Care for Women with Delusional Disorder: Towards a Specialized Approach
Abstract
:1. Introduction
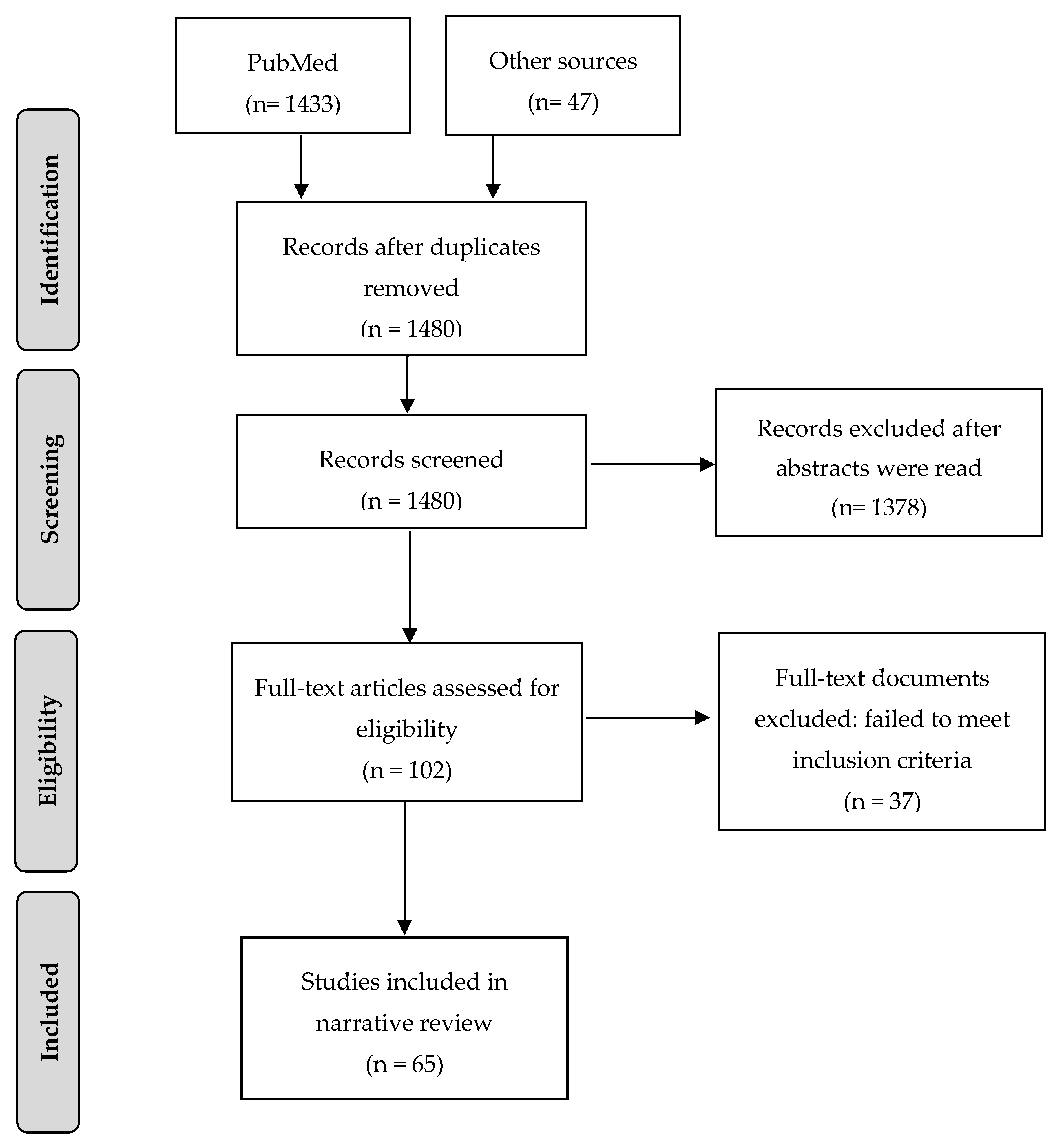
2. Method
3. Gender Differences in Delusional Disorder
4. How Gender Influences Health Outcomes in Delusional Disorder
5. Health Outcomes in Women with Delusional Disorder
5.1. Metabolic Disturbances and Cardiovascular Disease in Women with Delusional Disorder
5.2. Neurologic Disorders in Delusional Disorder
5.3. Autoimmune Diseases in Delusional Disorder
5.4. Risk of Cancer in Delusional Disorder
6. Social Needs in Women with DD
7. Discussion
8. Conclusions
9. Future Perspectives
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Klose, M.; Jacobi, F. Can gender differences in the prevalence of mental disorders be explained by sociodemographic factors? Arch. Women’s Ment. Health 2004, 7, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Kiely, K.M.; Brady, B.; Byles, J. Gender, mental health and ageing. Maturitas 2019, 129, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Riecher-Rössler, A. Sex and gender differences in mental disorders. Lancet Psychiatry 2017, 4, 8–9. [Google Scholar] [CrossRef]
- Lewine, R.R.J.; Hart, M. Schizophrenia spectrum and other psychotic disorders. Interv. Neuroradiol. 2020, 175, 315–333. [Google Scholar] [CrossRef]
- Cunningham, R.; Crowe, M.; Stanley, J.; Haitana, T.; Pitama, S.; Porter, R.; Baxter, J.; Huria, T.; Mulder, R.; Clark, M.T.R.; et al. Gender and mental health service use in bipolar disorder: National cohort study. BJPsych Open 2020, 6, e138. [Google Scholar] [CrossRef]
- Häfner, H. From Onset and Prodromal Stage to a Life-Long Course of Schizophrenia and Its Symptom Dimensions: How Sex, Age, and Other Risk Factors Influence Incidence and Course of Illness. Psychiatry J. 2019, 2019, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Seeman, M.V. Women who suffer from schizophrenia: Critical issues. World J. Psychiatry 2018, 8, 125–136. [Google Scholar] [CrossRef]
- Seeman, M.V. Schizophrenia Psychosis in Women. Women 2020, 1, 1. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Seeman, M.V. Addressing Delusions in Women and Men with Delusional Disorder: Key Points for Clinical Management. Int. J. Environ. Res. Public Health 2020, 17, 4583. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-5, 5th ed.; American Psychiatric Publishing: Arlinghton, VA, USA; Washington, DC, USA, 2013. [Google Scholar]
- Muralidharan, K.; Kulkarni, K.R.; Arasappa, R.; Prasad, M.K.; Zutshi, A.; Chand, P.K.; Murthy, P. Gender differences in persistent delusional disorder. Indian J. Psychol. Med. 2017, 39, 216–217. [Google Scholar] [CrossRef] [Green Version]
- Wustmann, T.; Pillmann, F.; Marneros, A. Gender-related features of persistent delusional disorders. Eur. Arch. Psychiatry Clin. Neurosci. 2010, 261, 29–36. [Google Scholar] [CrossRef]
- De Portugal, E.; González, N.; Vilaplana, M.; Haro, J.M.; Usall, J.; Cervilla, J.A. Gender differences in delusional disorder: Evidence from an outpatient sample. Psychiatry Res. 2010, 177, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Avezuela, N.R.; Díaz, N.E.; Manrique, L.D.; Longás, A.D.; Fernández, C.M.; De Portugal, E.; Del Rivero, F. Diferencias de género en el trastorno delirante. Rev. Asoc. Esp. Neuropsiquiatr. 2015, 35, 37–51. [Google Scholar] [CrossRef] [Green Version]
