1. Introduction
Obesity affects more than 40% of US adults and will affect one in two US adults by 2030 according to recent estimates [
1,
2]. Obesity is associated with increased risk of health complications such as type 2 diabetes and cardiovascular conditions [
3]. Behavioral lifestyle modification is considered a first-line treatment for obesity [
4]. Decades of research have shown that these approaches result in approximately 5–10% short-term (i.e., less than 1 year) weight loss, which is associated with improvement in risk of related health conditions [
5]. Studies across various interventions and populations have shown that individuals expect to lose approximately 20–31% of their original body weight [
6,
7], three to four times the amount of weight loss that is most commonly achieved in a behavioral approach and that provides substantial decrease in risk [
5].
Theoretically, unrealistic expectations, along with an emphasis on achieving a specific weight loss number as opposed to other non-weight goals, are thought to lead to discouragement, frustration, and disengagement once it is clear that the unrealistic goal cannot be readily achieved, and potentially to stall weight loss [
8]. The literature so far shows mixed consequences of unrealistic weight loss expectations, and recent but limited scholarship suggests some possible negative consequences for long-term weight and psychological outcomes. Most research has focused on the consequences in terms of weight loss (e.g., % or kg lost), and has largely found that baseline unrealistic weight loss expectations are not strongly associated with less successful weight loss, particularly in the short term [
6,
7]. Though there are relatively few studies on the psychological consequences of unrealistic expectations, there is evidence of greater attrition and negative psychological consequences, such as dissatisfaction, discouragement, or depressive symptoms, due to baseline unrealistic weight loss expectations [
9,
10,
11,
12,
13,
14,
15]. Recent work has suggested that unrealistic expectations could be helpful or at least not harmful in the short-term, but ultimately may increase frustration and discouragement in the long run, leading to worse weight loss outcomes at longer time points than usually studied [
16].
As a result, some studies have explored modified cognitive behavioral therapy (CBT) interventions specifically focused on making individuals’ weight loss expectations more realistic [
17,
18]. These interventions have shown that individuals adjust unrealistic weight loss expectations downwards (i.e., more realistically) after the intervention. CBT, in general, intends to help individuals recognize their underlying motivations for weight loss, expand their understanding of acceptability and success (e.g., better energy and health and not just the number on the scale), and come to understand that the weight loss goal they have in mind may not be as important as previously thought or may be shaped by a host of other internal thoughts and feelings [
8,
17]. In contrast, other studies of standard behavioral weight loss interventions (i.e., non-CBT-based) have shown that even when individuals are informed at the start about realistic weight loss goals (5–10% at 4–6 months) or observe their weight loss progress over time, individuals still do not adjust their expectations in more realistic directions [
19].
There are several substantial gaps in the existing literature. Generally, researchers point to the need for more work on how expectations change over time during the course of weight loss, as most research has measured expectations only at baseline [
11]. More specifically, it is unknown whether individuals would adjust their expectations over time in a general CBT-based intervention addressing thoughts and feelings surrounding weight loss, rather than a modified CBT intervention heavily focused on adjusting weight expectations; as mentioned above, general components of CBT theoretically may help individuals adjust their expectations in more realistic directions. Furthermore, if individuals do adjust their expectations, the related consequences are unclear, as most research has explored the consequences of baseline expectations only. So far, then, it is unclear how adjusting weight expectations, and not just baseline expectations, relates to outcomes such as the amount of weight lost. Finally, it is unknown to what extent adjusting weight loss expectations is moderated by program engagement, or the extent to which adjustment occurs most with active engagement with CBT-based content. This helps to disentangle whether adjustment occurs due to learning principles of CBT, or whether it occurs naturally over the course of weight loss when individuals see that their goal is unachievable.
