A Systematic Review of Moderators of the Association between Dietary Restraint and Binge Eating
Abstract
1. Introduction
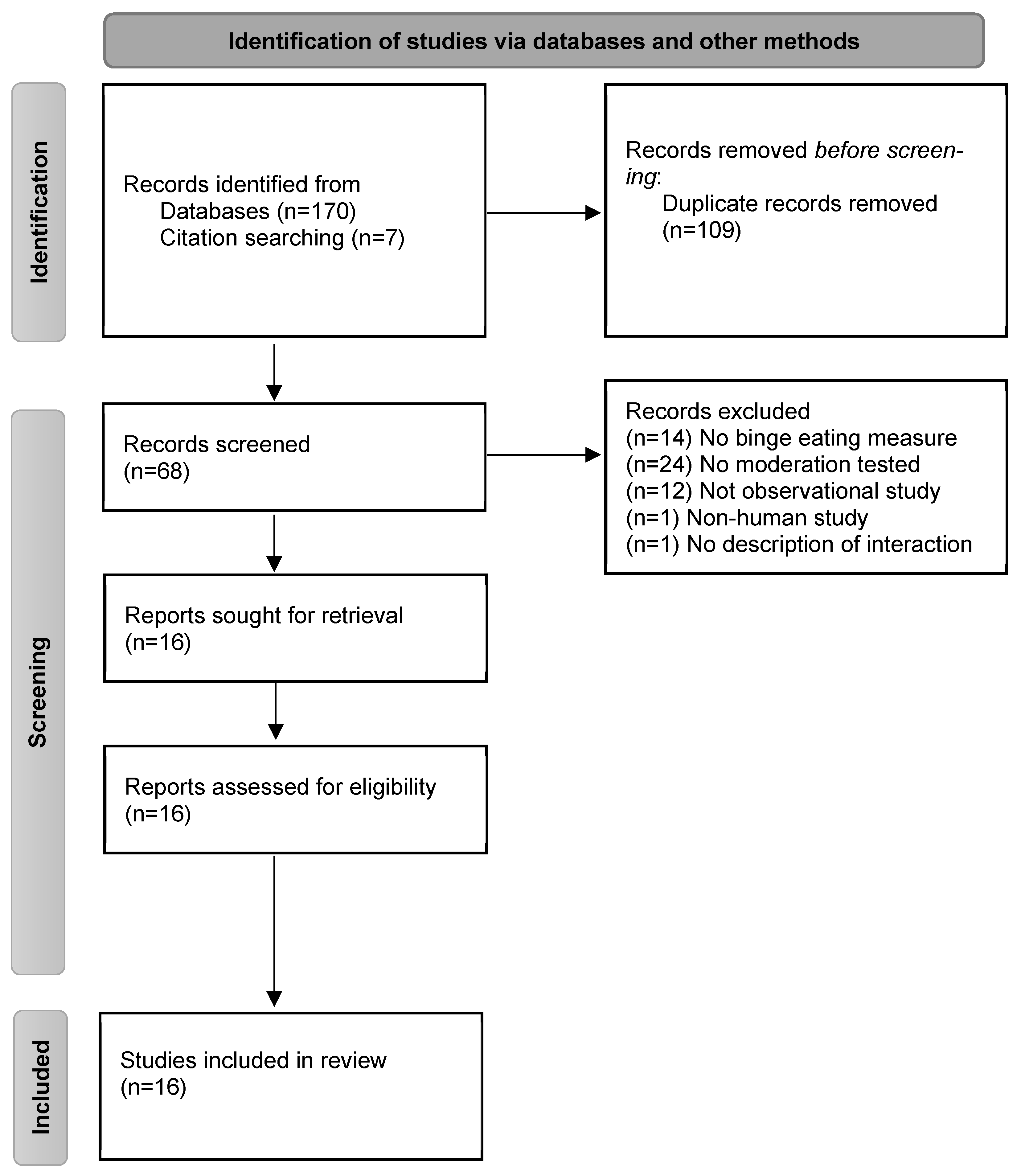
2. Method
3. Results
3.1. Descriptive Findings
3.2. Primary Findings
3.3. Cognitive Factors
3.4. Social Factors
3.4.1. Affect and Cognitive Factor Interactions
3.4.2. Genetic and Cognitive Factor Interactions
4. Discussion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Cecchini, M.; Sassi, F.; Lauer, J.A.; Lee, Y.Y.; Guajardo-Barron, V.; Chisholm, D. Tackling of unhealthy diets, physical inactivity, and obesity: Health effects and cost-effectiveness. Lancet 2010, 376, 1775–1784. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Guerra, L.S.; Coêlho, B.M.; Santo, M.A.; Wang, Y.P. Psychiatric disorders among obese patients seeking bariatric surgery: Results of structured clinical interviews. Obes. Surg. 2015, 25, 830–837. [Google Scholar] [CrossRef] [PubMed]
- Simon, G.E.; Von Korff, M.; Saunders, K.; Miglioretti, D.L.; Crane, P.K.; Van Belle, G.; Kessler, R.C. Association between obesity and psychiatric disorders in the US adult population. Arch. Gen. Psychiatry 2006, 63, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Graubard, B.I.; Williamson, D.F.; Gail, M.H. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005, 293, 1861–1867. [Google Scholar] [CrossRef]
- Curioni, C.C.; Lourenco, P.M. Long-term weight loss after diet and exercise: A systematic review. Int. J. Obes. 2005, 29, 1168. [Google Scholar] [CrossRef] [PubMed]
- Karfopoulou, E.; Brikou, D.; Mamalaki, E.; Bersimis, F.; Anastasiou, C.A.; Hill, J.O.; Yannakoulia, M. Dietary patterns in weight loss maintenance: Results from the MedWeight study. Eur. J. Nutr. 2017, 56, 991–1002. [Google Scholar] [CrossRef] [PubMed]
- Montesi, L.; El Ghoch, M.; Brodosi, L.; Calugi, S.; Marchesini, G.; Dalle Grave, R. Long-term weight loss maintenance for obesity: A multidisciplinary approach. Diabetes Metab. Syndr. Obes. 2016, 9, 37. [Google Scholar] [CrossRef] [PubMed]
- Heatherton, T.F.; Polivy, J. Chronic dieting and eating disorders: A spiral model. In The Etiology of Bulimia Nervosa: The Individual and Familial Context; Crowther, J.H., Tennenbaum, D.L., Hobfoll, S.E., Stephens, M.A.P., Eds.; Series in Applied Psychology: Social Issues and Questions; Hemisphererp: Washington, DC, USA, 1992; pp. 133–155. [Google Scholar]
- Stice, E. A prospective test of the dual-pathway model of bulimic pathology: Mediating effects of dieting and negative affect. J. Abnorm. Psychol. 2001, 110, 124–135. [Google Scholar] [CrossRef]
- Field, A.E.; Austin, S.B.; Taylor, C.B.; Malspeis, S.; Rosner, B.; Rockett, H.R.; Colditz, G.A. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics 2003, 112, 900–906. [Google Scholar] [CrossRef]
- Mann, T.; Tomiyama, A.J.; Westling, E.; Lew, A.M.; Samuels, B.; Chatman, J. Medicare’s search for effective obesity treatments: Diets are not the answer. Am. Psychol. 2007, 62, 220–233. [Google Scholar] [CrossRef]
- Bartholomay, J.; Schaefer, L.M.; Forester, G.; Crosby, R.D.; Peterson, C.B.; Crow, S.J.; Wonderlich, S.A. Evaluating dietary restriction as a maintaining factor in binge-eating disorder. Int. J. Eat. Disord. 2023, 57, 1172–1180. [Google Scholar] [CrossRef]
- Schaumberg, K.; Anderson, D.A.; Anderson, L.M.; Reilly, E.E.; Gorrell, S. Dietary restraint: What’s the harm? A review of the relationship between dietary restraint, weight trajectory and the development of eating pathology. Clin. Obes. 2016, 6, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Catenacci, V.A.; Odgen, L.; Phelan, S.; Thomas, J.G.; Hill, J.; Wing, R.R.; Wyatt, H. Dietary habits and weight maintenance success in high versus low exercisers in the National Weight Control Registry. J. Phys. Act. Health 2014, 11, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Klem, M.L.; Wing, R.R.; McGuire, M.T.; Seagle, H.M.; Hill, J.O. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. The Am. J. Clin. Nutr. 1997, 66, 239–246. [Google Scholar] [CrossRef]
