Abstract
This study sought to investigate the macro determinants of maternal mortality in Southern African Development Community (SADC) states. The study drew on the fact that maternal mortality remains a major public health issue in developing countries. The Millennium Development Goals (MDGs) were adopted by UN member states in 2000, and one of them was to reduce maternal deaths by three-quarters by 2015. While the Millennium Development Goals increased efforts, the goal was not met in the countries with the highest death rates. The World Health Organisation (WHO) estimates that every single day about 810 women die from pregnancy or childbirth-related complications around the world. This is despite several international initiatives being adopted to reduce maternal mortality. The study was quantitative, and it used secondary data to achieve its objective. A panel data estimation (Generalized Method of Moments) covering the period from 2005–2019 was used to examine how various factors affect maternal mortality. The analysis included the following variables: education, fertility, GDP per capita, institutional quality, health expenditure and HIV infection. The econometric analysis reveals a significant positive impact of fertility, GDP per capita and HIV on maternal mortality. This implies that when fertility, GDP per capita and HIV are increasing, maternal mortality also increases. The analysis also showed that education has a negative relationship with maternal mortality. This implies that when literacy levels (education) increase, maternal mortality decreases. Based on the results, this study emphasizes that, in order to improve maternal health and consequently reduce maternal mortality, access to family planning (to reduce fertility), access to early prenatal care and promoting women’s access to education should be a priority in government policies.
1. Introduction
Maternal mortality remains a major public health issue in developing countries. The World Health Organisation (WHO) estimates that every single day about 810 women die from pregnancy or childbirth-related complications around the world [1]. This is despite several international initiatives being adopted to reduce maternal mortality. In 1987, the WHO launched the Safe Motherhood Initiative and it was intended to improve the quality of maternal health around the world [2,3]. This global initiative was created to build political will, find effective interventions and organize resources to address maternal mortality [4]. The Millennium Development Goals (MDGs) were adopted by UN member states in 2000, and one of them was to reduce maternal deaths by three-quarters by 2015. While the Millennium Development Goals increased efforts, the goal was not met in low-income countries. The problem has really gotten worse in some countries [5,6]. Sub-Saharan Africa is a case in point. The majority of maternal deaths occur in sub-Saharan Africa, which accounted for two-thirds of global maternal deaths in 2017 [7,8,9,10].
Failure to improve maternal health in sub-Saharan African countries has adverse effects as it affects a variety of health and socioeconomic outcomes. A maternal death can have a detrimental impact on families, including the family members’ physical and mental health. A growing body of evidence shows that maternal mortality has negative consequences for children who are left behind [11,12]. Mothers’ and children’s health outcomes are intricately linked; maternal mortality and morbidities have an impact on newborn and child survival, growth and development [13,14,15]. Often a maternal death can have spillover effects on child health, via obstetric complications, infant feeding behaviors and care for orphans [16]. The death of a mother substantially increases the likelihood that her newborn child will die. Bazile et al. [17] observed that the loss of a mother increased the vulnerability of surviving children to sickness and starvation, reduced and derailed education and resulted in early work involvement, marriage and/or parenthood. Knight et al. [18] used focus group qualitative methodologies to investigate the effects of a mother’s death on surviving children and families. The study found the following effects: substantial financial costs, missed educational chances and sexual and social danger. The study further showed that adolescents, even those who couldn’t recall their mothers, had a harder time transitioning to adulthood, especially older female children.
Maternal and newborn deaths also slow economic growth and lead to global productivity losses [19]. On the other hand, investing in better health for women and babies has far-reaching benefits for countries. For example, between one-third and one-half of Asia’s economic growth from 1965 to 1990 has been attributed to improvements in reproductive health and reductions in infant and child mortality and fertility rates [19,20]. In the majority of low-income countries, reducing maternal and infant mortality will impact GDP, and reducing child mortality by 1% could also increase GDP by as much as 4.6% in African countries [21,22]. Stenberg et al. [23] suggest that increasing health expenditure by just five US$ per person per year through 2035 in the 74 countries that account for the bulk of maternal and child mortality could yield up to nine times that value in social and economic benefits. In Bangladesh, for example, research shows that impoverished families with maternal health issues spend 30 to 40% of their savings to cover expenses, compared to only 8% for the richest quintile [23]. In many developing countries, a mother’s death is much more than an emotional crisis, often leading to long-term social and economic breakdown, both for her immediate family and the wider community [24].
Given the psychological, socio-economic and economic problems that people and economies experience after a maternal death, maternal mortality is undeniably a terrible injustice. In order to reduce maternal mortality and its negative socioeconomic consequences, it is necessary to identify the factors that influence it. Determinants can be at individual level (micro), it can be at the level of health care provision (meso) or at the wider societal level (macro) within a given context [25]. The major medical causes of maternal morbidity and mortality include haemorrhage, infection, high blood pressure, unsafe abortion and obstructed labour [26,27,28,29,30]. However, it should be noted that these factors are micro in nature, and little has been done to investigate the macro determinants of maternal mortality [31]. Macro factors refer to the broader political, institutional, economic, social and environmental conditions and institutions at national, regional or international levels that influence maternal mortality. These macro-level factors include: availability of skilled attendance, family planning, poverty, female education, access to reproductive health care services, government expenditure, fertility and HIV [32,33,34,35,36]. Understanding the macro-level factors that influence maternal mortality and their relative importance for health policy and planning is a critical component of putting successful programs to reduce maternal mortality in place in Africa. The purpose of this paper is, therefore, to investigate the macro determinants of maternal mortality in Southern African Development Countries (SADC). The analysis included the following variables: education, fertility, GDP per capita, health expenditure and HIV infection.
The rest of the study is organized into five sections. Section 2 reviews the trends in selected macro-level factors that affect maternal mortality. The purpose of the section is to demonstrate how African nations compare to the rest of the world in terms of the factors that influence maternal mortality. Section 3 discusses and synthesizes a review of the relevant literature. Section 4 discusses the data methods and the econometric approach used in the study. In Section 5 the results of the econometric analysis are presented and discussed. The last section, Section 6, concludes the study and offers policy recommendations.
2. A Review of the Trends in Maternal Mortality
Maternal mortality rates have generally decreased in recent years as countries work toward the Sustainable Development Goal of lowering the global maternal mortality ratio to fewer than 70 deaths per 100,000 live births by 2030. Unfortunately, certain parts of the world are still far from achieving this goal. Figure 1 shows the maternal deaths per 100,000 live births in different regions of the world.
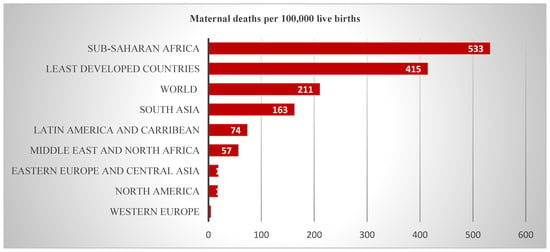
Figure 1.
Maternal deaths per 100,000 live births (2017). Source: Graph computed using statistics from the World Bank (2022). World Bank. 2022. Indicators. Available online: https://data.worldbank.org/indicator (accessed on 25 April 2022).
Figure 1 shows that sub-Saharan Africa continues to have the highest maternal death rate, followed by Central and South Asia. Figure 1 also shows that in 2017, sub-Saharan Africans suffered from the highest maternal mortality ratio (MMR) of 533 maternal deaths per 100,000 live births. This is even higher than the average MMR for the least developing countries (415) and the world average (211). The SADC region falls under the sub-Saharan region. Fifteen of the sixteen nations with very high maternal mortality rates—500–999 deaths per 100,000 live births—were in sub-Saharan Africa, with Haiti being the only country outside that area [37]. Several factors have been seen to be causing the high maternal mortality. One of these factors is the utilisation of antenatal care. One of the major causes of maternal mortality is the insufficient use of antenatal care (ANC) services [38]. Women and newborn babies can be saved with expert treatment before, during and after childbirth. ANC enables the early detection and treatment of pregnancy-related problems, as well as the prevention and control of concomitant disorders [39,40]. However, in some countries of sub-Saharan Africa pregnant women do not attend any pregnancy-related appointments [41]. Figure 2 shows the trends in pregnant women receiving prenatal care in different regions of the world.
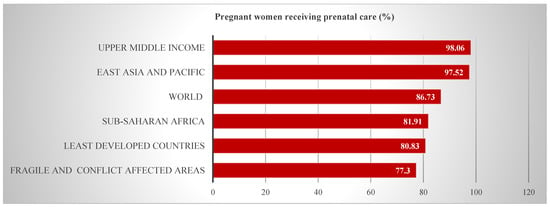
Figure 2.
Pregnant women receiving prenatal care (2020). Source: Graph computed using statistics from the World Bank (2022).
