Psychiatric Partial Hospitalization Programs: Following World Health Organization Guidelines with a Special Focus on Women with Delusional Disorder
Abstract
1. Introduction: Delusional Disorder
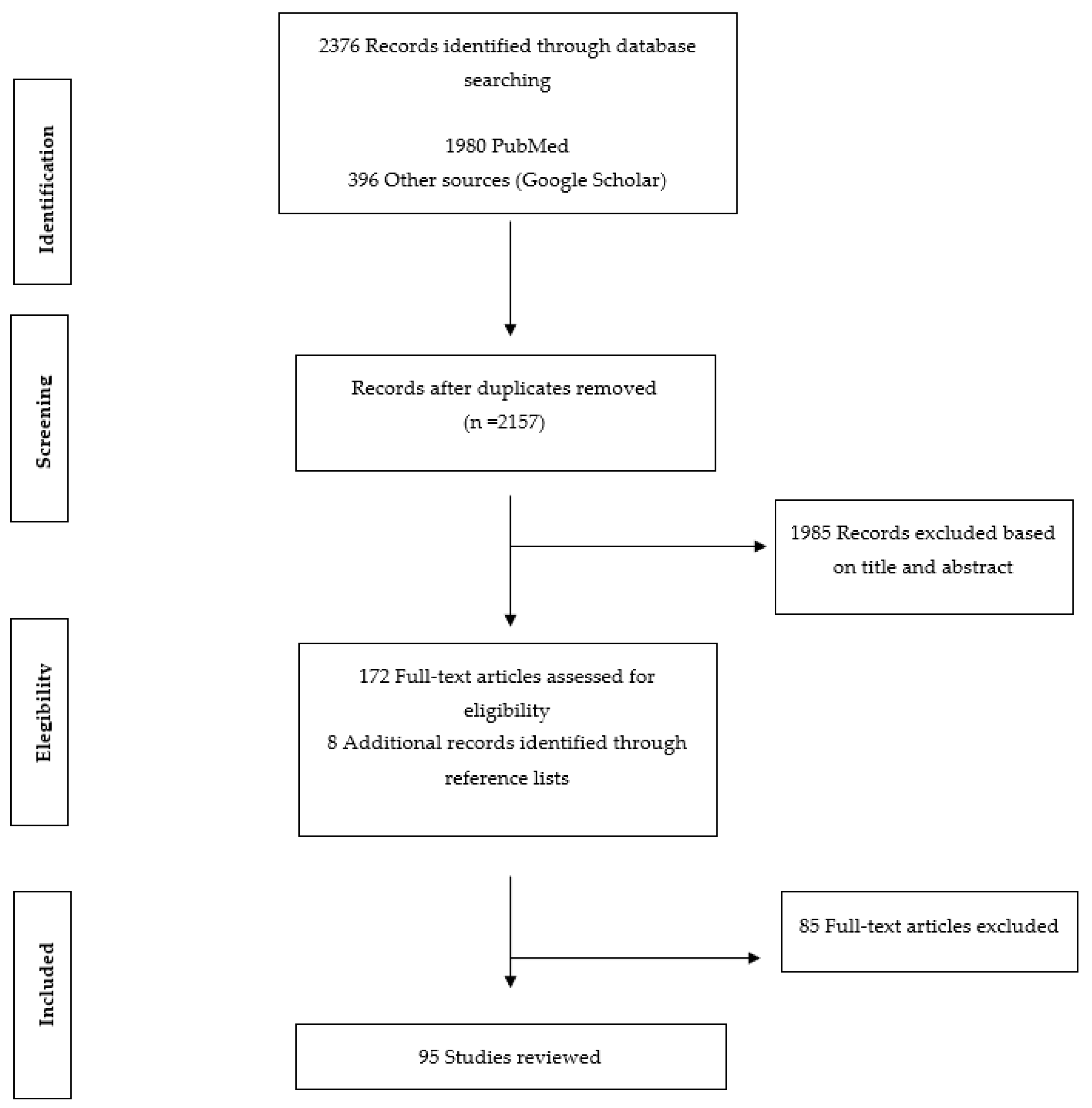
2. Methods
3. Community-Based Mental Health Models in the Treatment of Delusional Disorder
- (a)
- address the needs of a specific population, with accessibility viewed as a crucial element;
- (b)
- harness the goals and strengths of persons with mental illness through rehabilitation, leading to recovery;
- (c)
- promote a network of adequate support, services, and resources via multidisciplinary teamwork;
- (d)
- emphasize services that are evidence-based and recovery-oriented [18].