- Phelan, S.; Liu, T.; Gorin, A.; Lowe, M.; Hogan, J.; Fava, J.; Wing, R.R. What distinguishes weight-loss maintainers from the treatment-seeking obese? Analysis of environmental, behavioral, and psychosocial variables in diverse populations. Ann. Behav. Med. 2009, 38, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Phelan, S. Long-term weight loss maintenance. Am. J. Clin. Nutr. 2005, 82, 222S–225S. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Akutagawa, D.; Gaggar, A.; Agras, W.S. Negative affect moderates the relation between dieting and binge eating. Int. J. Eat. Disord. 2000, 27, 218–229. [Google Scholar] [CrossRef]
- Loth, K.A.; Goldschmidt, A.B.; Wonderlich, S.A.; Lavender, J.M.; Neumark-Sztainer, D.; Vohs, K.D. Could the resource depletion model of self-control help the field to better understand momentary processes that lead to binge eating? Int. J. Eat. Disord. 2016, 49, 998–1001. [Google Scholar] [CrossRef] [PubMed]
- Parums, D.V. Review articles, systematic reviews, meta-analysis, and the updated preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2020 guidelines. Med. Sci. Monit. 2021, 27, e934475-1. [Google Scholar] [CrossRef]
- Chervinko, S.M. Potential Moderators of the Relationship between Dietary Restraint and Binge Eating: Affect Intensity, Body Shame, and Coping Styles; Michigan State University: East Lansing, MI, USA, 2004. [Google Scholar]
- Emery, R.L.; King, K.M.; Fischer, S.F.; Davis, K.R. The moderating role of negative urgency on the prospective association between dietary restraint and binge eating. Appetite 2013, 71, 113–119. [Google Scholar] [CrossRef]
- Greenberg, B.R.; Harvey, P.D. Affective lability versus depression as determinants of binge eating. Addict. Behav. 1987, 12, 357–361. [Google Scholar] [CrossRef]
- Linardon, J. The relationship between dietary restraint and binge eating: Examining eating-related self-efficacy as a moderator. Appetite 2018, 127, 126–129. [Google Scholar] [CrossRef]
- Mason, T.B.; Heron, K.E.; Braitman, A.L.; Lewis, R.J. A daily diary study of perceived social isolation, dietary restraint, and negative affect in binge eating. Appetite 2016, 97, 94–100. [Google Scholar] [CrossRef]
- Mason, T.B.; Smith, K.E.; Lavender, J.M.; Lewis, R.J. Independent and interactive associations of negative affect, restraint, and impulsivity in relation to binge eating among women. Appetite 2018, 121, 147–153. [Google Scholar] [CrossRef]
- Mason, T.B.; Dolgon-Krutolow, A.; Smith, K.E.; Leventhal, A.M. Body dissatisfaction and binge eating: The moderating roles of sweet taste reward sensitivity and dietary restraint among tobacco product users. Int. J. Environ. Res. Public Health 2022, 19, 15523. [Google Scholar] [CrossRef]
- Nadel, A.L. Impulsivity, Negative Affect, and Binge Eating in College Students: A daily Diary Approach. Doctoral Dissertation, Fairleigh Dickinson University, Teaneck, NJ, USA, 2014. [Google Scholar]
- Pearson, C.M.; Mason, T.B.; Cao, L.; Goldschmidt, A.B.; Lavender, J.M.; Crosby, R.D.; Peterson, C.B. A test of a state-based, self-control theory of binge eating in adults with obesity. Eat. Disord. 2018, 26, 26–38. [Google Scholar] [CrossRef]
