Abstract
Background: The Orbay approach to volar distal radius described a volar zig-zag incision across the wrist crease, allowing a more distal exposure than traditional approaches. This adaptation enhances mobilization of the proximal radial fragment and improves visualization of both the articular surface and dorsally displaced distal radius fractures. Methods: In the present paper, we propose a further modification of the volar zig-zag approach, positioning the apex of the incision at the level of the radial styloid. Results: This modification aims to improve visualization of the radial styloid, the articular comminution, and the dorsal aspect of the distal radius, thereby optimizing fracture exposure and reduction. Conclusions: The principal advantage lies in the reduced need for traction along the radial margin of the incision to achieve adequate visualization and the avoidance of crossing the wrist crease, thereby preventing the formation of unsightly or adherent scars.
1. Introduction
The evolution of volar wrist approaches for volar plating of distal radius fractures has been the focus of continuous research and refinement. The original Henry approach, along with its secondary modification [1], was the first technique described for volar plate application and remains widely utilized in clinical practice. However, these approaches are limited by the difficulty in adequately exposing intra-articular fragments, often requiring excessive traction.
In 1996, Jupiter et al. [2] introduced an extended variation in the flexor carpi radialis (FCR) approach, which traverses the FCR tendon sheath and continues distally into Henry’s approach. This modification was developed to improve visualization and facilitate reduction in fractures characterized by significant articular displacement, as well as to enable efficient release of the dorsal callus.
The conventional FCR approach provides direct access to the distal radius and the scaphoid. In 2001, Orbay et al. [3] described a volar zig-zag incision across the wrist crease, allowing a more distal exposure. This adaptation enhances mobilization of the proximal radial fragment and improves visualization of both the articular surface and dorsally displaced distal radius fractures.
In the present paper, we propose a further modification of the volar zig-zag approach, positioning the apex of the incision at the level of the radial styloid. This modification aims to improve visualization of the radial styloid, the articular comminution, and the dorsal aspect of the distal radius, thereby optimizing fracture exposure and reduction.
2. Materials and Methods
2.1. Indications/Contraindications
This surgical technique is indicated for distal radius fractures with articular involvement, including radial styloid fractures, particularly in cases presenting with multifragmentation. It is also suitable for acute traumatic fractures and early malunions, where wide exposure is required to achieve anatomic reduction.
Fracture configurations necessitating precise restoration of the articular surface represent favorable indications, especially in young and elderly patients who maintain functional independence, as well as in individuals with high functional demands or in polytraumatized patients requiring complex rehabilitation.
Radiographic criteria defining instability include angulation exceeding 15° in any plane, an intra-articular step-off greater than 2 mm, or a radial shortening of more than 2 mm. Consequently, the use of this approach is recommended in unstable fractures characterized by severe comminution, significant articular displacement, or compromised bone quality.
2.2. Surgical Technique
A skin incision is made directly over the flexor carpi radialis (FCR) tendon, extending approximately 6–8 cm. Distally, the incision continues in a zig-zag configuration, beginning at least 1.5 cm proximal to the radial styloid and directed towards it, with the apex of the “V” positioned near—but not directly over—the styloid process to prevent exposure of the radial artery. The distal tip of the “V” lies proximal to the wrist flexion crease, corresponding to the most distal course of the FCR tendon (Figure 1).
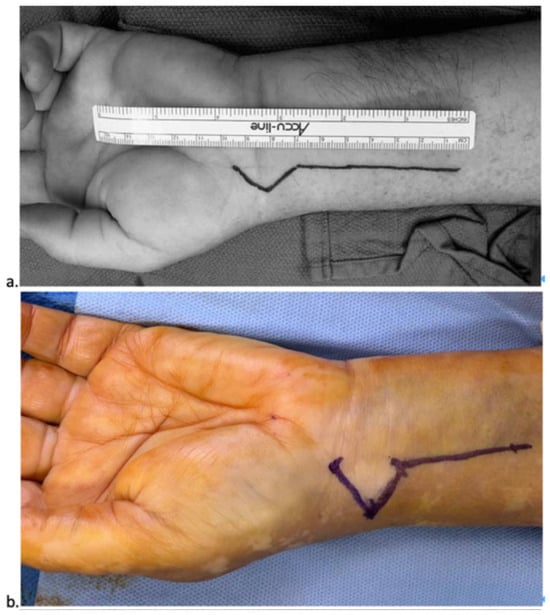
Figure 1.