3.1. The Role of Community Treatment in Delusional Disorder
3.1.1. Primary Care in Delusional Disorder
3.1.2. Community Mental Health Centers and DD
- (1)
- Rapid identification of emergencies and crises, thus avoiding decompensation and hospital admission.
- (2)
- Availability of psychological therapy, such as cognitive–behavioral, systemic family, group, and occupational therapy, all of which improve insight and prevent relapse, readmission, and secondary symptoms such as anxiety.
- (3)
- Ready access and support to family members.
- (4)
- Rehabilitation and supportive work opportunities.
3.2. The Concept of Empowerment in DD
- (1)
- (2)
- Promote patients’ personal self-help and support processes through their social networks [36].
- (3)
- Support the development of practical problem-solving and decision-making with respect to treatment and other aspects of life [36].
- (4)
- Establish a non-paternalistic relationship framework that favors consensus [37].
- (5)
- Offer sufficient information to enable patients to make knowledgeable decisions [36].
4. Core Strategies of the Mental Health Action Plans Designed for Patients with Delusional Disorder
4.1. Theme 1: Promotion of Mental Health and Prevention in Delusional Disorder
4.1.1. Objective 1: Promotion of Mental Health and Prevention of Mental Disorders
4.1.2. Objective 2: Prevention of Suicidality and Substance Use
4.1.3. Objective 3: Anti-Stigma and Discrimination Actions
4.2. Theme 2: Improvement of Quality, Equity, and Continuity of Care
Objective 4: Improving Quality, Equity, and Continuity of Care (Including Physical Health) in DD
4.3. Theme 3: Coordination and Cooperation across Different Levels of Care (Measuring Health and Social Outcomes)
4.4. Theme 4: Specific Training for Mental Health Professionals
5. Partial Hospitalization Programs for Women with Delusional Disorder: Targets and Actions
5.1. Health Promotion in Women with DD
5.2. Prevention of Suicide, Substance Use Disorders, and Other Risk Factors in Women with Delusional Disorder
5.3. Coordination and Cooperation
5.4. Training
5.5. Research
6. Discussion and Conclusions: Planning the Future
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- González-Rodríguez, A.; Esteve, M.; Álvarez, A.; Guardia, A.; Monreal, J.A.; Palao, D.; Labad, J. What We Know and Still Need to Know about Gender Aspects of Delusional Disorder: A Narrative Review of Recent Work. J. Psychiatry Brain Sci. 2019, 4, 190009. [Google Scholar] [CrossRef]
- Serrano, B.G.; Bailón, L.A.; Calvo, P.; Negro, J.M.; Ballesteros, J.C. Psychiatrists’ opinion on treatment adherence in Delusional Disorder. Eur. Psychiatry 2016, 33, S570. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Seeman, M.V. Addressing Delusions in Women and Men with Delusional Disorder: Key Points for Clinical Management. Int. J. Environ. Res. Public Health 2020, 17, 4583. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Publishing: Arlinghton, VA, USA; Washington, DC, USA, 2013. [Google Scholar]
- De Portugal, E.; Martínez, C.; González, N.; del Amo, V.; Haro, J.M.; Cervilla, J.A. Clinical and cognitive correlates of psychiatric comorbidity in delusional disorder outpatients. Aust. N. Z. J. Psychiatry 2011, 45, 416–425. [Google Scholar] [CrossRef]
- Crowe, R.R.; Roy, M.A. Delusional Disorders. In The Medical Basis of Psychiatry, 3rd ed.; Fatemi, S.H., Clayton, P.J., Eds.; Humana Press: Totowa, NJ, USA, 2008; pp. 125–131. [Google Scholar]
- Tamburello, A.C.; Bajgier, J.; Reeves, R. The prevalence of delusional disorder in prison. J. Am. Acad. Psychiatry Law 2015, 43, 82–86. [Google Scholar] [PubMed]
- Román Avezuela, N.; Esteve Díaz, N.; Domarco Manrique, L.; Domínguez Longás, A.; Miguélez Fernández, C.; de Portugal, E. Gender differences in delusional disorder. Rev. Asoc. Esp. Neuropsiq. 2015, 35, 37–51. [Google Scholar] [CrossRef][Green Version]