Therefore, in this prospective one-armed cohort study, the main objective was to evaluate whether individuals on a mobile CBT-based behavior-change program would significantly adjust their expectations for their weight loss from baseline to six months both in terms of the amount of weight loss (%) and the rate of weight loss change (pounds per week). We hypothesized that both would be significantly adjusted downwards (i.e., to be more realistic). Another objective was to examine whether adjustment of expectations was related to weight loss, and if so, in which direction (e.g., greater weight loss or less weight loss). We hypothesized that greater downwards (i.e., more realistic) adjustment over time would be associated with greater weight loss. An additional objective was to explore if adjustment of weight expectations, if it occurred, was moderated by engagement, and if so, which type of engagement. Based on past work [
17,
18,
19], we hypothesized that adjustment would be moderated by the amount of engagement, in which greater adjustment depends on greater engagement. Further, we hypothesized that the extent to which individuals read articles, which contain the CBT-based content, but not necessarily the amount of engagement with primarily weight-related components of the program (e.g., steps or weight logs), would be most associated with adjusting weight expectations.
2. Materials and Methods
This was a prospective cohort study in which participants participated in a commercial behavior-change program (Noom Weight) for 6 months and completed surveys at baseline and 6 months after starting the program. The study occurred remotely.
2.1. Participants
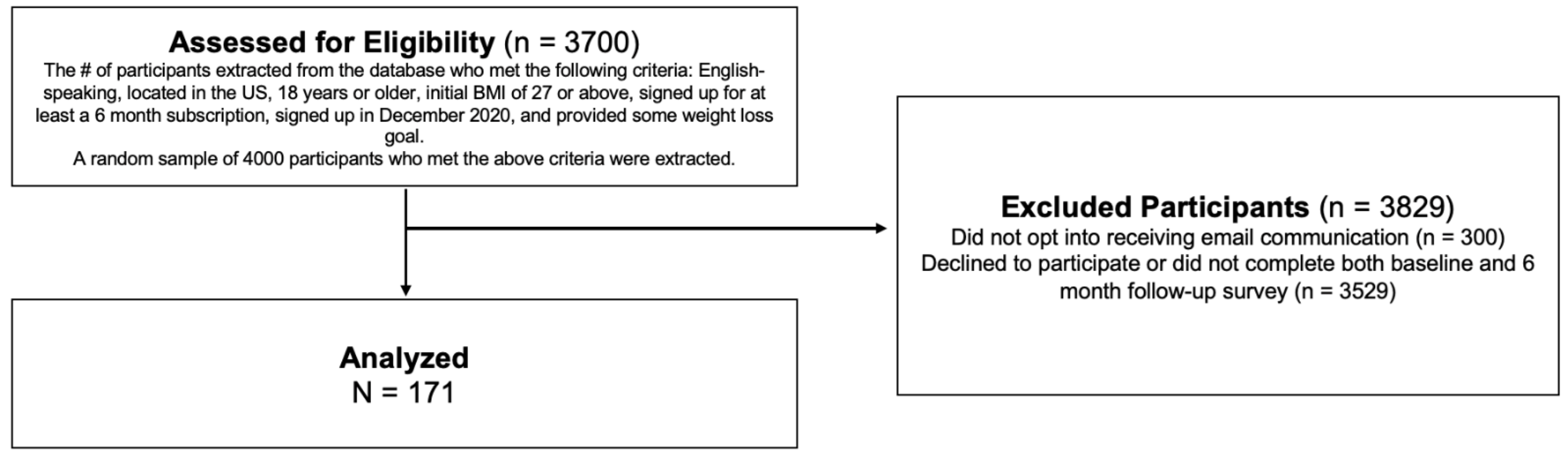
Adults who recently signed up for Noom Weight (≤three days ago) were recruited for the study in December 2020. Participants were eligible if they were located in the US, English-speaking, older than 18 years old, had a starting BMI of ≥27, signed up for at least a 6-month-long subscription, and had provided some weight loss goal at the start of the program. From the database, 4000 eligible participants were randomly chosen and invited to participate in the study, with emails sent to 3700 who had opted into receiving email communication from Noom. Eligible participants consented to participate in the 6-month prospective study in December 2020 and for their de-identified program data to be extracted after participation; all procedures were approved by the Advarra Institutional Review Board. The final sample size consisted of 171 participants who completed both the baseline survey and the 6-month follow-up survey (in June 2021; see
Figure 1). There were no significant differences in demographic characteristics between those who completed the baseline survey and those who completed both surveys.