- Fusar-Poli, P.; Cappucciati, M.; Rutigliano, G.; Heslin, M.; Stahl, D.; Brittenden, Z.; Caverzasi, E.; McGuire, P.; Carpenter, W.T. Diagnostic Stability of ICD/DSM First Episode Psychosis Diagnoses: Meta-analysis. Schizophr. Bull. 2016, 42, 1395–1406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marneros, A.; Pillmann, F.; Wustmann, T. Delusional Disorders--Are They Simply Paranoid Schizophrenia? Schizophr. Bull. 2010, 38, 561–568. [Google Scholar] [CrossRef]
- Almeida, O.P.; Ford, A.H.; Hankey, G.J.; Yeap, B.B.; Golledge, J.; Flicker, L. Risk of dementia associated with psychotic disorders in later life: The health in men study (HIMS). Psychol. Med. 2019, 49, 232–242. [Google Scholar] [CrossRef] [Green Version]
- Jauncey-Cooke, J. What is the evidence for treating delusional Disorder? Issues. Ment. Health. Nurs. 2016, 37, 619–620. [Google Scholar] [CrossRef]
- Skelton, M.; Khokhar, W.A.; Thacker, S.P. Treatments for delusional disorder. Schizophr. Bull. 2015, 41, 1010–1012. [Google Scholar] [CrossRef] [Green Version]
- Muñoz-Negro, J.E.; Cervilla, J. The comprehensive treatment of delusional disorder. Rev. Psiquiatr. Salud Ment. 2017, 10, 221–223. [Google Scholar] [CrossRef]
- O’Connor, K.P.; Stip, É.; Pélissier, M.-C.; Aardema, F.; Guay, S.; Gaudette, G.; Van Haaster, I.; Robillard, S.; Grenier, S.; Careau, Y.; et al. Treating delusional disorder: A comparison of cognitive-behavioural therapy and attention placebo control. Can. J. Psychiatry 2007, 52, 182–190. [Google Scholar] [CrossRef] [Green Version]
- Seeman, M.V. Men and women respond differently to antipsychotic drugs. Neuropharmacology 2020, 163, 107631. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, A.; Esteve, M.; Álvarez, A.; Guardia, A.; Monreal, J.A.; Palao, D.; Labad, J. What We Know and Still Need to Know about Gender Aspects of Delusional Disorder: A Narrative Review of Recent Work. J. Psychiatry Brain Sci. 2019, 4, 190009. [Google Scholar] [CrossRef] [Green Version]
- Lindamer, L.A.; Buse, D.C.; Auslander, L.; Unützer, J.; Bartels, S.J.; Jeste, D.V. A Comparison of Gynecological Variables and Service Use among Older Women with and without Schizophrenia. Psychiatr. Serv. 2003, 54, 902–904. [Google Scholar] [CrossRef] [PubMed]
- Castañeda, I.E. Theoretical reflections on the differences in health attributable to gender. Cub. J. Public Health 2007, 33, 2007. [Google Scholar]
- Maas, A.; Appelman, Y. Gender differences in coronary heart disease. Neth. Hear. J. 2010, 18, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Moisan, F.; Kab, S.; Mohamed, F.; Canonico, M.; Le Guern, M.; Quintin, C.; Carcaillon, L.; Nicolau, J.; Duport, N.; Singh-Manoux, A.; et al. Parkinson disease male-to-female ratios increase with age: French nationwide study and meta-analysis. J. Neurol. Neurosurg. Psychiatry 2015, 87, 952–957. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.-H.; Lin, C.-L.; Jeng, L.-B. Association between chronic pancreatitis and urolithiasis: A population-based cohort study. PLoS ONE 2018, 13, e0194019. [Google Scholar] [CrossRef] [Green Version]