Figure 2 shows that sub-Saharan Africa’s percentage of pregnant women receiving prenatal care (81.91%) is below the world average (86.73%). The percentage of pregnant women in sub-Saharan Africa who receive prenatal care is comparable to that of least developed countries (80.83%). This shows that developing countries face challenges when it comes to prenatal care [41]. Despite the fact that 81% of women have at least one ANC consultation, many do not receive the entire range of evidence-based components during pregnancy [39,42]. However, it must be noted that, under normal circumstances, the World Health Organization (WHO) recommended that a pregnant woman should have at least four ANC visits [43,44]. African countries still fall short of this. Almost all women in high-income nations have at least four antenatal appointments, are attended by a professional health worker during labor and receive postpartum care. In 2015, 40% of pregnant women in low-income countries received the recommended prenatal care visits [42,45]. This shows that there is a substantial quality deficit in ANC facilities in sub-Saharan Africa.
Another factor that has been linked to high maternal mortality in sub-Saharan Africa is the lack of qualified health staff present at births. One of the primary indicators in the Sustainable Development Goals (SDG) is to increase the number of births supported by qualified health staff to 90%. However, despite recent progress, millions of births, and maternal deaths, occur each year without the support of a skilled attendant [46]. Figure 3 shows the percentage of births attended by skilled health staff.
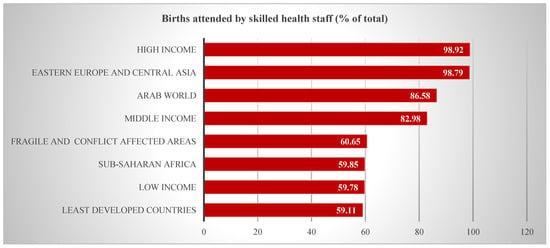
Figure 3.
Births attended by skilled health staff (2020). Source: Graph computed using statistics from the World Bank (2022).
Figure 3 shows that in SSA only 59% of births were assisted by skilled health personnel in 2020 compared to 87% in the Arab world, 98% in high-income countries and 99% in Europe and Central Asia. Sub-Saharan Africa’s percentage is even lower than that of fragile and conflict-affected areas (60.65%). This shows that there is a substantial shortage of skilled health staff in sub-Saharan Africa. Darmian et al. [47] state that the main issue is that in most sub-Saharan African nations, coverage of deliveries attended by qualified health staff remains poor, despite the region accounting for 66% of global maternal fatalities. It should be underlined, however, that not having access to this critical support is harmful to women’s health and gender empowerment because it can result in the mother’s death or long-term impairment, particularly in marginalized areas.
3. Macro-Level Factors Associated with Maternal Deaths: A Literature Survey
The literature has identified several structural (macro-level) factors that influence maternal mortality. These are discussed below.
3.1. GDP/Income
Maternal mortality explanations must take into account socioeconomic factors such as income [48,49]. Brenner [50] presented evidence that indicated that economic downturns and upswings have played a substantial effect on prenatal, newborn and maternal mortality. Indeed, the apparent lack of consistency in the decline in baby and maternal death rates since 1950 was most likely due to economic instability. Women in developing nations have significantly more pregnancies on average than women in industrialized countries, and their lifetime risk of pregnancy-related death is higher. This is 1 in 5400 in high-income countries, compared to 1 in 45 in low-income countries [51]. Lower-income increases not only the danger per pregnancy but also the number of births. Where mothers have more children, maternal death rates are greater. These factors enhance the risk disparities between high- and low-income countries. Other factors, such as nutrition, are influenced by income. Fertility and maternal mortality are strongly linked to economic progress [52]. In order to achieve optimal birth outcomes, maternal health and offspring development, adequate nutrition during pregnancy is critical [53,54].
The high frequency of maternal mortality in impoverished nations is a direct result of poor prenatal health and nutrition, as well as inadequate treatment throughout pregnancy and delivery [55]. Okwan’s [56] study confirmed the hypothesis of an inverse relationship between maternal health outcome proxy by maternal mortality ratio and economic growth proxy by Gross Domestic Product (GDP) per capita. Thus, increasing economic growth by investing in the health care systems to reduce pregnancy and childbirth complications will help reduce maternal mortality in the sub-region. However, Shiffman [57] found that the wealth indicators explained only a small proportion of the variance in maternal mortality ratios in developing countries. Other factors, such as women’s literacy rates and the proportion of deliveries attended by qualified birth attendants, were found to be considerably better predictors of maternal mortality than per capita income [57]. The marginal contribution of economic growth to reductions in maternal mortality has also been identified by other studies. For instance, Okwan’s [57] claimed that despite the region’s progressive economic growth during the global economic crisis, the sub-Saharan region has the highest maternal death rate.
3.2. Skilled Birth Attendants
Skilled delivery encompasses the presence of professionals (midwives, doctors, nurses and others) during delivery. It also comprises a supportive atmosphere with the necessary equipment, medications and other supplies for the effective and efficient management of obstetric problems [58]. Adegoke et al. [59] note that in the 1800s, the establishment of midwifery as a profession, and widespread access to skilled and competent midwives, were linked to a decrease in maternal mortality in Scandinavia to less than 300 per 100,000 births. An increase in the number of deliveries attended by a skilled birth attendant has also been linked to a reduction in maternal mortality in low- and middle-income nations [59,60,61]. Bell et al. [58] argue that several babies or mothers are lost due to critical issues such as the inability to recognize delivery complications and ensure quick referrals. According to the most recent data available, more than 90% of all births in most high- and higher-middle-income nations benefit from the presence of a qualified midwife, doctor or nurse [62].
Skilled birth attendants and emergency obstetric care are two of the most potent weapons in the battle against maternal mortality [63]. However, in several low- and lower-middle-income nations, such skilled health staff help fewer than half of all deliveries. Poverty-stricken women are the most likely to lack access to sufficient health care and experience maternal mortality [9]. Sub-Saharan Africa has a shortage of maternity care providers. SSA has the lowest health care worker density in the world, which limits the improvements in maternal health [64]. Nurses and midwives play a critical role in reducing mother and newborn mortality as well as delivering sexual and reproductive health care. Without their support, new mothers are vulnerable to infectious diseases and disorders such as pregnancy-induced haemorrhage, hypertension and uterine rupture, which are among the main causes of maternal death in sub-Saharan Africa.
3.3. Access to Health Care Facilities and Services
Another crucial factor in preventing maternal fatalities is access to health care facilities and services. Maswime and Chauke [65] and the United Nations [10] concur and state that maternal mortality is a measure of health care access and quality. All pregnant women should have access to antenatal care, professional birthing care and postpartum care and support [66]. In Ethiopia, where maternal mortality is the greatest threat to women of reproductive age, fewer than half of all women attend even one antenatal appointment [67]. For the health of women and their unborn children, prenatal care is critical. Women can learn about healthy behaviors throughout pregnancy from competent health staff, better understand warning signals during pregnancy and childbirth and receive social, emotional and psychological support during this vital period in their life through this type of preventative health care. Pregnant women can also get vitamin supplements, hypertension treatment to avoid eclampsia and tetanus vaccination through antenatal care [68].
Prenatal care can also include HIV testing and medication to prevent HIV transmission from mother to child. Women in distant parts of Africa, however, do not have access to health care due to distance, poverty and a lack of information [69]. Less formal education, lower health literacy, unplanned pregnancies and poor transportation have also been associated with late prenatal care [70]. Spousal violence reduces the likelihood of maternal health care visits for prenatal care in locations where health care facilities are already inadequate [71]. For these frequent and regular encounters to take place, ease of access is critical. When facilities are readily available, moms will spend less time, money and mental energy on each visit, and hence are less likely to skip prenatal appointments. Access to health facilities improves reproductive health. Reproductive health is improved by access to medical facilities. Certain risk factors and disorders (such as polycystic ovarian syndrome or oligo-menorrhea) that can impair a woman’s reproductive health can be identified when a woman has access to adequate medical services.
The quality of care in many nations is inadequate, and while the initial antenatal check-up is usually free, women must pay for future visits. Evidence from South Africa shows that poor quality of care is a contributing factor to maternal deaths. A report covering 2017 to 2019 found that 80% of women who died received substandard care at district hospitals [72]. Deaths occur in district hospitals in South Africa, where specialist, critical care or efficient emergency medical services may not be readily available [65].
