1. Introduction
Recent advancements in implant dentistry have reported that immediate implant placement in the esthetic zone replacing upper anterior incisors is preferable compared to late placement [
1]. This approach offers several notable advantages over delayed placement, including the preservation of existing soft and hard tissue volumes, reduction in the number of surgical steps, and enhanced esthetic outcomes [
2,
3]. However, rehabilitating this anterior esthetic zone presents a series of unique challenges due to the presence of limited bone, soft tissue, and the proximity of anatomic structures, such as the nasopalatine canal, also called the incisive canal (IC).
The IC, located at the midline, posterior to the maxillary central incisor teeth, is an important anatomic structure of this area. The nasopalatine nerve and the terminal branch of the nasopalatine artery pass through this canal [
4]. Previous studies report that perforation or insertion of implants into the IC may lead to contact of implants with nervous tissue and cause non-osseointegration or lead to neurovascular bundle injury and sensory alteration [
5,
6].
Clinical guidelines for immediate implants in the maxillary esthetic zone suggest that an ideal outcome requires a minimum buccal bone thickness of 1–2 mm, with the implant engaging 4 to 5 mm of bone apico-palatal to the root apex and positioned more palatally, thereby minimizing stress on the buccal bone [
7,
8,
9]. Buccal bone dimensions are important for long-term soft tissue stability and aesthetic outcome, and the palatal bone is essential for implant engagement and achieving primary stability [
10]. In clinical practice, however, proper restoratively driven implant position is often challenged due to the proximity and morphology of the IC and thin buccal bone below the recommended 2 mm of width [
11,
12,
13].
The available palatal bone and proximity of the IC to the roots of the central incisors direct the position of an implant [
13]. This apico-palatal region is considered equally critical as buccal bone thickness [
14]. Therefore, proximity of the IC should be considered when assessing the incisor and surrounding bone during the diagnostic and planning phases. Despite the International Team for Implantology’s consensus on the importance of sufficient palatal bone volume, there remains a lack of detailed research on the specific relationship between palatal bone parameters, the central incisor, and the IC [
7,
14].
Cone beam computed tomography (CBCT) has been used extensively in dentistry because of its ability to produce adequately accurate two- and three-dimensional images [
15]. Linear measurements made from CBCT images were not significantly different from the actual direct measurements of anatomic structures in the dento-maxillofacial area [
15,
16,
17].
The primary objective of this study is to investigate the proximity of the incisive canal to the apex of the maxillary central incisor root and the surrounding palatal and buccal bone width in the Korean population. In this investigation, we employed CBCT to provide detailed and accurate three-dimensional imaging, and the results were used to assess the implications and considerations for immediate implant placement in this region.
This study aims to contribute to the field of oral surgery by quantifying the spatial relationship between the IC and the apical region of the maxillary central incisors in a Korean population using axial CBCT imaging. It provides essential data for immediate implant planning, particularly highlighting gender and anatomical variations.
2. Materials and Methods
2.1. Study Design
CBCT data of patients who underwent examination for oral surgery and implantology purposes of an implant-prosthetic rehabilitation dental therapy at the Gangnam Dental clinic, 415 Gangnam-daero, Seocho-gu, Seoul, South Korea, were collected between June 2024 and September 2024 with informed consent provided. Data were analyzed by one of the authors (Y.S.K.) at Unicamillus International University, who performed the statistical analyses. The local ethical committee approved the retrospective study with protocol number E00332-2024.
The CBCT data of a total of 94 patients comprising 48 men and 46 women were selected. The samples were grouped into male or female and then into 3 different age groups: A. 20–39-year-olds; B. 40–59-year-olds; and C. 60–79-year-olds. Exclusion criteria from the samples were missing maxillary anterior teeth (from canine to canine), severe crowding in the region, severe periodontitis, infection or pathology at the region of interest, wearing of orthodontic appliances, indication of root resorption or resection of apex, and any distortion or artifact in the image at the region of interest.
2.2. Acquisition of CBCT Imaging
All CBCT data were obtained using a Vatech CBCT equipment (Green CT 2, Vatech Co, Hwaseong, Republic of Korea) with the following parameters: 7.9 mA, 94 kV, 9.0 s exposure time, 0.2 mm voxel size, and a field of view of 160 × 900 mm. CBCT data were saved in the Digital Imaging and Communications in Medicine (DICOM) format, and the images were viewed and measured using Ez3D Plus professional CBCT software (Vatech Co., Hwaseong, Republic of Korea). The slice interval was 0.2 mm, and the slice thickness was 0.00 mm in reconstructed sagittal images and axial images. Each image was examined to identify fully formed, intact permanent central upper incisors 11 and 21 for analysis.
2.3. Data Measurement
All measurements were performed by a single investigator (Y.S.K.). All CBCT measurements were performed by the same calibrated examiner. Reliability tests were performed to check the consistency and accuracy by repeating the measurements of the maxillary incisor of 10 random patients among the samples in a 2-week-period. The Dahlberg formula was used to calculate method errors [
18]. The method errors ranged from 0.21 to 0.68.