- Alswat, K.A. Gender Disparities in Osteoporosis. J. Clin. Med. Res. 2017, 9, 382–387. [Google Scholar] [CrossRef] [Green Version]
- Kostev, K.; Bohlken, J.; Jacob, L. Association Between Migraine Headaches and Dementia in More than 7400 Patients Followed in General Practices in the United Kingdom. J. Alzheimer’s Dis. 2019, 71, 353–360. [Google Scholar] [CrossRef]
- Ochoa, S.; Usall, J.; Cobo, J.; Labad, X.; Kulkarni, J. Gender Differences in Schizophrenia and First-Episode Psychosis: A Comprehensive Literature Review. Schizophr. Res. Treat. 2012, 2012, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Meaney, A.M.; Smith, S.; Howes, O.D.; O’Brien, M.; Murray, R.M.; O’Keane, V. Effects of long-term prolactin-raising antipsychotic medication on bone mineral density in patients with schizophrenia. Br. J. Psychiatry 2004, 184, 503–508. [Google Scholar] [CrossRef] [PubMed]
- O’Keane, V. Antipsychotic-induced hyperprolactinaemia, hypogonadism and osteoporosis in the treatment of schizophrenia. J. Psychopharmacol. 2008, 22, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Boke, O.; Aker, S.; Sarisoy, G.; Saricicek, E.B.; Sahin, A.R. Prevalence of metabolic syndrome among inpatients with schizophrenia. Int. J. Psychiatry Med. 2008, 38, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Copeland, J.R.; Dewey, M.E.; Scott, A.; Gilmore, C.; Larkin, B.A.; Cleave, N.; McCracken, C.F.; McKibbin, P. Schizophrenia and Delusional Disorder in Older Age: Community Prevalence, Incidence, Comorbidity, and Outcome. Schizophr. Bull. 1998, 24, 153–161. [Google Scholar] [CrossRef] [Green Version]
- Lepping, P.; Noorthoorn, E.O.; Kemperman, P.M.J.H.; Harth, W.; Reichenberg, J.S.; Squire, S.B.; Shinhmar, S.; Freudenmann, R.W.; Bewley, A. An international study of the prevalence of substance use in patients with delusional infestation. J. Am. Acad. Dermatol. 2017, 77, 778–779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gurvich, C.; Gavrilidis, E.; Worsley, R.; Hudaib, A.; Thomas, N.; Kulkarni, J.; Hadaib, A. Menstrual cycle irregularity and menopause status influence cognition in women with schizophrenia. Psychoneuroendocrinology 2018, 96, 173–178. [Google Scholar] [CrossRef] [PubMed]
- González-Rodríguez, A.; Guàrdia, A.; Palao, D.J.; Labad, J.; Seeman, M.V. Moderators and mediators of antipsychotic response in delusional disorder: Further steps are needed. World J. Psychiatry 2020, 10, 34–45. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Molina-Andreu, O.; Navarro, V.; Gastó, C.; Penadés, R.; Catalán, R. Delusional disorder: No gender differences in age at onset, suicidal ideation, or suicidal behavior. Rev. Bras. Psiquiatr. 2014, 36, 119–124. [Google Scholar] [CrossRef] [Green Version]
- Feng, Y.; Hong, X.; Wilker, E.; Li, Z.; Zhang, W.; Jin, D.; Liu, X.; Zang, T.; Xu, X.; Xu, X. Effects of age at menarche, reproductive years, and menopause on metabolic risk factors for cardiovascular diseases. Atherosclerosis 2008, 196, 590–597. [Google Scholar] [CrossRef] [Green Version]
- Auro, K.; Joensuu, A.; Fischer, K.; Kettunen, J.; Salo, P.; Mattsson, H.; Niironen, M.; Kaprio, J.; Eriksson, J.G.; Lehtimäki, T.; et al. A metabolic view on menopause and ageing. Nat. Commun. 2014, 5, 4708. [Google Scholar] [CrossRef] [Green Version]
