Abstract
Isolated tricuspid regurgitation (TR) represents a significant yet understudied cardiac condition, primarily arising from structural valve anomalies or secondary to right ventricular (RV) dysfunction. This thesis reviews the pathophysiology, clinical picture, and evolving management strategies for isolated TR, focusing on medical and surgical interventions and emerging transcatheter therapies. Employing a comprehensive literature review and retrospective analyses, we delve into the etiological factors, diagnostic challenges, and treatment outcomes associated with this condition. Notably, we explore the prognostic implications of isolated TR following mitral valve surgery and the efficacy of various treatment modalities in improving patient survival and quality of life.
1. Introduction
Isolated tricuspid regurgitation (TR) refers to the presence of significant TR without other significant concomitant valve disease. It continues to be associated with an adverse prognosis. Etiologies are divided into primary and secondary, with important prognostic and management implications [1]. Cardiac multimodality imaging is critical in identifying TR severity, etiology, risk stratification, and impact on cardiac chamber size and function to guide treatment and surveillance. Management of isolated TR includes medical, surgical, and the rapidly evolving transcatheter interventions landscape [2,3]. In this contemporary review, we discuss etiologies, clinical features, evaluation, and management of isolated TR.
2. Etiology and Pathophysiology of Isolated TR
Isolated tricuspid regurgitation (TR) can arise from primary structural abnormalities of the tricuspid valve or secondary functional changes due to RV dysfunction. Primary TR can be caused by endocarditis, degenerative prolapse, cardiac device lead adherence, impingement or entanglement, prosthetic valve dysfunction, rheumatic heart disease, and carcinoid heart disease, medications such as fenfluramine and phentermine, or even autoimmune rheumatology conditions such as systemic lupus erythematosus or rheumatoid arthritis [4]. Infective endocarditis, particularly in intravenous drug users or patients with indwelling catheters, can lead to leaflet destruction or perforation [5]. Prosthetic valve regurgitation, whether due to degeneration, thrombosis, or paravalvular leaks, can also cause significant TR, often requiring reintervention [6]. Variable degrees of lead-induced isolated TR ranging from 7 to 45% have been reported in patients with cardiac implantable electronic devices (CIEDs) such as implantable cardioverter defibrillator, permanent pacemaker, or cardiac resynchronization therapy [7]. The underlying mechanisms contributing to CIED-induced TR can be categorized into implantation-related, pacing-induced, and device-mediated factors [7]. Congenital anomalies, such as Ebstein’s anomaly, are characterized by apical displacement of the tricuspid valve leaflets, leading to atrialization of the right ventricle (RV) and severe TR. The pathophysiology of primary TR involves direct valve damage or malformation, leading to increased RV volume overload, elevated right atrial pressures (more than 15 mmHg), and systemic venous congestion [8]. Over time, chronic volume overload results in RV dilatation, reduced RV ejection fraction, and progressive right-sided heart failure [6].
Secondary TR, more common than primary TR, typically arises from left-sided heart disease or pulmonary hypertension, leading to functional changes in the tricuspid valve apparatus. In patients with left-sided valvular disease, such as mitral stenosis or regurgitation, elevated left atrial pressures are transmitted backward, increasing pulmonary artery pressures (usually more than 50 mmHg) and causing RV pressure overload [9]. This results in tricuspid annular dilatation (>40 mm in diastole) and leaflet tethering, impairing coaptation and leading to significant TR. Similarly, in heart failure with reduced ejection fraction, elevated left ventricular (LV) filling pressures contribute to pulmonary hypertension and subsequent TR [8]. The pathophysiology of secondary TR involves a combination of pressure and volume overload on the RV, leading to progressive annular dilatation, leaflet malcoaptation, and worsening regurgitation. Hemodynamically, severe secondary TR is associated with regurgitant volumes > 45 mL/beat and regurgitant fractions > 40%, often accompanied by RV dysfunction and systemic venous congestion [10]. Over time, chronic TR exacerbates RV remodeling, further reducing cardiac output and perpetuating a cycle of worsening heart failure [11].
Vieitz et al. [12] aimed to evaluate the burden of TR in a large cohort of patients. They included echocardiographic data of more than 35,000 patients across 10 centers. The TR was moderate in 69.6%, severe in 25.5%, massive in 3.9%, and torrential in 1.0%. RV dilation was seen in 81.7% of patients with massive/torrential TR, 55.9% with severe TR, and 29.3% with moderate TR. Isolated TR was found in 16% of cases [12]. More than half of the cohort were categorized as high surgical risk, defined by pulmonary artery systolic pressure more than 50 mmHg, left ventricular ejection fraction (LVEF) < 35%, New York Heart Association class III-IV, or age > 85 years [12]. In a complementary study by Topilsky et al. [13], the prevalence and clinical consequences of isolated TR were further elucidated. They analyzed echocardiographic data between 1990 and 2000 to identify patients with moderate to severe TR. Isolated TR was found in 8.1% of those patients and was independently associated with increased mortality (adjusted risk ratio: 1.68) [13].
A recent large retrospective study was conducted by Wang et al. [11]: From January 2004 to December 2018, 9045 patients following the Cleveland Clinic Foundation had a mean age of 70.4 years and at least moderate to severe isolated TR. The patients were analyzed to understand the etiologies and associated outcomes. The TR etiologies were categorized as primary (5.2% of cases) and secondary (94.8% of cases), with the leading secondary causes being left heart disease, atrial functional impairment, and pulmonary disease, and primary causes including endocarditis, valve degeneration, or prolapse, and prosthetic valve failure. The primary endpoint was all-cause mortality, observed in 44% of patients over an average follow-up of 2.6 ± 3.3 years. They found that patients with secondary TR had worse survival than those with primary TR (HR: 1.56), but this result was not statistically significant in multivariable analysis [11].
3. Clinical Evaluation of Isolated TR
Patients with isolated TR are often incidentally diagnosed and are usually asymptomatic during the initial stages of the disease. The main symptoms of TR are associated with right heart failure (right-sided venous congestion followed by decreased cardiac output), such as peripheral edema, ascites, fatigue, and exercise intolerance. In severe cases, dyspnea on exertion can also be present, along with orthopnea and paroxysmal nocturnal dyspnea [14]. In advanced cases, patients may experience RV strain with angina pectoris and cardiac cachexia. Chronic RV pressure overload may result in atrial arrhythmias, such as atrial fibrillation, potentially worsening RV cardiac output due to tachycardia (shortened diastolic filling time) and atrioventricular uncoupling/dissociation. This process imposes a significant risk of intra-cardiac clots, which may lead to systemic or pulmonary embolization [13,15].
Physical examination findings encountered in patients with severe TR include systemic congestive signs such as pulsatile liver, hepatomegaly with or without jaundice, peripheral edema, ascites, and cachexia in advanced cases. Jugular venous distention with a prominent V wave is considered a hallmark finding and often accompanied by a pansystolic murmur that is high-pitched and loudest at the left lower sternal border, intensifying with inspiration (Carvallo’s sign). Other signs include an S3 gallop, indicative of right-sided volume overload, and decreased volume of peripheral pulsation, reflecting impaired forward blood flow. If left untreated, isolated TR will cause RV hypertrophy and strain, clinically manifested as RV heave or S4 gallop [16,17,18].
The clinical and hemodynamic differences between isolated TR and TR in the context of multivalvular disease are significant, primarily due to the interplay of multiple valvular pathologies and their combined impact on cardiac function. In isolated TR, the primary pathology is localized to the tricuspid valve or right ventricle, leading to symptoms and signs predominantly related to RV failure [3]. On the other side, multivalvular disease associated with TR, such as concomitant mitral or aortic valve disease, often results from LV failure with or without pulmonary hypertension, eventually worsening RV afterload and TR severity. This results in a more complex clinical picture, where symptoms of left-sided heart failure (e.g., pulmonary edema and orthopnea) coexist with right-sided manifestations [16]. Additionally, physical examination findings in multivalvular disease may include murmurs of mitral or aortic pathology, such as a diastolic rumble in mitral stenosis or a blowing holosystolic murmur in mitral regurgitation, alongside the classic TR findings [14].
The initial diagnostic workup for patients with isolated TR starts with an electrocardiogram, chest X-ray, and laboratory tests, including N-terminal-pro-B-type natriuretic peptide (NT-proBNP), renal function, and liver function studies. EKG may reveal right atrial enlargement, right ventricular hypertrophy, or atrial fibrillation [15]. Chest X-ray can show cardiomegaly, particularly right atrial and ventricular enlargement, and may also demonstrate pleural effusions or pulmonary congestion in decompensated cases. Laboratory testing is crucial, as elevated NT-proBNP levels are concerning [2]. NT-proBNP is the hallmark of heart failure, released by the myocardial cell in response to wall stretch and strain. As a direct effect of systemic venous congestion, decreased cardiac output, and possibly cardiorenal syndrome, renal function tests may show some degree of impairment. Liver function tests may also show a cholestatic transaminitis pattern with elevated bilirubin or transaminases, indicating hepatic congestion from retrogressive flow of the TR jet [19]. Renal dysfunction, with or without hepatic dysfunction, was found in cases of isolated TR without significant other etiologies, raising concerns about hemodynamic compromise even before the classic stigmata of congestive heart failure [20]. These findings collectively help assess the severity of TR and its systemic impact, directing the management decisions [19].
4. Multimodality Imaging Evaluation
The tricuspid valve has recently gained increased attention due to the suboptimal outcomes associated with existing treatment options and new advances in percutaneous valvular interventions. A thorough comprehension of the TV’s anatomy and associated pathologies is essential for effectively evaluating and managing isolated TR. Using a multimodality imaging approach, including transthoracic and transesophageal echocardiography, computed tomography, and magnetic resonance imaging, plays a vital role in assessing TR and guiding surgical and percutaneous procedures [13]. Table 1 shows the widely used imaging modalities for TR evaluation. Combined with clinical considerations, these imaging techniques help determine the timing, indications, modality selection, and risk stratification for tricuspid valve interventions, although these aspects remain subject to ongoing debate [10].

Table 1.