(a) Orbay incision; (b) Authors modified incision.
The superficial layer of the FCR sheath is longitudinally incised, and the FCR tendon is retracted ulnarly to protect the median nerve (Figure 2). The antebrachial fascia and the deep layer of the sheath are then exposed and opened (Figure 3). Adequate proximal exposure of the sheath is essential, and the distal floor should be opened carefully to avoid neurovascular injury.

Figure 2.
Exposure of the FCR tendon.
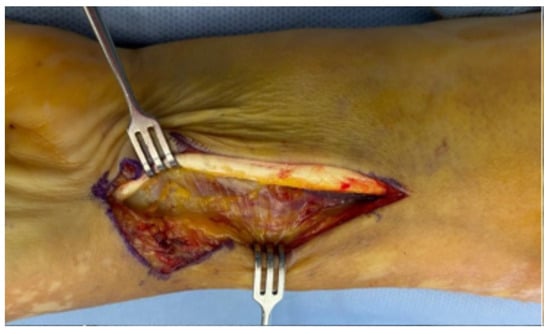
Figure 3.
Medial retraction of the FCR; exposure of the antebrachial fascia.
The flexor pollicis longus (FPL) is gently retracted ulnarly using blunt dissection and a deep retractor, allowing exposure of the pronator quadratus muscle (Figure 4). Bipolar electrocautery is frequently required at this stage due to the increased number of perforating vessels encountered. The pronator quadratus is released along its distal and radial borders through an L-shaped incision, enabling full exposure of the distal radius and the watershed line.

Figure 4.
Pronator Quadratus exposure.
Once the pronator quadratus is elevated, the anterior joint capsule becomes visible, and the brachioradialis (BR) release can be performed, providing direct visualization of the radial styloid (Figure 5). A retractor is positioned around the radial styloid to allow complete exposure of the volar aspect of the distal radius while simultaneously safeguarding the radial artery. At this stage, the first extensor compartment is also clearly identifiable.
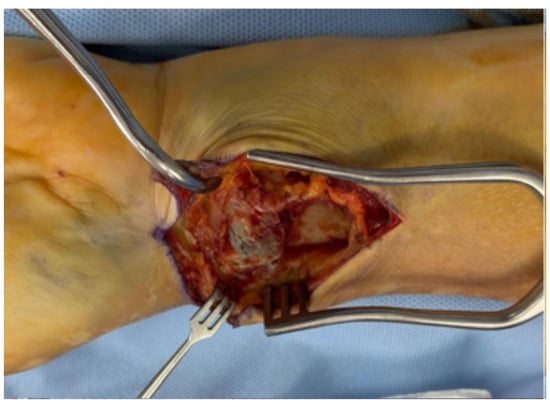
Figure 5.
Pronator quadratus incision has been carried out, and the first compartment and BR can be visualized.
During fracture exposure, meticulous dissection along the ulnar margin of the distal radius is required to achieve optimal visualization and accurate reduction of the fracture and the distal radioulnar joint (DRUJ). Frequently, fibers of the pronator quadratus are interposed within the fracture site and must be released to facilitate anatomical reduction. Reduction forceps are applied to the radial diaphysis to assist in realignment and correction of rotational deformities.
In subacute fractures, a fine elevator can be introduced between the fracture lines to mobilize the dorsal margin of the radius and release the fibrous callus. This maneuver may need to be repeated on both the radial and ulnar columns depending on fracture morphology. When dorsal continuity cannot be restored solely through the volar approach—as in early malunions or fibrous callus formation—the proximal radial fragment can be mobilized in pronation with a bone-holding forceps to complete dorsal exposure.
A complementary elevator may be used to mobilize distal fragments, facilitating reduction maneuvers to correct dorsal and radial tilt under fluoroscopic guidance. This method is also effective in reducing impacted fragments.