- Racine, S.E.; Culbert, K.M.; Larson, C.L.; Klump, K.L. The possible influence of impulsivity and dietary restraint on associations between serotonin genes and binge eating. J. Psychiatr. Res. 2009, 43, 1278–1286. [Google Scholar] [CrossRef]
- Racine, S.E.; Burt, S.A.; Iacono, W.G.; McGue, M.; Klump, K.L. Dietary restraint moderates genetic risk for binge eating. J. Abnorm. Psychol. 2011, 120, 119–128. [Google Scholar] [CrossRef]
- Racine, S.E.; VanHuysse, J.L.; Keel, P.K.; Burt, S.A.; Neale, M.C.; Boker, S.; Klump, K.L. Eating disorder-specific risk factors moderate the relationship between negative urgency and binge eating: A behavioral genetic investigation. J. Abnorm. Psychol. 2017, 126, 481–494. [Google Scholar] [CrossRef]
- Sehm, M.; Warschburger, P. The specificity of psychological factors associated with binge eating in adolescent boys and girls. J. Abnorm. Child Psychol. 2015, 43, 1563–1571. [Google Scholar] [CrossRef]
- Wenzel, K.R.; Weinstock, J.; Vander Wal, J.S.; Weaver, T.L. Examining the role of negative urgency in a predictive model of bulimic symptoms. Eat. Behav. 2014, 15, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Woods, A.M.; Racine, S.E.; Klump, K.L. Examining the relationship between dietary restraint and binge eating: Differential effects of major and minor stressors. Eat. Behav. 2010, 11, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Sommet, N.; Weissman, D.L.; Cheutin, N.; Elliot, A.J. How many participants do I need to test an interaction? Conducting an appropriate power analysis and achieving sufficient power to detect an interaction. Adv. Methods Pract. Psychol. Sci. 2023, 6, 25152459231178728. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [CrossRef]
- Stunkard, A.J.; Messick, S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J. Psychosom. Res. 1985, 29, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Van Strien, T.; Frijters, J.E.; Bergers, G.P.; Defares, P.B. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 1986, 5, 295–315. [Google Scholar] [CrossRef]
- Polivy, J.; Herman, C.P.; Mills, J.S. What is restrained eating and how do we identify it? Appetite 2020, 155, 104820. [Google Scholar] [CrossRef] [PubMed]
- Bond, M.J.; McDowell, A.J.; Wilkinson, J.Y. The measurement of dietary restraint, disinhibition and hunger: An examination of the factor structure of the Three Factor Eating Questionnaire (TFEQ). Int. J. Obes. 2001, 25, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, L.M.; Forester, G.; Dvorak, R.D.; Steinglass, J.; Wonderlich, S.A. Integrating aspects of affect, reward, and cognition to develop more comprehensive models of binge-eating pathology. Int. J. Eat. Disord. 2023, 56, 1502–1510. [Google Scholar] [CrossRef]
- Ahrberg, M.; Trojca, D.; Nasrawi, N.; Vocks, S. Body image disturbance in binge eating disorder: A review. Eur. Eat. Disord. Rev. 2011, 19, 375–381. [Google Scholar] [CrossRef]
- Levine, M.P.; Piran, N. The role of body image in the prevention of eating disorders. Body Image 2004, 1, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, R.F.; DuBois, R.H. Cognitive biases to appearance-related stimuli in body dissatisfaction: A systematic review. Clin. Psychol. Rev. 2016, 46, 1–11. [Google Scholar] [CrossRef] [PubMed]
| Reference | Sample Characteristics | Sample Recruited | Dietary Restraint/Restriction Measure | Moderator | Binge Eating Measure | Moderation Findings |
|---|---|---|---|---|---|---|