Comprehensive imaging modalities for TR evaluation.
As per recent guidelines, TV imaging is essential for comprehensively assessing its function and structure. For transthoracic echocardiography (TTE), multiple views are recommended to overcome the challenges posed by the TV’s complex anatomy, particularly the difficulty in visualizing all three leaflets simultaneously due to their arrangement and the variability in transducer angulation [21]. The guidelines specify several optimal transthoracic windows for viewing the TV and right ventricle (RV), intended to improve the accuracy of diagnosing conditions such as TR. This includes the parasternal inflow and short-axis views, which help identify the septal and posterior leaflets under different angulations, and the apical four-chamber views focus on the anterior leaflet with an anterior tilt and the posterior leaflet with a posterior tilt [26,27]. Additionally, 3D imaging offers significant advantages by providing full-face views of the valve, simplifying the identification of the leaflets without reconstructing 2D images. The ASE Chamber Quantification Guideline also emphasizes the importance of specialized views and measurements for assessing the RV, including subcostal views for evaluating RV wall thickness and Doppler alignments for TR jets [28].
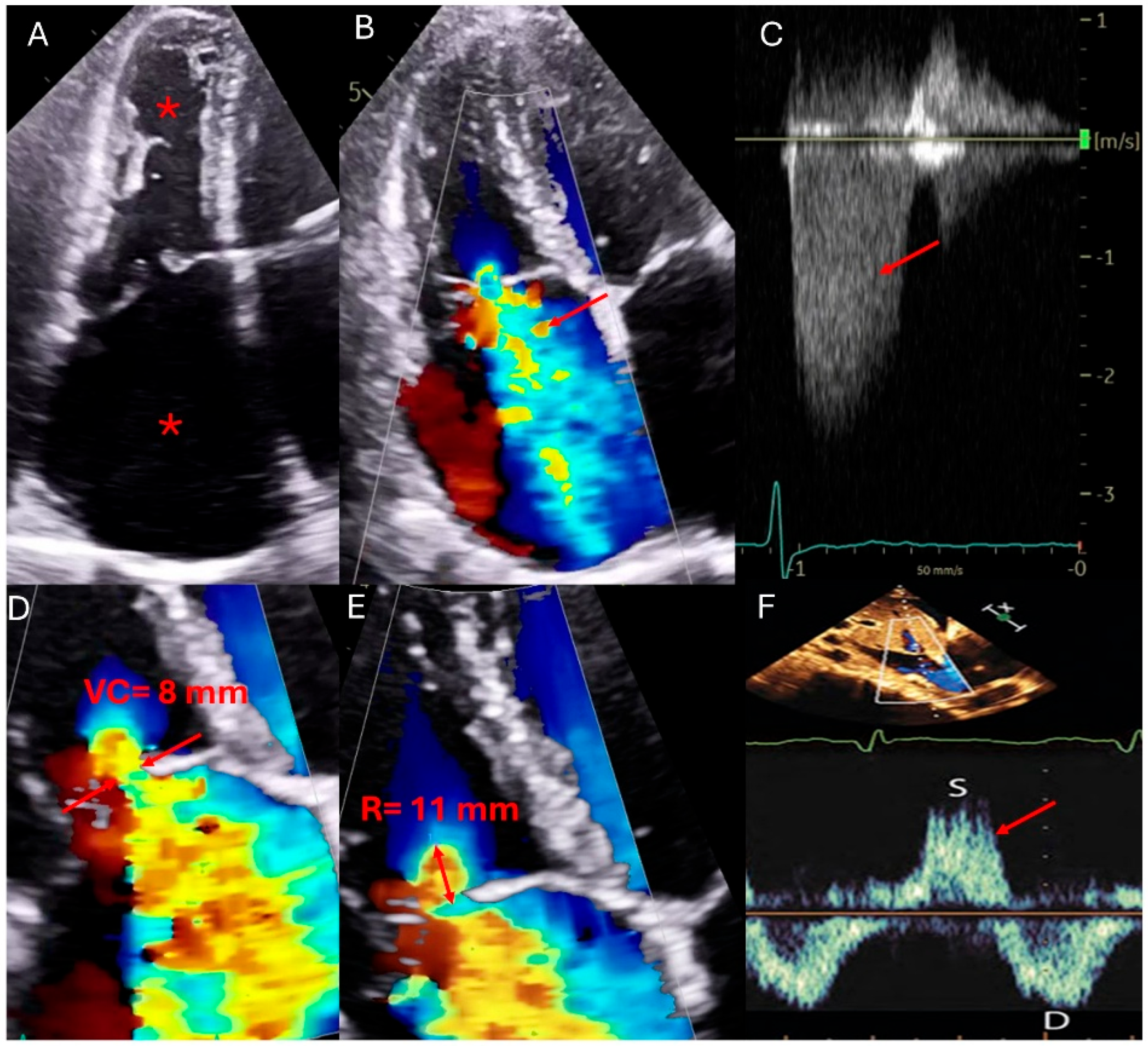
Figure 1—Echocardiographic qualitative and quantitative measures of TR.
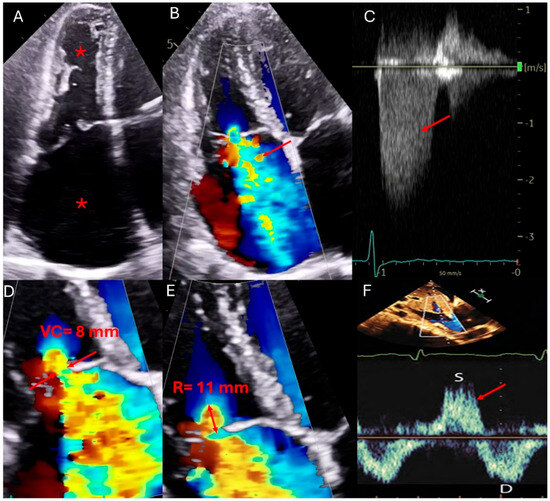
Figure 1.
Qualitative and quantitative parameters of severe tricuspid regurgitation (TR by echocardiography). (A) Apical four-chamber view showing right atrial (RA) and right ventricular (RV) dilation (asterisks). (B) Color Doppler highlights a large TR jet occupying > 50% of the RA. (C) Continuous-wave Doppler across the tricuspid valve reveals a dense, early peaking spectral Doppler profile (red arrow). (D) Zoomed view of the tricuspid valve shows a vena contracta width exceeding 7 mm (distance between tips of red arrows). (E) Proximal Isovelocity Surface Area (PISA) method demonstrates a large flow convergence zone (radius of 11 mm), with an effective regurgitant orifice area (EROA) ≥ 0.4 cm2. (F) Pulsed-wave Doppler of the hepatic veins shows systolic flow reversal (red arrow), a key marker of severe TR.
In the echocardiographic assessment of TR, various qualitative, semi-quantitative, and quantitative parameters are used to classify the severity into mild, moderate, and severe categories. Qualitatively, TV morphology can range from mildly abnormal leaflets, such as mild rheumatic thickening or limited prolapse in mild cases, to severe valve lesions like flail leaflets, ruptured papillary muscles, severe retraction, or large perforations in severe TR [22]. Interventricular septal motion and characteristics of the flow convergence zone and the TR jet’s continuous wave (CW) Doppler signal vary significantly, from minimal abnormalities in mild cases to extensive changes in severe TR (Figure 1). Semi-quantitatively, the inferior vena cava (IVC) diameter, color flow jet area, vena contracta width, and proximal iso-velocity surface area (PISA) radius provide insights into the regurgitant flow, with all parameters increasing significantly as the severity progresses [22].
Quantitative measures such as the effective regurgitant orifice area (EROA) and regurgitant volume by PISA and 3D techniques further delineate the severity, with values escalating from less than 20 mm2 and under 30 mL in mild cases to more than 40 mm2 and over 75 mL in severe TR [22]. Hepatic vein flow and tricuspid inflow measurements complement these findings, helping to confirm the severity as indicated by systolic dominance in mild cases and systolic flow reversal in severe TR. These comprehensive assessments not only enhance the understanding of the pathological impact of TR but also guide clinical decision-making regarding the timing and type of therapeutic intervention needed [23,26] (Table 2).

Table 2.
Qualitative and quantitative parameters used to grade the severity of TR.
