Twenty-Four-Hour Movement Behaviors, Fitness, and Adiposity in Preschoolers: A Network Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Population Characteristics
2.2. Procedures
2.3. Measurements
2.3.1. Anthropometric Measures
2.3.2. Physical Activity
2.3.3. Sleep Time
2.3.4. Screen Time
2.3.5. Physical Fitness
- Cardiorespiratory fitness (CRF) was measured using the PREFIT 20-m shuttle run test [28]. Participants completed the PREFIT 20-m shuttle run keeping in time with an audible “bleep” signal. The frequency of the sound signals was increased every minute by 0.5 km/h, increasing the intensity of the test, and the children were encouraged to run to exhaustion. Some adaptations of the original test were made by decreasing the initial speed (i.e., 6.5km/h instead of the original 8.5 km/h). Evidence for the acceptable reliability and validity of the PREFIT 20-m shuttle run test for preschoolers was previously provided [27].
- Speed–agility (shuttle run test 4 × 10 m) consisted of running and turning as fast as possible between two parallel lines (10 m apart), covering a distance of 40 m. The best of two attempts was recorded (seconds). This test had a good correlation in boys and girls (r = 0.86) [27].
- Lower-body muscular strength was assessed by the standing long jump. From a parallel standing position and with the arms hanging loose at the sides, participants were instructed to jump twice as far as possible in the horizontal direction and land on both feet. The test score (the best of two trials) was the distance in centimeters, measured from the starting line to the point where the back of the heel landed on the floor, as previously proposed [27].
2.4. Statistical Analysis
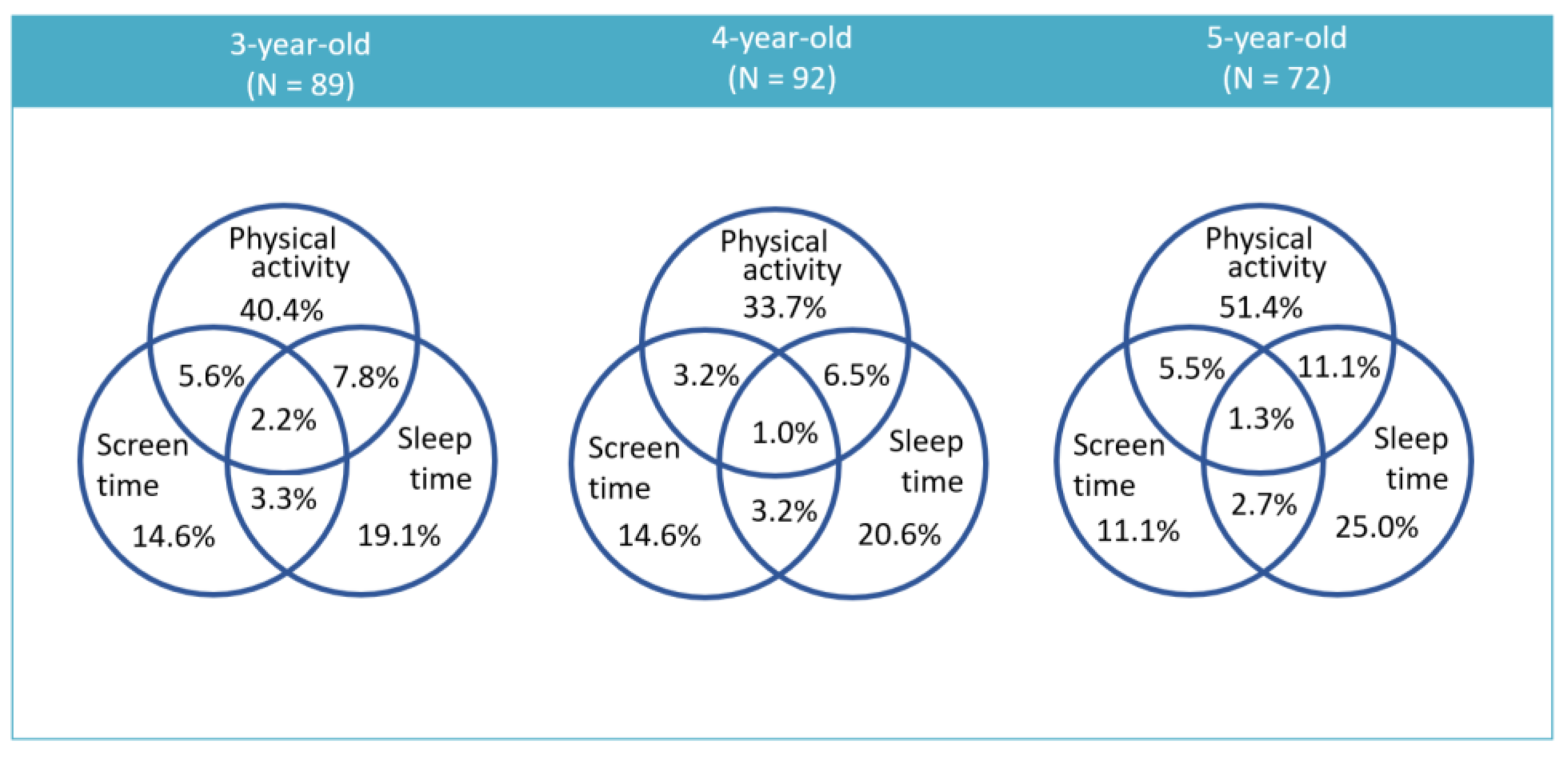
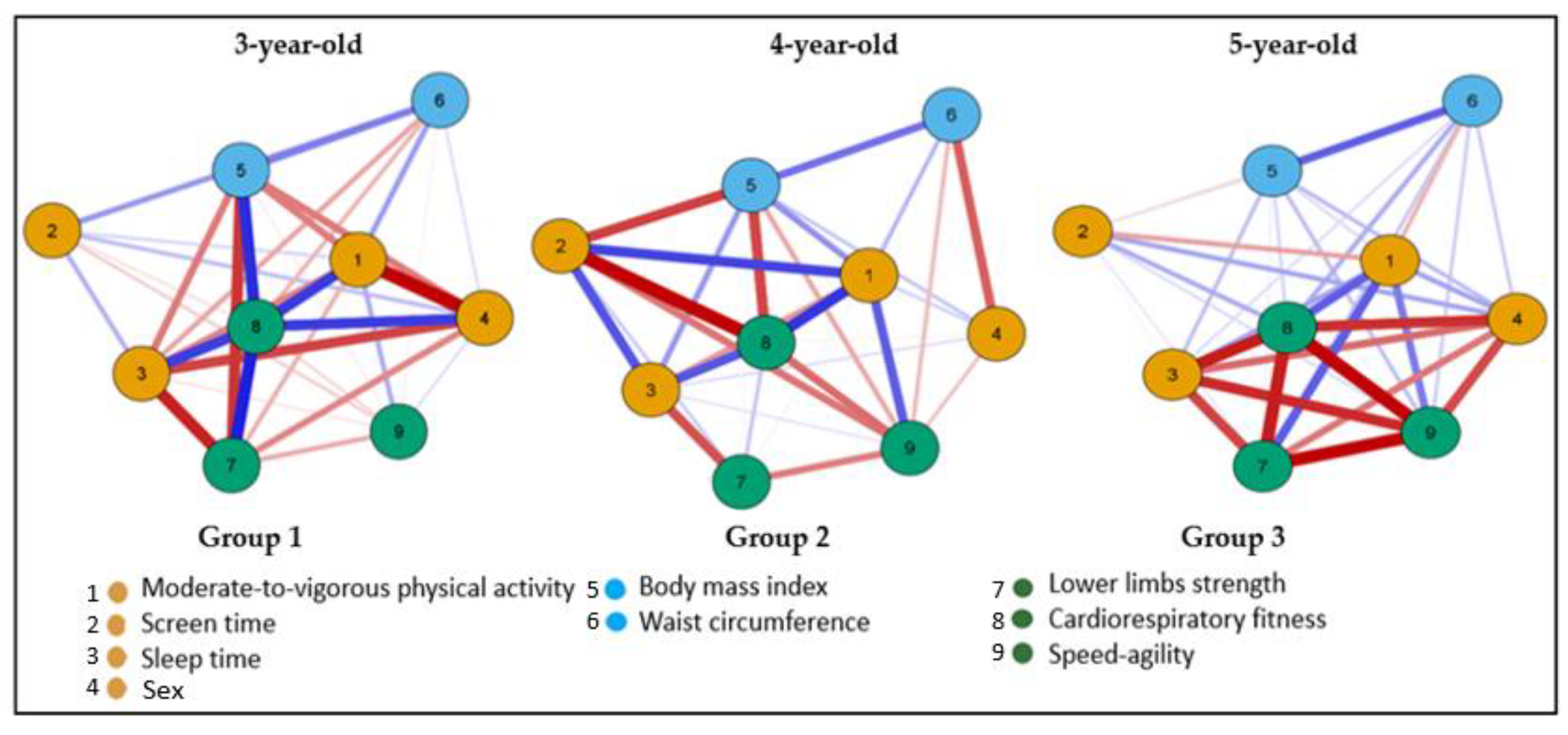
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance; World Helath Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children under 5 Years of Age; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Finkelstein, E.A.; Ruhm, C.J.; Kosa, K.M. Economic causes and consequences of obesity. Annu. Rev. Public Health 2005, 26, 239–257. [Google Scholar] [CrossRef]
- Finegood, D.T.; Merth, T.D.N.; Rutter, H. Implications of the Foresight Obesity System Map for Solutions to Childhood Obesity. Obesity 2010, 18 (Suppl. S1), S13–S16. [Google Scholar] [CrossRef] [PubMed]