2.2. Procedure
Participants were invited to complete the baseline questionnaire upon consenting to the study. After using the Noom Weight program for 6 months, they were invited to complete the 6-month follow-up survey. The surveys measured weight loss expectations, current weight and height, and psychological well-being. Engagement data were automatically recorded by the program.
2.3. Program
Noom Weight (NW) is a mobile commercial behavior-change program that has been shown to promote clinically significant weight loss as well as improvement of psychological factors such as self-compassion [
20,
21,
22]. NW is driven by principles of psychology based on CBT and third-wave CBT such as acceptance and commitment therapy (ACT) and dialectical behavior therapy (DBT), which aid in weight management and have positive psychological outcomes [
8,
23,
24]. NW provides daily articles founded on CBT principles that address, generally, the psychology behind behavior change and weight loss (i.e., recognizing and replacing thought distortions and the deeper reasons behind behaviors), as well as behavior change and healthy habits (e.g., fruit and vegetable intake and physical activity). In terms of topics specifically related to expectations for the amount of weight loss, there are a number of articles addressing thought patterns underlying the desire for specific weight loss goals and the “number on the scale”, or expectations surrounding sustainable and realistic behavior change. Articles help individuals understand and accept progress unrelated to the amount of weight loss, guide individuals through defining those non-scale progress indicators, and provide psychoeducation about realistic changes, especially for the amount of weight loss. For example, one article provides psychoeducation surrounding ways to define progress other than weight and examples of ways to define progress (e.g., physical: more energy; psychological: changing a thought distortion; social: compliments from others) and a space for reflection for individuals to define physical, psychological, social, and other measures of progress for their own lives. Other articles provide education surrounding biological impediments towards drastically changing weight (e.g., metabolic factors preventing large changes and maintenance of weight loss), guide individuals to reflect on their ideal weight and whether their happiness is tied specifically to that weight loss goal and ask individuals to identify goals “without looking at your weight at all”, such as “chasing after your kids without getting winded” instead of “losing 20 lbs”. Articles also define and explain thought distortions (e.g., “I will never get to X pounds” or “I have to get to X pounds”) and walk individuals through reframing them (“it’s okay not to get to X pounds − I am improving on Y”). Participants in this study received the same program and articles as the typical user who did not participate in this study. NW also provides features such as individualized coaching; weight, meal, and exercise logging to enable self-monitoring; a step counter; and in-app community groups.
2.4. Measures
2.4.1. Measures of Weight Loss Expectations
Amount of weight loss: Weight loss expectations for the amount of weight loss were measured at baseline and 6 months with the Goals and Relative Weights Questionnaire (GRWQ; [
25]), which asks for individuals’ goal weight and their perception of dream, happy, disappointing, or acceptable weights. Weight loss expectations were defined in two ways. The primary definition was individuals’ goal weight as a percentage of individuals’ starting weight (% body weight loss). The secondary definition was the average of goal, happy, disappointed, and acceptable weights (baseline α = 0.97) as a percentage of starting weight (% body weight loss). (Throughout the manuscript, “weight loss
goal expectations” or “weight loss
goal” are used to represent the weight that participants reported as their goal in the GRWQ, not their dream, happy, disappointing, or acceptable weights.) Adjustment of weight loss expectations was calculated as the change in expectations from baseline to 6-month follow-up as a percentage of original body weight. This meant that larger discrepancies between expectations and starting weight were expressed in positive values. Positive values indicated greater downward adjustment.
Rate of weight loss: Expectations for the rate of weight loss were measured at baseline and 6 months with the question, “Thinking back to your goal weight, what is the timeframe in weeks in which you plan to achieve this weight?” We used the formula weight loss rate expectation = (current weight − goal weight)/time frame.
2.4.2. Other Measures
Weight loss: Weight loss was calculated by subtracting individuals’ 6-month weight from their starting weight. Individuals self-reported their weight at baseline and 6 months on the survey.
Program engagement: Program engagement was automatically recorded by the program and consisted of the number of articles read, messages sent to a coach, exercises logged, weigh-ins, and meals logged per week. A variable indicating the total engagements per day was also recorded. In order to mirror real-world engagement, participants were not given minimum engagement requirements.