3.4. Family Planning
Access to contraception is also critical to preventing maternal mortality, because without pregnancy there would be no maternal death [73,74]. Family planning is essential for gender equality and women’s empowerment, as well as poverty reduction. Reduced mother and infant mortality have come from the increased usage of contraceptive techniques [75,76,77,78,79]. There are still significant gaps in the usage of current treatments among couples who seek to avoid pregnancy. In sub-Saharan Africa, however, nearly half of all women of reproductive age (15 to 49 years) do not have access to contemporary contraceptive techniques, a figure that rises to nearly 60% among adolescent girls (aged 15 to 19 years) [80]. By limiting the number of births, family planning helps to reduce maternal mortality. Fewer pregnancies provide fewer chances for women to be exposed to the risk of maternity-related mortality, making contraception an important direct determinant of fertility reduction. Mbizvo and Burke [81] estimate that global family planning could prevent up to 30% of maternal deaths going forward. The Harvard Chan School [82] states that one proposed mechanism for this effect is that contraceptive use reduces the number of high-risk and high-parity births, thereby reducing maternal mortality. Access to contraceptives also helps to prevent unwanted pregnancies, some of which result in unsafe abortions—one of the causes of global maternal deaths.
3.5. Women’s Empowerment
Empowerment is widely recognized as a process through which persons who have been disempowered can improve their self-efficacy, make better decisions and gain control over resources [83]. Prata, Tavrowa and Upadhyay [84] are of the view that increased women’s empowerment will result in improved health, particularly in areas where disparities are greatest, such as maternal mortality. Evidence demonstrates that when girls exercise their rights to postpone marriage and childbirth in order to pursue their education, maternal mortality decreases [85,86]. These factors contribute to women’s empowerment by enhancing their ability to care for and choose for themselves, such as autonomy over their reproductive lives and health care decisions, access to health care services and options and the ability to influence service quality through participatory mechanisms and social accountability.
The ability and right of women to make active decisions has a favorable impact on the health of their children and families. Women who marry before they reach the legal age of marriage are less likely to seek expert medical care for their mothers [86]. As a result, they are more likely to give birth at home, which is linked to a higher prevalence of maternal death and morbidity [71]. Pandey, Lama and Lee [87] showed that three of the five indicators of empowerment—women’s age at birth of their first child, their education and their knowledge about sexually transmitted diseases—significantly increased utilization of health services, especially antenatal and delivery services. Adolescent girls (aged 10–19 years) face higher risks of eclampsia, systemic infections and complications during childbirth than women aged 20–24 years [88,89,90]. This shows that early childbirth can be harmful to newborn children’s health as well as the health of young mothers and pregnant adolescents.
3.6. Education
Nwogwugwu [91] states that the more educated and economically empowered women are, the more capable they are of making autonomous decisions, especially those that influence their personal health. Lack of knowledge is highlighted as one of a number of stressors impacting women during pregnancy and childbirth (together with a lack of money and decision-making authority), generating vulnerability and raising the likelihood of unfavorable outcomes [92]. Pilla et al. [48] argue that women who are literate are less likely to be poor, and more likely to maintain optimal nutritional status, make health and well-being decisions, access and use information, and have fewer children. Maternal mortality would be cut in half if all women received only a primary education, saving 189,000 women’s lives per year [93]. Women who are educated are more likely to marry later in life and to use family planning methods. Mothers with a primary education are more likely than those without one to take better care of their children and to seek medical care, such as immunization. The link between education, health and earning potential is clear [10].
Education must also extend to sexual and reproductive education. Pregnant women, as well as all reproductive women, including teenagers, should receive education about reproductive health [94]. Understanding reproductive health during pregnancy is crucial for the mother’s and the unborn child’s safety. Reproductive health is crucial for teenagers because it helps them avoid unintended pregnancies. Girls and women who receive education on sexual and reproductive health are more likely to use contraceptives effectively throughout their lives, have better knowledge of contraception, use it during their first sexual encounter and use it more frequently overall [95,96]. Generally, sex education increases one’s knowledge of contraception, increases the likelihood of using it at any time in one’s life and promotes effective and regular use. Sexual education has also been seen to prevent other issues such as unsafe abortions which are major causes of maternal mortality [97].
3.7. HIV and Other Factors
Women living with HIV/AIDS may be more vulnerable to maternal death due to direct or obstetric factors [98]. HIV infection has a strong negative influence on adult population health in countries with a high frequency of HIV infection, which therefore has an impact on maternal and child health [99,100]. In 2013, of the 7500 AIDS-related maternal deaths worldwide, 6800 (91%) were in sub-Saharan Africa. Sub-Saharan Africa accounts for 91 % of the maternal deaths attributed to HIV/AIDS [101]. There are also other factors that cause maternal mortality. Hanif et al. [71] are of the opinion that a number of contributing factors such as poverty, a lack of education, gender-based inequalities, inadequate and poor quality health care services, remote facilities, sociocultural values, malnutrition and violence against women, unequal resource distribution and the political environment, can all be considered key indicators for increased maternal deaths. Wagstaff, Van Doorslaer and Watanabe [102] show that the development of a good policy and the quality of institutions are important determinants of the impact of public-health expenditure. Disrespectful maternal care is an issue too. The abuse in South African maternity services was described as “one of the world’s greatest disgraces” in 2015. It included verbal and physical abuse, non-consensual care, non-confidential care, neglect and abandonment [65].
4. Materials and Methods
4.1. Data and Estimation Procedures
The study was quantitative in nature, and it used secondary statistical data. The data covering the period under investigation was collected from the World Bank and UNDP, respectively. The researcher used annual panel data for the period between 2005 and 2019. All SADC countries (Angola, Botswana, Comoros, Democratic Republic of Congo, Eswatini, Lesotho, Madagascar, Malawi, Mozambique, Namibia, Seychelles, South Africa, United Republic Tanzania, Zambia and Zimbabwe) were included in this study except for Mauritius. Mauritius was omitted to reduce panel attrition due to the large missing values for the data set. The study followed the model of Karlsen [103] whose study conducted an analysis of the relationship between maternal education and mortality among women giving birth in health care institutions. This study built on Karlsen [103] and formulated the following model:
where MM is maternal mortality, is the lagged value of the dependent variable (maternal mortality), F is fertility, EDU is education, GDPC is GDP per capita, INST is institutional quality, HE is health expenditure, HIV is human deficiency syndrome and is the error term. The description of the variable presented in the Equation (i) above is presented in Table 1 below.

Table 1.
Summary of Variable Description.
4.2. Estimation Techniques
This study employs Arellano and Bond’s [104] Generalized Method of Moments (GMM), which is one of the most extensively used approaches in empirical economic research. GMM estimators are also used in research related to human development, such as Asiama and Quartey [105], Akinbode and Bolarinwa [106] and Aksentijevic et al. [107]. As a result, we found GMM to be very relevant in this study. The construction of a GMM model requires an instrumental variable procedure to correct the endogeneity. While strictly exogenous instruments are in general hard to come by, it is possible to construct internal predetermined instruments using lagged values of the right-hand side variable [108]. This study used suitably lagged differences between the dependent and independent variables as instruments. The GMM estimator delivers unbiased and consistent parameter estimates in this way [107]. The Generalized Method of Moments (GMM) in the dynamic panel gives an efficient estimate of such a model (contrary to the OLS) while making it possible to control the individual and time-specific effects and to mitigate the endogeneity bias of variables [105]. The problem with endogeneity is that it can cause a serious bias when estimating how the independent variables in the equation affect the dependent variable in the model.
The system GMM performs by estimating two system equations. First, the original levels equation with a suitable lagged first difference is used as an instrument, and the first difference equation with a suitable lagged level is used as an instrument. Second, the application of system GMM reduces the finite sample bias and increases consistency in estimation [109]. This version is preferred to difference GMM because it mitigates small sample biases from the difference GMM and does not eliminate cross-country variations. Furthermore, instead of using the one-step system GMM, we employ an extension of the system GMM, which is a two-step system GMM developed by Roodman [110] because of its robustness to heteroscedasticity and autocorrelation problems in econometrics research. The generalized specification of the system GMM at a level and after first difference are as follows:
The difference form is:
5. Results and Discussion
5.1. Descriptive Statistics
The estimation process begins with the preliminary tests to check the normality of the series and to ensure that there is no multicollinearity among the explanatory variables. Table 2 shows the summary statistics of the variables used in this study.

Table 2.
Descriptive statistics.
Table 2 shows that the variables were not normally distributed. This is shown by the Jarque–Bera statistics which had p-values of less than 0.05. Table 2 also shows that there were 170 observations in this study. The correlation analysis of the main variables is displayed in Table 3.

Table 3.
Correlation.
Considering the range of the absolute values (0.003–0.614) in the table, it can be concluded that there is no multicollinearity problem among the explanatory variables. This is because the values are below the benchmark of 0.80.
5.2. Presentation of Main Results
This paper estimates the effects of ICT on maternal mortality in the SADC region. The empirical results for the model are presented in Table 4.

Table 4.
Regression results (Dependent variable: MM).
Although the analysis used the Generalized Method of Moments (Sys-GMM), the Fixed Effects (FE) and Random Effects (RE) were also performed. However, these were only performed to show the robustness of the GMM results. Their results are not reported in this study because RE and FE ignore unobservable heterogeneity and endogeneity.