- Chastin, S.F.M.; Palarea-Albaladejo, J.; Dontje, M.L.; Skelton, D.A. Combined Effects of Time Spent in Physical Activity, Sedentary Behaviors and Sleep on Obesity and Cardio-Metabolic Health Markers: A Novel Compositional Data Analysis Approach. PLoS ONE 2015, 10, e0139984. [Google Scholar] [CrossRef]
- Apovian, C.M. Obesity: Definition, comorbidities, causes, and burden. Am. J. Manag. Care 2016, 22 (Suppl. S7), S176–S185. [Google Scholar] [PubMed]
- Timmons, B.W.; LeBlanc, A.G.; Carson, V.; Gorber, S.C.; Dillman, C.; Janssen, I.; Kho, M.E.; Spence, J.C.; Stearns, J.A.; Tremblay, M.S. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl. Physiol. Nutr. Metab. 2012, 37, 773–792. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight Factsheet; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Roy, M.; Haszard, J.J.; Savage, J.S.; Yolton, K.; Beebe, D.W.; Xu, Y.; Galland, B.; Paul, I.M.; Mindell, J.A.; Mihrshahi, S.; et al. Bedtime, body mass index and obesity risk in preschool-aged children. Pediatr. Obes. 2020, 15, e12650. [Google Scholar] [CrossRef]
- Xiu, L.; Ekstedt, M.; Hagströmer, M.; Bruni, O.; Bergqvist-Norén, L.; Marcus, C. Sleep and Adiposity in Children From 2 to 6 Years of Age. Pediatrics 2020, 145, e20191420. [Google Scholar] [CrossRef]
- Tremblay, M.S.; LeBlanc, A.G.; Kho, M.E.; Saunders, T.J.; Larouche, R.; Colley, R.C.; Goldfield, G.; Gorber, S.C. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 98. [Google Scholar] [CrossRef]
- Reiff, G.; Dixon, W.; Jacoby, D.; Ye, X.; Spain, C.; Hunsiker, P. The President’s Council on Physical Fitness and Sports 1985. National School Population Fitness Survey; President’s Council on Physical Fitness and Sports: Washington, DC, USA, 1986; 107p. [Google Scholar]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef]
- Janssen, I.; LeBlanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Kelley, G.A.; Kelley, K.S.; Pate, R.R. Exercise and BMIz-score in Overweight and Obese Children and Adolescents: A Systematic Review and Network Meta-Analysis of Randomized Trials. J. Evid. Based Med. 2017, 10, 108–128. [Google Scholar] [CrossRef] [PubMed]
- Crouter, S.E.; Salas, C.; Wiecha, J. Effects of an afterschool community center physical activity program on fitness and body composition in obese youth. J. Sports Sci. 2017, 35, 1034–1040. [Google Scholar] [CrossRef]