2.5. Statistical Analysis
Linear mixed-effects models [
26] were used to account for repeated measurement. As we analyzed data from those who completed both baseline and 6-month data (i.e., per-protocol), data were complete on all measures except for three missing responses to the goal expectation measure; these missing responses were excluded from analysis. To assess changes in weight loss expectations over time, mixed-effects models were conducted with time as a predictor of weight loss expectations (in percent of original body weight) and weight loss rate expectations (pounds/week). Random intercepts were specified across participants. In order to evaluate the relationship between adjusting weight loss expectations and weight loss over time, mixed-effects models were used to predict weight using the interaction of time and change in weight loss expectation from baseline to 6 months as a continuous variable. Random intercepts were specified across participants.
Finally, to assess whether (and how) weight expectations were moderated by engagement, we first ran a mixed-effects linear model predicting weight loss expectations from time, program engagement, and the interaction of time and program engagement. To further examine the effects of each engagement type on changes in expectations (i.e., whether reading the CBT-based articles, weight logging, and more were associated with adjusting one’s expectation), we conducted separate mixed-effects models predicting goal expectations from time, each type of program engagement (separately), and each time x engagement interaction. The types of engagement assessed were the number of articles read, messages sent to the coach, exercises logged, meals logged, weigh-ins, and group interactions.
3. Results
3.1. Baseline Characteristics and Weight Loss
Participants’ baseline characteristics are displayed in
Table 1. Participants began the study with a baseline BMI of 34.93 (SD = 5.77) and starting weight of 215.96 pounds (SD = 40.12). At 6 months, participants’ average weight reduced to 205.64 pounds (SD = 39.53), which constituted 4.8% weight loss. This change was significant, b = −10.32, SE = 1.33,
p < 0.001.
3.2. Change in Weight Loss Expectations
First, we investigated whether participants significantly adjusted their weight loss expectations from baseline to 6-month follow-up. At baseline, participants reported a goal to lose an average of 26.72% (SD = 13.03%) of their current weight. At 6 months, this goal significantly decreased to 18.94% (SD = 9.64%; b = −5.77, s.e. = 0.57, p < 0.001). A vast majority of the sample (80%) decreased their weight loss goal expectations. Most (62%) decreased their expectations by at least 3% of their original body weight. Furthermore, at baseline, participants expected to lose weight at a rate of 1.71 pounds per week, which significantly decreased to 1.26 lbs/week at 6-month follow-up (b = −0.53, s.e. = 0.09, p < 0.001). Overall, 73% of the sample adjusted their expectations of weight loss rate downward.
The same result occurred for dream, happy, acceptable, and disappointed weight loss expectations. At baseline, participants conceived of a dream weight loss as 30.39% (SD = 9.5%), a happy weight loss as 20.83% (SD = 9.14%), an acceptable weight loss as 17.23% (SD = 8.14%), and a disappointing weight loss as 9.42% (SD = 6.61%), with an aggregated average of 20.45% (SD = 7.41%). At 6 months, participants significantly decreased their aggregated expectations to 15.22% (b = −5.14, s.e. = 0.45, p < 0.001), which corresponded to a dream weight loss of 24.69% (SD = 10.53%), a happy weight loss of 15.89% (SD = 9.12%), and acceptable weight loss of 12.45% (SD = 8.41%), and a disappointed weight loss of 4.53% (SD = 8.05%).
Since a similar pattern was found across all indicators of weight loss expectations (i.e., goal, dream, happy, acceptable, disappointed), subsequent analyses use “weight loss goal expectations” as the indicator of weight loss expectation, as this represents individuals’ most expected weight loss (i.e., their actual goal for weight loss, in contrast to a dream or happy weight which they may not expect to actually achieve).
