additionally, we made a rigorous effort to include work from experts and consultants who played a crucial role in the establishment of the first human milk bank in an African country.
The findings were thematically synthesized to identify patterns in current practices, outcomes, barriers, and the expansion opportunities. This approach enabled us to maintain a comprehensive view of the field while ensuring practical applicability for future implementation efforts in African contexts.
All evidence was critically evaluated to assess quality and relevance to the context of Africa, especially regarding implementation likelihood in resource-deficient areas. Our review identified critical frameworks and models and major challenges for implementing human milk bank systems nationwide.
5. Conclusions
Africa has significant opportunities to develop life-saving and life-preserving human milk bank systems, which can be integrated with maternal and child health services, despite the existence of numerous hurdles and challenges (e.g., cultural limitations, lack of resources, and policy deficiencies). Groundbreaking advances in milk banking in South Africa provide valuable lessons for scaling up milk banking across the continent. With proper investment, supportive policies, and community engagement, expanded access to safe donor human milk could play an important role in reducing the unacceptably high infant mortality rates that persist in many parts of Africa. As more countries establish milk banks and build evidence of their impact, the momentum for expanding this life-saving intervention will likely grow.
Author Contributions
Conceptualization, B.O.-G.; methodology, B.O.-G. and C.S.O.; software, B.O.-G. and C.S.O.; validation, C.S.O., E.O.-G., T.M.N. and K.B.; formal analysis, C.S.O. and B.O.-G.; investigation, C.S.O. and B.O.-G.; resources, C.S.O.; data curation, B.O.-G. and C.S.O.; writing—original draft preparation, B.O.-G.; writing—review and editing, C.S.O., T.M.N., B.O.-G., K.B. and E.O.-G.; visualization, C.S.O. supervision, C.S.O.; project administration, C.S.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Indiana University Institutional Review Board (Protocol ##15224 Date (26 April 2022)).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study. The authors affirm that human research participants provided informed consent for publication.
Data Availability Statement
The data from this study are available upon reasonable request and approval by the IRB of the author’s institution.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kehinde, J.; O’Donnell, C.; Grealish, A. The effectiveness of prenatal breastfeeding education on breastfeeding uptake postpartum: A systematic review. Midwifery 2023, 118, 103579. [Google Scholar] [CrossRef] [PubMed]
- Boquien, C.-Y. Human milk: An ideal food for nutrition of preterm newborn. Front. Pediatr. 2018, 6, 295. [Google Scholar] [CrossRef] [PubMed]
- Israel-Ballard, K.; Cohen, J.; Mansen, K.; Parker, M.; Engmann, C.; Kelley, M.; Brooks, E.; Chatzixiros, E.; Clark, D.; Grummer-Strawn, L.; et al. Call to action for equitable access to human milk for vulnerable infants. Lancet Glob. Health 2019, 7, e1484–e1486. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Bahl, R.; Barros, A.J.; França, G.V.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef] [PubMed]