- Yuksel, D.; de Zambotti, M.; Sugarbaker, D.; Schulte, T.; Colrain, I.M.; Baker, F.C. Physiological responses to acute psychosocial stress in women with menopausal insomnia. Int. J. Psychophysiol. 2021, 164, 87–94. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, A.; Molina-Andreu, O.; Gurrutxaga, M.L.I.; Campos, R.C.; Arroyo, M.B. A descriptive retrospective study of the treatment and outpatient service use in a clinical group of delusional disorder patients. Rev. Psiquiatr. Salud Ment. 2014, 7, 64–71. [Google Scholar] [CrossRef]
- De Portugal, E.; González, N.; Vilaplana, M.; Haro, J.M.; Usall, J.; Cervilla, J.A. Gender differences in delusional disorder: Evidence from an outpatient sample. Psychiatry Res. 2010, 177, 235–239. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health Action Plan 2013–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Lindamer, L.A.; Buse, D.C.; Auslander, L.; Unützer, J.; Bartels, S.J.; Jeste, D.V. A Comparison of Gynecological Variables and Service Use Among Older Women with and Without Schizophrenia. Psychiatr. Serv. 2003, 54, 902–904. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Molina-Andreu, O.; Rubio, R.P.; Campos, R.C.; Arroyo, M.B.; Bernardo, M. Variables reproductivas y uso de consulta ginecológica en pacientes con trastorno delirante. Rev. Psiquiatr. Salud Ment. 2015, 8, 92–96. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Seeman, M.V.; Álvarez, A.; Guàrdia, A.; Sanz, N.; Fucho, G.F.; Palao, D.J.; Labad, J. Care for Women with Delusional Disorder: Towards a Specialized Approach. Women 2021, 1, 46–59. [Google Scholar] [CrossRef]
- Thornicroft, G.; Deb, T.; Henderson, C. Community mental health care worldwide: Current status and further developments. World Psychiatry 2016, 15, 276–286. [Google Scholar] [CrossRef]
- Thornicroft, G.; Tansella, M. The balanced care model for global mental health. Psychol. Med. 2012, 43, 849–863. [Google Scholar] [CrossRef]
- Thornicroft, G.; Szmukler, G.; Mueser, K.; Drake, R.E. Oxford Textbook of Community Mental Health; Oxford University Press: Oxford, UK, 2011; pp. 179–191. [Google Scholar]
- WHO. What is primary care mental health?: WHO and Wonca Working Party on Mental Health. Ment. Health Fam. Med. 2008, 5, 9–13. [Google Scholar]
- Attepe, S. Community based mental health services in the eye of community mental health professionals. J. Psychiatr. Nurs. 2018, 9, 186–194. [Google Scholar]
- Vijverberg, R.; Ferdinand, R.; Beekman, A.; van Meijel, B. The effect of youth assertive community treatment: A systematic PRISMA review. BMC Psychiatry 2017, 17, 1–18. [Google Scholar] [CrossRef]
- Kalayasiri, R.; Kraijak, K.; Mutirangura, A.; Maes, M. Paranoid schizophrenia and methamphetamine-induced paranoia are both characterized by a similar LINE-1 partial methylation profile, which is more pronounced in paranoid schizophrenia. Schizophr. Res. 2019, 208, 221–227. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, A.; Molina-Andreu, O.; Odriozola, V.N.; Ferrer, C.G.; Penadés, R.; Catalán, R. Delusional disorder: An overview of affective symptoms and antidepressant use. Eur. J. Psychiatry 2013, 27, 265–276. [Google Scholar] [CrossRef]
- Loebel, A.D.; Lieberman, J.A.; Alvir, J.M.; Mayerhoff, D.I.; Geisler, S.H.; Szymanski, S.R. Duration of psychosis and outcome in first-episode schizophrenia. Am. J. Psychiatry 1992, 149, 1183–1188. [Google Scholar] [CrossRef] [PubMed]
- McGlashan, T.H.; Johannessen, J.O. Early Detection and Intervention with Schizophrenia: Rationale. Schizophr. Bull. 1996, 22, 201–222. [Google Scholar] [CrossRef] [PubMed]
- Verdoux, H.; Maurice-Tison, S.; Gay, B.; Van Os, J.; Salamon, R.; Bourgeois, M.L. A survey of delusional ideation in primary-care patients. Psychol. Med. 1998, 1, 127–134. [Google Scholar] [CrossRef]
- Verhaak, P.F. Analysis of referrals of mental health problems by general practitioners. Br. J. Gen. Pr. 1993, 43, 203–208. [Google Scholar]