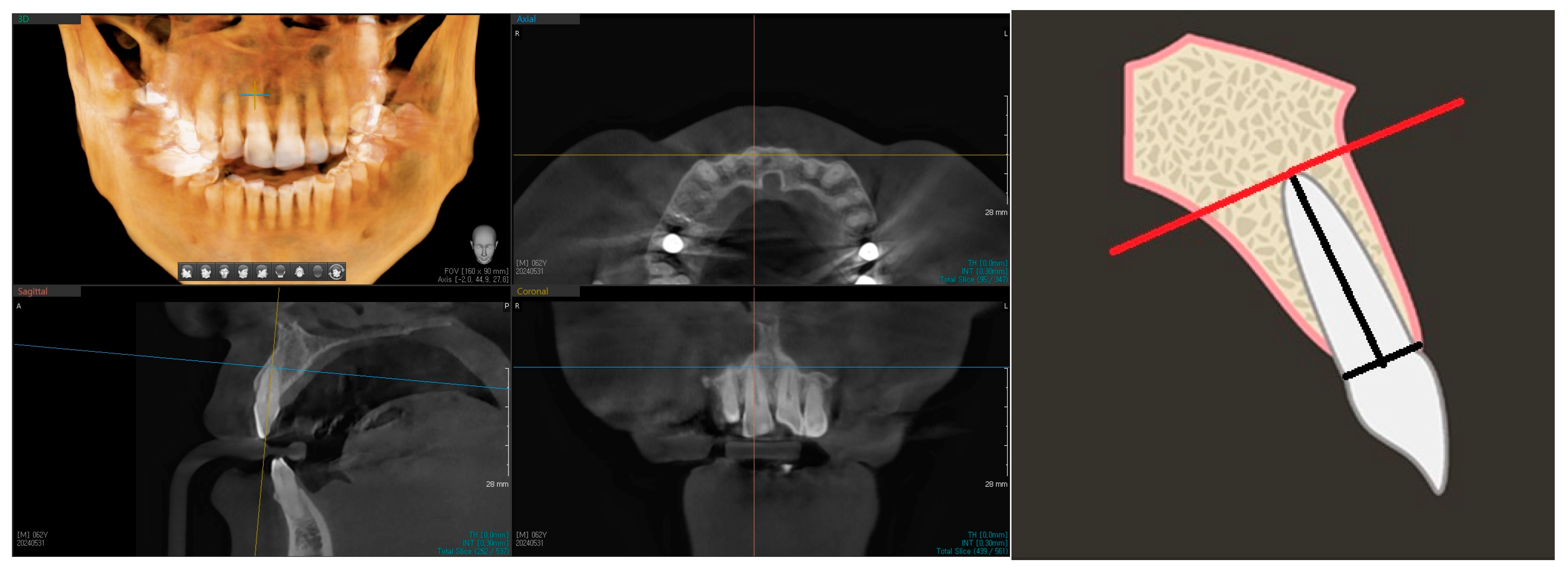
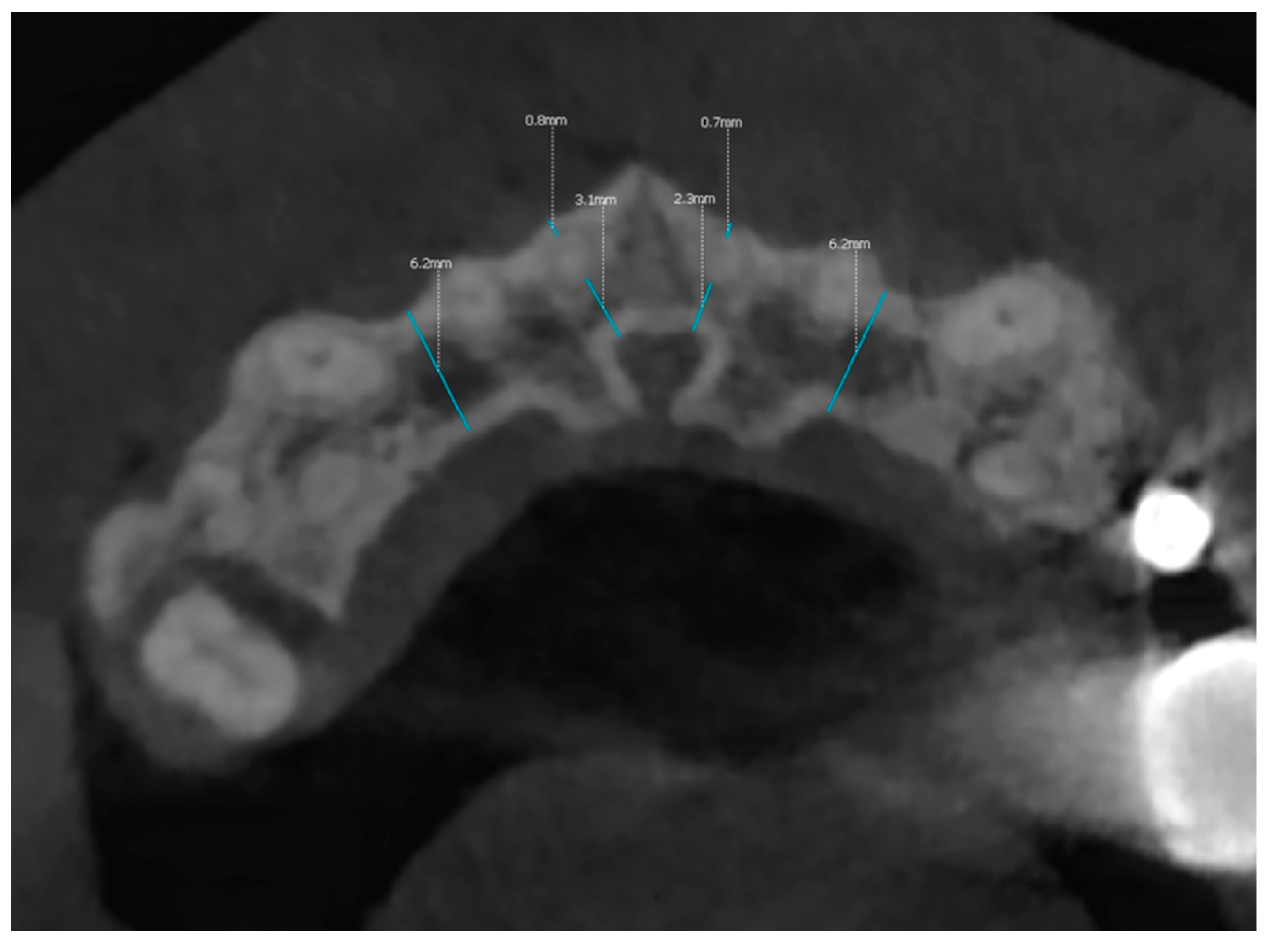
Landmarks (central incisor root apex, anterior IC wall, and buccal alveolar bone) were identified and marked in the software before the measurements were performed. The sagittal section of the chosen incisor was viewed at the center of its mesial-distal dimension (
Figure 1). The long axis of the tooth was marked by the midpoint of the line drawn from the buccal enamel–dentine junction to its palatal counterpart, the apex of the root. The long axis of the tooth root, instead of the long axis of the whole tooth, was used because the range of the crown-root angle is known to be 25.5 degrees for maxillary central incisors [
16,
17]. From this reference line, a perpendicular line was drawn from the apex of long axis of the root, spanning from the anterior border of the incisive canal toward the buccal bone surface (
Figure 2).