- Dritsakou, K.; Liosis, G.; Valsami, G.; Polychronopoulos, E.; Souliotis, K.; Skouroliakou, M. Mother’s breast milk supplemented with donor milk reduces hospital and health service usage costs in low-birthweight infants. Midwifery 2016, 40, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Wight, N.E. Donor human milk for preterm infants. J. Perinatol. 2001, 21, 249–254. [Google Scholar] [CrossRef]
- Chantry, C.J.; Eglash, A.; Labbok, M. ABM Position on Breastfeeding-Revised 2015. Breastfeed. Med. 2015, 10, 407–411. [Google Scholar] [CrossRef]
- Chowdhury, R.; Sinha, B.; Sankar, M.J.; Taneja, S.; Bhandari, N.; Rollins, N.; Bahl, R.; Martines, J. Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 96–113. [Google Scholar] [CrossRef]
- Eidelman, A.I. Breastfeeding and the use of human milk: An analysis of the American Academy of Pediatrics 2012 Breastfeeding Policy Statement. Breastfeed. Med. 2012, 7, 323–324. [Google Scholar] [CrossRef] [PubMed]
- Haiden, N.; Ziegler, E.E. Human Milk Banking. Ann. Nutr. Metab. 2016, 69 (Suppl. 2), 8–15. [Google Scholar] [CrossRef]
- Kimani-Murage, E.W.; Wanjohi, M.N.; Kamande, E.W.; Macharia, T.N.; Mwaniki, E.; Zerfu, T.; Ziraba, A.; Muiruri, J.W.; Samburu, B.; Govoga, A.; et al. Perceptions on donated human milk and human milk banking in Nairobi, Kenya. Matern. Child Nutr. 2019, 15, e12842. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.T.; Nguyen, T.T.; Barnett, D.; Weaver, G.; Nguyen, O.T.X.; Van Ngo, Q.; Le, H.T.T.; Huynh, L.T.; Do, C.T.; Mathisen, R. Trends and Dynamics in the First Four Years of Operation of the First Human Milk Bank in Vietnam. Nutrients 2021, 13, 1107. [Google Scholar] [CrossRef]
- Ndezwa, R. Assessing the Need for Donated Breast Milk Use and Human Milk Banking in Kenyatta National Hospital. Master’s Thesis, University of Nairobi, Nairobi, Kenya, 2020. [Google Scholar]
- Nangia, S.; Sachdeva, R.C.; Sabharwal, V. Human milk banking: An Indian experience. Neoreviews 2018, 19, e201–e210. [Google Scholar] [CrossRef]
- Wagg, A.J.; Hassett, A.; Callanan, M.M. “It’s more than milk, it’s mental health”: A case of online human milk sharing. Int. Breastfeed. J. 2022, 17, 5. [Google Scholar] [CrossRef]
- Quigley, M.; Embleton, N.D.; McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 2019, 7, CD002971. [Google Scholar] [CrossRef] [PubMed]
- Parker, M.G.; Stellwagen, L.M.; Noble, L.; Kim, J.H.; Poindexter, B.B.; Puopolo, K.M. Promoting human milk and breastfeeding for the very low birth weight infant. Pediatrics 2021, 148, e2021054272. [Google Scholar] [CrossRef] [PubMed]
- Stubbe, D.E. Practicing Cultural Competence and Cultural Humility in the Care of Diverse Patients. Focus 2020, 18, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Committee on Nutrition; Section on Breastfeeding; Committee on Fetus and Newborn; Daniels, S.; Corkins, M.; de Ferranti, S.; Golden, N.H.; Kim, J.H.; Magge, S.N.; Schwarzenberg, S.J.; et al. Donor Human Milk for the High-Risk Infant: Preparation, Safety, and Usage Options in the United States. Pediatrics 2017, 139, e20163440. [Google Scholar] [CrossRef]
- Arslanoglu, S.; Corpeleijn, W.; Moro, G.; Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Domellöf, M.; Fewtrell, M.; Hojsak, I. Donor human milk for preterm infants: Current evidence and research directions. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 535–542. [Google Scholar]
