Prophylactic and Therapeutic Indications for Third Molar Extractions as Compared to Observation and Conservative Management: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
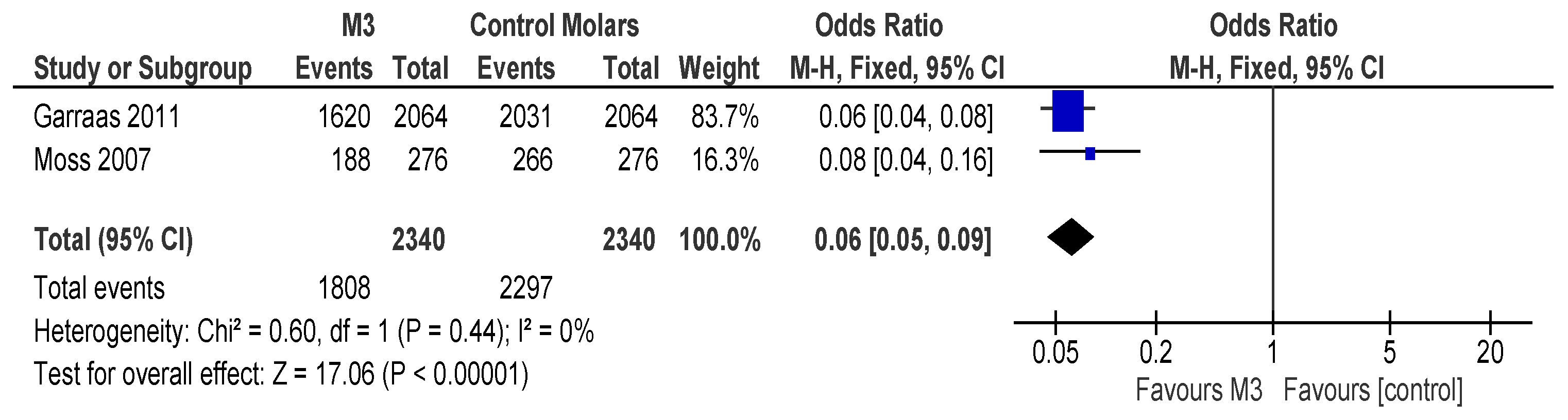
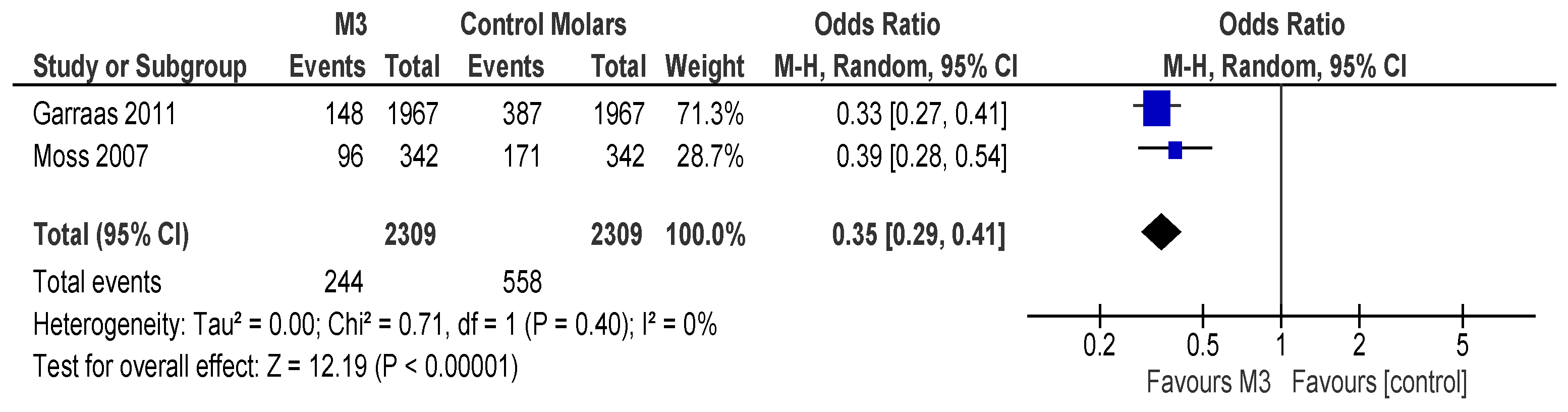
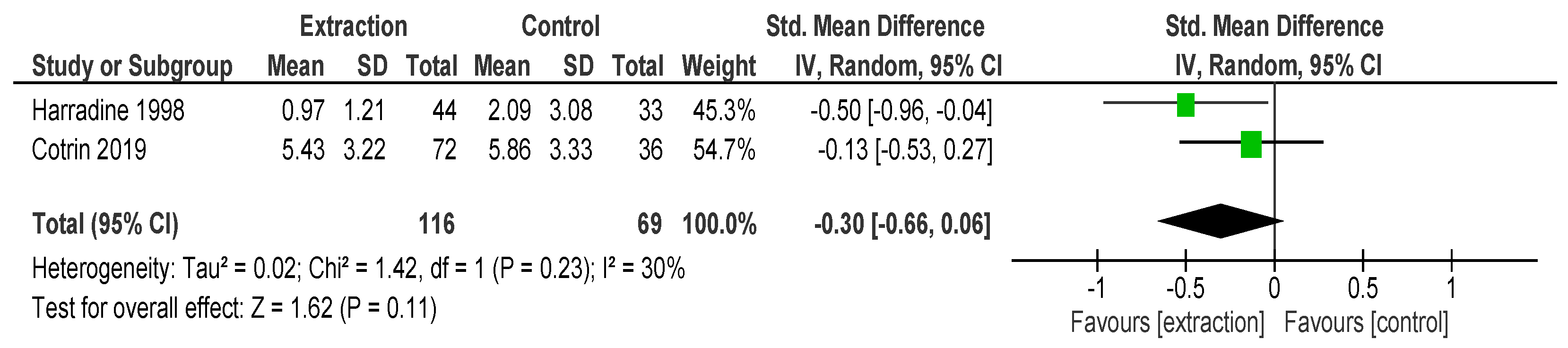
2.1. Guidelines Followed
2.2. Search Strategy
2.3. Inclusion and Exclusion CRITERIA