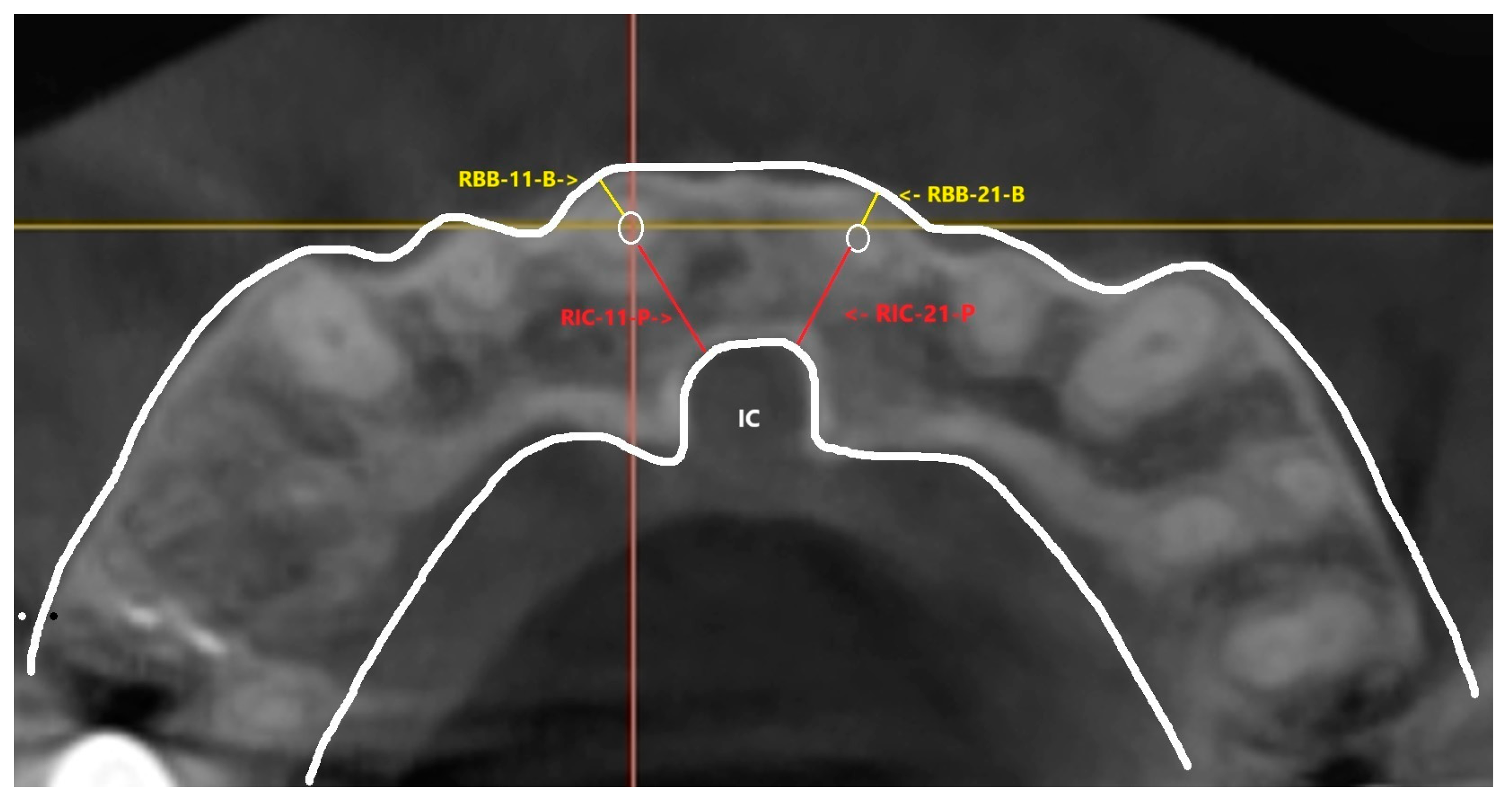
This perpendicular line was transferred to the axial slices of the CBCT image to set the axial slices horizontal to this reference. From the axial slices where root apex of central incisors are located, linear measurements of the shortest distance between the IC and each maxillary central incisor root apex were performed, defining thickness of the available palatal bone—marked as RIC-11-P and RIC-21-P for right central incisor 11 and the left central incisor 21, respectively. Shortest distance between each central incisor root apex and the buccal bone border was measured, defining thickness of the buccal bone at the apical level—marked as RBB-11-B and RBB-21-B for right central incisor 11 and the left central incisor 21, respectively. (
Figure 3 and
Figure 4) Similar linear method of measurement on axial slices of CBCT was observed in a study by Ishii T et al., 2023 [
19].
The root apex, along with the perpendicular plane extending from the root apex to the IC, was selected as the reference for the axial or horizontal plane in this study. This choice was made because the root apex serves as a clear and clinically relevant landmark, and the palatal bone can be easily distinguished from the labial bone at the level of root apex with visualization of the apex point [
14]. This can also be easily identified by clinicians during the planning and surgical setting.
By orienting the CBCT measurements from this axial plane, the study effectively simulates the clinician’s perspective during implant placement in the maxillary central incisor region with root apex as a clear landmark where measurements were based. The axial plane was preferred over the sagittal plane due to the latter’s limited view of the incisive canal and root apex, as there can be variations in IC shapes and sizes and tilting and curvature of roots [
20].
This approach ensures more accurate and clinically applicable measurements, aligning with the real-world conditions faced by dental practitioners during implant placement.
Although it might be worthwhile information, we purposely did not include the measurements of the buccal and palatal bone thickness at the crestal region because of the uncontrollably high percentage of error owing to its relative thinness. Although magnification is possible in the computer, the resolution will be too low for measurement. Moreover, a beam hardening effect is always present over the edge, making measuring the bone thickness at the crestal level worthless.
2.4. Statistical Analysis
All measurements were performed by a single investigator (Y.S.K.). Reliability tests were performed to check the consistency and accuracy by repeating the measurements of the maxillary incisor from 10 random patients. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS, Chicago, IL, USA). For the comparison of two sets of data, a Welch’s t-test was used. For comparison of three or more independent sets of data, an “analysis of variance” (ANOVA) test was used. Pearson Correlation analysis was conducted, and correlation coefficient was used to describe the statistical correlation. The level of statistical significance was set at 0.05.