- Corpeleijn, W.E.; Vermeulen, M.J.; van Vliet, I.; Kruger, C.; van Goudoever, J.B. Human milk banking-facts and issues to resolve. Nutrients 2010, 2, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Kair, L.R.; Flaherman, V.J.; Newby, K.A.; Colaizy, T.T. The experience of breastfeeding the late preterm infant: A qualitative study. Breastfeed. Med. 2015, 10, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, M.R.; Kair, L.R.; Sipsma, H.L.; Phillipi, C.A.; Larson, I.A. Human Donor Milk or Formula: A Qualitative Study of Maternal Perspectives on Supplementation. Breastfeed. Med. 2018, 13, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Marinelli, K.A.; Ball, H.L.; McKenna, J.J.; Blair, P.S. An Integrated Analysis of Maternal-Infant Sleep, Breastfeeding, and Sudden Infant Death Syndrome Research Supporting a Balanced Discourse. J. Hum. Lact. 2019, 35, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Tyebally Fang, M.; Chatzixiros, E.; Grummer-Strawn, L.; Engmann, C.; Israel-Ballard, K.; Mansen, K.; O’Connor, D.L.; Unger, S.; Herson, M.; Weaver, G.; et al. Developing global guidance on human milk banking. Bull. World Health Organ. 2021, 99, 892–900. [Google Scholar] [CrossRef] [PubMed]
- Moges, N.; Dessie, A.M.; Anley, D.T.; Zemene, M.A.; Gebeyehu, N.A.; Adella, G.A.; Kassie, G.A.; Mengstie, M.A.; Seid, M.A.; Abebe, E.C.; et al. Burden of early neonatal mortality in Sub-Saharan Africa. A systematic review and meta-analysis. PLoS ONE 2024, 19, e0306297. [Google Scholar] [CrossRef] [PubMed]
- Alagboso, C.O. Onyinye Saving Lives: Nigeria’s First Breast Milk Bank Gives Babies a Fighting Chance. Available online: https://articles.nigeriahealthwatch.com/saving-lives-nigerias-first-breast-milk-bank-gives-babies-a-fighting-chance/ (accessed on 14 January 2025).
- Nakibuuka, V.; Kainza, J.; Nasiima, R.; Nalunga, S.; Nazziwa, R.; Mponye, H.; Nuwahereza, C.; Kyambadde, R.; Nantenza, R.; Nassonko, C. Setting up the first human milk bank in Uganda: A success story from Nsambya hospital. Front. Nutr. 2024, 10, 1275877. [Google Scholar] [CrossRef]
- Coutsoudis, I.; Petrites, A.; Coutsoudis, A. Acceptability of donated breast milk in a resource limited South African setting. Int. Breastfeed. J. 2011, 6, 3. [Google Scholar] [CrossRef]
- Program-for-Appropriate-Technology-in-Health. Models of Milk Banking in South Africa. Available online: https://media.path.org/documents/MCHN_5_milk_banking_models.pdf (accessed on 14 January 2025).
- Villanueva, T. First human breast milk bank opens in Africa. BMJ Br. Med. J. (Online) 2011, 343, d5179. [Google Scholar] [CrossRef] [PubMed]
- Câmera, A. First breast milk bank opens in Mozambique. Available online: https://portal.fiocruz.br/en/news/first-breast-milk-bank-opens-mozambique (accessed on 14 January 2025).
- Bandeira, S.; Joaquim, R.; Janasse, S.; Balate, M.; Amaral, D.; João, D. Home collection as a strategy to increase human milk donations during the COVID-19 pandemic in Mozambique. J. Afr. Neonatol. 2023, 1, 19–26. [Google Scholar]
- Wilunda, C.; Israel-Ballard, K.; Wanjohi, M.; Lang’at, N.; Mansen, K.; Waiyego, M.; Kibore, M.; Kamande, E.; Zerfu, T.; Kithua, A. Potential effectiveness of integrating human milk banking and lactation support on neonatal outcomes at Pumwani Maternity Hospital, Kenya. Matern. Child Nutr. 2024, 20, e13594. [Google Scholar] [CrossRef] [PubMed]
- VERANGOLA. Ministers of Health of Angola and Brazil Visited a Human Milk Bank. Available online: https://www.verangola.net/va/en/082023/Health/36942/Ministers-of-Health-of-Angola-and-Brazil-visited-a-human-milk-bank.htm (accessed on 14 January 2025).
- Lusa/VERANOLA. Doctor Defends Human Milk Bank as Public Policy in the Country. Available online: https://www.verangola.net/va/en/052024/Health/39950/Doctor-defends-Human-Milk-Bank-as-public-policy-in-the-country.htm (accessed on 14 January 2025).