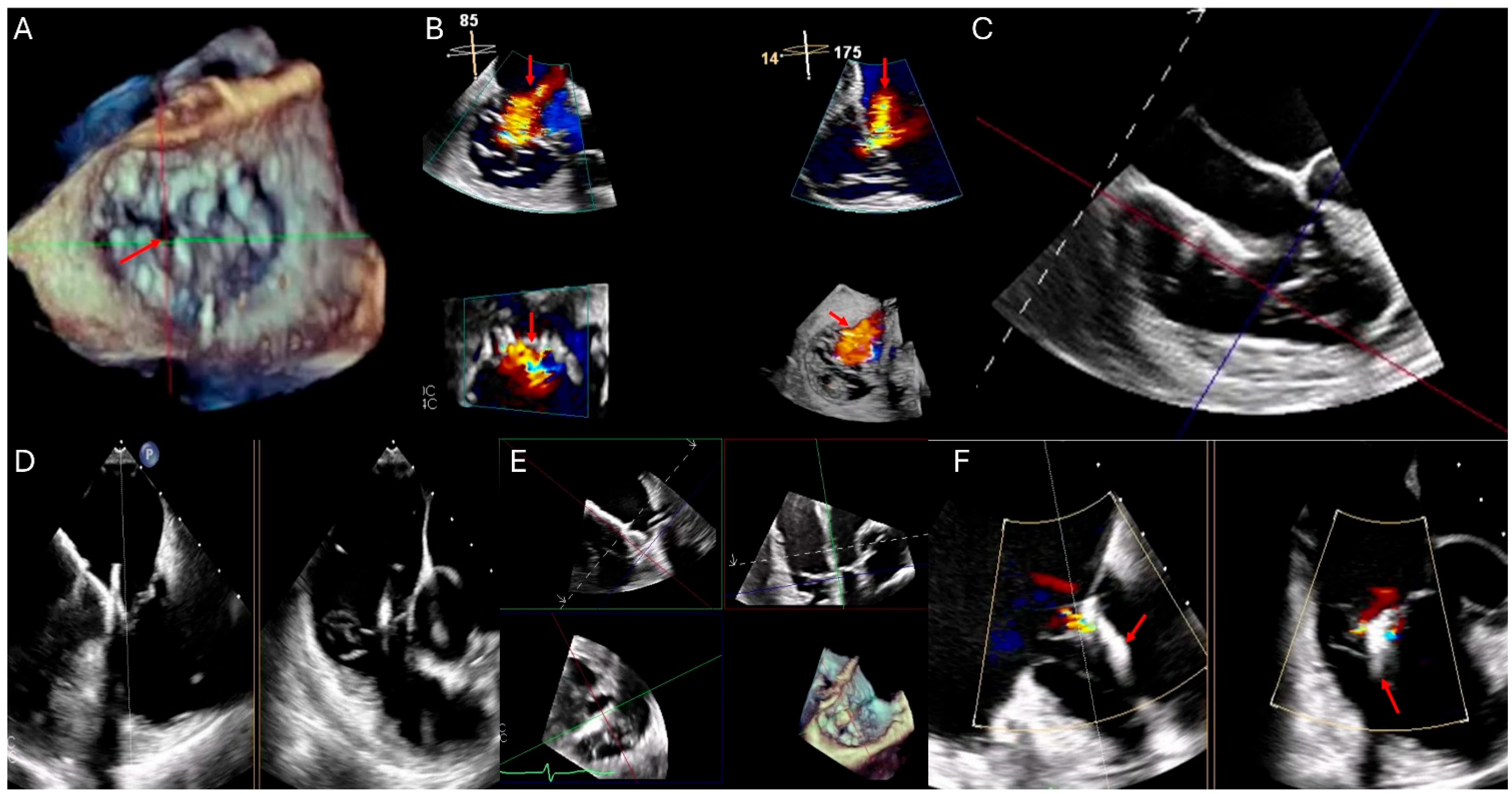
Transesophageal echocardiography (TEE) complements TTE by allowing for detailed visualization of the TV through various esophageal and gastric views. The guidelines for TEE outline a systematic approach involving multiplane angles and varying depths, from mid-esophageal to deep transgastric positions, to capture comprehensive images of the TV. This method enables the visualization of all three TV leaflets and the adjacent cardiac structures [29]. The proximity of the esophagus and stomach to the heart’s position facilitates these detailed examinations, which are particularly beneficial in 3D imaging, which offers superior resolution in the axial plane compared to lateral and elevational planes [29]. Furthermore, 3D echocardiography enhances the identification of tricuspid leaflets (number of leaflets, shapes, and presence of indentations) and related anatomical structures, providing crucial insights into the TV complex’s spatial orientation and aiding in the accurate assessment of valve pathology and function [30]. During procedures like transcatheter edge-to-edge repair, TEE offers real-time guidance, ensuring precise device placement and monitoring for potential complications (Figure 2). Additionally, post-procedural TEE helps evaluate residual regurgitation, leaflet integrity, and overall procedural success, optimizing patient outcomes [31]. Stress echocardiography, though less commonly used in TR, helps assess pulmonary hypertension and functional assessment, particularly in concomitant pulmonary conditions. Typically, TR worsens with exercise due to increased right ventricular afterload or pulmonary hypertension. In addition, stress echocardiograms can provide insights into right ventricular functional reserve and exercise-induced changes in regurgitant volume, which may guide therapeutic decisions. TEE and stress echocardiography play complementary roles in characterizing isolated TR, especially in complex cases or when the parameters are approaching indications for surgical intervention [27].
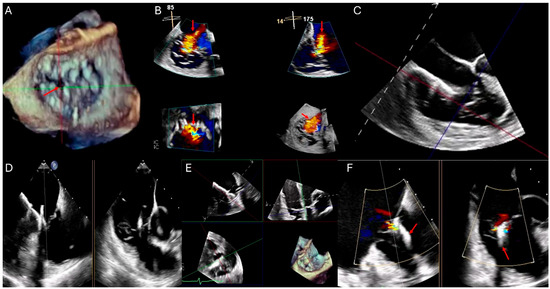
Figure 2.
This composite echocardiographic figure illustrates stepwise transesophageal echocardiographic (TEE) guidance for transcatheter tricuspid clip placement using 3D multiplanar reconstruction (MPR). (A) En-face 3D view of the tricuspid valve for leaflet assessment showing central coaptation gap (red arrow). (B) MPR views demonstrating tricuspid regurgitant jet severity (red arrows). (C) Mid-esophageal 0-degree view showing catheter direction through IVC directed towards the tricuspid valve. (D) Biplane imaging confirming clip orientation and leaflet approximation. (E) 3D MPR-guided leaflet grasping during clip deployment. (F) Post-deployment color Doppler showing trivial residual tricuspid regurgitation and successful leaflet coaptation using the tricuspid clip (red arrows).
Figure 2—TEE-3D MPR showing guidance for transcatheter tricuspid clip.
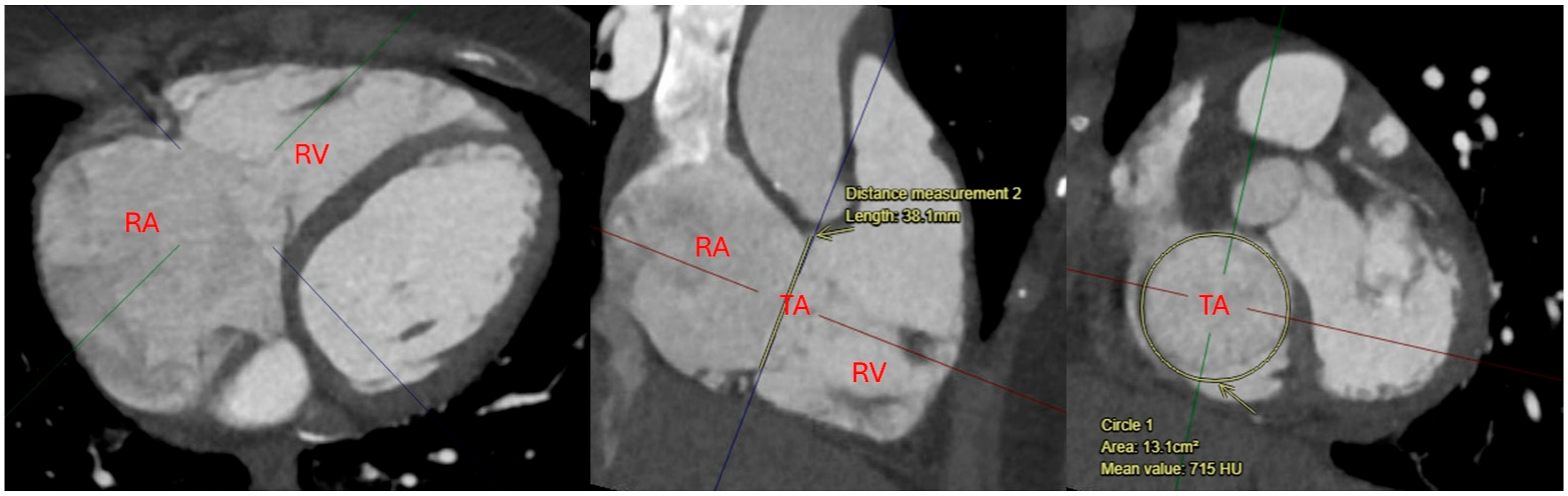
Computed tomography (CT) plays a critical role in preoperative planning for isolated TR before surgical and transcatheter repair approaches. CT provides high-resolution, three-dimensional imaging with detailed anatomical information of the tricuspid valve apparatus and right heart structures throughout the cardiac cycle. This information is essential for assessing valve morphology, annular dimensions, and the spatial relationship of the tricuspid valve to adjacent structures such as the coronary sinus and right coronary artery [32]. For transcatheter interventions, CT is invaluable for determining patient eligibility, guiding device sizing, and identifying potential procedural challenges, such as annular calcification or unfavorable anatomy (Figure 3). CT also provides a tool to assess venous access routes, including the femoral and jugular veins used for transcatheter procedures. In surgical planning, CT aids in visualizing the extent of right atrial and ventricular enlargement, as well as associated pathologies like endocarditis or congenital abnormalities [33]. The combination of anatomical and functional data provided by CT enhances diagnostic accuracy, optimizes patient selection, and improves the safety and efficacy of novel transcatheter therapies for severe TR [32,33].
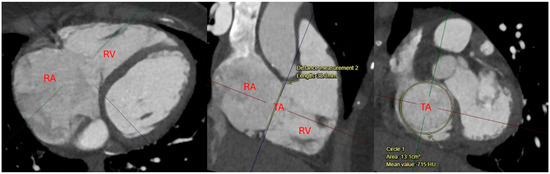
Figure 3.
4D-CTA MPR image showing tricuspid annulus anatomy measurements Abbreviations: TA: tricuspid annulus; RA: right atrium; RV: right ventricle.
Figure 3—4D-CTA MPR image showing tricuspid annulus anatomy measurements.