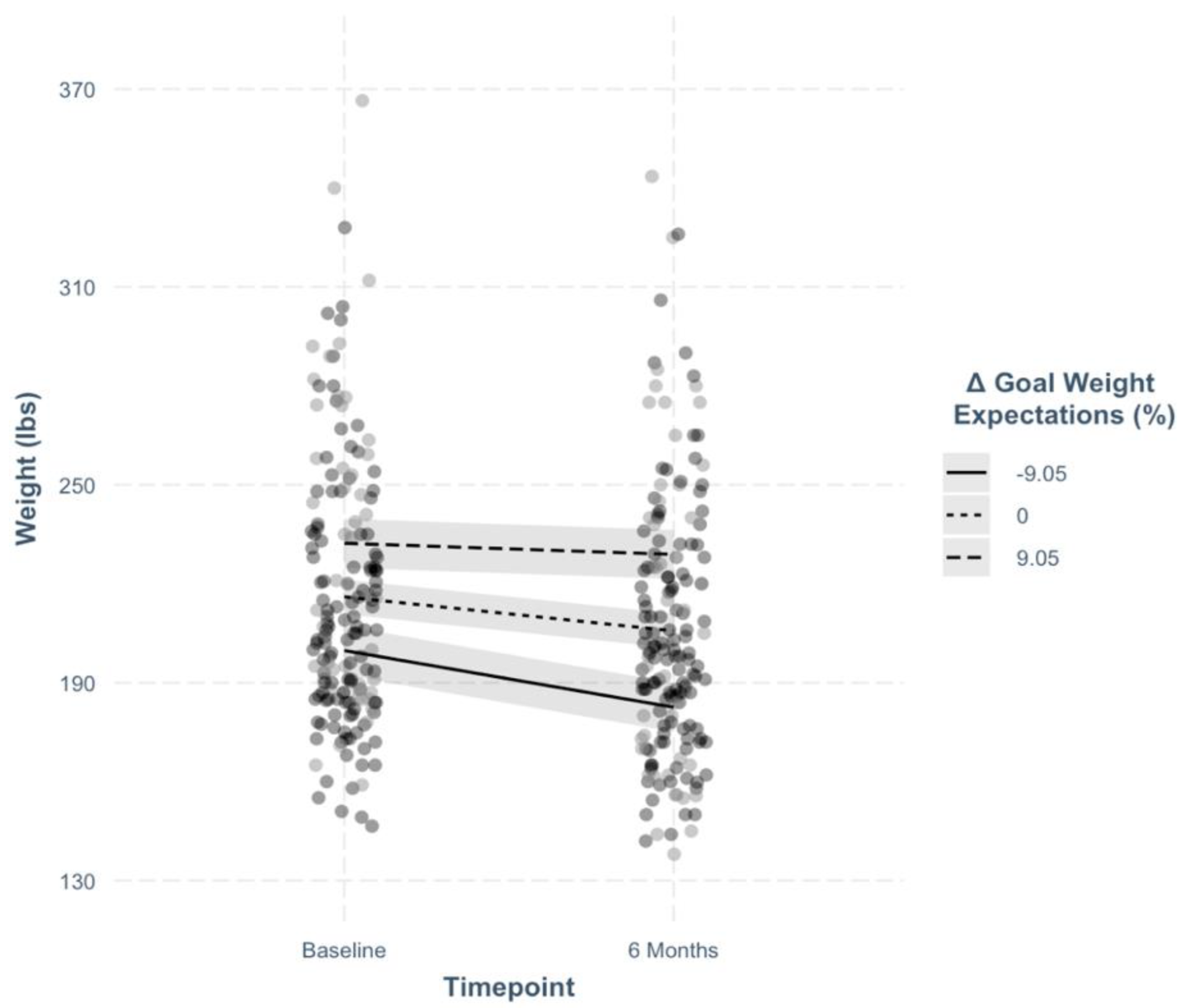
3.3. Change in Weight Loss Expectations and Weight Loss
Next, we explored whether adjustment in weight loss goal expectations was related to the amount of weight loss. Adjustment in weight loss goal expectations was calculated as a residualized change score (residuals for each participant were calculated by saving residual values from a linear regression model predicting 6-month goal weight expectations from baseline goal weight expectations. This variable is commonly called a residual change score) from baseline to 6 months and entered as a continuous variable into a mixed model predicting weight from time, change in weight loss expectation, and the interaction of time and change in weight loss expectation. The interaction between time and adjustment significantly predicted weight (
Table 2; b = 0.765, s.e. = 0.137,
p < 0.001). Simple slopes analyses revealed that weight loss was greater for participants who adjusted their expectations downward (−1SD from the mean), b = −17.22, s.e. = 1.76,
p < 0.001, compared to those who did not adjust their expectations (b = −10.30, s.e. = 1.24,
p < 0.001) or adjusted them upward (b = −3.38, s.e. = 1.76,
p = 0.06). When categorizing participants into groups who adjusted expectations downward (n = 170, 51%) vs. those who did not (n = 166, 49%), we found that those who adjusted downward lost 15.00lbs on average whereas those who did not lost 5.50 lbs on average.