- Plessmann, J. Brazil opens 3rd Human Milk Bank in Africa. Available online: https://portal.fiocruz.br/en/news/brazil-opens-3rd-human-milk-bank-africa (accessed on 14 January 2025).
- Ahmed, M.A.M.; Namisi, C.P.; Kirabira, N.V.; Lwetabe, M.W.; Rujumba, J. Acceptability to donate human milk among postnatal mothers at St. Francis hospital Nsambya, Uganda: A mixed method study. Int. Breastfeed. J. 2024, 19, 9. [Google Scholar] [CrossRef]
- Obeng, C.; Jackson, F.; Amissah-Essel, S.; Nsiah-Asamoah, C.; Perry, C.A.; Gonzalez Casanova, I.; Obeng-Gyasi, E. Women’s perspectives on human milk banking in Ghana: Results from a cross-sectional study. Front. Public Health 2023, 11, 1128375. [Google Scholar] [CrossRef] [PubMed]
- Adhisivam, B.; Vishnu Bhat, B.; Banupriya, N.; Poorna, R.; Plakkal, N.; Palanivel, C. Impact of human milk banking on neonatal mortality, necrotizing enterocolitis, and exclusive breastfeeding—Experience from a tertiary care teaching hospital, south India. J. Matern. Fetal Neonatal Med. 2019, 32, 902–905. [Google Scholar] [CrossRef]
- Patra, K.; Hamilton, M.; Johnson, T.J.; Greene, M.; Dabrowski, E.; Meier, P.P.; Patel, A.L. NICU Human Milk Dose and 20-Month Neurodevelopmental Outcome in Very Low Birth Weight Infants. Neonatology 2017, 112, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Reimers, P.; Israel-Ballard, K.; Craig, M.; Spies, L.; Thior, I.; Tanser, F.; Coutsoudis, A. A cluster randomised trial to determine the efficacy of the “feeding buddies” programme in improving exclusive breastfeeding rates among HIV-infected women in rural KwaZulu-Natal, South Africa. AIDS Behav. 2018, 22, 212–223. [Google Scholar] [CrossRef]
- Powell, A.M.; Knott-Grasso, M.A.; Anderson, J.; Livingston, A.; Rosenblum, N.; Sturdivant, H.; Byrnes, K.C.; Martel, K.; Sheffield, J.S.; Golden, W.C. Infant feeding for people living with HIV in high resource settings: A multi-disciplinary approach with best practices to maximise risk reduction. Lancet Reg. Health–Am. 2023, 22, 100509. [Google Scholar] [CrossRef]
- Mathias, E.G.; Patil, D.S.; Kolakemar, A.; Krishnan, J.B.; Renjith, V.; Gudi, N.; Swamy, R.S.; Brand, A. Barriers and facilitators for the donation and acceptance of human breast milk: A scoping review. Curr. Nutr. Rep. 2023, 12, 617–634. [Google Scholar] [CrossRef] [PubMed]
- PATH. A Resource Toolkit for Establishing and Integrating Human Milk Bank Programs—A Global Implementation Framework; PATH: Seattle, WA, USA, 2019. [Google Scholar]
- Coutsoudis, I.; Adhikari, M.; Nair, N.; Coutsoudis, A. Feasibility and safety of setting up a donor breastmilk bank in a neonatal prem unit in a resource limited setting: An observational, longitudinal cohort study. BMC Public Health 2011, 11, 356. [Google Scholar] [CrossRef] [PubMed]
- Ighogboja, I.S.; Olarewaju, R.S.; Odumodu, C.U.; Okuonghae, H.O. Mothers’ attitudes towards donated breastmilk in Jos, Nigeria. J. Hum. Lact. 1995, 11, 93–96. [Google Scholar] [CrossRef]
- Naicker, M.; Coutsoudis, A.; Israel-Ballard, K.; Chaudhri, R.; Perin, N.; Mlisana, K. Demonstrating the efficacy of the FoneAstra pasteurization monitor for human milk pasteurization in resource-limited settings. Breastfeed. Med. 2015, 10, 107–112. [Google Scholar] [CrossRef]
- Taylor, C.; Joolay, Y.; Buckle, A.; Lilford, R. Prioritising allocation of donor human breast milk amongst very low birthweight infants in middle-income countries. Matern. Child Nutr. 2018, 14 (Suppl. 6), e12595. [Google Scholar] [CrossRef]
- World-Health-Organization. Baby-friendly Hospital Initiative Training Course for Maternity Staff: Customisation Guide. Available online: https://www.who.int/publications/i/item/9789240008915 (accessed on 14 January 2025).