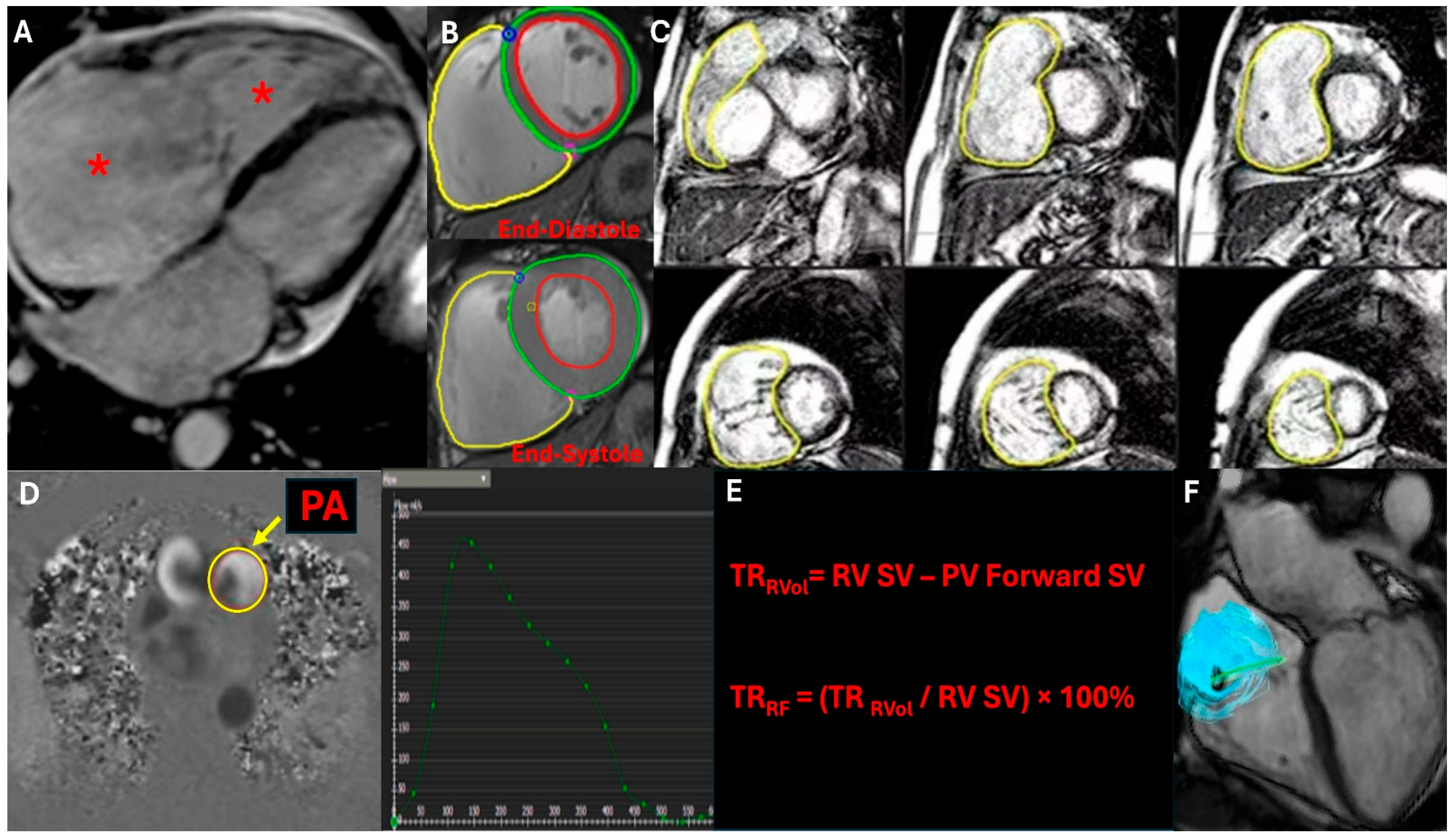
Cardiac magnetic resonance imaging (CMR) is a complementary imaging modality for evaluating isolated TR and assessing RV geometry and function. CMR is generally considered when echocardiographic findings are inconclusive [24]. CMR employs phase-contrast flow imaging to measure forward stroke volume (FSV), defined as the volume of blood ejected through the pulmonic valve, and reverse stroke volume (RSV), representing the volume of blood regurgitated through the tricuspid valve, which enables measurement of regurgitant volume (RV) and regurgitant fraction (RF) across the tricuspid valve. The net stroke volume (NSV), derived from the difference between FSV and RSV, quantitatively assesses TR severity. It also offers a detailed assessment of RV size, morphology, and function, including RV end-diastolic volume, end-systolic volume, and ejection fraction (Figure 4) [25,26]. Additionally, cardiac MRI can evaluate RV myocardial strain, fibrosis, and ventricular remodeling resulting from the long-standing right-sided volume overload. Additionally, CMR allows the detection of pulmonary vascular disorders such as pulmonary hypertension (PH) and other pathologies, such as congenital abnormalities or myocardial diseases. Given its robust reproducibility and non-invasive nature, CMR is increasingly recognized as the gold standard for quantifying right-sided valvular lesions, guiding clinical decision-making and improving risk stratification in patients with moderate to severe TR, and is a promising tool in preoperative/preprocedural planning [24].
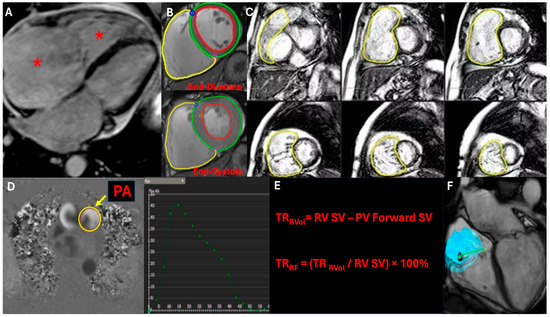
Figure 4.
This CMR imaging figure presents a comprehensive assessment of tricuspid regurgitation (TR). (A) Cine four-chamber view showing right atrial (RA) and right ventricular (RV) dilation (red asterisks). (B) Phase-contrast flow imaging capturing the TR jet. (C) 3D whole-heart CMR for RV volumetric assessment, calculating RV end-diastolic volume (RVEDV) and RV end-systolic volume (RVESV). (D) Phase-contrast imaging through the pulmonary artery (PA) to determine pulmonary forward stroke volume (FSV). (E) Quantification of TR severity using regurgitant volume (RVSV-PSV) and regurgitant fraction formulas. (F) 4D flow CMR visualizing TR’s hemodynamic impact through altered flow streamlines.
Figure 4—CMR evaluation of TR (showing RV quantification, TR qualitative, and pulmonic flow and formula)
A retrospective study at the Cleveland Clinic Foundation investigated the prognostic value of echocardiography and CMR in patients with isolated severe TR [25]. Among 262 patients (21% with primary TR), 33.2% underwent tricuspid valve surgery after CMR. Over a mean follow-up of 2.5 years, 26.0% of patients died. CMR-derived TR fraction (HR: 1.15 per 5% increase) and echocardiography-derived right ventricle free wall longitudinal strain (HR: 1.10 per 1% decrease in magnitude) were independently associated with worse survival, along with right heart failure symptoms (HR: 2.03). Tricuspid valve surgery showed borderline protective effects (HR: 0.55). Optimal thresholds for mortality prediction included a regurgitant fraction ≥ 30%, regurgitant volume ≥ 35 mL, and RV free wall longitudinal strain ≥ −11% [25].
5. Risk Scores of Isolated TR
EuroSCORE and EuroSCORE II are commonly used scores for risk stratification to predict mortality for general cardiac surgery. However, recent trials have shown that they tend to overestimate the mortality risk when applied to isolated tricuspid valve surgery (ITVS) [34]. Historically, TR has been undertreated in the context of the perceived high surgical risk and limited therapeutic options. However, more recent data highlight the detrimental impact of untreated TR RV function and quality of life, emphasizing the need for acceptable risk stratification and tailored management protocols [35]. Dedicated risk scores have become valuable tools for predicting outcomes and optimizing patient care. Among these, the TRI-SCORE [36] and the novel risk score [11] have been recognized as the most widely validated models to assess risk and inform therapeutic decisions in cases of isolated TR.
The TRI-SCORE is designed to predict in-hospital mortality following ITVS for severe TR. It was developed by Dreyfus et al. [36] through a multicenter analysis of 466 patients. They integrated eight clinically accessible parameters: age ≥ 70 years, NYHA Class III-IV, RV failure signs, a daily furosemide dose ≥ 125 mg, impaired renal function (GFR less than 30 mL/min), impaired liver function (high bilirubin), LVEF less than 60%, and moderate to severe RV dysfunction. The TRI-SCORE ranges from 0 to 12 points, with risk stratification showing a progressive increase in in-hospital mortality from 0% for scores of 0 to 60% for scores equal to or above 9. The TRI-SCORE has proven discrimination potential, with a higher area under the receiver operating characteristic (ROC) curve of 0.81, better than EuroSCORE (0.67) and EuroSCORE II (0.63) [36].
A second risk stratification model for isolated TR was developed by Wang et al. [11] in a large contemporary cohort study encompassing 9045 patients with moderate to severe TR, providing a broader and more comprehensive perspective compared to earlier models. This study, conducted from 2004 to 2018, categorized TR etiologies as primary (5.2%) or secondary (94.8%). Over a mean follow-up of 2.6 ± 3.3 years, 44% of patients died, with secondary TR associated with worse unadjusted survival compared to primary TR (HR: 1.56). However, this association was not significant after multivariable adjustment. The study introduced a novel risk score to predict 1-year mortality. The score included more parameters such as the history of myocardial infarction, peripheral vascular disease, chronic lung disease, chronic kidney disease, current loop diuretic use, anemia, thrombocytopenia, albumin, INR more than 1.5, and pulmonary artery systolic pressure more than 50 mmHg. It has more categories for age and right ventricular systolic function. The total score is 16 with a gradual increase of 1 year, with an all-cause mortality from 2.3% at a score of 0, 9.3% at 3, 24.7% at 6, and 67% at 12–16 [11].
6. Medical Management of Isolated TR
The medical management of isolated TR aims first to address its underlying causes. In cases of infective endocarditis, prompt initiation of antibiotic therapy is critical. Empirical regimens typically include intravenous antibiotics such as vancomycin or ampicillin-sulbactam, tailored based on blood culture results and local resistance patterns. For fungal endocarditis, antifungal agents like amphotericin B or echinocandins are recommended [37]. While medical therapy may suffice for uncomplicated cases, surgery is often necessary for persistent infection, large vegetations (>10 mm), or hemodynamic instability. In some cases, a “0.2 to face” approach may be employed, where the tricuspid valve is removed to control infection and replaced after a few months of antibiotic therapy [37]. Lead-induced TR in patients with pacemakers or defibrillators occurs when CIED lead impinges on one of the TV leaflets, causing restriction and impaired systolic coaptation, thus leading to regurgitation of blood into the right atrium. Lead extraction is usually performed in the setting of infection, malfunction, or mechanical complications such as lead impingement [7]. The therapeutic procedure involves techniques such as simple traction, mechanical or laser-assisted extraction, or surgical removal, depending on the complexity and adherence of the lead. While it carries risks like vascular injury or cardiac perforation, lead extraction is often necessary to address life-threatening conditions and may require temporary pacing or lead reimplantation post-procedure [38].