3. Results
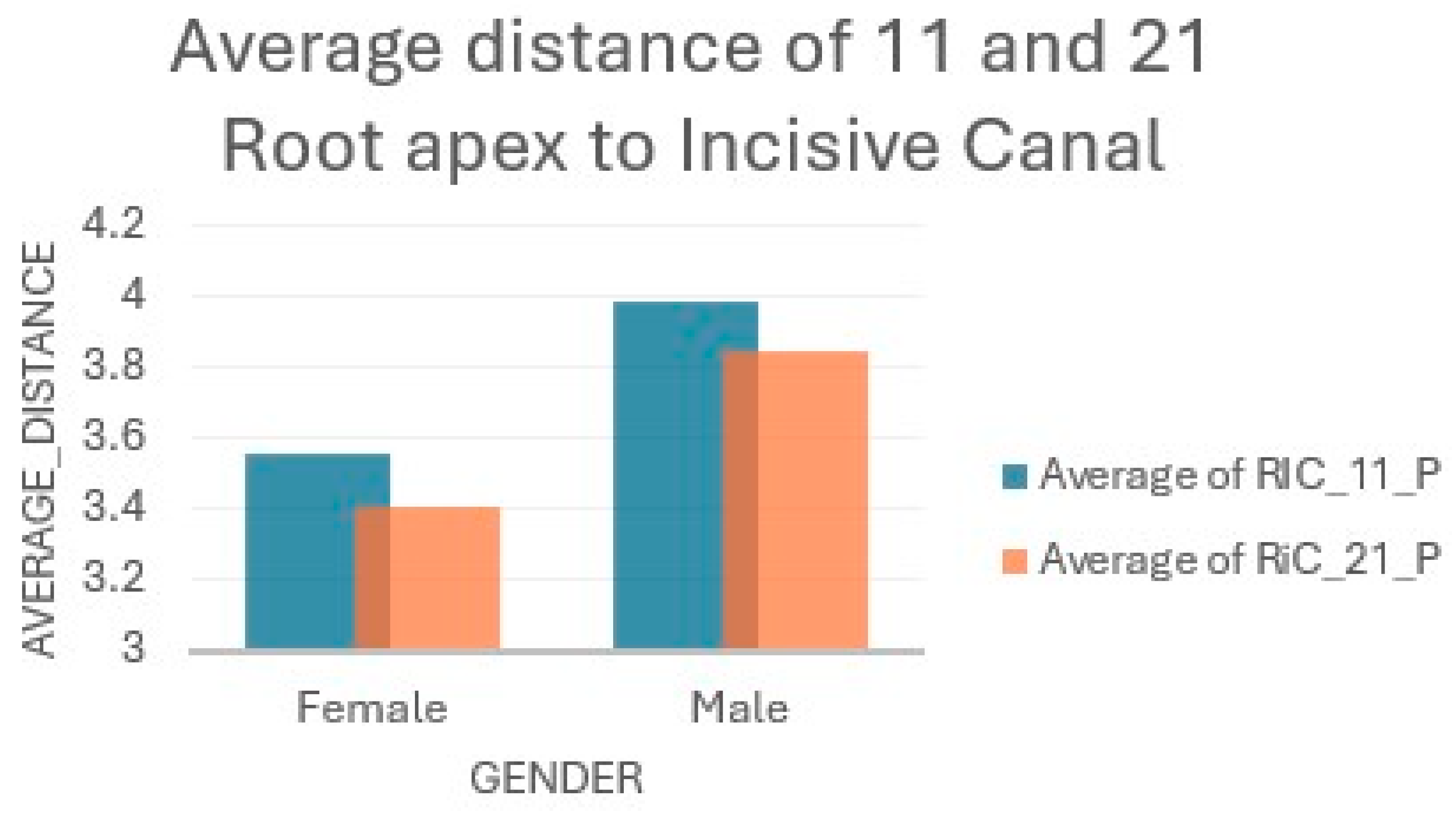
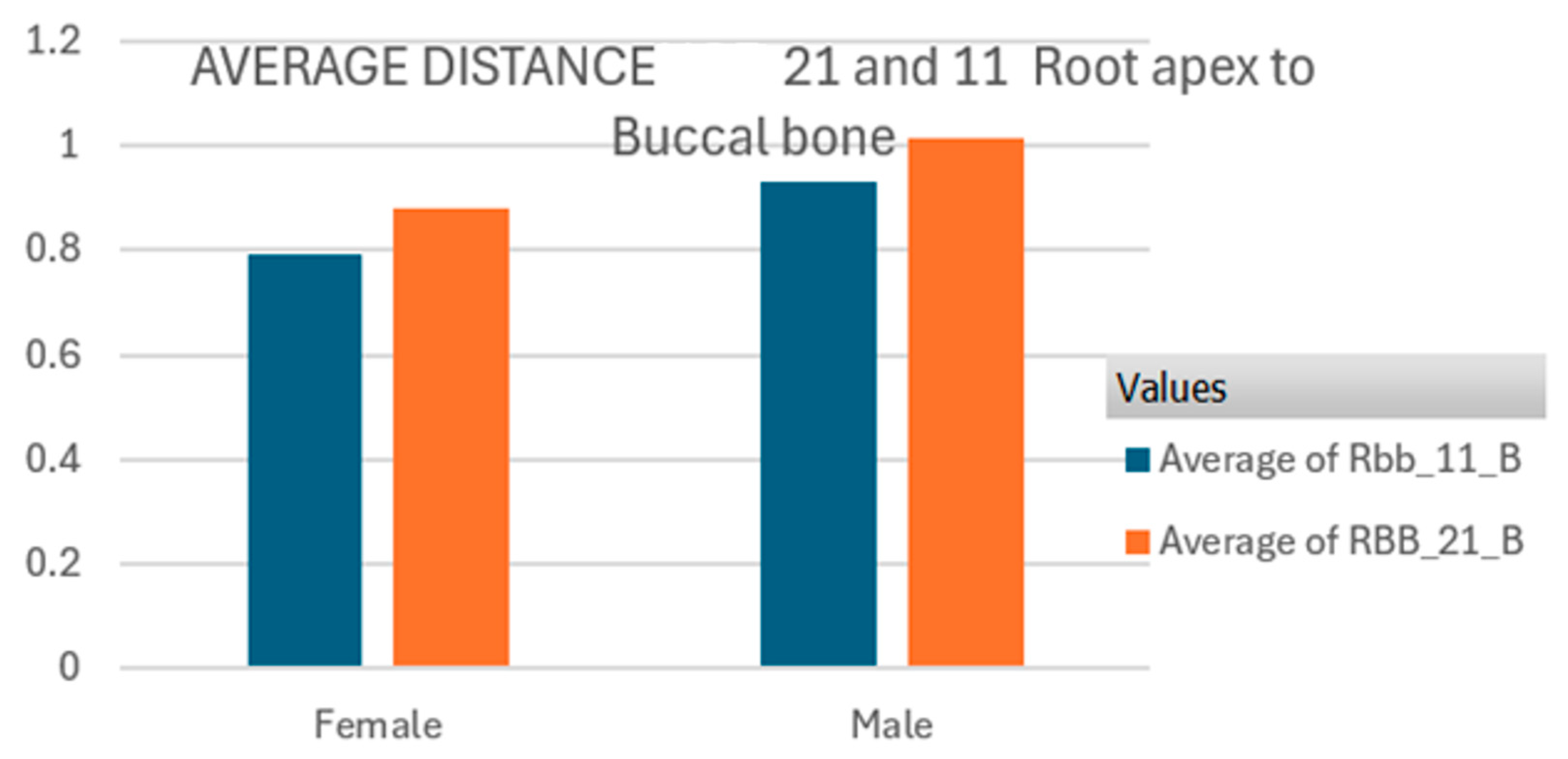
The overall sample mean distances for RIC-11-P (root apex to incisive canal for maxillary right central incisor 11) and RIC-21-P (root apex to incisive canal for maxillary left central incisor 21) were 3.77 mm, std 1.07, and 3.62 mm, std 0.99, respectively. The mean RBB (root apex to buccal bone) distances for maxillary right incisor 11 and maxillary left incisor 21 were 0.86 and 0.94, respectively (
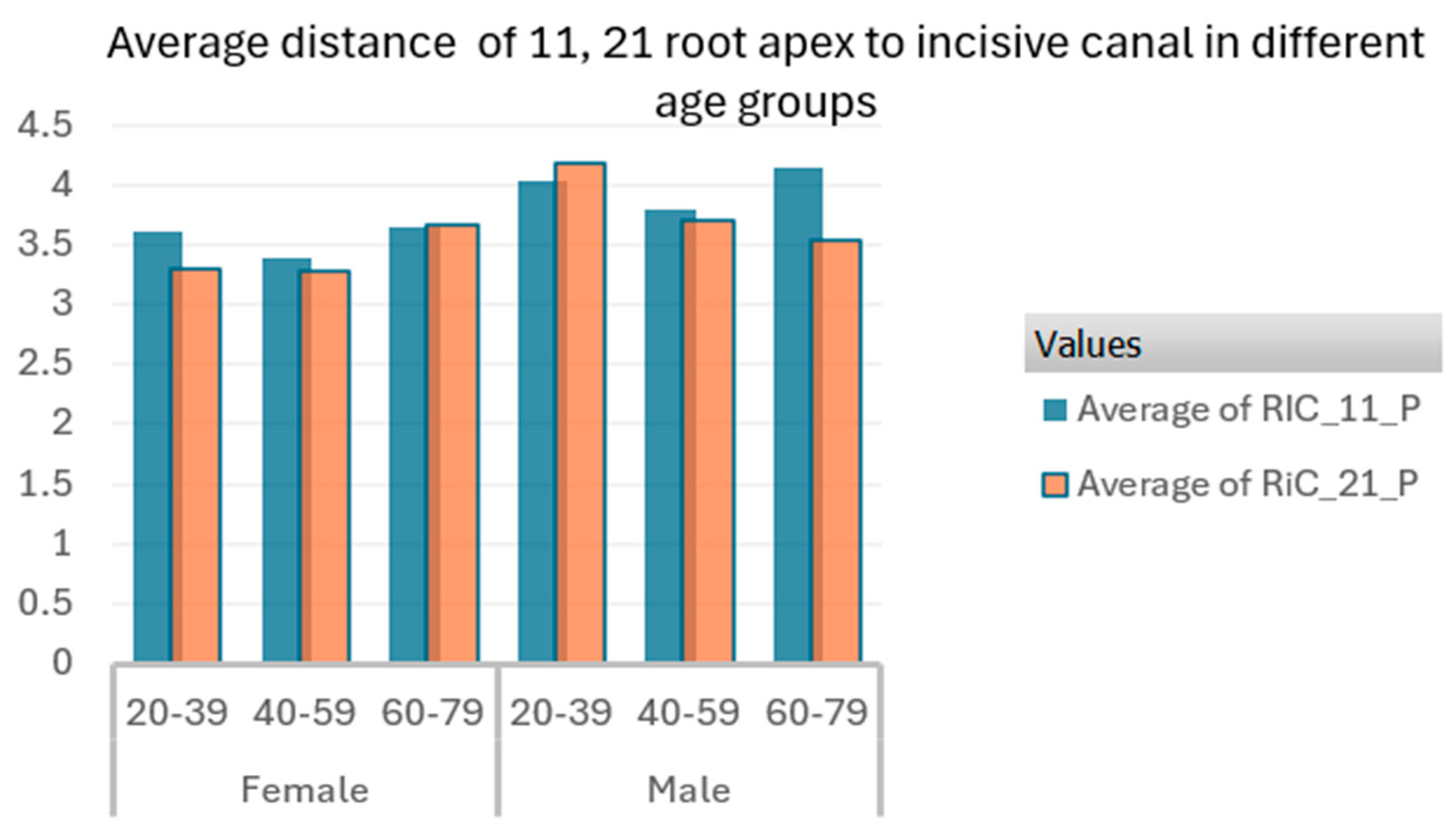
Table 1). Men demonstrated greater mean distances in both incisors than women, according to the
t-test, with a significance level of
p < 0.05, as shown in
Table 2 and
Figure 4 and
Figure 5.
The age of patients ranged between 20 and 79 years, with a mean age of 46.47 ± 17.5.
Figure 4.
Average distance (mm) from root apex of 11 (RIC-11-P) and 21 (RIC-21-P) to incisive canal in female and male patients.
Figure 4.
Average distance (mm) from root apex of 11 (RIC-11-P) and 21 (RIC-21-P) to incisive canal in female and male patients.