| Chervinko 2004 [21] | N = 139; 100% female; mean age = 20.2 years; 80.6% White, 0.7% Asian, 12.2% Black, 2.2% Hispanic, 0.7% Arabic, 2.2% Multiracial; mean BMI = 23.4; 4.3% LGBTQ | College/university | Eating Inventory—Cognitive Restraint subscale; Revised Restraint Scale | Affect intensity assessed with the Affect Intensity Measure; body shame assessed with the Objectified Body Consciousness Scale-Body Shame Scale; coping assessed with the Coping Inventory for Stressful Situations | Bulimia Test-Revised-Binge Control Scale | There were no interactions between restraint and any of the moderators (i.e., body shame, affect intensity, emotion-focused coping, and avoidance-focused coping) in relation to binge eating. |
| Emery et al. 2013 [22] | N = 460; 100% female; mean age = 18.04 years; 75.9% White, 7.4% Asian, 10.7% Black, 1.7% Hispanic, 3.0% biracial, 1.3% other race | College/university | Eating Disorder Examination Questionnaire—Restraint | Negative urgency assessed with UPPS Impulsive Behavior Scale | Eating Disorder Examination Questionnaire—binge eating frequency | Controlling for baseline binge eating, among those who reported binge eating, higher restraint increased binge eating frequency three months later for those with low and mean negative urgency; those with high negative urgency had higher binge eating frequency regardless of restraint level. There was no interaction between restraint and negative urgency predicting likelihood of binge eating vs. not binge eating. |
| Greenberg and Harvey 1987 [23] | N = 73; 100% female; mean age = 18.33 ± 0.73 years | College/university | Restraint Scale | Depressive symptoms assessed with the Beck Depression Inventory; depressive, hypomania, and biphasic symptom assessed with the General Behavior Inventory | Binge Scale | There was a significant interaction between restraint and biphasic symptoms in relation to binge eating, such that biphasic symptoms strengthened the association between restraint and higher binge eating |
| Linardon 2018 [24] | N = 237; 100% female; mean age = 24.93 ± 8.98; mean BMI = 23.30 ± 8.90 | College/university and community | Cognitive Restraint Scale—Flexible Restraint and Rigid Restraint subscales | Eating self-efficacy assessed with the Eating Behavior Self-Efficacy Measure | Binge Eating Scale | There was a significant interaction between flexible restraint and eating self-efficacy in relation to binge eating, such that the association between flexible restraint and binge eating was greatest for those with moderate to strong self-efficacy. There was no interaction between eating self-efficacy and rigid restraint and binge eating. |
| Mason et al. 2016 [25] | N = 54; 100% female; mean age = 24.98 ± 7.8; 57.3% White, 25.9% Black, 1.9% Asian, 1.9% Native Hawaiian or Pacific Islander, 11.1% two or more races, 1.9% other race; mean BMI = 26.65 ± 7.16 | College/university | Combination of four items from the Dutch Restrained Eating Scale; three items from the Dietary Intent Scale; four items from the Three-Factor Eating Questionnaire—Restraint subscale | Negative affect assessed with the Positive and Negative Affect Schedule; perceived social isolation assessed with the Friendship Scale | Combination of four items from the Eating Disorder Inventory—Bulimia Scale and seven items from the Eating Disorder Diagnostic Scale | Neither daily negative affect nor daily perceived social isolation moderated the association between daily restraint and binge eating. |
| Mason et al. 2018 [26] | N = 556; 100% female; mean age = 22.943 ± 6.61; 46.0% White, 34.7% Black, 12.0% two or more races, 7.2% other race; mean BMI = 25.00 ± 5.98; 15% LGBTQ | College/university | Dutch Eating Behavior Questionnaire—Restraint subscale | Negative affect assessed with the Positive and Negative Affect Schedule; impulsivity assessed with Barratt Impulsiveness Scale | Combination of four items from the Eating Disorder Inventory—Bulimia Scale and seven items from the Eating Disorder Diagnostic Scale | There was a three-way interaction between restraint, attentional impulsivity, and negative affect, such that participants with elevated levels of all three factors reported the greatest levels of binge eating. There were no interactions with motor or nonplanning impulsivity. |