The current treatment options for isolated TR, particularly in the context of right heart failure, present a complex therapeutic challenge due to the limited data defining effective medical therapy. Despite the lack of Class I recommendations in current guidelines, diuretics hold a Class IIa recommendation in the American College of Cardiology/American Heart Association valve guidelines. The strategy involves a nuanced understanding of renal physiology and diuretic pharmacokinetics to manage heart failure effectively [14]. European guidelines advocate a stepwise pharmacologic approach, emphasizing frequent reassessment of treatment to achieve successful decongestion, particularly in diuretic resistance, which often complicates late-stage right heart failure. These guidelines also underscore the importance of addressing the primary cause of heart failure, such as utilizing pulmonary vasodilators for elevated pulmonary artery pressures or guideline-directed medical therapy for heart failure with varying ejection fractions. This comprehensive approach aims to mitigate the severity of TR and improve patient outcomes through tailored medical treatment [39].
For patients with isolated TR and associated right-sided heart failure or atrial fibrillation, medical management focuses on optimizing volume status and rhythm control. Diuretics, particularly loop diuretics like furosemide, are the cornerstone of therapy to reduce systemic congestion [21]. In cases of atrial fibrillation, rate control with beta-blockers or calcium channel blockers is preferred, while rhythm control may be considered in symptomatic patients. Anticoagulation with warfarin is recommended for atrial fibrillation with a CHA2DS2-VASc score ≥ 2, as per the 2021 ESC/EACTS valvular heart disease guidelines [21]. For refractory right-sided heart failure, advanced therapies such as inotropes or pulmonary vasodilators may be considered, though the evidence remains limited. Recent guidelines emphasize a multidisciplinary approach, integrating medical therapy with timely surgical intervention when indicated to improve outcomes in isolated TR [14,21].
7. Surgical Management of Isolated TR
Multiple clinical guidelines exist for diagnosing and managing TR, but the recommendations may sometimes vary. In many cases, surgical intervention is of choice according to TR grading, association with AF, and indications for valve surgery in primary vs. secondary TR, symptomatic vs. asymptomatic patients, and isolated TR forms. Table 3 shows guidelines for isolated TR surgery in contemporary guidelines. Discrepancies exist in the role of biomarkers, multimodality imaging, exercise TTE, and cardiopulmonary exercise testing for risk stratification and clinical decision-making [40]. TV diseases generally have poor prognoses when treated medically and are associated with significant morbidity and mortality with traditional surgical techniques [41].

Table 3.
Guidelines for isolated TR surgery in contemporary guidelines [14,21].
Tricuspid valve repair had a better outcome in preserving RV function and preventing all-cause mortality. In the nationwide inpatient sample database (NIS) between 1999 and 2008, hospital mortality for replacement was 13.6 versus 9.5 in cases of tricuspid repair except those with hepatic involvement [42]. TV repair with annuloplasty is generally preferred where feasible [43]. It aims to correct the dilation of the tricuspid annulus along its posterior portion using suture, band, and ring techniques. Kay procedure or suture bicuspidisation includes the placement of pledget-supported mattress sutures in the annulus to obliterate the annular segment causing TR [44]. De Vega annuloplasty consists of a couple of C-shaped suture lines along the anterior and posterior tricuspid leaflet bases from the anteroseptal commissure, back to the origin of the coronary sinus to reduce the orifice diameter [45]. The use of undersized rigid or semirigid ring or flexible band has been more used in the last decade as it is associated with lower rates of late recurrent TR and better quality of life [46]. Although these rings or bands do not cover the septal part of the tricuspid annulus to avoid injury to the AV node, a mild increase in ring dehiscence may require a redo surgery [47].
Surgical replacement of tricuspid valve in isolated TR is considered when repair is not feasible or expected to have a high failure rate, such as in significant RV dilation and systolic dysfunction and/or severe pulmonary hypertension [45]. Generally, there are two types of valvular prosthesis: bioprosthesis or tissue valve versus mechanical or metallic prosthesis. Bioprosthesis is constructed from animal tissue, such as bovine pericardium and porcine valves, chemically treated with formaldehyde, or human dura mater, treated with glycerol. It has a lower immunological reaction and thrombotic burden [48]. That is why bioprosthesis has a lower incidence of valvular thrombosis, only requiring a few months of systemic anticoagulation. Hence, it is preferred when long-term anticoagulation is not desirable, such as in the elderly, bleeding diathesis, or short life expectancy [48,49]. However, the viscoelastic properties of bioprosthetic materials decrease with higher pressure gradients over the years following TR replacement, favoring the choice of mechanical prosthesis in patients with a long life expectancy, such as young patients or those already requiring systemic anticoagulation [48,49].
Cardiopulmonary bypass (CPB) is an extracorporeal circulation that collects venous return from both superior and inferior vena cavae, oxygenates, and then delivers to the ascending aorta. It enables surgeons to work on an arrested heart, allowing delicate manipulations on a motionless, bloodless field. CPB decreases myocardial oxygen demand, allowing more prolonged and complex reconstructive surgeries [50]. The procedure includes aortic, venous, and coronary sinus cannulation and requires antegrade (before aortic cross-clamping) or retrograde (in the coronary sinus) cardioplegia using hypothermic and hyperkalemic solutions [50]. The CPB can be complicated with systemic hypotension, serious arrhythmia, blood loss, thrombosis, systemic embolization, or distributive shock [51]. The other less manipulative surgical choice is working on a beating heart (off-pump). It is important to distinguish that “off-pump” surgery specifically refers to procedures performed without the use of a cardiopulmonary bypass, whereas “beating-heart” describes operations in which myocardial activity is maintained, regardless of whether a bypass is employed. Beating-heart tricuspid valve surgery has gained popularity to reduce myocardial ischemia and bypass-associated complications, particularly in reoperations or high-risk patients. Off-pump beating-heart techniques aim to avoid the systemic effects of cardiopulmonary bypass altogether, while on-pump beating-heart procedures maintain perfusion support without cross-clamping or cardioplegia [52]. While the off-pump technique requires higher surgical skills and only applies to valvular interventions with no capability to perform more concomitant or complex cardiac or coronary interventions, it has the advantages of faster recovery, less need for blood transfusion, and avoidance of cardiopulmonary bypass complications [52].
Minimal access TV surgeries aim to reduce the surgical risks associated with open-heart surgery to relieve pain, blood loss, and wound infection risks and eventually shorten hospital stays [53]. The surgical techniques for Minimal Access TV Surgery (MATVS) involve several key steps to minimize patient trauma and improve recovery outcomes. These include using smaller cosmetic incisions like the per areolar skin incision, often video-assisted for better visibility. Procedures typically employ peripheral cannulation for cardiopulmonary bypass, with careful planning around clamping and cardioplegia delivery to protect myocardial function. These minimally invasive approaches leverage endoscopic and robotic technologies to enhance precision and reduce the surgical footprint [52].
Recent data challenge the reluctance to pursue surgical intervention for isolated TR. Early surgical correction, particularly in patients without advanced RV dysfunction or end-organ damage, has demonstrated excellent outcomes [3]. In this context, Sala et al. [2] reported no in-hospital, 5-year mortality, or further hospitalizations for RV failure in patients undergoing early surgical repair or replacement. These results contrast sharply with the historically high in-hospital mortality rates (8.8–37%) and poor long-term outcomes (55% mortality at 5 years) reported in older studies [3,6], which often included patients with advanced disease and severe RV dysfunction. Sala et al. created a novel clinical classification system (Stages 1–5) for patient stratification according to the TR severity, RV function, and end-organ involvement. This score should help to figure out the optimal timing for intervention. Lowish stages (less than or equal to 3) are associated with fewer complications, hospital stays, and better long-term outcomes versus higher stages (Stages 4–5) associated with higher morbidity and mortality [2].
Older studies on isolated TR repair versus replacement have shown equivocal outcomes, with mixed evidence on survival benefits and long-term prognosis. Lee et al. [16] found a non-significant trend toward improved survival in patients undergoing tricuspid valve surgery (TVS) compared to medical management, with a 5-year survival rate of 74% in the non-surgical group. Key predictors of mortality included TR severity, pulmonary hypertension, and right ventricular (RV) dysfunction. Similarly, Izumi et al. [15] identified preoperative atrial fibrillation and ejection fraction as predictors of severe isolated TR development after left-sided valve surgery, with significant increases in tricuspid annular diameter and right atrial area postoperatively. A more considerable retrospective analysis by Saran et al. [54] of 2541 patients undergoing TV surgery found higher mortality rates associated with valve replacement (HR:1.54) compared to repair, with overall survival rates of 54% at 5 years and 13% at 15 years. These studies highlight the complexity of managing isolated TR and the need for careful patient selection, as outcomes are influenced by factors such as RV function, TR severity, and timing of intervention.
A large meta-analysis encompassing over 15,000 patients evaluated outcomes of isolated tricuspid valve repair versus replacement, providing critical insights for surgical intervention in isolated TR. The analysis included 16 studies (6808 repairs and 8261 replacements) identified from 811 screened abstracts, with patient ages ranging from 36 to 68 years and female representation varying between 24% and 92%. Pooled operative mortality rates were significantly lower for tricuspid valve repair compared to replacement (8.4% vs. 9.9%, OR:0.80). Repair was also associated with reduced rates of in-hospital acute renal failure (12.4% vs. 15.6%, OR: 0.82) and pacemaker implantation (9.4% vs. 21.0%, OR:0.37). However, repair was associated with an increased cerebrovascular accident rate (1.5% vs. 0.9%, OR:1.63). In both treatment options, no significant differences were found regarding prolonged ventilation, mediastinitis, operating room return, or late mortality. Despite the higher incidence of cerebrovascular events, the meta-analysis conclusion advocates for TR repair over replacement in cases of isolated TR [41].