- Armijo, J.; Mendez, E.; Morales, R.; Schilling, S.; Castro, A.; Alvarado, R.; Rojas, G. Efficacy of Community Treatments for Schizophrenia and Other Psychotic Disorders: A Literature Review. Front. Psychiatry 2013, 4, 116. [Google Scholar] [CrossRef]
- Fitzsimons, S.; Fuller, R. Empowerment and its implications for clinical practice in mental health: A review. J. Ment. Health 2002, 11, 481–499. [Google Scholar] [CrossRef]
- López, M.; Laviana, M.; García-Cubillana, P. Los Hospitales Psiquiátricos en La(s) Reforma(s). Notas Para Orientar una Investigación Necesaria. In Dos Décadas Tras la Reforma Psiquiátrica; Pérez, F., Ed.; AEN: Madrid, Spain, 2006; pp. 237–723. [Google Scholar]
- FAISEM. Soportes Para la Ciudadanía; FAISEM: Sevilla, Spain, 2012. [Google Scholar]
- López, M. El empleo y la recuperación de personas con trastornos mentales graves. La experiencia de Andalucía. Norte Salud Mental 2010, 8, 11–23. [Google Scholar]
- WHO-EURO. User Empowerment in Mental Health—A Statement by the WHO Regional Office for Europe; WHO: Copenhagen, Denmark, 2010. [Google Scholar]
- Deegan, P.E. Recovery and Empowerment for People with Psychiatric Disabilities. Soc. Work. Health Care 1997, 25, 11–24. [Google Scholar] [CrossRef] [PubMed]
- López, M.; Laviana, M. Rehabilitación, apoyo social y atención comunitaria a personas con trastorno mental grave: Propuestas desde Andalucía. Rev. Asoc. Española Neuropsiquiatría 2007, 27, 187–223. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. World Health Report 2001—Mental Health: New Knowledge, New Hope; WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Drake, R.E.; Deegan, P.E.; Rapp, C. The promise of shared decision making in mental health. Psychiatr. Rehabil. J. 2010, 34, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Evans, A., Jr.; Okeke, B.; Ali, S.; Achara-Abrahams, I.; Ohara, T.; Stevenson, T.; Warner, N.; Bolton, C.; Lim, S.; Faith, J.; et al. Converting partial hospitals to community integrated recovery centers. Community Ment. Health J. 2012, 48, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Rickerby, M.L.; Der Marderosian, D.; Nassau, J.; Houck, C. Family-Based Integrated Care (FBIC) in a Partial Hospital Program for Complex Pediatric Illness: Fostering Shifts in Family Illness Beliefs and Relationships. Child Adolesc. Psychiatr. Clin. N. Am. 2017, 26, 733–759. [Google Scholar] [CrossRef] [PubMed]
- Roesler, T.A.; Nassau, J.H.; Rickerby, M.L.; Laptook, R.S.; Der Marderosian, D.; High, P.C. Integrated, Family-based, Partial Hospital Treatment for Complex Pediatric Illness. Fam. Process. 2018, 58, 68–78. [Google Scholar] [CrossRef]
- Weber, C.A.T.; Juruena, M.F. Day hospital and psychosocial care center: Expanding the discussion of partial hospitalization in mental health. Rev. Assoc. Médica Bras. 2016, 62, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, P.J. Common mental disorders and work. Br. Med. Bull. 2018, 126, 113–121. [Google Scholar] [CrossRef]
- Pillmann, F.; Wustmann, T.; Marneros, A. Clinical course and personality in reactive, compared with nonreactive, delusional disorder. Can. J. Psychiatry 2012, 57, 216–222. [Google Scholar] [CrossRef]
- Molina-Andreu, O.; González-Rodríguez, A.; Villanueva, A.P.; Penadés, R.; Catalán, R.; Bernardo, M. Awareness of illness and suicidal behavior in delusional disorder patients. Arch. Clin. Psychiatry 2014, 41, 156–158. [Google Scholar] [CrossRef][Green Version]
- Weise, J.; Schomerus, G.; Speerforck, S. Die SARS-CoV-2-Pandemie und ein Suizidversuch bei wahnhafter Störung. Psychiatr. Prax. 2020, 47, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Kawohl, W.; Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry 2020, 7, 389–390. [Google Scholar] [CrossRef]
- Ornell, F.; Moura, H.F.; Scherer, J.N.; Pechansky, F.; Kessler, F.H.P.; von Diemen, L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res. 2020, 289, 113096. [Google Scholar] [CrossRef]