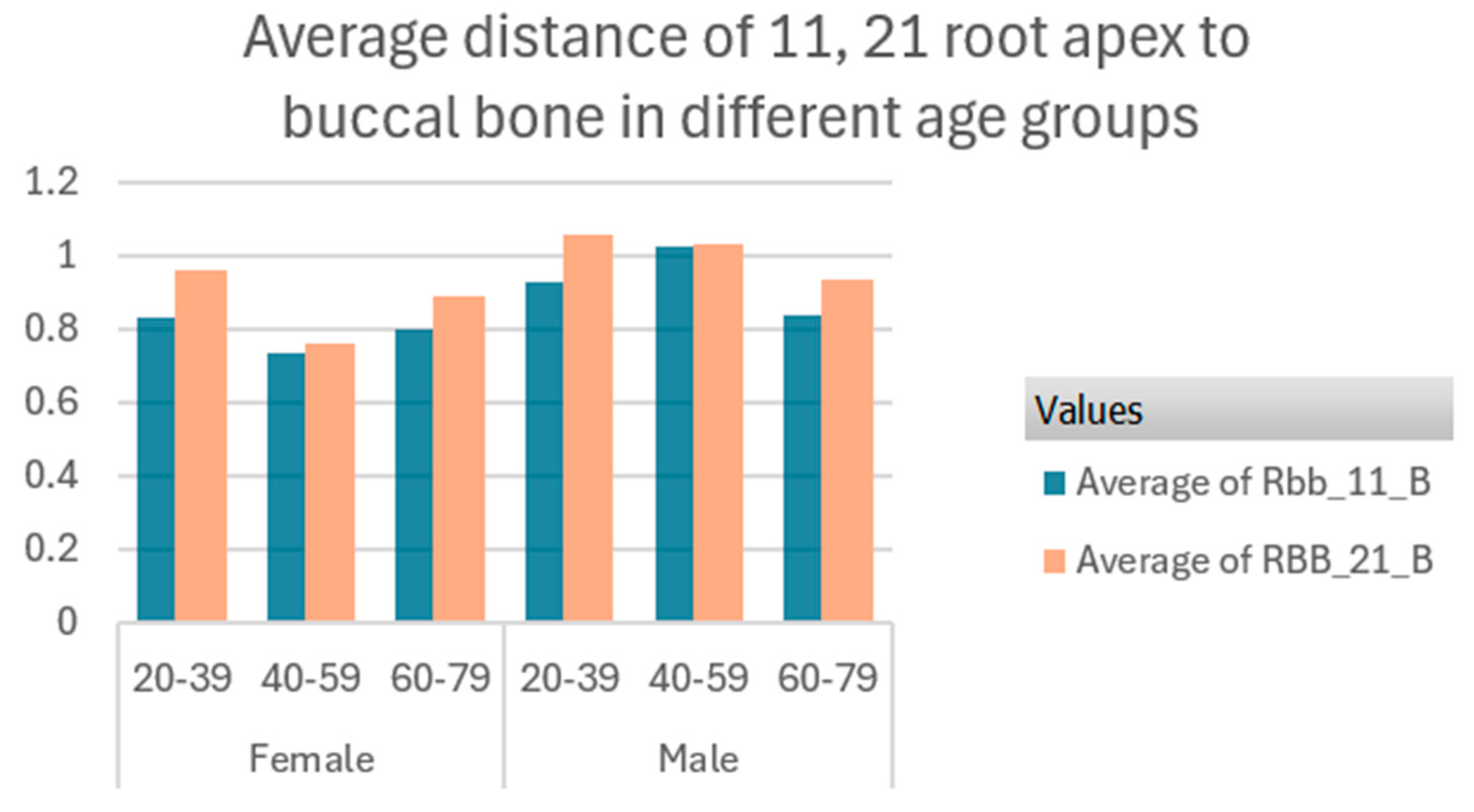
Figure 5.
Average distance (mm) from root apex of 11 (RBB-11-B) and 21 (RBB-21-B) to buccal bone in female and male patients.
Figure 5.
Average distance (mm) from root apex of 11 (RBB-11-B) and 21 (RBB-21-B) to buccal bone in female and male patients.
The Welch’s t-test was performed to compare the mean average value for the distance from the root apex of 11 and 21 to the incisive canal (RIC-11-P and RIC-21-P) for male and female participants in the population. This test was repeated for the mean average for the distance between the root apex of 11 and 21 to buccal bone (RBB-11-B and RBB-21-B) for male and female patients. The results show that the mean average values are not equal for both males and females at a confidence level of 0.05, since our p-value for the test is less than 0.05. Males clearly have higher mean distances for both root to incisive canal and root to buccal bone than females.
A Pearson correlation test was conducted to determine if there is a link between gender and these measurements (RIC-11-P, RIC-21-P, RBB-11-B, RBB-21-B). The results reveal that there are positive associations between gender and these distances, with correlation coefficient being positive and in low figures for RIC-11-P at 0.02156358 and RIC-21-P at 0.221028314. The correlation coefficients between gender and the distances from the root to the buccal bone (RBB_11_B and RBB_21_B) were 0. 254252344 and 0. 255508454, respectively, supporting the link between gender and these measurements, i.e., males tend to have greater distances from the root tip to both the incisive canal and the buccal bone compared to females.
In females, the average distance for 11 root apex to incisive canal (RIC-11-P) in the age group (20–39 years) was 3.61 mm; for the age group (40–59 years), it was 3.39 mm, and for the elderly group (60–79 years), it was 3.65 mm. For males, it was 4.02 mm, 3.78 mm, and 4.15 mm for the age groups (20–39 years), (40–59 years), and (60–79 years), respectively. The average distance of 21 root apex to incisive canal (RIC_21_P) was 3.30 mm, 3.27 mm, and 3.66 mm for the age groups (20–39), (40–59), and (60–79), respectively, in the female gender and 4.17 mm, 3.70 mm, and 3.53 mm for age groups (20–39), (40–59), and (60–79), respectively, for the male gender (
Figure 6). The distance shows a slight increase in the means in the male population in most age groups.
Figure 7 shows that the average distances from the upper central incisor 11 root apex to buccal bone (RBB_11_B) are 0.8333 mm, 0.7357 mm, and 0.8 mm for the age groups (20–39), (40–59), and (60–79), respectively, for the females. In males, this is 0.926 mm, 1.0267 mm, and 0.8357 mm in ages (20–39), (40–59), and (60–79), respectively. For the left central incisor 21 root apex to buccal bone (RBB_21_B), the average distance is 0.9611 mm, 0.764 mm, and 0.8929 mm in females for the ages (20–39), (40–59), and (60–79), respectively, and 1.0578 mm, 1.0333 mm, and 0.9357 mm for the ages (20–39), (40–59), and (60–79), respectively.
The analysis of variance was used to compare the mean average distance from the root apex to the IC and the buccal bone for different age groups, (20–39), (40–59), and (60–79), at a significance level of 0.05. The results for RIC-11-P and RIC-21-P show that the p-value (0.654) is much greater than the significance level of 0.05, failing to reject the null hypothesis. This suggests that there is no statistically significant difference in the mean distances measured across the six age groups based on this data. These values show that the calculated F-statistic (0.661) is less than the critical F value (2.264), confirming that there is no significant difference between the group means at the 0.05 significance level.
Similar results were obtained for the ANOVA test performed for average distance between the root apex and the buccal bone (RBB-11-B and RBB-21-B) in different age groups. The p-value (0.107) is greater than the significance level of 0.05, and the F-statistic (1.842) is less than the critical F value (2.264), confirming there is no marked difference between the age groups in the mean distance from the root apex to the buccal bone.
In other words, the mean distances for these age groups are not significantly different from each other.
The correlation between the age groups and the root apex-to-IC distance was calculated using a matrix. Correlation between RIC_11_P and Transform_age_group (0.020355652): This value indicates a very weak positive correlation between the RIC_11_P distance and the age group. This weak correlation suggests that age has little to no impact on the distance of RIC_11_P, as the coefficient is very close to zero. Correlation between RIC_21_P and Transform_age_group (−0.070519491): This coefficient shows a weak negative correlation between the RIC_21_P distance and age. Although the correlation is weak, the negative sign implies that as age increases, there is a slight tendency for the distance of RIC_21_P to decrease. However, the weak value indicates that age is not a strong predictor of this distance.