- Merz, A.; Cheng, S. Sex differences in cardiovascular ageing. Heart 2016, 102, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Chohan, P.S.; Mittal, R.; Javed, A. Antipsychotic Medication and QT Prolongation. Pak. J. Med. Sci. 2015, 31, 1269–1271. [Google Scholar] [PubMed]
- Somberg, J.; Preston, R.A.; Ranade, V.; Cvetanovic, I.; Molnar, J. Gender Differences in Cardiac Repolarization Following Intravenous Sotalol Administration. J. Cardiovasc. Pharmacol. Ther. 2011, 17, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Kane, A.E.; Howlett, S. Differences in Cardiovascular Aging in Men and Women. In Sex-Specific Analysis of Cardiovascular Function; Springer: Cham, Switzerland, 2018; pp. 389–411. [Google Scholar] [CrossRef]
- Keller, K.M.; Howlett, S. Sex Differences in the Biology and Pathology of the Aging Heart. Can. J. Cardiol. 2016, 32, 1065–1073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shufelt, C.L.; Pacheco, C.; Tweet, M.S.; Miller, V.M. Sex-Specific Physiology and Cardiovascular Disease. In Sex-Specific Analysis of Cardiovascular Function; Springer: Cham, Switzerland, 2018; pp. 433–454. [Google Scholar] [CrossRef]
- Muka, T.; Oliver-Williams, C.; Kunutsor, S.; Laven, J.S.E.; Fauser, B.C.J.M.; Chowdhury, R.; Kavousi, M.; Franco, O.H. Association of Age at Onset of Menopause and Time Since Onset of Menopause With Cardiovascular Outcomes, Intermediate Vascular Traits, and All-Cause Mortality. JAMA Cardiol. 2016, 1, 767–776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colpani, V.; Baena, C.P.; Jaspers, L.; Van Dijk, G.M.; Farajzadegan, Z.; Dhana, K.; Tielemans, M.J.; Voortman, T.; Freak-Poli, R.; Veloso, G.G.V.; et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: A systematic review and meta-analysis. Eur. J. Epidemiol. 2018, 33, 831–845. [Google Scholar] [CrossRef]
- Scheyer, O.; Rahman, A.; Hristov, H.; Berkowitz, C.; Isaacson, R.S.; Diaz Brinton, R.; Mosconi, L. Female sex and Alzheimer’s risk: The menopause connection. J. Prev. Alzheimer’s Dis. 2018, 5, 225–230. [Google Scholar]
- Marongiu, R. Accelerated Ovarian Failure as a Unique Model to Study Peri-Menopause Influence on Alzheimer’s Disease. Front. Aging Neurosci. 2019, 11, 242. [Google Scholar] [CrossRef] [Green Version]
- Díaz-Caneja, C.M.; Cervilla, J.; Haro, J.M.; Arango, C.; De Portugal, E. Cognition and functionality in delusional disorder. Eur. Psychiatry 2019, 55, 52–60. [Google Scholar] [CrossRef]
- Kørner, A.; Lopez, A.G.; Lauritzen, L.; Andersen, P.K.; Kessing, L.V. Delusional disorder in old age and the risk of developing dementia–a nationwide register-based study. Aging Ment. Health 2008, 12, 625–629. [Google Scholar] [CrossRef]
- Reekes, T.H.; Higginson, C.I.; Ledbetter, C.R.; Sathivadivel, N.; Zweig, R.M.; Disbrow, E.A. Sex specific cognitive differences in Parkinson disease. npj Park. Dis. 2020, 6, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Caroff, S.N.; Campbell, E.C. Drug-induced extrapyramidal syndromes: Implications for contemporary practice. Psychiatr. Clin. N. Am. 2016, 39, 391–411. [Google Scholar]
- Ricciardi, L.; Pringsheim, T.; Barnes, T.R.; Martino, D.; Gardner, D.; Remington, G.; Addington, D.; Morgante, F.; Poole, N.; Carson, A.; et al. Treatment Recommendations for Tardive Dyskinesia. Can. J. Psychiatry 2019, 64, 388–399. [Google Scholar] [CrossRef] [PubMed]