- Mazza, D.; Chakraborty, S.P.; Brijnath, B.; Nowak, H.; Howell, C.; Brott, T.; Atchison, M.; Gras, D.; Kenardy, J.; Buchanan, R.; et al. Diagnosing and managing work-related mental health conditions in general practice: New Australian clinical practice guidelines. Med. J. Aust. 2019, 211, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Álvarez, A.; Guàrdia, A.; González-Rodríguez, A.; Betriu, M.; Parra, I.; Monreal, J.A.; Palao, D.J.; Labad, J. Suicidality in schizophrenia, delusional disorder, schizoaffective disorder and first-episode of psychosis: A systematic review. Eur. Psychiatry 2020, 63, S577–S578. [Google Scholar]
- Freeman, D.; Bold, E.; Chadwick, E.; Taylor, K.M.; Collett, N.; Diamond, R.; Černis, E.; Bird, J.C.; Isham, L.; Forkert, A.; et al. Suicidal ideation and behaviour in patients with persecutory delusions: Prevalence, symptom associations, and psychological correlates. Compr. Psychiatry 2019, 93, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Florentin, S.; Rosca, P.; Bdolah-Abram, T.; Neumark, Y. Community Rehabilitation and Hospitalizations Among People with Chronic Psychotic Disorder: Is There a Differential Association by Co-occurring Substance Use Disorder? Front. Psychiatry 2021, 12, 621259. [Google Scholar] [CrossRef] [PubMed]
- Christensen, R.C.; Ramos, E. The Social and Treatment Consequences of a Shared Delusional Disorder in a Homeless Family. Innov. Clin. Neurosci. 2011, 8, 42–44. [Google Scholar] [PubMed]
- Martin, I.D.S.; Giacon, B.C.C.; Vedana, K.G.G.; Zanetti, A.C.G.; Fendrich, L.; Galera, S.A.F. Where to seek help? Barriers to beginning treatment during the first-episode psychosis. Int. J. Nurs. Sci. 2018, 5, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Currie, H.; Abernethy, K.; Hamoda, H. Vision for menopause care in the UK. Post Reprod. Health 2021, 27, 10–18. [Google Scholar] [CrossRef]
- Kaiser, B.N.; Weaver, L.J. Culture-bound syndromes, idioms of distress, and cultural concepts of distress: New directions for an old concept in psychological anthropology. Transcult. Psychiatry 2019, 56, 589–598. [Google Scholar] [CrossRef]
- 5Marshall, M.; Sledge, W.; Wiersma, D.; Crowther, R.; Kluiter, H.; Bond, G.R.; Almaraz-Serrano, A.; Roberts, C.; Huxley, P.; Creed, F.; et al. Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care. Health Technol. Assess. 2001, 5, 1–75. [Google Scholar] [CrossRef]
- Deshmukh, P.; Kulkarni, G.; Ganocy, S.J. Adults with Severe Psychiatric Symptoms in a Community Partial Hospitalization Program: Characteristics and Predictors of Clinical Response. Community Ment. Health J. 2021, 57, 667–674. [Google Scholar] [CrossRef]
- Seeman, M.V. Sex differences in schizophrenia relevant to clinical care. Expert Rev. Neurother. 2021, 1–11. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Labad, J.; Seeman, M.V. Schizophrenia and cancer. Curr. Opin. Support. Palliat. Care 2020, 14, 232–238. [Google Scholar] [CrossRef]
- Lähteenvuo, M.; Batalla, A.; Luykx, J.J.; Mittendorfer-Rutz, E.; Tanskanen, A.; Tiihonen, J.; Taipale, H. Morbidity and mortality in schizophrenia with comorbid substance use disorders. Acta Psychiatr. Scand. 2021. [Google Scholar] [CrossRef]
- Siskind, D.J.; Wu, B.T.; Wong, T.T.; Firth, J.; Kisely, S. Pharmacological interventions for smoking cessation among people with schizophrenia spectrum disorders: A systematic review, meta-analysis, and network meta-analysis. Lancet Psychiatry 2020, 7, 762–774. [Google Scholar] [CrossRef]
- Cowman, S.; Farrelly, M.; Gilheany, P. An examination of the role and function of psychiatric nurses in clinical practice in Ireland. J. Adv. Nurs. 2001, 34, 745–753. [Google Scholar] [CrossRef]
- McCardle, J.; Parahoo, K.; McKenna, H. A national survey of community psychiatric nurses and their client care activities in Ireland. J. Psychiatr. Ment. Health Nurs. 2007, 14, 179–188. [Google Scholar] [CrossRef]