| Mason et al. 2022 [27] | N = 221 tobacco product users; 45.7% female; mean age = 34.53 ± 13.28; 67.1% White, 13.2% Black, 5.5% Hispanic, 4.6% Asian or Pacific Islander, 0.9% American Indian or Alaskan Native, 0.9% other race, 7.8% Multiracial; mean BMI = 26.91 ± 6.11, 16.44–52.37 | Community | Eating Pathology Symptoms Inventory—Restraint subscale | Body dissatisfaction assessed with EPSI | Eating Pathology Symptoms Inventory—Binge Eating subscale | Dietary restraint did not moderate the association between body dissatisfaction and binge eating. |
| Nadel 2014 [28] | N = 383; 52.5% female; mean age = 19.30 ± 1.41; 79.1% White, 3.9% Black, 1.8% Hispanic, 14.6% Asian, 0.3% American Indian or Alaskan Native, 0.3% other race; mean BMI = 25.00 ± 5.98; 16.76–43.08 | College/university | Eating Disorder Examination Questionnaire-Restraint | Negative and positive affect assessed with the Positive and Negative Affect Schedule-X | Modified questions of the Eating Disorder Examination Questionnaire | There was an interaction between baseline restraint and daily anger, such that those with low restraint had a stronger relationship between daily anger and binge eating. There were no two-way interactions between baseline restraint and daily anxiety, daily positive affect, or daily depressive affect. No significant three-way interactions were found beween gender, affect, and restraint. |
| Pearson et al. 2018 [29] | N = 50 adults with obesity; 84% female; mean age = 43.0 ± 11.9; 76.0% White; mean BMI = 40.3 ± 8.5 | Community | One item—“I will eat less to lose weight or avoid gaining weight” | Eating expectancies assessed with one item—“If I eat this, I will feel better”; negative affect assessed with the Positive and Negative Affect Schedule | Eating episodes in which participants reported a “3” on 5-point scale for overeating and loss of control items | There was a three-way interaction between momentary restraint, negative affect, and eating expectancies, such that high levels of momentary restraint were related to binge eating only when both momentary negative affect and eating expectancies were high; low momentary restraint was generally associated with higher odds of binge eating, particularly when momentary negative affect and eating expectancies were higher. |
| Racine et al. 2009 [30] | N = 344; 100% female; mean age = 19.04 ± 1.44; 100% White | College/university | Combination of items from the Eating Disorder Examination Questionnaire—Restraint subscale and Dutch Eating Behavior Questionnaire—Restraint subscale | Impulsivity assessed with Barratt Impulsiveness Scale; serotonin genes (5-HT) | Minnesota Eating Behaviors Survey—Binge Eating subscale | There were no two- or three-way interactions between dietary restraint, impulsivity, and serotonin genes in relation to binge eating. |
| Racine et al. 2011 [31] | N = 1678 twins; 100% female; mean age = 18.87 ± 3.3; 98% White | Minnesota Twin Family Study and Michigan State University Twin Registry | Eating Disorder Examination Questionnaire—Restraint | Genetic, shared, and non-shared environmental factors for binge eating | Minnesota Eating Behaviors Survey—Binge Eating subscale | Dietary restraint did not moderate shared environmental factors for binge eating. Genetic and non-shared environmental factors for binge eating increased at elevated levels of dietary restraint. |