- Vicens, V.; Radua, J.; Salvador, R.; Anguera-Camós, M.; Canales-Rodríguez, E.J.; Sarró, S.; Maristany, T.; McKenna, P.J.; Pomarol-Clotet, E. Structural and functional brain changes in delusional disorder. Br. J. Psychiatry 2016, 208, 153–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- González-Rodríguez, A.; Molina-Andreu, O.; Penadés, R.; Catalán, R.; Bernardo, M. Structural and Functional Neuroimaging Findings in Delusional Disorder: Diagnostic and Therapeutic Implications. Open Psychiatry J. 2015, 9, 17–25. [Google Scholar] [CrossRef]
- Ngo, S.; Steyn, F.; McCombe, P.A. Gender differences in autoimmune disease. Front. Neuroendocr. 2014, 35, 347–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solmi, M.; Murru, A.; Pacchiarotti, I.; Undurraga, J.; Veronese, N.; Fornaro, M.; Stubbs, B.; Monaco, F.; Vieta, E.; Seeman, M.V.; et al. Safety, tolerability, and risks associated with first- and second-generation antipsychotics: A state-of-the-art clinical review. Ther. Clin. Risk Manag. 2017, 13, 757–777. [Google Scholar] [CrossRef] [Green Version]
- Jeppesen, R.; Benros, M.E. Autoimmune Diseases and Psychotic Disorders. Front. Psychiatry 2019, 10, 131. [Google Scholar] [CrossRef] [Green Version]
- Debnath, M.; Das, S.K.; Bera, N.K.; Nayak, C.R.; Chaudhuri, T.K. Genetic Associations between Delusional Disorder and Paranoid Schizophrenia: A Novel Etiologic Approach. Can. J. Psychiatry 2006, 51, 342–349. [Google Scholar] [CrossRef] [Green Version]
- Pearman, T.P. Delusional Disorder and Oncology: Review of the Literature and Case Report. Int. J. Psychiatry Med. 2013, 45, 237–243. [Google Scholar] [CrossRef]
- González-Rodríguez, A.; Labad, J.; Seeman, M.V. Schizophrenia and cancer. Curr. Opin. Support. Palliat. Care 2020, 14, 232–238. [Google Scholar] [CrossRef]
- Hodgson, R.; Wildgust, H.J.; Bushe, C.J. Review: Cancer and schizophrenia: Is there a paradox? J. Psychopharmacol. 2010, 24, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Kredentser, M.S.; Martens, P.J.; Chochinov, H.M.; Prior, H.J. Cause and rate of death in people with schizophrenia across the lifespan: A population-based study in Manitoba, Canada. J. Clin. Psychiatry 2014, 75, 154–161. [Google Scholar] [CrossRef]
- Fond, G.; Salas, S.; Pauly, V.; Baumstarck, K.; Bernard, C.; Orleans, V.; Llorca, P.-M.; Lancon, C.; Auquier, P.; Boyer, L. End-of-life care among patients with schizophrenia and cancer: A population-based cohort study from the French national hospital database. Lancet Public Health 2019, 4, e583–e591. [Google Scholar] [CrossRef] [Green Version]
- Zhuo, C.; Tao, R.; Jiang, R.; Lin, X.; Shao, M. Cancer mortality in patients with schizophrenia: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 211, 7–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christensen, R.C.; Ramos, E. The Social and Treatment Consequences of a Shared Delusional Disorder in a Homeless Family. Innov. Clin. Neurosci. 2011, 8, 42–44. [Google Scholar] [PubMed]