- Reid, R.E.; Fillon, A.; Thivel, D.; Henderson, M.; Barnett, T.A.; Bigras, J.-L.; Mathieu, M.-E. Can anthropometry and physical fitness testing explain physical activity levels in children and adolescents with obesity? J. Sci. Med. Sport 2020, 23, 580–585. [Google Scholar] [CrossRef]
- Pei, S.; Wang, J.; Morone, F.; Makse, H.A. Influencer identification in dynamical complex systems. J. Complex Netw. 2020, 8, cnz029. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Carson, V.; Chaput, J.-P. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl. Physiol. Nutr. Metab. 2016, 41, S311–S327. [Google Scholar] [CrossRef] [PubMed]
- Vale, S.; Mota, J. Adherence to 24-hour movement guidelines among Portuguese preschool children: The prestyle study. J. Sports Sci. 2020, 38, 2149–2154. [Google Scholar] [CrossRef]
- Chen, B.; Bernard, J.Y.; Padmapriya, N.; Yao, J.; Goh, C.; Tan, K.H.; Yap, F.; Chong, Y.-S.; Shek, L.; Godfrey, K.M.; et al. Socio-demographic and maternal predictors of adherence to 24-hour movement guidelines in Singaporean children. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 70. [Google Scholar] [CrossRef]
- De Craemer, M.; McGregor, D.; Androutsos, O.; Manios, Y.; Cardon, G. Compliance with 24-h Movement Behaviour Guidelines among Belgian Pre-School Children: The ToyBox-Study. Int. J. Environ. Res. Public Health 2018, 15, 2171. [Google Scholar] [CrossRef]
- Martins, C.M.D.L.; Lemos, L.F.G.B.P.; Filho, A.N.D.S.; Bezerra, T.A.; Soares, I.A.A.; Mota, J.G.; Bandeira, P.F.R.; Mota, J.A.P.S.; Tassitano, R.M.; Duncan, M.J. Adherence to 24-hour movement guidelines in low-income Brazilian preschoolers and associations with demographic correlates. Am. J. Hum. Biol. 2021, 33, e23519. [Google Scholar] [CrossRef]
- Decraene, M.; Verbestel, V.; Cardon, G.; Iotova, V.; Koletzko, B.; Moreno, L.; Miguel-Berges, M.; Gurzkowska, B.; Androutsos, O.; Manios, Y.; et al. Compliance with the 24-Hour Movement Behavior Guidelines and Associations with Adiposity in European Preschoolers: Results from the ToyBox-Study. Int. J. Environ. Res. Public Health 2021, 18, 7499. [Google Scholar] [CrossRef]
- Lioret, S.; Campbell, K.J.; McNaughton, S.A.; Cameron, A.J.; Salmon, J.; Abbott, G.; Hesketh, K.D. Lifestyle Patterns Begin in Early Childhood, Persist and Are Socioeconomically Patterned, Confirming the Importance of Early Life Interventions. Nutrients 2020, 12, 724. [Google Scholar] [CrossRef] [PubMed]