Managing an intracardiac device lead as PPM and ICD can be challenging in the context of TR surgeries, particularly if they are considered related to the pathogenesis of isolated TR. Surgical techniques include lead extraction versus lead preservation (jailing) and repositioning of the lead. Lead extraction is preferred in isolated TR with significant lead fibrosis. If lead has minimal impact on the isolated TR pathology, lead preservation (jailing) and repositioning would carry less tissue manipulation and postsurgical complications [55]. Managing device leads become more difficult in patients undergoing percutaneous interventions due to the higher incidence of lead fracture and subsequent infections. Transvenous lead extraction has an inconsistent profile on worsening or improving TR severity. A multidisciplinary approach is used to optimize the patient medically, assess whether lead is the main mechanism in isolated TR, and whether the patient is a safe candidate for extraction before performing the procedure. A leadless, epicardial pacemaker or extravascular ICD are choices for those who are pacemaker-dependent or class I ICD candidates [56].
8. Transcatheter Interventions for Isolated TR
Despite the increasing prevalence of TR and its association with poor survival, isolated TV surgery remains infrequently performed [57]. To address this unmet clinical need, several less invasive transcatheter TV therapies have emerged as an alternative to surgery in high-risk patients with severe functional TR [57]. Transcatheter TV repair devices aim to improve leaflet coaptation by bringing the leaflets together or indirectly by addressing the dilated annulus. Transcatheter TV replacement, on the other hand, can be orthotopic (implantation of prosthetic valve in an anatomically correct position in the tricuspid annulus) or heterotopic (implantation of prosthetic valve in a different anatomic location to counter the hemodynamic and clinical consequences of severe TR). Data from first-in-man studies on the safety and efficacy of various transcatheter TV therapies are promising. Technological advancements and increased experience are anticipated to improve outcomes of transcatheter TV therapy in the coming years. Ongoing and future studies should focus on careful patient selection, optimal timing of intervention, long-term clinical outcomes, and device durability [57].
In a study involving 2413 patients with severe isolated functional TR, participants were divided into three groups: 1217 were conservatively managed, 551 underwent isolated TV surgery, and 645 received transcatheter valve repair. Survival over two years served as the primary endpoint. The TRI-SCORE, which assesses the severity of TR, showed 32% of patients with a low score (≤3), 33% with an intermediate score (4–5), and 35% with a high score (≥6). Successful correction rates were high, with 97% in the surgical group and 65% in the transcatheter group. Survival rates decreased across all treatment modalities with increasing TRI-SCORE severity [35]. Notably, in the low TRI-SCORE category, survival was significantly better in the surgical and transcatheter groups compared to conservative management, with rates of 93%, 87%, and 79%, respectively. However, in the intermediate score category, overall survival rates showed no significant differences among the groups. Still, an important benefit was seen in patients with successful correction [35]. No survival benefit was observed in the high TRI-SCORE category between the groups. The study concluded that, while survival decreased with higher TRI-SCOREs across all treatment modalities, early and successful surgical or transcatheter interventions significantly improved two-year survival rates in patients with low and, to a lesser extent, intermediate TRI-SCOREs, but no improvement was seen in those with high scores [35].
In an extension of the previous study conducted in the TRIGISTRY [58], an international cohort study across 33 centers in 10 countries, researchers investigated the 10-year survival rates of patients with severe isolated functional TR. The study compared the outcomes between 1217 patients managed conservatively and 551 who underwent isolated TV surgery, including 200 repairs and 351 replacements, stratified by TRI-SCORE categories [58]. The 10-year survival rates showed no significant overall difference between surgical and conservative management. However, surgery significantly improved survival in the low TRI-SCORE category compared to conservative management (72% vs. 44%; HR:0.27). In this category, both repair and replacement methods showed benefits over conservative management, with survival rates of 84% for repairs and 61% for replacements (HR 0.11 and 0.65, respectively). For the intermediate category, only repair showed a survival benefit (59% vs. 37%; HR 0.49), while replacement appeared possibly harmful (25% vs. 37%; HR 1.43). No significant survival benefit was observed in the high TRI-SCORE category for surgical intervention [58].
Orban et al. [59] reported a dual-center observational study that assessed the mid-term safety, efficacy, and clinical outcomes of transcatheter edge-to-edge TV repair in 50 patients with right heart failure and severe TR. Of these, 14 patients were treated for isolated TR and 36 for combined MR and TR. At a 6-month follow-up, 90% experienced a reduction in at least one echocardiographic TR grade, and 79% showed improvement in the NYHA class. Additionally, the 6-MW distance increased by 44% (+84 m), the median pro-BNP decreased by 30%, and the quality-of-life score improved by 16% (a decrease of six points in the Minnesota Living with Heart Failure Questionnaire score). The outcomes were similar regardless of whether the patients underwent isolated TR or combined MR and TR treatment [59]. During the follow-up period, there were eight deaths, 14 hospitalizations for worsening HF, two patients underwent TV surgery, and two received a second TV clip procedure. The study concludes that transcatheter edge-to-edge TV repair is a safe and effective treatment for severe TR, leading to significant clinical improvements in most patients [59]. Orban et al. [60] extended their research to include 119 patients undergoing isolated transcatheter TV repair. The procedure was successful in reducing TR to moderate or less with no in-hospital deaths. At the one-year follow-up, 72% maintained a durable TR reduction. TTVR led to a 22% reduction in the annual hospitalization rate for heart failure, with significant improvements in NYHA functional class, 6 min walk distance, and Minnesota Living with Heart Failure Questionnaire scores. The procedural success was associated with improved 1-year survival and event-free survival rates, demonstrating comparable outcomes to patients who underwent combined mitral and TV repairs [60].
The CLASP TR Early Feasibility Study, a single-arm, multicenter, prospective study, assessed the 1-year outcomes of the Edwards PASCAL transcatheter valve repair system in patients with severe or greater TR who remained symptomatic despite medical treatment. The study involved 65 patients with a mean age of 77.4 years [61]. Initial results showed a CVS mortality of 3.1%, a stroke rate of 1.5%, and no device-related reinterventions within the first 30 days. From 30 days to one year, there were additional outcomes, including three CVS deaths (4.8%), two strokes (3.2%), and one unplanned reintervention (1.6%). By the end of the first year, TR severity had significantly decreased, with 86.0% of patients achieving moderate or less TR and all patients experiencing at least one grade reduction in TR severity. The Kaplan–Meier analysis showed freedom from all-cause mortality and heart failure hospitalization at 87.9% and 78.5%, respectively. There was a notable improvement in NYHA functional class (92% in class I or II), a 94 m increase in the 6 min walk distance, and an 18-point improvement in Kansas City Cardiomyopathy Questionnaire scores [61].
A meta-analysis performed by Bocchino et al. [62], which had fourteen studies, included more than 770 patients who underwent isolated transcatheter TV repair with a mean age of 77 years and a mean European system for cardiac operative risk evaluation score of 6.8%. Patients were followed up for a mean of 7 months. The investigator found that patients undergoing isolated transcatheter TV repair for significant TR experienced significant improvements in NYHA functional status, 6 min walking distance, and a significant reduction in TR severity [62].
In February 2024, the U.S. Food and Drug Administration (FDA) approved the Edwards EVOQUE Tricuspid Valve Replacement System, marking the first transcatheter therapy approved for TR. The EVOQUE system features a self-expanding nitinol frame with bovine pericardial leaflets and an intra-annular sealing skirt, which is delivered transfemorally via a 28F delivery system [63]. Subsequently, in April 2024, the FDA approved Abbott’s TriClip Transcatheter Edge-to-Edge Repair (TEER) System, offering a minimally invasive option for patients with symptomatic severe TR who are at an intermediate or greater risk for surgery [64]. The TriClip G4 System utilizes transcatheter edge-to-edge repair (TEER) technology, clipping portions of the tricuspid valve leaflets together to reduce regurgitation without needing open-heart surgery. Both devices represent significant advancements in the minimally invasive treatment of severe tricuspid regurgitation, offering new options for patients who are at a high surgical risk or ineligible for traditional open-heart procedures [63,64].
9. Conclusions
The management of isolated TR remains complex, given its varied etiologies and the multifaceted approach required for its diagnosis and treatment. Our findings underscore the importance of early detection and timely intervention to mitigate the progression of TR and its sequelae.
With the historical in-hospital mortality rates of 8.8–37% and 5-year mortality of 55% after isolated tricuspid valve surgeries, careful patient selection and timing of surgical intervention is needed, preferably performed at expert surgical centers. The FDA approval of Edwards EVOQUE Tricuspid Valve Replacement System and Abbott’s TriClip Transcatheter Edge-to-Edge Repair (TEER) Systems in 2024 has started a new era of less invasive and more durable, safe strategies for the management of high-risk isolated TR patients. Future research should focus on refining multimodality imaging evaluation and risk stratification, optimizing timing for intervention, randomized controlled trials comparing surgical, transcatheter, and medical options, and developing personalized treatment strategies to enhance patients’ survival and quality of life to improve their clinical outcomes.
Author Contributions
M.S.: conceptualization, methodology, writing—original draft preparation, writing—review and editing; J.E.R.: methodology, writing—original draft preparation, writing—review and editing; M.A.M.: writing—original draft preparation, writing—review and editing; A.D.A.: writing—original draft preparation, writing—review and editing; E.H.: writing—original draft preparation, writing—review and editing; T.K.M.W.: conceptualization, methodology, writing—original draft preparation, writing—review and editing, supervision, project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable (N/A) as this is a review article and does not involve participants or require ethics approval.