Reduction of the radial styloid is achieved primarily through longitudinal traction on the thumb, using a Kirschner wire as a joystick to achieve and maintain anatomical alignment. In cases requiring direct reduction, this approach permits excellent visualization of the articular fragments of the styloid. A free elevator can be employed to restore contact between the styloid and proximal radius before definitive fixation.
The volar plate is then positioned according to standard variable-angle principles. Additional fixation of the radial styloid may be achieved using one or two 3.0 mm headless screws inserted percutaneously or, alternatively, with a dedicated radial styloid plate. The pronator quadratus is then re-approximated to cover the plate, minimizing the risk of flexor pollicis longus irritation. Final fluoroscopic images are obtained to confirm reduction and hardware placement (Figure 6).
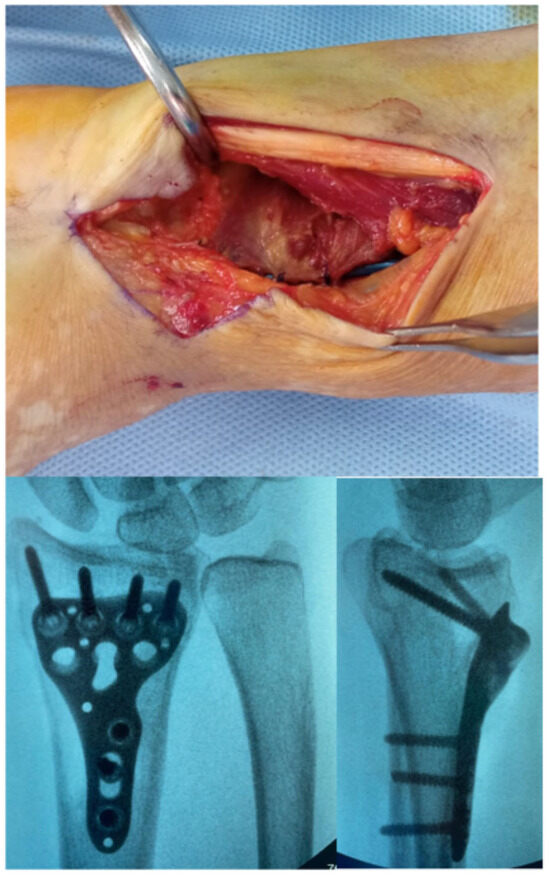
Figure 6.
Final closure of the Pronator Quadratus and post operative X-ray control.
A volar plaster splint is applied postoperatively below the elbow, leaving the metacarpophalangeal joints and fingers free.
2.3. Rehabilitation
Postoperative rehabilitation begins immediately with active motion of the fingers, elbow, and forearm rotation. On postoperative day 15, sutures are removed, and a short thermoplastic splint is applied by the physiotherapist to relieve symptoms. At this stage, gradual resumption of hand use for daily activities is encouraged.
2.4. Expected Outcomes
Typically, patients are able to flex their fingers sufficiently to touch the palm within the first postoperative days, as finger motion exercises are initiated while still in the plaster splint. Patients who fail to begin early mobilization and present with greater stiffness generally require a more intensive physiotherapy regimen.
Under physiotherapeutic supervision, patients follow a standardized protocol to initiate active wrist mobilization by intermittently removing the splint several times a day. Concurrently, passive wrist mobilization is introduced with the assistance of the therapist to progressively improve the range of motion.
At approximately four weeks postoperatively, follow-up radiographs are obtained to assess fracture alignment and healing. Upon confirmation of adequate bone consolidation, patients are advised to discontinue splint use and gradually resume normal hand function. The duration of immobilization and subsequent withdrawal of the splint are tailored according to the radiographic evidence of union and the individual patient’s clinical progression.
3. Results
The authors have been employing this approach for more than three decades, with its application in over 3000 cases of distal radius fractures. With careful surgical execution, most complications can be effectively avoided. Notably, the use of this technique has not been associated with any complications involving the flexor tendons.
Complications described in the existing literature—such as dorsal tendon irritation caused by excessively long screws—are independent of the surgical approach itself. Consequently, the risk profile of this technique is comparable to that reported in previous studies and can be minimized through accurate intraoperative fluoroscopic projections and adherence to established preventive measures [4,5].