- Cadenas-Sanchez, C.; Martinez-Tellez, B.; Sanchez-Delgado, G.; Mora-Gonzalez, J.; Castro-Piñero, J.; Löf, M.; Ruiz, J.R.; Ortega, F.B. Assessing physical fitness in preschool children: Feasibility, reliability and practical recommendations for the PREFIT battery. J. Sci. Med. Sport 2016, 19, 910–915. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Garza, C.; Onyango, A.; Rolland-Cachera, M.-F. WHO growth standards for infants and young children. Arch. Pediatr. 2008, 16, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Butte, N.F.; Wong, W.W.; Lee, J.S.; Adolph, A.L.; Puyau, M.R.; Zakeri, I.F. Prediction of energy expenditure and physical activity in preschoolers. Med. Sci. Sport. Exerc. 2014, 46, 1216. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. qgraph: Network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2007, 9, 432–441. [Google Scholar] [CrossRef]
- Chen, J.; Chen, Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika 2008, 95, 759–771. [Google Scholar] [CrossRef]
- Foygel, R.; Drton, M. Extended Bayesian information criteria for Gaussian graphical models. In Proceedings of the 24th Annual Conference on Advances in neural information processing systems 2010, Vancouver, BC, Canada, 6–9 December 2010. [Google Scholar]
- Robinaugh, D.J.; Millner, A.J.; McNally, R.J. Identifying highly influential nodes in the complicated grief network. J. Abnorm. Psychol. 2016, 125, 747–757. [Google Scholar] [CrossRef]
- Hesketh, K.D.; Downing, K.L.; Campbell, K.; Crawford, D.; Salmon, J.; Hnatiuk, J.A. Proportion of infants meeting the Australian 24-hour Movement Guidelines for the Early Years: Data from the Melbourne InFANT Program. BMC Public Health 2017, 17, 191–198. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Chaput, J.-P.; Adamo, K.B.; Aubert, S.; Barnes, J.D.; Choquette, L.; Duggan, M.; Faulkner, G.; Goldfield, G.S.; Gray, C.E.; et al. Canadian 24-Hour Movement Guidelines for the Early Years (0–4 years): An Integration of Physical Activity, Sedentary Behaviour, and Sleep. BMC Public Health 2017, 17, 874. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.H.; Kim, K. A review of factors limiting physical activity among young children from low-income families. J. Exerc. Rehabil. 2017, 13, 375–377. [Google Scholar] [CrossRef]