- Ozten, E.; Tufan, A.E.; Cerit, C.; Sayar, G.H.; Ulubil, I.Y. Delusional parasitosis with hyperthyroidism in an elderly woman: A case report. J. Med. Case Rep. 2013, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Sudhir, P.M. Advances in psychological interventions for lifestyle disorders: Overview of interventions in cardiovascular disorder and type 2 diabetes mellitus. Curr. Opin Psychiatry 2017, 30, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Rehman, A.; Waite, F.; Sheaves, B.; Biello, S.; Freeman, D.; Gumley, A. Clinician perceptions of sleep problems, and their treatment, in patients with non-affective psychosis. Psychosis 2016, 9, 129–139. [Google Scholar] [CrossRef]
- Khazaie, H.; Rezaie, L.; Tahmasian, M.; Schwebel, D.C. Insomnia treatment by olanzapine. Is sleep state misperception a psychotic disorder? Neuroscience 2010, 15, 110–112. [Google Scholar]
- Calati, R.; Ferrari, C.; Brittner, M.; Oasi, O.; Olié, E.; Carvalho, A.F.; Courtet, P. Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. J. Affect. Disord. 2019, 245, 653–667. [Google Scholar] [CrossRef]
- Segovia, A.P.; Jimenez, M.G.; Calahorro, C.C.D.A.; Ballesteros, J.C. Comorbidity between delusional disorder and sensory deficits. Results from the deliranda case register. Eur. Psychiatry 2016, 33, S144–S145. [Google Scholar] [CrossRef]
- Seeman, M.V. Understanding the Delusion of Theft. Psychiatr. Q. 2018, 89, 1–9. [Google Scholar] [CrossRef]
- Shoham, N.; Lewis, G.; McManus, S.; Cooper, C. Common mental illness in people with sensory impairment: Results from the 2014 adult psychiatric morbidity survey. BJPsych. Open 2019, 5, e94. [Google Scholar] [CrossRef]
- Naylor, P.D.; Labbé, E.E. Exploring the effects of group therapy for the visually impaired. Br. J. Vis. Impair. 2017, 35, 18–28. [Google Scholar] [CrossRef]
- Hayashi, H.; Akahane, T.; Suzuki, H.; Sasaki, T.; Kawakatsu, S.; Otani, K. Successful Treatment by Paroxetine of Delusional Disorder, Somatic Type, Accompanied by Severe Secondary Depression. Clin. Neuropharmacol. 2010, 33, 48–49. [Google Scholar] [CrossRef]
- Schneider, B. Substance Use Disorders and Risk for Completed Suicide. Arch. Suicide Res. 2009, 13, 303–316. [Google Scholar] [CrossRef]
- Kerrigan, A.J.; Kaough, J.E.; Wilson, B.L.; Boeringa, J.A.; Monga, T.N.; Wilson, J.V. Vocational Rehabilitation Outcomes of Veterans with Substance Use Disorders in a Partial Hospitalization Program. Psychiatr. Serv. 2000, 51, 1570–1572. [Google Scholar] [CrossRef] [PubMed]
- Harrison, L.A.; Kats, A.; Williams, M.E.; Aziz-Zadeh, L. The Importance of Sensory Processing in Mental Health: A Proposed Addition to the Research Domain Criteria (RDoC) and Suggestions for RDoC 2.0. Front. Psychol. 2019, 10, 103. [Google Scholar] [CrossRef] [PubMed]
- Mouchet-Mages, S.; Gourevitch, R.; Lôo, H. Folie à deux: Actualités d’un concept ancien, à propos de deux cas. Encephale 2008, 34, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Guidry, L.S.; Winstead, D.K.; Levine, M.; Eicke, F.J. Evaluation of day treatment center effectiveness. J. Clin. Psychiatry 1979, 40, 221–224. [Google Scholar]
- Hoge, M.A.; Davidson, L.; Hill, W.L.; Turner, V.E.; Ameli, R. The Promise of Partial Hospitalization: A Reassessment. Psychiatr. Serv. 1992, 43, 345–354. [Google Scholar] [CrossRef]
- Thornicroft, G.; Tansella, M. Components of a modern mental health service: A pragmatic balance of community and hospital care. Br. J. Psychiatry 2004, 185, 283–290. [Google Scholar] [CrossRef]
- Lamb, C.E. Alternatives to admission for children and adolescents: Providing intensive mental healthcare services at home and in communities: What works? Curr. Opin. Psychiatry 2009, 22, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Taube-Schiff, M.; Mehak, A.; Marangos, S.; Kalim, A.; Ungar, T. Advancing Care Within an Adult Mental Health Day Hospital: Program Re-Design and Evaluation. J. Behav. Health Serv. Res. 2017, 46, 15–28. [Google Scholar] [CrossRef]