The age group shows negative correlation with RBB-11-B and RBB-21-B, with correlation coefficients of −0.091550606 and −0.1599506, respectively. This means that age is correlated with RBB_11-B and RBB-21-B, and as the age increases, both upper central incisors 11 and 21 root apexes tend to be closer to the buccal bone. However, the negative coefficient values are too weak to claim that there is a strong correlation.
Lastly, a Pearson correlation test was performed on the overall mean distances from the incisor root tip to IC and from the root tip to buccal bone of the population.
There is a negative correlation between the root-to-buccal bone (RBB_11_B) distance and the root-to-incisive canal (RIC_11_P) distance, which is −0.03893335; this means that with an increase in the root-to-buccal bone (RBB_11_B) distance, there will be a negative effect on the distance of RIC_11_P. In the same way, there is a negative correlation (−0.0494404) between the root-to-buccal bone (RBB_21_B) distance and the root-to-incisive canal (RIC_11_P) distance; this means that increasing the distance of root to buccal bone has an inverse effect on the root-to-incisive canal (RIC_21_P) distance. In other words, a greater palatal bone width (distance between the incisor root apex and the IC) is generally associated with a reduced buccal bone width, reflected in a shorter distance between the root apex and the buccal bone.
4. Discussion
This study examined the spatial relationship between the incisive canal and the root apex of the maxillary central incisors to analyze the thickness of the buccal and palatal bone in the Korean population using CBCT imaging. The results of the study were further analyzed to assess the implications for immediate implant placement in the esthetic zone. The results were compared to similar studies conducted in other populations to better understand the potential variability in anatomical features critical for treatment planning and clinical procedures.
For our sample of the Korean population, the mean distances between the maxillary central incisor root apex and the IC were 3.77 mm for the right central incisor 11 and 3.62 mm for the left central incisor 21. Furthermore, the distances between the root apex and the buccal bone were 0.86 mm and 0.94 mm for upper right central incisor 11 and left central incisor 21, respectively. The IC was closer to the left central incisor 21, having a shorter distance. Men exhibited greater distances compared to women in both the width of palatal and buccal bone. Many other previous studies on different populations and ethnicities showed varying results when compared with the present study. A previous study in the Korean population by Cho and co-workers reported a higher average measurement of 4.9 mm for the width of palatal bone between the root apex and IC and 1.18 mm for the buccal bone width [
19]. In a recent Japanese study where they studied 157 patients, the distance between the apex and the IC was approximately 3.3 mm, which is more in line with our results [
20]. This study was also consistent with our finding of the left incisor root apex being closer to the incisive than the right central incisor. However, there are contradicting studies that showed that the incisive canal was closer to the right central incisor [
21,
22]. A study involving a more multiethnic population by Alkanderi and collaborators reported a similar average palatal bone (3.25 mm) between the root apex and the IC and showed a strong association between male gender and greater distances [
23]. Also, a Saudi Arabian study showed a higher mean value (4.28 mm) of the width of palatal bone between the same landmarks as our study (root apex of maxillary central incisor to IC), and males tended to have larger distances and bone dimensions in this region [
24].
The majority of the literature on palatal bone width at the apical level of upper central incisors showed much larger average values ranging from 5.06 mm to -7.43 mm compared to our results [
14,
16,
25]. The reason for this would be the use of sagittal view rather than axial slices of CBCT to measure the palatal bone width where the IC may not be visible, and their measurement parameter did not include IC. Gender-based difference was also present in this study, where palatal bone width was larger in male patients than in female patients.
According to our investigation on the Korean population, the distance between root apex and the buccal bone was 0.86 mm and 0.94 mm for upper right central incisor 11 and left central incisor 21, respectively. They were found to be less than 1 mm in width, which is often the minimum recommended value when planning for immediate implant placement. Men had a higher average than women. A previous Korean study by Jung et al. showed the average buccal bone width at the apex of the central incisor root to be 1.18 mm—slightly higher than our findings; however, 58.3% of the examined central incisors had a buccal bone width less than 1 mm [
26]. This study also looked at the incisor root position in relation to the buccal bone width, and the majority of the samples had a root position close to the buccal plate and a thin buccal bone width. A study by Lau et al. on the Hong Kong population revealed a slightly higher mean value of 2.04 mm, but when the distribution of the width was analyzed in detail, more than half of the sample (51.8%) had a thickness of less than 2 mm [
16]. However, these comparable studies used sagittal sections to measure the distance between the root apex and the buccal bone, hence resulting in slightly higher average figures than our axial slice measurements. However, consistency across the populations suggests that buccal bone is generally thin and commonly less than 1 mm in many cases. The finding that males have a thicker buccal bone compared to females from our study was consistent with the results from other studies [
27,
28].
The average palatal and buccal bone widths from the current study were smaller when compared to many other previous studies, and there appear to be variations among different populations and ethnicities with no characteristic patterns when compared. Males having larger palatal and buccal bone width in this apical region of central incisors was consistent across other previous studies. This difference might be explained by the compensatory or remodeling phenomenon of bone induced by a greater physiologic load in male subjects, resulting in greater distances between the root apex and the incisive canal [
27]. These findings are consistent across different ethnic groups, suggesting that sexual dimorphism in the maxillary bone surrounding IC is a common trait.
The impact of age on the palatal and buccal bone width was less pronounced in our study, and similar results were shown from other comparable studies, having no significant association [
25,
27]. The analysis of variance (ANOVA) conducted in this study showed that there were no statistically significant differences in the mean distances from the root apex to the IC and the buccal bone across different age groups. This suggests that, despite slight variations in means, age does not have a significant impact on the spatial relationship between the maxillary central incisor root and these anatomical structures. The correlation between age and these measurements was not consistent across all parameters, indicating that factors other than age may play a role in determining these distances.
However, there are studies that claim the maxillary labial bone thickness decreases with age, and Zhang et al. 30 reported that the labial bone was thinner in elderly women [
28,
29,
30]. These variations from studies and literature could be due to ethnic differences in craniofacial morphology, as well as lifestyle and physiologic factors that influence bone density and thickness. The Pearson correlation analysis in the current study revealed a negative correlation between age and the distance from the root apex to the buccal bone (RBB-11-B and RBB-21-B). Although the correlation coefficient was weak, this could lightly reflect that as individuals age, the root apex tends to be closer to the buccal bone, which could have implications for implant placements in older patients. These results and reflections suggest that clinicians should be aware of the possibility of thin labial bone thickness, especially in elderly female patients.
In the esthetic zone, the success of immediate implant placement requires a sufficient amount of buccal bone for soft tissue architecture and palatal bone apical to the root socket for primary implant stability. When the maxillary central incisors are involved, it is vital that their proximity to the IC be considered during treatment planning and clinical procedure. The measurements allow quantification of maxillary bone anterior to the IC as a prerequisite for dental implant positioning [
31].