- Magowan, S.; Burgoine, K.; Ogara, C.; Ditai, J.; Gladstone, M. Exploring the barriers and facilitators to the acceptability of donor human milk in eastern Uganda—A qualitative study. Int. Breastfeed. J. 2020, 15, 28. [Google Scholar] [CrossRef] [PubMed]
- Hanson, L.; Korotkova, M.; Telemo, E. Human milk: Its components and their immunobiologic functions. In Mucosal Immunology; Elsevier: Amsterdam, The Netherlands, 2005; pp. 1795–1827. [Google Scholar]
- Lurie, N.; Dubowitz, T. Health disparities and access to health. Jama 2007, 297, 1118–1121. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. An Evidence Map of Social, Behavioural and Community Engagement Interventions for Reproductive, Maternal, Newborn and Child Health; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Subudhi, S.; Sriraman, N. Islamic beliefs about milk kinship and donor human milk in the United States. Pediatrics 2021, 147, e20200441. [Google Scholar] [CrossRef]
- Chaudhri, R.; Vlachos, D.; Borriello, G.; Israel-Ballard, K.; Coutsoudis, A.; Reimers, P.; Perin, N. Decentralized human milk banking with ODK sensors. In Proceedings of the 3rd ACM Symposium on Computing for Development, Bangalore, India, 11–12 January 2013; pp. 1–10. [Google Scholar]
- McGuire, W.; Anthony, M.Y. Donor human milk versus formula for preventing necrotising enterocolitis in preterm infants: Systematic review. Arch. Dis. Child. Fetal Neonatal Ed. 2003, 88, F11–F14. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.; Buffin, R.; Sanlaville, D.; Picaud, J.C. Milk kinship is not an obstacle to using donor human milk to feed preterm infants in Muslim countries. Acta Paediatr. 2016, 105, 462–467. [Google Scholar] [CrossRef]
- Ozdemir, R.; Ak, M.; Karatas, M.; Ozer, A.; Dogan, D.; Karadag, A. Human milk banking and milk kinship: Perspectives of religious officers in a Muslim country. J. Perinatol. 2015, 35, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.K.; Reyes-Foster, B.M. Introduction: Sharing Milk. In Sharing Milk; Bristol University Press: Bristol, UK, 2020; pp. 1–34. [Google Scholar]
- Varer Akpinar, C.; Mandiracioglu, A.; Ozvurmaz, S.; Adana, F.; Koc, N.; Kurt, F. Attitudes towards human milk banking among native turkish and refugee women residing in a rural region of Turkey: A mixed-methods approach. Int. Breastfeed. J. 2022, 17, 74. [Google Scholar] [CrossRef]
- Al Naqeeb, N.; Tolba, A.; Elhassanin, A.F.; Adel Ata, S.; Azab, A. Ambulatory human milk donors: An innovative solution for human milk banking in Muslim countries. J. Hum. Lact. 2021, 37, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, K.; Dahlui, M.; Nik Farid, N.D. Motivators and barriers to the acceptability of a human milk bank among Malaysians. PLoS ONE 2024, 19, e0299308. [Google Scholar] [CrossRef]
- Alnakshabandi, K.; Fiester, A. Creating religiously compliant milk banks in the Muslim world: A commentary. Paediatr. Int. Child Health 2016, 36, 4–6. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).