- Leppänen, M.H.; Nyström, C.D.; Henriksson, P.; Pomeroy, J.; Ruiz, J.R.; Ortega, F.B.; Cadenas-Sánchez, C.; Löf, M. Physical activity intensity, sedentary behavior, body composition and physical fitness in 4-year-old children: Results from the ministop trial. Int. J. Obes. 2016, 40, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Roman-Viñas, B.; Chaput, J.-P.; Katzmarzyk, P.T.; Fogelholm, M.; Lambert, E.V.; Maher, C.; Maia, J.; Olds, T.; Onywera, V.; Sarmiento, O.L.; et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 123. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Gray, C.E.; Poitras, V.J.; Carson, V.; Gruber, R.; Birken, C.S.; MacLean, J.E.; Aubert, S.; Sampson, M.; Tremblay, M.S. Systematic review of the relationships between sleep duration and health indicators in the early years (0–4 years). BMC Public Health 2017, 17, 855. [Google Scholar] [CrossRef]
- Kuzik, N.; Poitras, V.J.; Tremblay, M.S.; Lee, E.-Y.; Hunter, S.; Carson, V. Systematic review of the relationships between combinations of movement behaviours and health indicators in the early years (0–4 years). BMC Public Health 2017, 17, 109–122. [Google Scholar] [CrossRef]
- Martins, C.M.D.L.; Clark, C.C.T.; Bandeira, P.F.R.; Mota, J.; Duncan, M. Association between Compliance with the 24-Hour Movement Guidelines and Fundamental Movement Skills in Preschoolers: A Network Perspective. Int. J. Environ. Res. Public Health 2020, 17, 5443. [Google Scholar] [CrossRef]
- Fruchterman, T.M.J.; Reingold, E.M. Graph drawing by force-directed placement. Softw. Pract. Exp. 1991, 21, 1129–1164. [Google Scholar] [CrossRef]
- Cadenas-Sánchez, C.; Alcántara-Moral, F.; Sanchez-Delgado, G.; Mora-Gonzalez, J.; Martinez-Tellez, B.; Herrador-Colmenero, M.; Jimenez-Pavon, D.; Femia, P.; Ruiz, J.R.; Ortega, F.B. Assessment of cardiorespiratory fitness in preschool children: Adaptation of the 20 metres shuttle run test. Nutr. Hosp. 2014, 30, 1333–1343. [Google Scholar] [CrossRef] [PubMed]
| 3 | 4 | 5 | ||||
|---|---|---|---|---|---|---|
| M ± SD (N = 89) | p1 | M ± SD (N = 92) | p2 | M ± SD (N = 72) | p3 | |
| Movement behaviors | ||||||
| LPA (min/day) | 212.88 ± 49 | 0.075 | 213.55 ± 53 | 0.930 | 216.47 ± 52 | 0.893 |
| MVPA (min/day) | 54.57 ± 19 | 0.443 | 58.67 ± 18 | 0.442 | 63.01 ± 24 | 0.095 |
| TPA (min/day) | 267.45 ± 57 | 0.865 | 272.22 ± 62 | 0.740 | 279.49 ± 65 | 0.492 |