Results (GMM 1) show that there is a negative relationship between education and maternal mortality. Health promotes learning potential, while education improves health. Together, education and health complement, enrich and support one another. Results show that there is a positive relationship between fertility and maternal mortality. High fertility levels are connected with high maternal mortality, making fertility a key driver of maternal mortality. The relationship between institutions and maternal mortality was seen to be insignificant. Countries with good institutions are supposed to have efficient health care systems. Institutions enable the adoption of right health policies and institutions and also ensure that resources are used efficiently. The relationship between health expenditure and maternal mortality was seen to be insignificant. This is surprising because health expenditure must contribute positively to maternal health care. The relationship between health expenditure and maternal mortality was seen to be insignificant. This is surprising because health expenditure must contribute positively to maternal health care. Results show that there is a positive relationship between HIV and maternal mortality. This is consistent with the literature. HIV and AIDS increase maternal mortality, as suppressed immunity causes a higher risk of pre-natal and childbirth complications. Results show that there is a positive relationship between GDP per capita and maternal mortality.
5.3. Discussion of Results
Findings (GMM 1) indicate a link between maternal mortality and education that is causally negative. Together, health and education enhance, support, and contribute to one another, building the foundation for a better future. [4]. Lack of education is highlighted as one of a number of stressors impacting women during pregnancy and childbirth (together with a lack of money and decision-making authority), generating vulnerability and raising the likelihood of unfavorable outcomes [103]. It is feasible that universal access to high-quality health services may alleviate much of the health disparities associated with low maternal education. Increasing women’s capacity to care for and choose for themselves leads to empowerment, which includes autonomy over their reproductive lives and health care decisions, as well as access to health care resources and options. The UN [111]) argues that women who are educated are more likely to be healthy, generate higher incomes and have greater decision-making power within their households. Providing opportunities for girls to complete their education, particularly secondary education, protects them against HIV and improves a variety of other health and development outcomes. Despite this, far too many students are still absent [80]. This could explain why African countries have such high maternal mortality rates.
Results show that there is a positive relationship between fertility and maternal mortality. High fertility levels are connected with high maternal mortality, making fertility a key driver of maternal mortality [112,113]. Girum and Wasie [61] maintain that the likelihood of complications increases with the number of pregnancies a woman has. Wei [114] conducted a study that showed that if all women had a maximum of one pregnancy each, the pregnancy mortality rate would decrease by 74%. Women in developing nations have significantly more pregnancies on average than women in industrialized countries, and their lifetime risk of pregnancy-related death is higher. Where mothers have more children, maternal death rates are greater. These factors enhance the risk disparities between high- and low-income countries. Stover and Ross [75] are of the view that by lowering the number of births and consequently the number of times a woman is exposed to the risk of mortality, family planning helps to reduce maternal mortality.
The relationship between institutions and maternal mortality was seen to be insignificant. Countries with good institutions are supposed to have efficient health care systems. Institutions enable the adoption of the right health policies and institutions also ensure that resources are used efficiently. Wagstaff and Cleason [115] discovered that good policies and institutions (as measured by the World Bank’s Country Policy and Institutional Assessment or CIPA index) are important determinants of the impact of government health expenditures on health outcomes. However, the institutions in many African states (SADC included) are poor. Mwanyika-Sando [116] did a study on care in Tanzanian public health facilities and found that the institutional performance was poor. The study showed that pregnant women reported feeling some form of abandonment during the actual time when they were so vulnerable and needed a health care provider to help them as they were about to deliver their child. It is for this reason that Alawode [117] advises that, as part of maternal health care quality improvement, stakeholders should clearly articulate the roles of different institutions and address institutional weaknesses that hinder the effective design and implementation of a quality improvement initiative.
The relationship between health expenditure and maternal mortality was seen to be insignificant. This is surprising because health expenditure must contribute positively to maternal health care. For instance, Baldacci, Guin-Siu and de Mello [118] and Gupta, Verhoeven and Tiongson [119] found that social spending plays a significant role in the health and education sectors. Maruthapu et al. [120] found that reduced government health care spending is linked to higher maternal death rates in the EU, which occurs through a range of processes, including fewer qualified health professionals attending births. They also discovered that policies targeted at cutting government health care spending, such as austerity and budget cuts, may increase maternal mortality in the EU. Bokhari, Gay and Gottret [121] also show that, while economic growth is one of the main determinants of health outcomes in developing countries, government spending on health is also an important factor in determining health outcomes.
However, the findings of this study are consistent with those of Rana et al. [122] who found that rising health expenditure can reduce child mortality but has an insignificant relationship with maternal mortality. Financial resources, on the other hand, are necessary but not sufficient for enhanced performance [123]. Other elements must be taken into account in order for financial resources to produce the best results. While it is widely acknowledged that skilled birth attendants and emergency obstetric care are critical in combating high maternal mortality, their provision requires functioning health systems that include trained and motivated workers, well-equipped facilities and rapid referral systems for complications. These are largely absent in many health systems of developing countries [63,124]. Fully functional health-care facilities are required that are: accessible and cheap, particularly for women in remote areas; staffed with competent and well-supported midwives and nurses; and equipped with water, sanitation, hygiene, medicines and supplies. In low- and middle-income countries, gaps in the availability and quality of maternal health care services are a key impediment to achieving desirable maternal health outcomes [117]. Wagstaff, Van Doorslaer and Watanabe [102] show that the development of a good policy and the quality of institutions are important determinants of the impact of public-health expenditure.
Results show that there is a positive relationship between HIV and maternal mortality. This is consistent with the literature. HIV and AIDS increase maternal mortality as suppressed immunity causes a higher risk of pre-natal and childbirth complications [125,126]. Madzimbamuto [127] claims that HIV infection is one of the most important conditions contributing to maternal deaths in the Southern Africa region. HIV-infected pregnant women have two to ten times the risk of dying during pregnancy and the postpartum period compared with uninfected pregnant women [99,128,129]. The main reason for the decline in maternal deaths in South Africa has been the success of the antiretroviral treatment programme for HIV-positive women [130].
Results show that there is a positive relationship between GDP per capita and maternal mortality. This result is not consistent with the literature. For instance, Thompson and Sofo [131] and Okwan’s [56] study demonstrated a significant negative relationship between maternal mortality and GDP per capita. Furthermore, women living in poverty are the least likely to receive adequate health care and experience maternal death [9]. Poverty increases the likelihood of seeking medical help before, during, or after pregnancy. Poverty remains one of the biggest factors in whether or not a woman receives adequate health care, and 94 percent of all maternal deaths still occur in low- and lower-middle-income countries [132]. Women from impoverished families have greater fertility rates, are more likely to have unsafe or conventional deliveries handled by inexperienced people and show less indication of following a family planning regimen. Strong data relating income and health implies that policies that promote economic justice may have far-reaching health implications [133]. Shiffman [57] found that the wealth indicators explained only a small proportion of the variance in maternal mortality ratios in developing countries. The study concluded that other variables such as women’s literacy rates and the proportion of deliveries attended by trained birth attendants were found to be far more effective predictors of maternal mortality than per capita income.
In order to test the robustness of the findings, the study replaced GDP per capita with GDP (economic growth). This was done in model 2 (GMM 2). The results for model 2 are in line with those obtained for the first model (GMM 1). However, the coefficient for the GDP variable is negative. These results indicate that GDP can contribute to the decrease in maternal mortality. This makes sense because an increase in income can improve the lives of the people. Studies have established that this relationship is largely causal—higher income leads to better health [56,133,134]. The latest available data suggest that in most high-income and upper-middle-income countries, more than 90% of all births benefit from the presence of a trained midwife, doctor or nurse [135]. However, fewer than half of all births in several low-income and lower-middle-income countries are assisted by such skilled health personnel.
5.4. Diagnostic Tests
The accuracy of the system GMM estimator is determined by the validity of the instruments. The diagnostic test for this is done using the Sargan Test (J-statistic) and the Arellano–Bond test. The results of the Sargan test are shown in Table 5 below.

Table 5.
Sargan Test.
The result of the test shows that the J-statistic of 1.7582 was not significant with a p-value of 0.8376, suggesting that the instruments are valid. The Arrellano–Bond test was also performed, and the results are shown in Table 6 below.

Table 6.
Arrellano–Bond serial correlation test.
The Arellano–Bond test for first-order (AR(1)) and for second-order (AR(2)) in the first differences was applied to the differenced residuals, being based on the no serial correlation null hypothesis. The tests show that the first-order statistic is statistically significant, whereas the second-order statistic is not, which is what should be expected if the model error terms are serial and uncorrelated in levels. It can thus be said that the model passed the diagnostic tests; therefore, inference can be made from the results.