- Al-Tannir, M.; AlGahtani, F.; Abu-Shaheen, A.; Al-Tannir, S.; Alfayyad, I. Patient experiences of engagement with care plans and healthcare professionals’ perceptions of that engagement. BMC Health Serv. Res. 2017, 17, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Strandås, M.; Bondas, T.E. The nurse-patient relationship as a story of health enhancement in community care: A meta-ethnography. J. Adv. Nurs. 2017, 74, 11–22. [Google Scholar] [CrossRef] [Green Version]
- Martin, L.R.; Williams, S.L.; Haskard, K.B.; DiMatteo, M.R. The challenge of patient adherence. Ther. Clin. Risk Manag. 2005, 1, 189–199. [Google Scholar]
- Leslie, J.L.; Lonneman, W. Promoting Trust in the Registered Nurse-Patient Relationship. Home Health Now 2016, 34, 38–42. [Google Scholar] [CrossRef]
- Feo, R.; Conroy, T.; Wiechula, R.; Rasmussen, P.; Kitson, A. Instruments measuring behavioural aspects of the nurse–patient relationship: A scoping review. J. Clin. Nurs. 2019, 29, 1808–1821. [Google Scholar] [CrossRef] [PubMed]
- Uhrenfeldt, L.; Sorensen, E.E.; Bahnsen, I.B.; Pedersen, P.U. The centrality of the nurse-patient relationship: A Scandinavian perspective. J. Clin. Nurs. 2018, 27, 3197–3204. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.A.; Wong, F.; Cheung, M.Y.; Lam, W. Patients’ perceptions of their experiences with nurse-patient communication in oncology settings: A focused ethnographic study. PLoS ONE 2018, 13, e0199183. [Google Scholar] [CrossRef] [PubMed]
| DSM-5 Criteria for DD | |
|---|---|
| Diagnostic criteria | Existence of one or more delusions that last for at least 1 month. |
| Exclusion criteria | - Criterion A for schizophrenia is never met - Functioning not obviously impaired - Manic or major depressive disorders brief - Delusions cannot be attributed to the physiological effects of a substance or a medical condition |
| Subtypes of DD according to delusional content | |
| Persecutory type | Belief that one is being persecuted or conspired against. |
| Jealous type | Conviction that one’s lover is unfaithful. |
| Erotomanic type | Belief that someone of relatively high social status is romantically interested. |
| Somatic type | Conviction that one’s body is infested, malformed or ill without possibility of cure. |
| Grandiose type | Belief that one is superior to others for several reasons. |
| Mixed type | False beliefs that are a mixture of the above. |
| Unspecified type | Vagueness in the expression of delusions that does not permit classification. |
| Health and Social Needs | Strategy |
|---|---|
| Women’s Mental Health | |
| Psychotic symptoms | Antipsychotics +/- psychological interventions (CBT) |
| Depressive symptoms | Antidepressants +/- psychologic interventions |
| Cognitive symptoms | Early detection; referral to memory clinics; psychological/educational approaches (cognitive remediation); cognitive enhancers |
| Physical comorbidities | |
| Hypertension, diabetes mellitus and obesity-cardiovascular disease risk factors, autoimmune disorders | Regular, routine, B.P., BMI checks, glucose, EKG checks, regular GP visits Attention to diet, smoking, exercise, sleep |
| Cancer | Regular screening and GP visits |
| Osteoporosis | Bone density measurements, assessment of fracture risk |
| Social Needs | |
| Low income, social adversity | Referral to social work, budgeting, meal preparation Housing, marital support, parenting support, household help Employment support |