During exposure of the radial styloid, the radial artery remains at potential risk; however, this can be effectively protected by avoiding placement of the distal limb of the incision directly over the styloid and by utilizing a small retractor for arterial shielding.
A rare complication encountered was a transient neurapraxia of the superficial branch of the radial nerve, likely resulting from excessive traction on the radial margin of the incision. This event was self-limiting and resolved completely, consistent with the anatomical course of the nerve, which does not directly intersect the surgical field of this approach.
4. Discussion
In contrast to Orbay’s original zig-zag approach [3], which traverses the wrist flexion creases, the authors propose a modified version in which the apex of the “V” is positioned near the radial styloid (Figure 1). This modification provides superior exposure of the radial styloid compared with Orbay’s method. By directly aligning the apex over the styloid process, the surgeon achieves immediate visualization of this structure without the need for excessive traction on adjacent soft tissues. Consequently, the radial artery—although clearly visible—is effectively protected, as it remains outside the direct operative field and is shielded from potential iatrogenic injury caused by surgical instruments.
The principal advantage of this modification lies in the reduced need for traction along the radial margin of the incision to achieve adequate visualization. A secondary advantage is the avoidance of crossing the wrist crease, thereby preventing the formation of unsightly or adherent scars. Scars extending across the flexion crease can act as tethering points, potentially impairing wrist flexion–extension and delaying postoperative rehabilitation and wound healing.
The brachioradialis (BR) release can be performed under direct visualization in the same manner as the reduction of the radial styloid. The first extensor compartment is clearly identifiable, and placement of a radial plate—typically considered technically challenging—is facilitated through the insertion of two retractors on the radial side, allowing optimal bone exposure not achievable with other approaches.
This technique also permits direct access to the articular surface and effective manipulation of intra-articular fragments, while maintaining clear visualization of both the radial and ulnar borders of the distal radius. After volar plating, this exposure provides a comprehensive view of the joint margins and the proximal distal radius, thereby reducing the number of intraoperative fluoroscopic checks required to ensure accurate plate positioning.
The approach additionally facilitates the disimpaction of fracture fragments and the removal of hematoma or fibrous callus. Interestingly, intraoperative findings have shown that the presence of a hematoma may sometimes assist fracture reduction through a ligamentotactic effect.
In cases of comminuted fractures that remain stable under fluoroscopic control following volar fixation, dorsal stabilization is generally unnecessary. For large distal articular fragments, distal screws acting as a buttress are sufficient to restore dorsal tilt and radial length. Only in rare instances of residual instability after volar fixation is a secondary dorsal approach required.
This report presents a technical description based on the authors’ extensive clinical experience; it does not include formal clinical outcome analysis or statistical validation.
Author Contributions
Conceptualization, G.L. and A.P.; writing—original draft preparation, C.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Conti Mica, M.A.; Bindra, R.; Moran, S.L. Anatomic considerations when performing the modified Henry approach for exposure of distal radius fractures. J. Orthop. 2016, 14, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Jupiter, J.B.; Fernandez, D.L.; Toh, C.L.; Fellman, T.; Ring, D. Operative treatment of volar intra-articular fractures of the distal end of the radius. J. Bone Jt. Surg. 1996, 78, 1817–1828. [Google Scholar] [CrossRef] [PubMed]
- Orbay, J.L.; Badia, A.; Indriago, I.R.; Infante, A.; Khouri, R.K.; Gonzalez, E.; Fernandez, D.L. The Extended Flexor Carpi Radialis Approach: A New Perspective for the Distal Radius Fracture. Tech. Hand Up. Extremity Surg. 2001, 5, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Ljungquist, K.L.; Agnew, S.P.; Huang, J.I. Predicting a safe screw length for volar plate fixation of distal radius fractures: Lunate depth as a marker for distal radius depth. J. Hand Surg. 2015, 40, 940–944. [Google Scholar] [CrossRef] [PubMed]
- Cha, S.M.; Shin, H.D. Detections of Screw Penetration during Volar Plating for Distal Radius Fractures. J. Wrist Surg. 2017, 06, 340–348. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).