- Taube-Schiff, M.; Ruhig, M.; Ba, A.M.; Van Dyk, M.D.; Cassin, S.E.; Ungar, T.; Koczerginski, D.; Sockalingam, S. Staff perspectives: What is the function of adult mental health day hospital programs? J. Psychiatr. Ment. Health Nurs. 2017, 24, 580–588. [Google Scholar] [CrossRef]
- Yanos, P.T.; Vreeland, B.; Minsky, S.; Fuller, R.B.; Roe, D. Partial hospitalization: Compatible with evidence-based and recovery-oriented treatment? J. Psychosoc. Nurs. Ment. Health Serv. 2009, 47, 41–47. [Google Scholar] [CrossRef]
- Davidson, L.; Tondora, J.; O’Connell, M.J.; Kirk, T., Jr.; Rockholz, P.; Evans, A.C. Creating a recovery-oriented system of behavioral health care: Moving from concept to reality. Psychiatr. Rehabil. J. 2007, 31, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Nuechterlein, K.H.; Subotnik, K.L.; Turner, L.R.; Ventura, J.; Becker, D.R.; Drake, R.E. Individual placement and support for individuals with recent-onset schizophrenia: Integrating supported education and supported employment. Psychiatr. Rehabil. J. 2008, 31, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Humensky, J.L.; Turner, L.R.; Dixon, L.B.; Drake, R.E.; Becker, D.R.; Subotnik, K.L.; Ventura, J.; Nuechterlein, K.H. Personnel time required for supported employment and education services for individuals in a recent-onset psychosis treatment program. Early Interv. Psychiatry 2021, 15, 402–405. [Google Scholar] [CrossRef]
- Tizón, J.L.; Morales, N.; Artigue, J.; Quijada, Y.; Pérez, C.; Pareja, F.; Salamero, M. Delusional disorders: Prevalence in two socially differentiated neighborhoods of Barcelona. Psychosis 2013, 6, 107–116. [Google Scholar] [CrossRef]
- . Guàrdia, A.; González-Rodríguez, A.; Álvarez, A.; Betriu, M.; Seeman, M.V.; Monreal, J.A.; Palao, D.; Labad, J. Therapeutic drug monitoring is useful when pharmacogenetic assessment is unavailable: Case report of delusional disorder. Psicosom. Psiquiatr. 2020, 14, 28–32. [Google Scholar]
- Manschreck, T.C.; Khan, N.L. Recent Advances in the Treatment of Delusional Disorder. Can. J. Psychiatry 2006, 51, 114–119. [Google Scholar] [CrossRef]
- Haugom, E.W.; Stensrud, B.; Beston, G.; Ruud, T.; Landheim, A.S. Mental health professionals’ experiences with shared decision-making for patients with psychotic disorders: A qualitative study. BMC Health Serv. Res. 2020, 20, 1093. [Google Scholar] [CrossRef]
- Légaré, F.; Stacey, D.; Turcotte, S.; Cossi, M.-J.; Kryworuchko, J.; Graham, I.D.; Lyddiatt, A.; Politi, M.C.; Thomson, R.; Elwyn, G.; et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst. Rev. 2014, 5, CD006732. [Google Scholar] [CrossRef] [PubMed]
- Paino, M.; Ordóñez-Camblor, N.; Fonseca-Pedrero, E.; García-Álvarez, L.; Pizarro-Ruiz, J.P. Development and Validation of an Instrument for the Detection of Early Traumatic Experiences (ExpTra-S) in Patients with Psychosis. Front. Psychol. 2020, 11, 528213. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Negro, J.E.; Gómez-Sierra, F.J.; Peralta, V.; González-Rodríguez, A.; Cervilla, J.A. A systematic review of studies with clinician-rated scales on the pharmacological treatment of delusional disorder. Int. Clin. Psychopharmacol. 2020, 35, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Beard, C.; Hearon, B.A.; Lee, J.; Kopeski, L.M.; Busch, A.B.; Björgvinsson, T. When Partial Hospitalization Fails: Risk Factors for Inpatient Hospitalization. J. Nerv. Ment. Dis. 2016, 204, 431–436. [Google Scholar] [CrossRef]
| Functions of the CMHC |
|---|
| Providing biological and psychosocial interventions for individuals with severe mental health problems |
| Cooperating closely with primary health care and hospital units |
| Providing psychoeducation and focused support to families |
| Coordinating with other institutions and community service organizations |
| Sustaining social functioning and increasing the time individuals spend in the community |
| Contributing to the reduction of mental illness stigma |
| Theme 1 |