Informed Consent Statement
Not applicable (N/A) as this is a review article and does not involve participants or require individual consent for publication.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Welle, G.A.; Hahn, R.T.; Lindenfeld, J.; Lin, G.; Nkomo, V.T.; Hausleiter, J.; Lurz, P.C.; Pislaru, S.V.; Davidson, C.J.; Eleid, M.F. New Approaches to Assessment and Management of Tricuspid Regurgitation Before Intervention. JACC Cardiovasc. Interv. 2024, 17, 837–858. [Google Scholar] [CrossRef]
- Sala, A.; Lorusso, R.; Alfieri, O. Isolated tricuspid regurgitation: A plea for early correction. Int. J. Cardiol. 2022, 353, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Fender, E.A.; Zack, C.J.; Nishimura, R.A. Isolated tricuspid regurgitation: Outcomes and therapeutic interventions. Heart 2018, 104, 798–806. [Google Scholar] [CrossRef] [PubMed]
- Moyssakis, I.; Tektonidou, M.G.; Vasilliou, V.A.; Samarkos, M.; Votteas, V.; Moutsopoulos, H.M. Libman-Sacks endocarditis in systemic lupus erythematosus: Prevalence, associations, and evolution. Am. J. Med. 2007, 120, 636–642. [Google Scholar] [CrossRef]
- Iftikhar, S.F.; Alahmadi, M.H.; Ahmad, F. Tricuspid Valve Endocarditis; StatPearls: Tampa, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538423/ (accessed on 13 April 2025).
- Sala, A.; Hahn, R.T.; Kodali, S.K.; Mack, M.J.; Maisano, F. Tricuspid Valve Regurgitation: Current Understanding and Novel Treatment Options. J. Soc. Cardiovasc. Angiogr. Interv. 2023, 2, 101041. [Google Scholar] [CrossRef] [PubMed]
- Addetia, K.; Harb, S.C.; Hahn, R.T.; Kapadia, S.; Lang, R.M. Cardiac Implantable Electronic Device Lead-Induced Tricuspid Regurgitation. JACC Cardiovasc. Imaging 2019, 12, 622–636. [Google Scholar] [CrossRef]
- Neumann, S.; Rüffer, A.; Sachweh, J.; Biermann, D.; Herrmann, J.; Jerosch-Herold, M.; Hazekamp, M.; Sinning, C.; Zengin, E.; Blankenberg, S. Narrative review of Ebstein’s anomaly beyond childhood: Imaging, surgery, and future perspectives. Cardiovasc. Diagn. Ther. 2021, 11, 1310. [Google Scholar] [CrossRef]
- Mas, P.T.; Rodríguez-Palomares, J.F.; Antunes, M.J. Secondary tricuspid valve regurgitation: A forgotten entity. Heart 2015, 101, 1840–1848. [Google Scholar]
- Wang, T.K.M.; Unai, S.; Xu, B. Contemporary review in the multi-modality imaging evaluation and management of tricuspid regurgitation. Cardiovasc. Diagn. Ther. 2021, 11, 804–817. [Google Scholar] [CrossRef]
- Wang, T.K.M.; Akyuz, K.; Mentias, A.; Kirincich, J.; Duran Crane, A.; Xu, S.; Popovic, Z.B.; Xu, B.; Gillinov, A.M.; Pettersson, G.B. Contemporary Etiologies, Outcomes, and Novel Risk Score for Isolated Tricuspid Regurgitation. JACC Cardiovasc. Imaging 2022, 15, 731–744. [Google Scholar] [CrossRef]
- Vieitez, J.M.; Monteagudo, J.M.; Mahia, P.; Perez, L.; Lopez, T.; Marco, I.; Perone, F.; González, T.; Sitges, M.; Bouzas, A. New insights of tricuspid regurgitation: A large-scale prospective cohort study. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Topilsky, Y.; Maltais, S.; Medina Inojosa, J.; Oguz, D.; Michelena, H.; Maalouf, J.; Mahoney, D.W.; Enriquez-Sarano, M. Burden of Tricuspid Regurgitation in Patients Diagnosed in the Community Setting. JACC Cardiovasc. Imaging 2019, 12, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., III; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, E72–E227. [Google Scholar]
- Izumi, C.; Miyake, M.; Takahashi, S.; Matsutani, H.; Hashiwada, S.; Kuwano, K.; Hayashi, H.; Nakajima, S.; Nishiga, M.; Hanazawa, K.; et al. Progression of isolated tricuspid regurgitation late after left-sided valve surgery. Clinical features and mechanisms. Circ. J. 2011, 75, 2902–2907. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Song, J.M.; Park, J.P.; Lee, J.W.; Kang, D.H.; Song, J.K. Long-term prognosis of isolated significant tricuspid regurgitation. Circ. J. 2010, 74, 375–380. [Google Scholar] [CrossRef]
- Haywood, N.; Mehaffey, J.H.; Chancellor, W.Z.; Beller, J.P.; Speir, A.; Quader, M.; Yarboro, L.T.; Teman, N.R.; Ailawadi, G. Burden of Tricuspid Regurgitation in Patients Undergoing Coronary Artery Bypass Grafting. Ann. Thorac. Surg. 2021, 111, 44–50. [Google Scholar] [CrossRef]
- Luo, Y.; Leng, J.; Shi, R.; Jiang, Y.; Chen, D.; Wu, Q.; Tie, H.; Wang, Z.; Zhao, Y.; Li, X.; et al. Concomitant tricuspid valve surgery in patients undergoing left ventricular assist device: A systematic review and meta-analysis. Int. J. Surg. 2024, 110, 3039–3049. [Google Scholar] [CrossRef]
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., III; Guyton, R.A.; O’Gara, P.T.; Ruiz, C.E.; Skubas, N.J.; Sorajja, P.; et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: Executive summary: A report of the american college of cardiology/american heart association task force on practice guidelines. Circulation 2014, 129, 2440–2492. [Google Scholar] [CrossRef]
- Maeder, M.T.; Holst, D.P.; Kaye, D.M. Tricuspid regurgitation contributes to renal dysfunction in patients with heart failure. J. Card. Fail. 2008, 14, 824–830. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Zaidi, A.; Oxborough, D.; Augustine, D.X.; Bedair, R.; Harkness, A.; Rana, B.; Robinson, S.; Badano, L.P.; Education Committee of the British Society of Echocardiography. Echocardiographic assessment of the tricuspid and pulmonary valves: A practical guideline from the British Society of Echocardiography. Echo Res. Pract. 2020, 7, G95–G122. [Google Scholar] [CrossRef] [PubMed]
- Peri, Y.; Sadeh, B.; Sherez, C.; Hochstadt, A.; Biner, S.; Aviram, G.; Ingbir, M.; Nachmany, I.; Topaz, G.; Flint, N.; et al. Quantitative assessment of effective regurgitant orifice: Impact on risk stratification, and cut-off for severe and torrential tricuspid regurgitation grade. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Karamitsos, T.D.; Francis, J.M.; Myerson, S.; Selvanayagam, J.B.; Neubauer, S. The role of cardiovascular magnetic resonance imaging in heart failure. JACC 2009, 54, 1407–1424. [Google Scholar] [CrossRef]
- Wang, T.K.M.; Akyuz, K.; Reyaldeen, R.; Griffin, B.P.; Popovic, Z.B.; Pettersson, G.B.; Gillinov, A.M.; Flamm, S.D.; Xu, B.; Desai, M.Y.; et al. Prognostic Value of Complementary Echocardiography and Magnetic Resonance Imaging Quantitative Evaluation for Isolated Tricuspid Regurgitation. Circ. Cardiovasc. Imaging 2021, 14, E012211. [Google Scholar] [CrossRef] [PubMed]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef]
- Lancellotti, P.; Tribouilloy, C.; Hagendorff, A.; Popescu, B.A.; Edvardsen, T.; Pierard, L.A.; Badano, L.; Zamorano, J.L. Recommendations for the echocardiographic assessment of native valvular regurgitation: An executive summary from the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 611–644. [Google Scholar] [CrossRef]
- Luxford, J.; Bassin, L.; D’Ambra, M. Echocardiography of the tricuspid valve: Acknowledgements. Ann. Cardiothorac. Surg. 2017, 6, 223. [Google Scholar] [CrossRef]
- Puchalski, M.D.; Lui, G.K.; Miller-Hance, W.C.; Brook, M.M.; Young, L.T.; Bhat, A.; Roberson, D.A.; Mercer-Rosa, L.; Miller, O.I.; Parra, D.A.; et al. Guidelines for Performing a Comprehensive Transesophageal Echocardiographic: Examination in Children and All Patients with Congenital Heart Disease: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2019, 32, 173–215. [Google Scholar] [CrossRef]
- Jost, Z.T.; Nooli, N.P.; Ali, A.E.; Jaganathan, V.; Nanda, N.C. Three-dimensional echocardiography of the tricuspid valve. Front. Cardiovasc. Med. 2023, 10, 1114715. [Google Scholar] [CrossRef]
- Hahn, R.T. State-of-the-Art Review of Echocardiographic Imaging in the Evaluation and Treatment of Functional Tricuspid Regurgitation. Circ. Cardiovasc. Imaging 2016, 9, e005332. [Google Scholar] [CrossRef]
- Ahn, Y.; Koo, H.J.; Kang, J.W.; Yang, D.H. Tricuspid Valve Imaging and Right Ventricular Function Analysis Using Cardiac CT and MRI. Korean J. Radiol. 2021, 22, 1946–1963. [Google Scholar] [CrossRef] [PubMed]
- Winkel, M.G.; Brugger, N.; Khalique, O.K.; Gräni, C.; Huber, A.; Pilgrim, T.; Billinger, M.; Windecker, S.; Hahn, R.T.; Praz, F.; et al. Imaging and Patient Selection for Transcatheter Tricuspid Valve Interventions. Front. Cardiovasc. Med. 2020, 7, 511948. [Google Scholar] [CrossRef]