6. Conclusions and Recommendations
This study sought to investigate the macro determinants of maternal mortality in SADC states. In poorer countries, maternal mortality remains a major public health concern. According to the World Health Organization (WHO), approximately 810 women die every day from pregnancy or childbirth-related problems around the world. This is despite the fact that various international programs to reduce maternal mortality have been implemented. Sub-Saharan Africa accounts for the bulk of maternal mortality, accounting for two-thirds of global maternal deaths in 2017. Using panel-data estimation, the study examined and investigated how various factors affect maternal mortality. The analysis included variables, namely: education, fertility, fertility, GDP per capita, institutional quality, health expenditure and HIV. The econometric analysis reveals a significant positive impact of fertility, GDP per capita and HIV on maternal mortality. The analysis also showed that education has a negative effect on maternal mortality.
Based on the results, this study emphasizes that government policy should prioritize improving access to family planning (to lower fertility), access to early prenatal care, and promoting women’s access to education in order to improve maternal health and thereby minimize maternal mortality. Integrating family planning services into maternal health care can be an effective way to reduce fertility. If women had better access to, and use of, family planning alternatives, they could have fewer children. Access to early prenatal care and initiation of ART through prenatal services could improve the availability of comprehensive pregnancy care and reduce maternal morbidity and mortality related to HIV in pregnancy. An education free of negative gender norms and higher educational attainment is also critical for women’s well-being. Women with greater education are more likely to recognize the value of prenatal care, sanitary childcare practices and appropriate nutrition for themselves and their newborns than women with less education. They are also more likely to know where to seek medical help and to be able to afford it. Increases in health spending are most effective when state policies and societal norms are changed in ways that empower the most disadvantaged individuals and allow them access to services.
Author Contributions
Conceptualization, C.M.; Formal analysis, C.M.; Methodology, C.M.; Project administration, C.M., B.N. and B.M.; Software, C.M., B.N. and B.M.; Writing—original draft, C.M.; Writing—review and editing, C.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience: Summary. 2018. Available online: https://apps.who.int/iris/bitstream/handle/10665/259947/WHO-RHR-18.02-eng.pdf (accessed on 18 May 2022).
- Santora, E. The Impact of the Safe Motherhood Initiative from 1987 to 2000. 2020. Available online: https://embryo.asu.edu/pages/impact-safe-motherhood-initiative-1987-2000 (accessed on 10 June 2022).
- Barnes, B. The 30th Anniversary of the Safe Motherhood Initiative. 2018. Available online: https://www.newsecuritybeat.org/2018/01/30th-anniversary-safe-motherhood-initiative/ (accessed on 16 June 2022).
- UN. Improving Maternal Health through Education: Safe Motherhood Is a Necessity. 2022. Available online: https://www.un.org/en/chronicle/article/improving-maternal-health-through-education-safemotherhood-necessity (accessed on 18 May 2022).
- UN. Making Pregnancy Safer in Least Developed Countries The Challenge of Delivering Available Services. 2022. Available online: https://www.un.org/en/chronicle/article/making-pregnancy-safer-least-developed-countries-challenge-delivering-available-services (accessed on 18 July 2022).
- Kokutse, F. Africa’s Maternal Deaths Need Urgent Action to Meet SDG Goals. Available online: https://www.globalissues.org/news/2023/01/03/32746 (accessed on 8 January 2023).
- Africa Health Organisation. Sub-Saharan Africa Tops Maternal Deaths Globally. 2017. Available online: https://aho.org/news/sub-saharan-africa-tops-maternal-deaths-globally/ (accessed on 18 May 2022).
- Musarandega, R.; Nyakura, M.; Machekano, R.; Pattinson, R.; Munjanja, S.P. Causes of maternal mortality in Sub-Saharan Africa: A systematic review of studies published from 2015 to 2020. J. Glob. Health 2021, 11. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, L. Why Maternal Mortality Is So High in Sub-Saharan Africa. 2021. Available online: https://www.globalcitizen.org/en/content/maternal-mortality-sub-saharan-africa-causes/ (accessed on 16 June 2022).
- United Nations. Improve Healthcare Access to End ‘Preventable Tragedy’ of Child Mortality. 2023. Available online: https://news.un.org/en/story/2023/01/1132187 (accessed on 10 January 2023).
- Zhou, H.; Zhang, L.; Ye, F.; Wang, J.; Huntington, D.; Huang, Y. The Effect of Maternal Death on the Health of the Husband and Children in a Rural Area of China: A Prospective Cohort Study. PLoS ONE 2016, 11, e0157122. [Google Scholar] [CrossRef] [PubMed]
- WHO. World Health Statistics. 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/324835/9789241565707-eng.pdf (accessed on 20 July 2022).
- Asiimwe, G. Maternal Mortality in Sub-Saharan Africa Still a Major Challenge: Uganda’s Perspective. 2020. Available online: http://makir.mak.ac.ug/handle/10570/8175 (accessed on 11 October 2022).
- Rivera, O. Texas Lawmakers Push Bills to Address Maternal Mortality in 2023. 2023. Available online: https://www.keranews.org/health-wellness/2023-01-09/maternal-mortality-texas-legislature-2023 (accessed on 19 January 2023).
- World Economic Forum. Women’s health: Is This the World’s Best—And Most Under-Financed—Investment? 2023. Available online: https://www.weforum.org/agenda/2023/01/is-this-the-world-s-best-and-most-under-financed-investment-davos23/ (accessed on 19 January 2023).
- Moucheraud, C.; Worku, A.; Molla, M.; E Finlay, J.; Leaning, J.; Yamin, A.E. Consequences of maternal mortality on infant and child survival: A 25-year longitudinal analysis in Butajira Ethiopia (1987–2011). Reprod. Health 2015, 12, S4. [Google Scholar] [CrossRef] [PubMed]
- Bazile, J.; Rigodon, J.; Berman, L.; Boulanger, V.M.; Maistrellis, E.; Kausiwa, P.; Yamin, A.E. Intergenerational impacts of maternal mortality: Qualitative findings from rural Malawi. Reprod. Health 2015, 12 (Suppl. S1), S1. [Google Scholar] [CrossRef]
- Knight, L.; Yamin, A. “Without a mother”: Caregivers and community members’ views about the impacts of maternal mortality on families in KwaZulu-Natal, South Africa. Reprod. Health 2015, 12 (Suppl. S1), S5. [Google Scholar] [CrossRef]
- UNFPA. Maternal Health in Africa. 2014. Available online: https://www.unfpa.org/sites/default/files/resourcepdf/EN_Maternal%20Health%20in%20Africa_factsheet_web.pdf (accessed on 16 June 2022).
- IMF. Booms, Busts, and Echoes. 2006. Available online: https://www.imf.org/external/pubs/ft/fandd/2006/09/bloom.htm (accessed on 13 June 2022).
- WHO. Maternal Mortality. 2013. Available online: https://www.who.int/pmnch/topics/part_publications/201303_Econ_benefits_econometric_study.pdf (accessed on 15 July 2022).
- Obo-Nai, P. It’s Time for Africa’s Maternal Mortality Battle To Go Digital. 2020. Available online: https://www.theafricareport.com/43509/its-time-for-africas-maternal-mortality-battle-to-go-digital/ (accessed on 23 August 2022).
- Stenberg, K.; Axelson, H.; Sheehan, P.; Anderson, I.; Gülmezoglu, A.M.; Temmerman, M.; Mason, E.M.; Friedman, H.S.; Bhutta, Z.; Lawn, J.E.; et al. Advancing social and economic development by investing in women’s and children’s health: A new Global Investment Framework. Lancet 2014, 383, 1333–1354. [Google Scholar] [CrossRef] [PubMed]
- Ostrowski, C. The Impact of Maternal Mortality and Morbidity on Economic Development. 2010. Available online: https://www.wilsoncenter.org/event/the-impact-maternal-mortality-and-morbidity-economicdevelopment (accessed on 15 July 2022).
- Tulloch, T. The Economic and Social Impacts of Maternal Death. 2015. Available online: https://blogs.biomedcentral.com/on-health/2015/05/06/economic-social-impacts-maternal-death/ (accessed on 3 June 2022).
- Nallala, S.; Ghosh, U.; Desaraju, S.S.; Kadam, S.; Kadarpeta, R.R.; Van Belle, S. Why are they “unreached”? Macro and Meso determinants of health care access in hard to reach areas of Odisha, India. Int. J. Equity Health 2023, 22, 1–12. [Google Scholar] [CrossRef]
- World Bank. Maternal Mortality. at a Glance. Washington, DC. © World Bank. 2006. Available online: https://openknowledge.worldbank.org/handle/10986/9617License:CCBY3.0IGO (accessed on 15 July 2022).
- Filippi, V.; Chou, D.; Ronsmans, C.; Graham, W.; Say, L. Levels and Causes of Maternal Mortality and Morbidity. Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, 3rd ed.; World Bank: Washington, DC, USA, 2016; Volume 2. [Google Scholar]
- Médecins Sans Frontières. Unsafe Abortion: A Forgotten Emergency. 2019. Available online: https://www.msf.org/unsafeabortion-forgotten-emergency-womens-health (accessed on 2 July 2022).