3.4. Program Engagement, Weight Loss, and Expectations
Next, we explored whether weight loss goal expectations were moderated by engagement; that is, we tested whether the more participants engaged with program content, the more their expectations would change. We found that the interaction of time and overall engagement was indeed significant in predicting weight loss goal expectations. When exploring this interaction further, we found that downward goal weight adjustment was more pronounced for participants who engaged more (+ 1SD from the mean), b = −8.06, t = −10.38,
p < 0.001, compared to those who engaged less (−1SD from the mean), b = −3.59, t= −4.62,
p < 0.001 (
Figure 2).
Finally, we examined which specific type of program engagement might be associated with downward adjustment of goal expectations over time. To test this, we predicted goal expectations with time, each type of program engagement, and each time x engagement interaction in separate mixed-effects models. Only the time x articles interactions were significant for goal weight expectations (b = −0.007, t = −2.219,
p = 0.027). Downward goal adjustments were greater for participants who read more articles (
Figure 3).
4. Discussion
Researchers point to the need for more research on how weight loss expectations change over the course of weight loss, as well as on the consequences of adjusting those expectations in more realistic directions [
11]. Further, it is unclear whether significant adjustment in weight loss expectations would be found in a general CBT-based intervention. In this prospective cohort study, we found that participants began with very unrealistic expectations, as is typical, and significantly adjusted their weight loss expectations after using a generalized (i.e., not primarily focused on adjusting weight loss expectations) mobile program with principles from CBT. The study also addressed additional gaps in the literature, such as how adjusting weight loss expectations relates to weight loss and program engagement. So far, most research has been limited to how expectations at baseline, rather than changes over time, relate to weight loss [
11,
27]. The present study found that decreasing weight loss expectations was associated with greater weight loss success. Of all types of engagement on the program, reading CBT-based articles was most associated with weight loss. Overall, our results suggest that this generalized CBT-based behavior-change program helped individuals to decrease their weight loss expectations, which may then be related to better weight loss outcomes.
Participants adjusted their weight loss expectations from 27% to 19% for their goal weight loss and from 20% to 15% for their general expectations, consisting of dream, happy, acceptable, and disappointing weight losses. In particular, happy, acceptable, and disappointed weight losses decreased to 16%, 13%, and 4.5%. The majority of the sample (73%) decreased their expectations. This adjustment is similar to the amount found in CBT interventions focused on realistic weight loss expectations [
17] and is greater than the amount found in standard weight loss interventions in which participants were informed about realistic weight loss at baseline [
28]. Aligning with previous research, in the present study, participants significantly adjusted their expectations for not just their goal but all conceptions of weight loss, including the rate of weight loss, dream weight loss, and a happy weight loss. If only participants’ “goal” expectations changed, one may assume that participants realized certain amounts of weight loss were practically unrealistic or unattainable at the current moment, but their idea of satisfactory weight loss remained unchanged. Instead, the results suggest that individuals’ general conception of realistic and satisfactory weight loss changed over the course of the program.