| Racine et al. 2017 [32] | N = 988 twins; 100% female; mean age = 16.88 ± 2.60; 80% White | Michigan State University Twin Registry | Youth Eating Disorder Examination Questionnaire—Restraint | Negative urgency assessed with UPPS Impulsive Behavior Scale | Minnesota Eating Behaviors Survey—Binge Eating subscale | Restraint did not moderate the association between negative urgency and binge eating |
| Sehm and Warschburger, 2015 [33] | N = 1039 adolescents; 49.3% female; mean age = 14.37 ± 1.56; 80% White | Community | Child Eating Disorder Examination Questionnaire—Restraint | Gender | Overeating and loss of control items from the German Eating Disorder Examination-Questionnaire for Children | There were no interactions between gender and dietary restraint in relation to binge eating vs. healthy controls or binge eating vs. elevated internalizing symptoms |
| Stice et al. 2000 [18] | N = 631; 51% female; 25 Asian, 15 Black, 498 White, 60 Latino, 7 Native American, and 26 who specified other. | High school adolescents | Dutch Restrained Eating Scale; Dietary Intent Scale | Negative affect assessed with the Positive and Negative Affect Schedule -X | Revised Bulimia Test—binge control subscale | Cross-sectionally, there were interactions between each dietary restraint measure and negative affect, such that higher negative affect strengthened the positive association between dietary restraint and binge eating; similar moderation was found for both females and males. Longitudinally, there were no interactions between each dietary restraint measure and negative affect predicting binge eating onset for either females or males. |
| Wenzel et al. 2014 [34] | N = 166; 100% female; mean age = 19.00 ± 1.21; 75.9% White, 6.0% Black, 16.7% Asian; 0.6% two or more races, 1.8% other race; mean BMI = 23.02 ± 4.16; 15% LGBTQ | College/university | Dietary Intent Scale; Three-Factor Eating Questionnaire | Negative urgency assessed with UPPS Impulsive Behavior Scale | Bulimia Test Revised | There were no interactions between dietary restraint and negative urgency in relation to bulimic symptoms. |
| Woods et al. 2010 [35] | N = 497; 100% female; mean age = 19.5 ± 0.47 | College/university | Restraint Scale | Stress assessed with the Social Readjustment Rating Scale | Eating Disorder Inventory 2—Bulimia subscale | There was a three-way interaction between restraint, daily stress, and life event stress, such that for individuals with high life event stress, restraint strengthens the association between daily life stress and binge eating. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mason, T.B.; Dolgon-Krutolow, A.; Smith, K.E. A Systematic Review of Moderators of the Association between Dietary Restraint and Binge Eating. Obesities 2024, 4, 132-144. https://doi.org/10.3390/obesities4020013
Mason TB, Dolgon-Krutolow A, Smith KE. A Systematic Review of Moderators of the Association between Dietary Restraint and Binge Eating. Obesities. 2024; 4(2):132-144. https://doi.org/10.3390/obesities4020013
Chicago/Turabian StyleMason, Tyler B., Anna Dolgon-Krutolow, and Kathryn E. Smith. 2024. "A Systematic Review of Moderators of the Association between Dietary Restraint and Binge Eating" Obesities 4, no. 2: 132-144. https://doi.org/10.3390/obesities4020013
APA StyleMason, T. B., Dolgon-Krutolow, A., & Smith, K. E. (2024). A Systematic Review of Moderators of the Association between Dietary Restraint and Binge Eating. Obesities, 4(2), 132-144. https://doi.org/10.3390/obesities4020013