- United Nations High Commissioner for Human Rights. Maternal Mortality and Morbidity. 2020. Available online: https://www.ohchr.org/sites/default/files/INFO_MMM_WEB.pdf (accessed on 15 July 2022).
- Owusu, P.A.; Sarkodie, S.A.; Pedersen, P.A. Relationship between mortality and health care expenditure: Sustainable assessment of health care system. PLoS ONE 2021, 16, e0247413. [Google Scholar] [CrossRef] [PubMed]
- World Bank. Maternal Mortality. 2006. Available online: http://web.worldbank.org/archive/website01213/WEB/0__CO53.HTM (accessed on 12 May 2022).
- Tsawe, M. Factors Influencing the Use of Maternal Healthcare Services. 2015. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4391603/ (accessed on 2 July 2022).
- Radkar, A. Correlates of Maternal Mortality: A Macro-level Analysis. J. Health Manag. 2018, 20, 337–344. [Google Scholar] [CrossRef]
- Adu, J. The Effects of Individual and Community-Level Factors. 2018. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6264832/ (accessed on 13 June 2022).
- Nakweya, G. Sub-Saharan Africa Tops Maternal Deaths Globally. 2019. Available online: https://www.scidev.net/subsaharan-africa/news/sub-saharan-africa-tops-maternal-deaths-globally/ (accessed on 27 August 2022).
- Ameyaw, K.E.; Dickson, K.S.; Adde, K.S.; Ezezika, O. Do women empowerment indicators predict receipt of quality antenatal care in Cameroon? Evidence from a nationwide survey. BMC Women’s Health 2021, 21, 1–9. [Google Scholar] [CrossRef]
- Konje, E.T.; Magoma, M.T.N.; Hatfield, J.; Kuhn, S.; Sauve, R.S.; Dewey, D.M. Missed opportunities in antenatal care for improving the health of pregnant women and newborns in Geita district, Northwest Tanzania. BMC Pregnancy Childbirth 2018, 18, 394. [Google Scholar] [CrossRef]
- Nasloon Ali Iffat, E.; Souha, A.; Fatima, A.; Tom, L.; Luai, A.A. Antenatal Care Initiation Among Pregnant Women in the United Arab Emirates: The Mutaba’ah Study. Front. Public Health 2020, 8, 211. [Google Scholar] [CrossRef]
- Tessema, Z.T.; Teshale, A.B.; Tesema, G.A.; Tamirat, K.S. Determinants of completing recommended antenatal care utilization in sub-Saharan from 2006 to 2018: Evidence from 36 countries using Demographic and Health Surveys. BMC Pregnancy Childbirth 2021, 21, 192. [Google Scholar] [CrossRef]
- Finlayson, K.; Downe, S. Why Do Women Not Use Antenatal Services in Low- and Middle Income Countries? A Meta-Synthesis of Qualitative Studies. PLoS Med. 2013, 10, e1001373. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Maternal Health. 2018. Available online: https://www.who.int/westernpacific/health-topics/maternal-health (accessed on 12 May 2022).
- Mchenga, M.; Burger, R.; von Fintel, D. Examining the impact of WHO’s Focused Antenatal Care policy on early access, underutilisation and quality of antenatal care services in Malawi: A retrospective study. BMC Health Serv. Res. 2019, 19, 295. [Google Scholar] [CrossRef] [PubMed]
- WHO Regional Officer for Africa. Maternal Health. 2022. Available online: https://www.afro.who.int/healthtopics/maternal-health (accessed on 27 August 2022).
- UNICEF. Delivery Care. 2021. Available online: https://data.unicef.org/topic/maternal-health/deliverycare/#:~:text=Globally%2C%20in%202020%2C%20approximately%2070,of%20births%20among20urban%20mothers (accessed on 2 April 2022).
- Damian, D.J.; Tibelerwa, J.Y.; John, B.; Philemon, R.; Mahande, M.J.; Msuya, S.E. Factors influencing utilization of skilled birth attendant during childbirth in the Southern highlands, Tanzania: A multilevel analysis. BMC Pregnancy Childbirth 2020, 20, 420. [Google Scholar] [CrossRef]
- Pillai, V.K.; Maleku, A.; Wei, F. Maternal Mortality and Female Literacy Rates in Developing Countries during 1970–2000: A Latent Growth Curve Analysis. Int. J. Popul. Res. 2013, 2013, 1–11. [Google Scholar] [CrossRef]
- Hamal, M.; Dieleman, M.; De Brouwere, V.; Buning, T. Social Determinants of Maternal Health: A Scoping Review of Factors Influencing Maternal Mortality and Maternal Health Service Use in India. 2020. Available online: https://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-020-00125-6 (accessed on 13 May 2022).
- Brenner, M.H. Fetal, Infant, and Maternal Mortality during Periods of Economic Instability. Instability. Int. J. Health Serv. 1973, 3, 145–159. [Google Scholar] [CrossRef]
- UNICEF. Maternal Mortality. 2019. Available online: https://data.unicef.org/topic/maternal-health/maternalmortality/#:~:text=The%20lifetime%20risk%20of%20maternal,100%2C%20to%201%20in20190 (accessed on 13 May 2022).
- OECD. 2020. Available online: https://www.oecd-ilibrary.org/sites/12a2742fen/index.html?itemId=/content/component/12a2742f-en (accessed on 2 April 2022).
- USAID. Role of Nutrition in Preventing Child and Maternal Deaths. 2017. Available online: https://www.usaid.gov/sites/default/files/documents/1864/role-of-nutrition-preventing-childmaternal-deaths.pdf (accessed on 2 April 2022).
- McKerricher, L.; Petrucka, P. Maternal Nutritional Supplement Delivery in Developing Countries: A Scoping Review. 2019. Available online: https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-0190270-2 (accessed on 2 April 2022).
- Mora, J.; Nestel, P. Improving prenatal nutrition in developing countries: Strategies, prospects, and challenges. Am. J. Clin. Nutr. 2000, 71, 1353S–1363S. [Google Scholar] [CrossRef]
- Okwan, F. Maternal Health Outcome and Economic Growth in Sub-Saharan Africa: A Dynamic Panel Analysis. World Academy of Science, Engineering and Technology International Journal of Economics and Management Engineering. 2020. Available online: https://publications.waset.org/10011406/maternal-health-outcome-and-economic-growth-in-sub-saharan-africa-a-dynamic-panel-analysis (accessed on 2 April 2022).
- Shiffman, J. Can poor countries surmount high maternal mortality? Stud. Fam. Plan. 2000, 31, 274–289. [Google Scholar] [CrossRef]
- Bell, J.; Curtis, S.L.; Alayon, S. Trends in Delivery Care in Six Counries [Internet]. DHS Analytical Studies No. 7. 2003. Available online: http://dhsprogram.com/pubs/pdf/AS7/AS7.pdf (accessed on 3 May 2022).
- Adegoke, A.; Utz, B.; Msuya, S.E.; Broek, N.V.D. Skilled Birth Attendants: Who is Who? A Descriptive Study of Definitions and Roles from Nine Sub Saharan African Countries. PLOS ONE 2012, 7, e40220. [Google Scholar]
- Joseph, G.; da Silva, I.; Wehrmeister, F.C.; Barros, J.D.; Victora, C. Inequalities in the coverage of place of delivery and skilled birth attendance: Analyses of cross-sectional surveys in 80 low and middle-income countries. Reprod. Health 2016, 13, 1–13. Available online: https://reproductivehealth-journal.biomedcentral.com/articles/10.1186/s12978-016-0192-2 (accessed on 5 May 2022). [CrossRef] [PubMed]
- Girum, T.; Wasie, A. Correlates of maternal mortality in developing countries: An ecological study in 82 countries. Matern. Health Neonatol. Perinatol. 2017, 3, 1–6. [Google Scholar] [CrossRef]
- WHO. Maternal Mortality. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality (accessed on 2 April 2022).
- Kruk, M.E.; Galea, S.; Prescott, M.; Freedman, L.P. Health care financing and utilization of maternal health services in developing countries. Health Policy Plan. 2007, 22, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Rosser, J.I.; Aluri, K.Z.; Kempinsky, A.; Richardson, S.; Bendavid, E. The Effect of Healthcare Worker Density on Maternal Health Service Utilization in Sub-Saharan Africa. Am. J. Trop. Med. Hyg. 2022, 106, 939–944. [Google Scholar] [CrossRef]
- Maswime, S.; Chauke, L. Most Maternal Deaths Are Preventable: How to Improve Outcomes in South Africa. 2022. Available online: https://theconversation.com/most-maternal-deaths-are-preventable-how-to-improve-outcomes-in-south-africa-181282#:~:text=Maternal%20mortality%20is%20an%20indicator,to%20those%20who%20are%20not (accessed on 10 April 2022).