Altering, and specifically decreasing, one’s weight loss expectations was significantly associated with greater weight loss over time. Those who decreased their expectations over 6 months lost 15 pounds on average, while those who increased their expectations or did not adjust their weight at all lost 5 pounds. This contributes important data to the mixed evidence base which shows some evidence aligning with our results but has increasingly found that unrealistic expectations at baseline are not strongly related to post-intervention weight loss or weight gain [
7,
11,
19,
27]. This discrepancy could be because these studies only measured baseline expectations. Unrealistic expectations at baseline may represent some individuals who adjusted their expectations over time and some who did not, particularly in standard behavioral interventions in which some individuals do not seem to adjust their expectations. This could lead to a null association, which is attributed to baseline unrealistic expectations, when it could actually be due to variation in adjusting expectations over time. Along similar lines, a study showed that the number of weight loss goals participants set during a program and the size of their first weight loss goal at baseline predicted better weight loss. The study ultimately argued that unrealistic expectations are more optimal for weight loss [
29]. However, it is likely that when individuals set multiple goals, they changed the goal they had previously set; otherwise, there would be no need to set another goal. Given that most individuals do not lose as much weight as they expect [
11], they likely decreased their expectations over time rather than increasing them. Therefore, it is unclear whether previous results are due to many unrealistic weight loss goals that are set and unchanged, as is their assumption, or whether adjusting weight loss goals over time in more realistic directions, as represented in multiple goals, actually relates to better weight loss. Future studies should measure adjusting weight expectations over time.
Lastly, we found that only article reading was associated with greater downward adjustment of expectations. This suggests that adjustment of expectations was most strongly linked to the components of the program derived from CBT, and that the experience of weight loss itself (e.g., tracking the weight that one has lost during the first few weeks or months and realizing it is not as much as expected) is not the main motivator to adjust expectations. This aligns with studies suggesting that CBT interventions may be more successful at changing weight loss expectations than standard behavioral interventions [
17,
19]. As stated above, CBT addresses thoughts and expectations underlying weight loss goals and what is unrealistic, and third-wave CBT such as ACT helps individuals accept undesirable states or feelings and overcome them towards valued action; these orientations, which were primarily conveyed through articles, may have helped individuals to adjust their ideas of what was realistic and to move away from needing to reach a very specific weight goal (e.g., “I have to get to 150 pounds”). Future research should extend these findings to further elucidate the role of generalized CBT on adjustment of weight loss expectations. Health professionals may consider emphasizing cognitive behavioral components of weight loss (e.g., about what is realistic, and the importance of other behavioral changes rather than the specific number on the scale), as individuals may not adjust even their realistic, practically achievable expectations for weight loss even when they track their progress over time.
Limitations. This study leveraged a unique dataset from a mobile program that participants had voluntarily signed up for and used naturally to explore real-world adjustment of weight loss expectations. However, the design has a few limitations. First, in order to measure adjustment after real-world use of a publicly available program and associated relationships with engagement, no comparison control group was used. It is unlikely that the control group would show the same degree of change given the association with engagement, especially in article reading, and adjustment of expectations, as well as previous work showing that even when individuals are informed about realistic weight loss goals, they do not readily change their expectations [
19]. However, future research should compare a CBT intervention condition to a control condition in a randomized design. Moreover, weight was measured via self-report and not objectively measured in person. The population was also highly educated, so future research should investigate how the results generalize to more representative general adult samples. Finally, the study quantitatively measured adjustment in weight loss expectations, but future research should qualitatively evaluate the extent to which individuals changed their ideas of what weight loss means, particularly in how important a weight loss number is to them and their range of acceptability of other weight loss benefits (e.g., greater energy).
5. Conclusions
Individuals typically have unrealistically large expectations for their weight loss (20–30% body weight). On a mobile CBT-based behavior-change program, individuals significantly adjusted their weight loss expectations in a more realistic direction from baseline to 6 months, which was associated with greater weight loss. Reading CBT-based program articles was related to greater adjustment of weight loss expectations. Overall, our findings suggest that generalized CBT programs can help adjust individuals’ expectations of weight loss and that such adjustment can be related to greater weight loss success. Even after this adjustment, however, goal expectations remained more unrealistic than the 5–10% weight loss benchmark, so public messaging, media portrayals, and health professionals may need to provide even clearer, more realistic expectations of weight loss, especially in the form of cognitive-behavioral understanding of weight loss. Future studies should build on this study by measuring over-time changes in weight loss expectations and a wide range of resulting consequences. Future studies should also evaluate the mechanisms at work in the relationships studied, such as changes in the importance one places on the specific number on the scale (as opposed to health in general); in autonomous motivation, leading to greater focus on deeper values; and in acceptance and self-compassion, helping one to accept themselves regardless of specifically how much weight is lost.