The literature suggests that the initial drill should be placed at the palatal bone beyond the mid-to-apical level of the socket due to the bone plate being thicker than 2 mm in this region anterior to the IC [
32].
The implant typically begins to engage with the socket walls around the middle of the root area of the extraction socket on the palatal side toward the apico-palatal bone between the apex and IC, further extending 4 mm beyond the apex [
25,
27]. The average palatal bone width, 3–3.5 mm, from our study quantifies the available bone and, in turn, the overall direction of the implant engagement. The closeness of the IC to the root apex of maxillary incisors guides how an implant should be placed [
33]. Our current data suggest that there is sufficient bone for the implant engagement in this region without risking interfering with the IC and the overall direction of the implant engagement. This aligns with the recommended palatal engagement concept from the literature, as the available bone is greater in the apico-palatal region than the buccal bone.
Although our results and previous studies have shown that the average IC-to-root distances at the apex levels generally appear adequate for implant engagement without risking interference with the IC, it is important to note that smaller distances were frequently observed in the samples (1–2 mm). Similar results were mentioned in the study by Chatriyanuyoke et al., with their lower end of data for distance from IC to root apex ranging from 1.01 to 2.00 mm. Care should be taken when assessing the bone anterior to the IC, as the proximity to the IC may be much higher in some cases, and variations exist [
27]. Given these considerations, tapered implants are recommended for maxillary central incisor placements, as they require less bone for apical engagement and have been shown to provide better primary stability compared to cylindrical implants [
26,
27,
31,
32,
33]. Jia et al. demonstrated a perforation rate of 16.7% in a Chinese population following virtual implant placement in dentate and partially edentulous patients [
34]. However, this perforation rate was reduced to 8.3% when tapered implants were selected instead of parallel fixtures.
The thickness of the buccal bone is another critical factor that influences the success of immediate implant placement [
35,
36,
37]. This study revealed that the buccal bone thickness is less than 1 mm, the recommended minimum required for implant placement.
The correlation analysis showed that where more palatal bone was available between the root apex and the IC, the buccal bone thickness on the other side of the root tended to decrease. A systematic review by Chen and Buser reported a high frequency of gingival recession with bone resorption in the immediate implant in this region, as a thin labial cortical plate is prevalent in the maxillary aesthetic zone [
1]. Although the recommended guideline for placing the implant is towards the palatal bone to avoid over compressing the buccal bone, severe tilting of the implant towards the buccal bone should be avoided, and care should be taken not to slip and perforate the implant towards the thin and vulnerable buccal plate [
25,
32,
38].
Age had no influence on the width of buccal bone in this study, but gender differences were observed, where men had thicker buccal bone compared to women. The findings underscore the importance of gender considerations in treatment planning, as the thinner buccal bone in women could pose challenges for immediate implant placement. The buccal bone width is generally thin, being less than 1 mm in this population and in many other previous studies [
25,
27,
36,
37]. It implies that additional measures, such as a bone graft procedure, may need to be considered as part of the default treatment planning for immediate implant placement in this aesthetic region.
The consistency of gender differences in both the RIC and RBB distance from the current study and across different studies reflects the importance of considering sex as a critical factor in implant treatment planning. However, the variability in age-related changes and buccal bone thickness between populations suggests that clinicians should be cautious when generalizing findings from one population to another and highlights the need for personalized treatment planning. In particular, the thinner buccal bone and palatal bone near the IC observed in women may necessitate the use of additional surgical techniques, such as bone grafts, augmentation of the IC, and modifications in implant design, to achieve optimal outcomes [
39].
Moreover, this study’s use of axial view images for measurements, rather than the more commonly used sagittal views, provides a different perspective on the anatomical challenges faced during implant placement. The axial view allows for the identification of the shortest distances, which can be crucial in determining the feasibility of implant placement without encroaching on the IC [
27].
It is worth noting that the measurements from this study could also be valuable for planning orthodontic treatments, particularly those involving significant retraction of the upper central incisors to improve soft tissue and occlusal relationships. Many studies in orthodontics have focused on determining the distance between the upper central incisor root apex and the IC. Understanding this distance is crucial for minimizing the risk of root resorption, which can occur if the root encounters the IC during treatment; the management of soft tissue, bone resorption, and provisional prosthesis is important too [
20,
21,
40,
41].
This study was conducted in a single center, which is a potential limitation. The scans included in our study were already stored in the practice database. The study results can only be generalized to the patients who visited the Gangnam dental practice in Seoul, Korea, a private dental practice, and thus may not be representative of the general population of Korea.
It is important to highlight that the measurements in this study were taken from axial view images, rather than the sagittal views commonly used in implant placement planning. The axial view was chosen to replicate the clinician’s perspective in operation, and it allows for the identification of the shortest distances from the root apex to IC and to the buccal bone at specific measurement levels. As a result, these findings should be interpreted with this in mind.
This study provides valuable insights into the anatomical considerations of the nearby incisive canal that must be considered during immediate implant placement in the maxillary aesthetic zone of the Korean population:
The mean width of palatal bone between the root apex of central incisor and the IC was 3 mm for both right and left central incisors.
The buccal bone thickness at the incisor root apex is mostly thin, with the average not exceeding 1 mm, which is lower than the recommended guideline for minimum bone for immediate implant placement.
Negative correlation was observed between the buccal bone width and the palatal bone width at the apex of the root and the IC, i.e., the greater the bone available between the root apex and the IC, the less buccal bone width is present.
A gender-related difference was observed in this study, where men had higher average distances compared to women. However, age had no influence, highlighting the variability of the anterior maxillary region; hence, the importance of individualized treatment planning to carefully evaluate the proximity of IC to the incisor and the surrounding buccal and palatal bone for the success of the implant placement procedure. The findings suggest that caution must be taken when treating female patients due to their tendency to have thinner buccal bone and the IC being closer to the incisor.
Tapered implants are recommended for this region, and adjunct procedures such as bone grafts may be considered as part of treatment planning.
Future research should aim to validate these findings in larger, multi-center cohorts, including patients from diverse ethnic backgrounds, to assess potential population-specific anatomical variations. Longitudinal studies could investigate how the spatial relationship between the IC, palatal bone, and buccal bone changes over time and in response to tooth loss or other clinical conditions. Furthermore, virtual surgical planning and finite element analysis could be applied to simulate different implant designs and placements in relation to the IC, providing a more robust basis for clinical decision-making. Finally, prospective clinical trials could evaluate whether incorporating these anatomical considerations into immediate implant placement protocols improves surgical outcomes, reduces complications, and enhances long-term aesthetic stability.