| Screen (min/day) | 169.75 ± 111 | 0.702 | 158.47 ± 83 | 0.551 | 173.99 ± 83 | 0.478 |
| Sleep (min/day) | 565.11 ± 68 | 0.791 | 558.55 ± 67 | 0.171 | 577.74 ± 68 | 0.193 |
| Anthropometrics | ||||||
| Weight (kg) | 16.37 ± 2 * | <0.001 | 18.00 ± 3 | <.001 | 19.66 ± 3 | <0.001 |
| Height (cm) | 101.13 ± 6 * | <0.001 | 106.23 ± 5 | <.001 | 112.17 ± 6 | <0.001 |
| BMI (kg/m2) | 15.96 ± 1 | 0.939 | 15.88 ± 1 | 0.475 | 15.59 ± 1 | 0.329 |
| WC (cm) | 52.15 ± 3 | 0.604 | 51.58 ± 3 | 0.935 | 50.72 ± 3 | 0.564 |
| Physical fitness | ||||||
| CRF (laps) | 19.45 ± 10 | 0.641 | 16.33 ± 9 | 0.060 | 17.50 ± 8 | 0.218 |
| Lower-body strength (cm) | 76.07 ± 22 | 0.320 | 71.3 ± 24 | 0.223 | 75.13 ± 23 | 0.127 |
| Speed–agility (s) | 10.90 ± 4 | 0.299 | 9.21 ± 3 | 0.993 | 11.54 ± 4 | 0.076 |
| Expected Influence | |||
|---|---|---|---|
| Variables | 3 | 4 | 5 |
| Physical activity | −0.213 | 2.222 | 1.310 |
| Screen | 0.596 | −0.436 | 0.577 |
| Sleep | −0.995 | 0.774 | −0.911 |
| BMI z-score | −0.498 | −0.084 | 1.260 |
| WC | 0.616 | 0.058 | 0.936 |
| Lower body strength | −0.910 | −0.495 | −0.841 |
| CRF | 2.169 | −0.481 | −0.846 |
| Speed–agility | −0.104 | −1.315 | −0.997 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Souza, A.R.; Bandeira, P.F.R.; da Silva, M.A.C.; da Cunha, G.L.; Pereira, D.F.; Martins, C. Twenty-Four-Hour Movement Behaviors, Fitness, and Adiposity in Preschoolers: A Network Analysis. Obesities 2023, 3, 36-45. https://doi.org/10.3390/obesities3010004
Souza AR, Bandeira PFR, da Silva MAC, da Cunha GL, Pereira DF, Martins C. Twenty-Four-Hour Movement Behaviors, Fitness, and Adiposity in Preschoolers: A Network Analysis. Obesities. 2023; 3(1):36-45. https://doi.org/10.3390/obesities3010004
Chicago/Turabian StyleSouza, Alyce Rodrigues, Paulo Felipe Ribeiro Bandeira, Morgana Alves Correia da Silva, Glacithane Lins da Cunha, Daniel Fernandes Pereira, and Clarice Martins. 2023. "Twenty-Four-Hour Movement Behaviors, Fitness, and Adiposity in Preschoolers: A Network Analysis" Obesities 3, no. 1: 36-45. https://doi.org/10.3390/obesities3010004
APA StyleSouza, A. R., Bandeira, P. F. R., da Silva, M. A. C., da Cunha, G. L., Pereira, D. F., & Martins, C. (2023). Twenty-Four-Hour Movement Behaviors, Fitness, and Adiposity in Preschoolers: A Network Analysis. Obesities, 3(1), 36-45. https://doi.org/10.3390/obesities3010004