| Barriers to help-seeking | Ensuring continuity of care, GP access, follow up of missed appointments; provision of disability income support and childcare |
| Men | Women |
|---|---|
| Gender influence on health outcomes in general population | |
| Heart disease Parkinson’s disease Kidney stones Pancreatitis | Osteoporosis Urinary tract problems Alzheimer’s disease Migraine Multiple sclerosis |
| Gender influence on health outcomes in schizophrenia | |
| Sexual dysfunction Coronary heart disease | Menstrual irregularities Reduced bone mineral density Metabolic syndrome Diabetes mellitus Autoimmune disorders |
| Gender influence on health outcomes in delusional disorder | |
| Cardiovascular disease Alcohol use | Alzheimer’s disease Osteoporosis |
| Metabolic Disturbances and Cardiovascular Disease | |
|---|---|
| Observation | Potential explanation |
| Increased adult adiposity, insulin sensitivity and blood lipid levels | Metabolic syndrome may be attributable to reduce estrogen levels at menopause and to the use of antipsychotics |
| Increased cardiovascular risk | Occurs at advanced age. Loss of estrogens at menopause, lifestyles (smoking and high BMI) and antipsychotics use also contribute |
| Neurologic disorders | |
| Observation | Potential explanation |
| Increased risk of cognitive disorders (or dementia) | Patients with DD show impaired verbal memory and other cognitive symptoms attributable to an increase in cerebrovascular events (because of age and the use of antipsychotics) |
| Movement disorders (extrapyramidal symptoms and tardive dyskinesia) | Loss of estrogens at menopause increases its risk of tardive dyskinesia. Antipsychotic dose may be too high. The incidence of extrapyramidal disorders: increases with age |
| Autoimmunity | |
| Autoimmune diseases | Women are more susceptible to autoimmune disorders than men. At menopause, the risk is increased |
| Risk of cancer | |
| Gynecological cancers | Women with DD may show low compliance with gynecological appointments and are less likely than peers to receive cancer screening |
| Other cancers | Little is known. Lifestyle factors may contribute to an increased mortality. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Rodríguez, A.; Seeman, M.V.; Álvarez, A.; Guàrdia, A.; Sanz, N.; Fucho, G.F.; Palao, D.J.; Labad, J. Care for Women with Delusional Disorder: Towards a Specialized Approach. Women 2021, 1, 46-59. https://doi.org/10.3390/women1010004
González-Rodríguez A, Seeman MV, Álvarez A, Guàrdia A, Sanz N, Fucho GF, Palao DJ, Labad J. Care for Women with Delusional Disorder: Towards a Specialized Approach. Women. 2021; 1(1):46-59. https://doi.org/10.3390/women1010004
Chicago/Turabian StyleGonzález-Rodríguez, Alexandre, Mary V. Seeman, Aida Álvarez, Armand Guàrdia, Nadia Sanz, Genís F. Fucho, Diego J. Palao, and Javier Labad. 2021. "Care for Women with Delusional Disorder: Towards a Specialized Approach" Women 1, no. 1: 46-59. https://doi.org/10.3390/women1010004
APA StyleGonzález-Rodríguez, A., Seeman, M. V., Álvarez, A., Guàrdia, A., Sanz, N., Fucho, G. F., Palao, D. J., & Labad, J. (2021). Care for Women with Delusional Disorder: Towards a Specialized Approach. Women, 1(1), 46-59. https://doi.org/10.3390/women1010004