- Ighobor, K. Improving Maternal Health in Africa. 2014. Available online: https://www.un.org/africarenewal/magazine/december-2014/improving-maternal-healthafrica (accessed on 20 April 2022).
- UNFPA. Maternal Health. 2022. Available online: https://esaro.unfpa.org/en/topics/maternal-health (accessed on 14 August 2022).
- UNICEF. Antenatal Care. 2021. Available online: https://data.unicef.org/topic/maternal-health/antenatal-care/ (accessed on 20 August 2022).
- Dahab, R.; Sakellariou, D. Barriers to Accessing Maternal Care in Low Income Countries in Africa: A Systematic Review. 2020. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7344902/ (accessed on 23 May 2022).
- Centre for Medicare Services. Improving Access to Maternal Health Care in Rural Communities. 2022. Available online: https://www.cms.gov/About-CMS/Agency-Information/OMH/equity-initiatives/rural-health/09032019-Maternal-Health-Care-in-Rural-Communities.pdf (accessed on 20 May 2022).
- Hanif, M.; Khalid, S.; Rasul, A.; Mahmood, A. Maternal Mortality in Rural Areas of Pakistan: Challenges and Prospects. 2021. Available online: https://www.intechopen.com/chapters/76143 (accessed on 10 May 2022).
- South African National Department of Health. South African South African National Department of Health Maternal, Perinatal, and Neonatal Health Policy. 2021. Available online: https://www.knowledgehub.org.za/system/files/ (accessed on 2 April 2022).
- Barnes, S.B.; Parker, M. Celebrating the 30th Anniversary of the Safe Motherhood Initiative at the Wilson Center. 2017. Available online: https://www.wilsoncenter.org/event/celebrating-the-30thanniversary-the-safe-motherhood-initiative-the-wilson-center (accessed on 4 June 2022).
- Barnes, S.B.; Percival, V.; Sciubba, J.B. On the Horizon 2023|Maternal Health. 2023. Available online: https://www.wilsoncenter.org/article/horizon-2023-maternal-health (accessed on 11 January 2022).
- Stover, J.; Ross, J. How Increased Contraceptive Use has Reduced Maternal Mortality. Matern. Child Health J. 2010, 14, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Bhutta, Z.A.; Das, J.K.; Bahl, R.; Lawn, J.E.; Salam, R.A.; Paul, V.K.; Sankar, M.J.; Blencowe, H.; Rizvi, A.; Chou, V.B.; et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014, 384, 347–370. [Google Scholar] [CrossRef]
- Chola, L.; McGee, S.; Tugendhaft, A.; Buchmann, E.; Hofman, K. Scaling Up Family Planning to Reduce Maternal and Child Mortality: The Potential Costs and Benefits of Modern Contraceptive Use in South Africa. PLoS ONE 2015, 10, e0130077. [Google Scholar] [CrossRef]
- Rutstein, S.; Winter, R. Contraception Needed to Avoid High-Fertility-Risk Births, and Maternal and Child Deaths that Would be Averted. 2015. Available online: https://dhsprogram.com/pubs/pdf/AS50/AS50.pdf (accessed on 10 July 2022).
- Aryanty, R.I.; Romadlona, N.; Besral, B.; Panggabean, E.D.P.; Utomo, B.; Makalew, R.; Magnani, R.J. Contraceptive use and maternal mortality in Indonesia: A community-level ecological analysis. Reprod. Health 2021, 18, 1–9. [Google Scholar] [CrossRef]
- UNAIDS. Women, Adolescent Girls and the Hiv Response. 2020. Available online: https://www.unaids.org/sites/default/files/media_asset/2020_women-adolescent-girls-and-hiv_en.pdf (accessed on 10 July 2022).
- Mbizvo, M.T.; Burke, A. Family planning global conference series. BMC Reprod. Health. 2016, 13, 9. [Google Scholar]
- Harvard Chan School. Family Planning and Maternal Health. 2022. Available online: https://www.mhtf.org/topics/family-planning-maternal-health/ (accessed on 10 July 2022).
- Kabeer, N. Reflections on the measurement of women’s empowerment. In Discussing Women’s Empowerment—Theory and Practice; Novum Grafiska, AB: Stockholm, Sweden, 2001. [Google Scholar]
- Prata, N.; Tavrow, P.; Upadhyay, U. Women’s empowerment related to pregnancy and childbirth: Introduction to special issue. BMC Pregnancy Childbirth 2017, 17, 352. [Google Scholar] [CrossRef]
- Alemayehu, M.; Meskele, M. Health care decision making autonomy of women from rural districts of Southern Ethiopia: A community based cross-sectional study. Int. J. Women’s Health 2017, ume 9, 213–221. [Google Scholar] [CrossRef]
- Marphatia, A.A.; Ambale, G.S.; Reid, A.M. Women’s Marriage Age Matters for Public Health: A Review of the Broader Health and Social Implications in South Asia. Front. Public Health 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Pandey, S.; Lama, S.; Lee, H. Effect of women’s empowerment on their utilization of health services: A case of Nepal. Int. Soc. Work. 2011, 55, 554–573. [Google Scholar] [CrossRef]
- Ganchimeg, T.; Ota, E.; Morisaki, N.; Laopaiboon, M.; Lumbiganon, P.; Zhang, J.; Yamdamsuren, B.; Temmerman, M.; Say, L.; Tunçalp, Ö.; et al. WHO Multicountry Survey on Maternal Newborn Health Research Network. Pregnancy and childbirth outcomes among adolescent mothers: A World Health Organization multicountry study. BJOG Int. J. Obstet. Gynaecol. 2014, 121 (Suppl. S1), 40–48. [Google Scholar] [CrossRef] [PubMed]
- Cavazos-Rehg, P.A.; Krauss, M.J.; Spitznagel, E.L.; Bommarito, K.; Madden, T.; Olsen, M.A.; Subramaniam, H.; Peipert, J.F.; Bierut, L.J. Maternal age and risk of labor and delivery complications. Matern. Child Health J. 2015, 19, 1202–1211. [Google Scholar] [CrossRef] [PubMed]
- Kiani, M.A.; Ghazanfarpour, M.; Saeidi, M. Adolescent Pregnancy: A Health Challenge. Int. J. Pediatr. 2019, 7, 9749–9752. [Google Scholar] [CrossRef]
- Nwogwugwu, N. Women’s Empowerment and Women’s Health in Africa. In The Palgrave Handbook of African Women’s Studies; Yacob Haliso, O., Falola, T., Eds.; Palgrave Macmillan: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Filippi, V.; Ronsmans, C.; Campbell, O.R.; Graham, W.J.; Mills, A.; Borghi, J.; Koblinsky, M.; Osrin, D. Maternal health in poor countries: The broader context and a call for action. Lancet 2006, 368, 1535–1541. [Google Scholar] [CrossRef]
- UNESCO. New UNESCO Data Proves Education Transforms Development. 2014. Available online: https://en.unesco.org/gem-report/sites/default/files/PR_Ed_transforms_En.pdf (accessed on 19 April 2022).