| Promotion of mental health |
| Prevention of mental health |
| Theme 2 |
| Improvement of quality, equity, and continuity of care |
| Theme 3 |
| Integration of health and social models of care |
| Theme 4 |
| Appropriate training for health workers |
| Health Promotion and Prevention of Mental and Physical Ill-Health | |
|---|---|
| Nurses | |
| Individual assessment and therapy | Medication management Psychopathological monitoring Health promotion (cancer screening and adherence to psychiatric, medical, and gynecological appointments) Patient and family support |
| Group therapies | Lifestyle intervention: motivation, learning, empowerment strategies, and behavioral skills Psychoeducation Sleep hygiene |
| Psychologists | |
| Individual assessment and therapy | Psychopathological assessment and behavioral monitoring Identification of psychotic exacerbation and emotional responses to delusional ideas Encouraging adherence Cognitive–behavioral therapy for insomnia, smoking cessation, and psychotic symptoms |
| Group therapies | CBT for psychopathological symptoms CBT for insomnia and smoking cessation Psychoeducation Family therapy |
| Moderator | Potential Intervention | Mediator | Potential Intervention | Behaviors |
|---|---|---|---|---|
| Substance use disorders Social isolation | Psychotherapy Pharmacological treatment Psychosocial intervention | Hostility | Antipsychotics Antidepressants (when needed) Psychotherapy | Aggressive behaviors |
| Aggressivity | ||||
| Impulsivity | ||||
| Depressive symptoms | Suicide attempts | |||
| Paranoid symptoms |
| Aims | |||
| To determine and compare the prevalence of DD in two neighborhoods of Barcelona, Spain (La Mina, Verneda) and describe psychosocial risk factors | |||
| Methods | |||
| Cross-sectional study of cases of DD included in the electronic Case Registry of the La Verneda–La Mina Community Mental Health Unit. | |||
| Results | |||
| Total Sample | La Verneda | La Mina | |
| Cases of DD | N = 209 | N = 145 | N = 64 |
| Prevalence of DD | 20.17/10,000 inhabitants | 18.13/10,000 inhabitants | 27/10,000 inhabitants |
| Employment Situation | Inactive: 115 (62.2%) Active: 70 (37.8%) | Inactive: 75 (60.0%) Active: 51 (40%) | Inactive: 40 (78.8%) Active: 19 (32.2%) |
| Conclusions | |||
| Prevalence of DD in this community-based sample is higher than the prevalence reported in hospital-based studies | |||
| Prevalence of DD is higher in neighborhoods with high frequency of psychosocial and socioeconomic risk factors | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Rodríguez, A.; Alvarez, A.; Guàrdia, A.; Penadés, R.; Monreal, J.A.; Palao, D.J.; Labad, J.; Seeman, M.V. Psychiatric Partial Hospitalization Programs: Following World Health Organization Guidelines with a Special Focus on Women with Delusional Disorder. Women 2021, 1, 80-96. https://doi.org/10.3390/women1020008
González-Rodríguez A, Alvarez A, Guàrdia A, Penadés R, Monreal JA, Palao DJ, Labad J, Seeman MV. Psychiatric Partial Hospitalization Programs: Following World Health Organization Guidelines with a Special Focus on Women with Delusional Disorder. Women. 2021; 1(2):80-96. https://doi.org/10.3390/women1020008
Chicago/Turabian StyleGonzález-Rodríguez, Alexandre, Aida Alvarez, Armand Guàrdia, Rafael Penadés, José Antonio Monreal, Diego J. Palao, Javier Labad, and Mary V. Seeman. 2021. "Psychiatric Partial Hospitalization Programs: Following World Health Organization Guidelines with a Special Focus on Women with Delusional Disorder" Women 1, no. 2: 80-96. https://doi.org/10.3390/women1020008
APA StyleGonzález-Rodríguez, A., Alvarez, A., Guàrdia, A., Penadés, R., Monreal, J. A., Palao, D. J., Labad, J., & Seeman, M. V. (2021). Psychiatric Partial Hospitalization Programs: Following World Health Organization Guidelines with a Special Focus on Women with Delusional Disorder. Women, 1(2), 80-96. https://doi.org/10.3390/women1020008