- Mastroiacovo, G.; Bonomi, A.; Ludergnani, M.; Franchi, M.; Maragna, R.; Pirola, S.; Baggiano, A.; Caglio, A.; Pontone, G.; Polvani, G.; et al. Is EuroSCORE II still a reliable predictor for cardiac surgery mortality in 2022? A retrospective study study. Eur. J. Cardio-Thoracic Surg. 2023, 64, ezad294. [Google Scholar] [CrossRef] [PubMed]
- Dreyfus, J.; Galloo, X.; Taramasso, M.; Heitzinger, G.; Benfari, G.; Kresoja, K.P.; Juarez-Casso, F.; Omran, H.; Bohbot, Y.; Iliadis, C.; et al. TRI-SCORE and benefit of intervention in patients with severe tricuspid regurgitation. Eur. Heart J. 2024, 45, 586–597. [Google Scholar] [CrossRef]
- Dreyfus, J.; Audureau, E.; Bohbot, Y.; Coisne, A.; Lavie-Badie, Y.; Bouchery, M.; Flagiello, M.; Bazire, B.; Eggenspieler, F.; Viau, F.; et al. TRI-SCORE: A new risk score for in-hospital mortality prediction after isolated tricuspid valve surgery. Eur. Heart J. 2022, 43, 654–662. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; Dulgheru, R.E.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 2015, 36, 3075–3128. [Google Scholar]
- Kusumoto, F.M.; Schoenfeld, M.H.; Wilkoff, B.L.; Berul, C.I.; Birgersdotter-Green, U.M.; Carrillo, R.; Cha, Y.M.; Clancy, J.; Deharo, J.C.; Ellenbogen, K.A.; et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm 2017, 14, e503–e551. [Google Scholar] [CrossRef]
- Hahn, R.T.; Lawlor, M.K.; Davidson, C.J.; Badhwar, V.; Sannino, A.; Spitzer, E.; Lurz, P.; Lindman, B.R.; Topilsky, Y.; Baron, S.J.; et al. Tricuspid Valve Academic Research Consortium Definitions for Tricuspid Regurgitation and Trial Endpoints. JACC 2023, 82, 1711–1735. [Google Scholar] [CrossRef]
- Ricci, F.; Bufano, G.; Galusko, V.; Sekar, B.; Benedetto, U.; Awad, W.I.; Dreyfus, G.D.; Dreyfus, X.; Van den Eynde, J.; De Bonis, M.; et al. Tricuspid regurgitation management: A systematic review of clinical practice guidelines and recommendations. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 8, 238–248. [Google Scholar] [CrossRef]
- Wang, T.K.M.; Griffin, B.P.; Miyasaka, R.; Xu, B.; Popovic, Z.B.; Pettersson, G.B.; Gillinov, A.M.; Desai, M.Y. Isolated surgical tricuspid repair versus replacement: Meta-analysis of 15 069 patients. Open Heart 2020, 7, e001227. [Google Scholar] [CrossRef]
- Vassileva, C.M.; Shabosky, J.; Boley, T.; Markwell, S.; Hazelrigg, S. Tricuspid valve surgery: The past 10 years from the Nationwide Inpatient Sample (NIS) database. J. Thorac. Cardiovasc. Surg. 2012, 143, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Jang, M.J.; Kim, K.H.; Hwang, H.Y. Repair versus replacement for the surgical correction of tricuspid regurgitation: A meta-analysis. European Eur. J. Cardio-Thoracic Surg. 2018, 53, 748–755. [Google Scholar] [CrossRef] [PubMed]
- Treatment Options for Severe Functional Tricuspid Regurgitation. Available online: https://www.congenitalcardiologytoday.com/post/treatment-options-for-severe-functional-tricuspid-regurgitation-indications-techniques-and-current (accessed on 16 March 2025).
- Pfannmüller, B.; Misfeld, M.; Borger, M.A.; Etz, C.D.; Funkat, A.K.; Garbade, J.; Mohr, F.W. Isolated reoperative minimally invasive tricuspid valve operations. Ann. Thorac. Surg. 2012, 94, 2005–2010. [Google Scholar] [CrossRef] [PubMed]
- Ren, W.J.; Zhang, B.G.; Liu, J.S.; Qian, Y.J.; Guo, Y.Q. Outcomes of tricuspid annuloplasty with and without prosthetic rings: A retrospective follow-up study. J. Cardiothorac. Surg. 2015, 10, 81. [Google Scholar] [CrossRef][Green Version]
- Pfannmüller, B.; Doenst, T.; Eberhardt, K.; Seeburger, J.; Borger, M.A.; Mohr, F.W. Increased risk of dehiscence after tricuspid valve repair with rigid annuloplasty rings. J. Thorac. Cardiovasc. Surg. 2012, 143, 1050–1055. [Google Scholar] [CrossRef]
- Lee, J. Tensile Viscoelastic Properties of Bioprosthetic Heart Valve Materials And of The Pericardium. Ph.D. Thesis, Western University, London, ON, Canada, 1982. [Google Scholar]
- Patlolla, S.H.; Saran, N.; Schaff, H.V.; Crestanello, J.; Pochettino, A.; Stulak, J.M.; Greason, K.L.; King, K.S.; Lee, A.T.; Daly, R.C.; et al. Prosthesis choice for tricuspid valve replacement: Comparison of clinical and echocardiographic outcomes. J. Thorac. Cardiovasc. Surg. 2024, 167, 668–679.e2. [Google Scholar] [CrossRef]
- Cardiopulmonary Bypass—StatPearls—NCBI Bookshelf. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482190/ (accessed on 16 March 2025).
- Roberts, A.; Duncan, E.C.; Hargrave, P.; Kingery, D.R.; Barnes, J.; Horstemeyer, D.L.; Stahl, R.F. Complications of Cardiopulmonary Bypass From an Anesthesia Perspective: A Clinical Review. HCA Healthc. J. Med. 2023, 4, 3–21. [Google Scholar] [CrossRef]
- Gaudino, M.; Angelini, G.D.; Antoniades, C.; Bakaeen, F.; Benedetto, U.; Calafiore, A.M.; Di Franco, A.; Di Mauro, M.; Fremes, S.E.; Girardi, L.N.; et al. Off-Pump Coronary Artery Bypass Grafting: 30 Years of Debate. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2018, 7, e009934. [Google Scholar] [CrossRef]
- Sauvé, J.A.; Wu, Y.S.; Ghatanatti, R.; Zacharias, J. Minimal Access Tricuspid Valve Surgery. J. Cardiovasc. Dev. Dis. 2023, 10, 118. [Google Scholar] [CrossRef]
- Saran, N.; Dearani, J.A.; Said, S.M.; Greason, K.L.; Pochettino, A.; Stulak, J.M.; Maltais, S.; Cicek, S.; Crestanello, J.; Daly, R.C.; et al. Long-term outcomes of patients undergoing tricuspid valve surgery†. Eur. J. Cardio-Thoracic Surg. 2019, 56, 950–958. [Google Scholar] [CrossRef]
- Andreas, M.; Burri, H.; Praz, F.; Soliman, O.; Badano, L.; Barreiro, M.; Cavalcante, J.L.; De Potter, T.; Doenst, T.; Friedrichs, K.; et al. Tricuspid valve disease and cardiac implantable electronic devices. Eur. Heart J. 2023, 45, 346–365. [Google Scholar] [CrossRef] [PubMed]
- Gabriels, J.K.; Schaller, R.D.; Koss, E.; Rutkin, B.J.; Carrillo, R.G.; Epstein, L.M. Lead management in patients undergoing percutaneous tricuspid valve replacement or repair: A ‘heart team’ approach. Europace 2023, 25, euad300. [Google Scholar] [CrossRef] [PubMed]
- Kolte, D.; Elmariah, S. Transcatheter Tricuspid Valve Therapy. Curr. Treat Options Cardiovasc. Med. 2019, 21, 26. [Google Scholar] [CrossRef] [PubMed]
- TRIGISTRY: Benefit of Isolated Surgical Valve Repair or Replacement for Functional Tricuspid Regurgitation and Long-Term Outcomes Stratified by the TRI-SCORE. Available online: https://www.pcronline.com/News/Whats-new-on-PCRonline/2024/ESC/TRIGISTRY-Benefit-of-isolated-surgical-valve-repair-or-replacement-for-functional-tricuspid-regurgitation-and-long-term-outcomes-stratified-by-the-TRI-SCORE (accessed on 13 April 2025).
- Orban, M.; Besler, C.; Braun, D.; Nabauer, M.; Zimmer, M.; Noack, T.; Mehilli, J.; Hagl, C.; Seeburger, J.; Borger, M.; et al. Six-month outcome after transcatheter edge-to-edge repair of severe tricuspid regurgitation in patients with heart failure. Eur. J. Heart Fail. 2018, 20, 1055–1062. [Google Scholar] [CrossRef]
- Orban, M.; Rommel, K.P.; Ho, E.C.; Unterhuber, M.; Pozzoli, A.; Connelly, K.A.; Deseive, S.; Besler, C.; Ong, G.; Braun, D.; et al. Transcatheter Edge-to-Edge Tricuspid Repair for Severe Tricuspid Regurgitation Reduces Hospitalizations for Heart Failure. JACC Heart Fail. 2020, 8, 265–276. [Google Scholar] [CrossRef]
- Kodali, S.K.; Hahn, R.T.; Davidson, C.J.; Narang, A.; Greenbaum, A.; Gleason, P.; Zahr, F.; Chadderdon, S.; Smith, R.; Grayburn, P.A.; et al. 1-Year Outcomes of Transcatheter Tricuspid Valve Repair. JACC 2023, 81, 1766–1776. [Google Scholar] [CrossRef]
- Bocchino, P.P.; Angelini, F.; Vairo, A.; Andreis, A.; Fortuni, F.; Franchin, L.; Frea, S.; Raineri, C.; Pidello, S.; Conrotto, F.; et al. Clinical Outcomes Following Isolated Transcatheter Tricuspid Valve Repair: A Meta-Analysis and Meta-Regression Study. JACC Cardiovasc. Interv. 2021, 14, 2285–2295. [Google Scholar] [CrossRef]
- Edwards EVOQUE Tricuspid Valve Replacement System—P230013|FDA. Available online: https://www.fda.gov/medical-devices/recently-approved-devices/edwards-evoque-tricuspid-valve-replacement-system-p230013 (accessed on 5 March 2025).
- FDA Approves First Transcatheter Tricuspid Valve Replacement Device|tctmd.com. Available online: https://www.tctmd.com/news/fda-approves-first-transcatheter-tricuspid-valve-replacement-device (accessed on 5 March 2025).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).