- Machdum, S.V.; Cholid, S.; Imelda, J.D. Home-based Reproduction Health Promotion for Minimizing Adolescent Maternal Mortality in Indonesia. KnE Soc. Sci. 2018, 3, 580–600. [Google Scholar] [CrossRef]
- Warner, C.; Carlson, S.; Crichlow, R.; Ross, M.W. Sexual Health Knowledge of U.S. Medical Students: A National Survey. J. Sex Med. 2018, 15, 1093–1102. [Google Scholar] [CrossRef]
- Seidu, A.-A.; Ameyaw, E.K.; Ahinkorah, B.O.; Baatiema, L.; Dery, S.; Ankomah, A.; Ganle, J.K. Sexual and reproductive health education and its association with ever use of contraception: A cross-sectional study among women in urban slums, Accra. Reprod Health. Reprod. Health 2022, 19, 7. [Google Scholar] [CrossRef] [PubMed]
- Olukoya, P. Reducing Maternal Mortality from Unsafe Abortion among Adolescents in Africa. Afr. J. Reprod. Health/Rev. Afr. St. Reprod. 2004, 8, 57–62. [Google Scholar] [CrossRef]
- McIntyre, J. Maternal Health and HIV. Matters 2005, 13, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Moran, N.; Moodley, J. The effect of HIV infection on maternal health and mortality. Int. J. Gynecol. Obstetrics 2012, 19, S26–S29. [Google Scholar] [CrossRef] [PubMed]
- Calvert, C.; Ronsmans, C. The contribution of HIV to pregnancy-related mortality. Aids 2013, 27, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Bailey, P.E.; Keyes, E.; Moran, A.C.; Singh, K.; Chavane, L.; Chilundo, B. The triple threat of pregnancy, HIV infection and malaria: Reported causes of maternal mortality in two nationwide health facility assessments in Mozambique, 2007 and 2012. BMC Pregnancy Childbirth 2015, 15, 293. [Google Scholar] [CrossRef]
- Wagstaff, A.; van Doorslaer, E.; Watanabe, N. On decomposing the causes of health sector inequalities, with an application to malnutrition inequalities in Vietnam. J. Econom. 2003, 112, 207–223. [Google Scholar] [CrossRef]
- Karlsen, S.; Say, L.; Souza, J.-P.; Hogue, C.J.; Calles, D.L.; Gülmezoglu, A.M.; Raine, R. The relationship between maternal education and mortality among women giving birth in health care institutions: Analysis of the cross sectional WHO Global Survey on Maternal and Perinatal Health. BMC Public Health 2011, 11, 606. [Google Scholar] [CrossRef]
- Arellano, M.; Bond, S.R. Some tests of specification for panel data: Monte Carlo evidence and an application to employment equations. Rev. Econ. Stud. 1991, 58, 277–297. [Google Scholar] [CrossRef]
- Asiama, J.P.; Quartey, P. Foreign aid and the human development indicators in sub Saharan Africa. J. Dev. Soc. 2009, 25, 57–83. [Google Scholar] [CrossRef]
- Akinbode, S.; Bolarinwa, T. Effect of Foreign Aid on Human Development in Sub-Saharan Africa: A System GMM Approach. South-East. Eur. J. Econ. Assoc. Econ. Univ. South East. Eur. Black Sea Reg. 2020, 18, 19–38. [Google Scholar]
- Aksentijević, N.K.; Ježić, Z.; Zaninović, P.A. The Effects of Information and Communication Technology (ICT) Use on Human Development—A Macroeconomic Approach. Economies 2021, 9, 128. [Google Scholar] [CrossRef]
- Giuliano, P.; Marta Ruiz-Arranz, M. Remittances, Financial Development, and Growth. J. Dev. Econ. 2009, 90, 144–152. [Google Scholar] [CrossRef]
- Blundell, R.; Bond, S. Initial conditions and moment restrictions in dynamic panel data models. J. Econom. 1998, 87, 115. [Google Scholar] [CrossRef]
- Roodman, D. How to Do Xtabond2: An Introduction to Difference and System GMM in Stata. Stata J. 2009, 9, 86–136. [Google Scholar] [CrossRef]
- UN. Facts & Figures: Rural Women and the Millennium Development Goals. 2012. Available online: https://www.un.org/womenwatch/feature/ruralwomen/facts-figures.html (accessed on 2 April 2022).
- Jose, L.A.; Valentín, H.; Angel, G. Factors associated with maternal mortality in Sub-Saharan Africa: An ecological study. BMC Public Health 2009, 14, 462. [Google Scholar] [CrossRef]
- WHO. Organization WH: Statistical Information System. 2016. Available online: http://www.who.int/whosis/en/index.html (accessed on 12 June 2022).
- Wei, H. The Impact of Fertility Changes on Maternal Mortality. Ph.D. Thesis, London School of Hygiene & Tropical Medicine, London, UK, 2011. [Google Scholar] [CrossRef]
- Wagstaff, A.; Cleason, M. The Millennium Development Goals for Health: Rising to the Challenge; World Bank: Washington, DC, USA. Available online: https://openknowledge.worldbank.org/handle/10986/14954 (accessed on 14 May 2022).
- Mwanyika-Sando. Respectful and Dignified Care in Tanzania. 2014. Available online: https://www.wilsoncenter.org/sites/default/files/media/documents/event/Mary%20Mwanyika%20Sado_Respectful%20and%20Dignified%20Care%20in%20Tanzania.pdf (accessed on 14 May 2022).
- Alawode, G. Strengthening Health System Governance for Improved Quality of Maternal Health Care in Nigeria. 2022. Available online: https://www.hfgproject.org/strengthening-health-system-governance-improvedquality-maternal-health-care-nigeria/ (accessed on 5 May 2022).
- Baldacci, E.; Guin-Siu, M.T.; de Mello, L. More on the effectiveness of public spending on health care and education: A covariance structure model. J. Int. Dev. 2003, 15, 709–725. [Google Scholar] [CrossRef]
- Gupta, S.; Verhoeven, M.; Tiongson, E.R. The effectiveness of government spending on education and health care in developing and transition economies. Eur. J. Politi- Econ. 2002, 18, 717–737. [Google Scholar] [CrossRef]
- Maruthappu, M.; Ng, K.; Williams, C.; Atun, R.; Agrawal, P.; Zeltner, T. TheAssociation between government health care spending and maternal mortality in the European Union, 1981 to 2010: A Retrospective study; Obstetric Anesthesia Digest. BJOG Int. J. Obstet. Gynaecol. 2016, 36, 73–74. [Google Scholar]
- Bokhari, F.; Gai, Y.; Gottret, P. Government health expenditures and health outcomes. Health Econ. 2007, 16, 257–273. [Google Scholar] [CrossRef]
- Rana, R.H.; Alam, K.; Gow, J. Health expenditure, child and maternal mortality nexus: A comparative global analysis. BMC Int. Health Hum. Rights 2018, 18, 29. [Google Scholar] [CrossRef] [PubMed]
- Fosu, P.; Ankrah, M. The effect of government expenditure and free maternal health care policy (FMHC) on household consumption in Ghana. J. Econ. Dev. 2021, 23, 184–202. [Google Scholar] [CrossRef]
- Aziz, N.; He, J.; Sarker, T.; Sui, H. Exploring the Role of Health Expenditure and Maternal Mortality in South Asian Countries: An Approach towards Shaping Better Health Policy. Int. J. Environ. Res. Public Health 2021, 18, 11514. [Google Scholar] [CrossRef]
- United Nations Office for the Coordination of Humanitarian Affairs. Improving Maternal Healthcare in Kenya—Integration of HIV Services with Maternal Healthcare. 2010. Available online: https://reliefweb.int/report/kenya/improving-maternal-healthcare-kenya-integration-hiv-servicesmaternal-healthcare (accessed on 11 April 2022).
- Calverta, C.; Marstona, M.; Slaymakera, E.; Crampina, A.C.; Pricea, A.J.; Reniers, G. Direct maternal deaths attributable to HIV in the era of antiretroviral therapy: Evidence from three population-based HIV cohorts with verbal autopsy. Aids 2020, 34, 1397–1405. [Google Scholar] [CrossRef] [PubMed]
- Madzimbamuto, F.D.; Ray, S.; Mogobe, K.D. Integration of HIV care into maternal health services: A crucial change required in improving quality of obstetric care in countries with high HIV prevalence. BMC Int. Health Hum. Rights 2013, 13, 27. [Google Scholar] [CrossRef]
- Lathrop, E.; Jamieson, D.J.; Danel, I. HIV and maternal mortality. Int. J. Gynecol. Obstet. 2014, 127, 213–215. [Google Scholar] [CrossRef]
- Borenstein, D. Maternal Health and HIV: Global Priorities for Research and Action. 2014. Available online: https://www.wilsoncenter.org/event/maternal-health-and-hiv-global-priorities-for-research-and-action (accessed on 7 July 2022).
- Moodley, J.F.; Fawcus, R.P. Improvements in maternal mortality in South Africa. South Afr. Med. J. 2018, 108, s4–s8. [Google Scholar]
- Thompson, E.; Sofo, S. Economic Impact of Maternal Mortality in Africa: A Panel Data Approach. J. Stat. Econom. Methods. 2015, 4, 65–78. [Google Scholar]
- United Nations Population Division. Trends In Maternal Mortality: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. 2019. Available online: https://reliefweb.int/report/world/trends-maternal-mortality-2000-2017 (accessed on 17 July 2022).
- Khullar, D.; Chokshi, D. Health, Income, & Poverty: Where We Are & What Could Help. 2018. Available online: https://www.healthaffairs.org/do/10.1377/hpb20180817.901935/ (accessed on 15 July 2022).
- Public Health Scotland. 2021. Available online: http://www.healthscotland.scot/healthinequalities/fundamental-causes/incomeinequality/income#:~:text=How%20income%20affects%20health,of%20health%20inequalities%20wthin%20populations (accessed on 13 May 2022).
- The Health Foundation. Relationship between Income and Health. 2021. Available online: https://www.health.org.uk/evidence-hub/money-and-resources/income/relationship-betweenincome-and-health (accessed on 10 May 2022).
- WHO. Adolescent Pregnancy. 2020. Available online: https://www.who.int/news-room/factsheets/detail/adolescentpregnancy#:~:text=Adolescent%20mothers%20aged%2010%E2%80%9319,women%20age%2020%E2%80%9324%20years.&text=Additionally%2C%20some%203.9%20million%2unsafe,morbidity%20and%20lasting%20health%20problems (accessed on 10 August 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).