2.4. Data Extraction
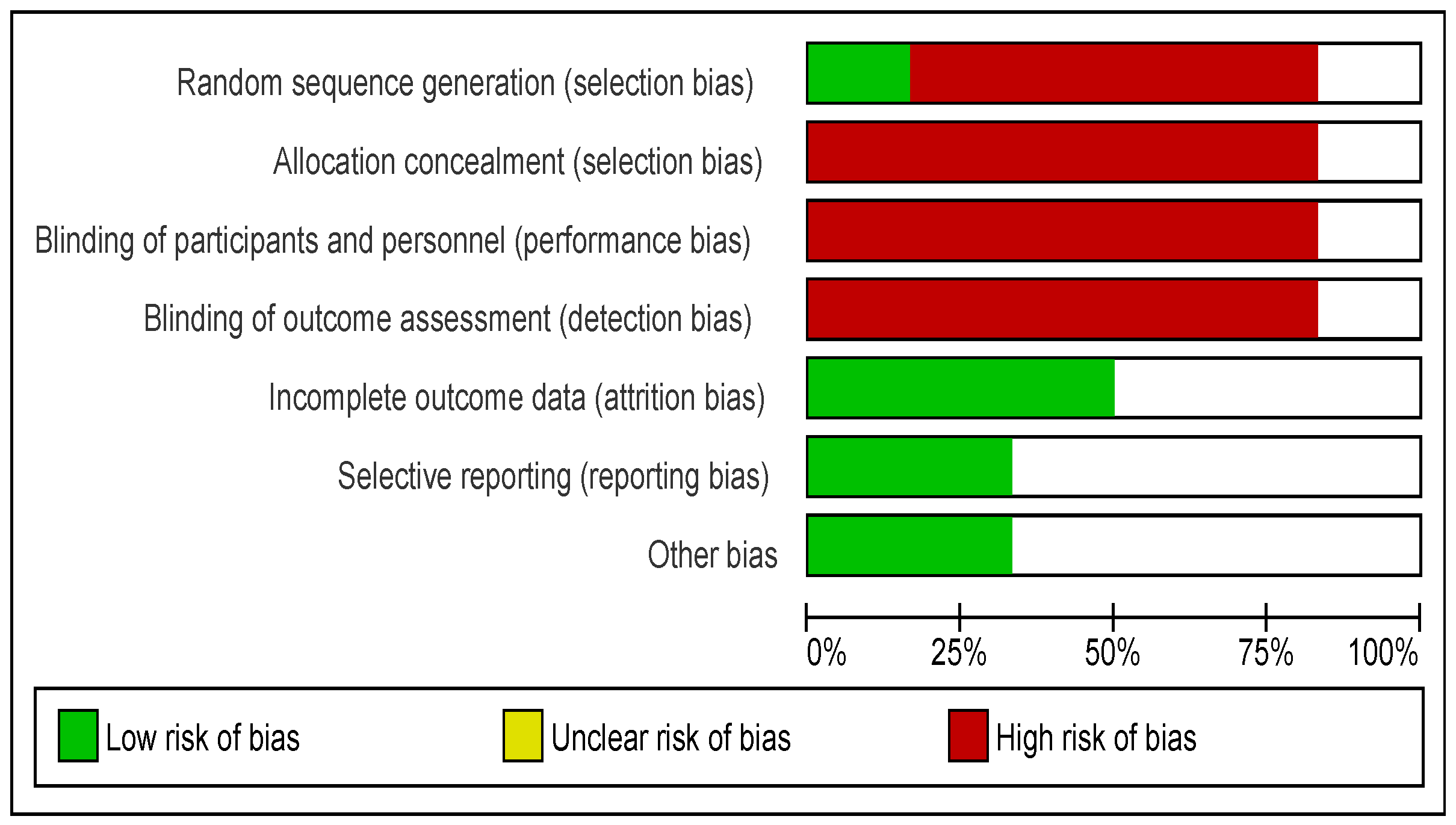
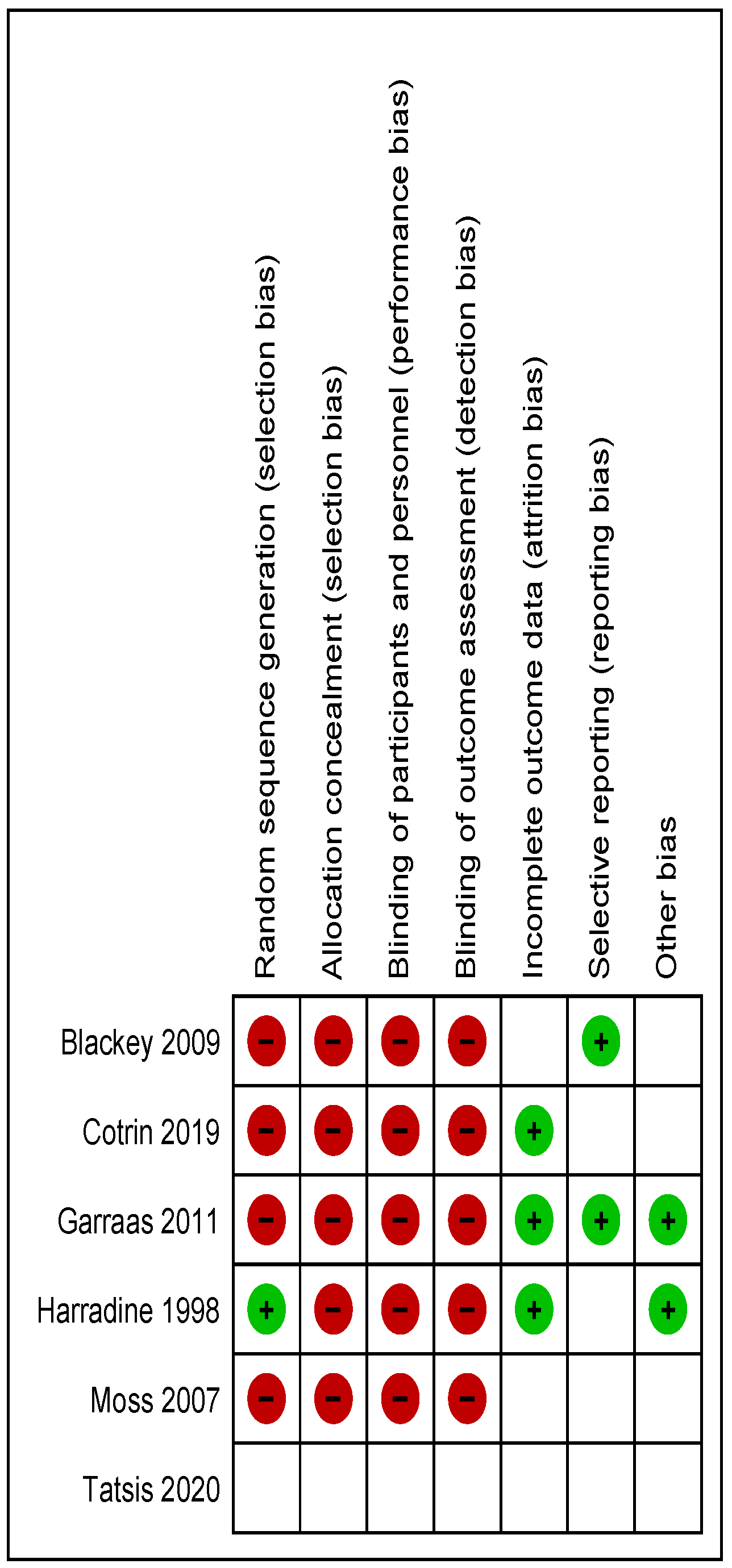
2.5. Risk of Bias and Study Quality Assessment
2.6. Statistical Analysis
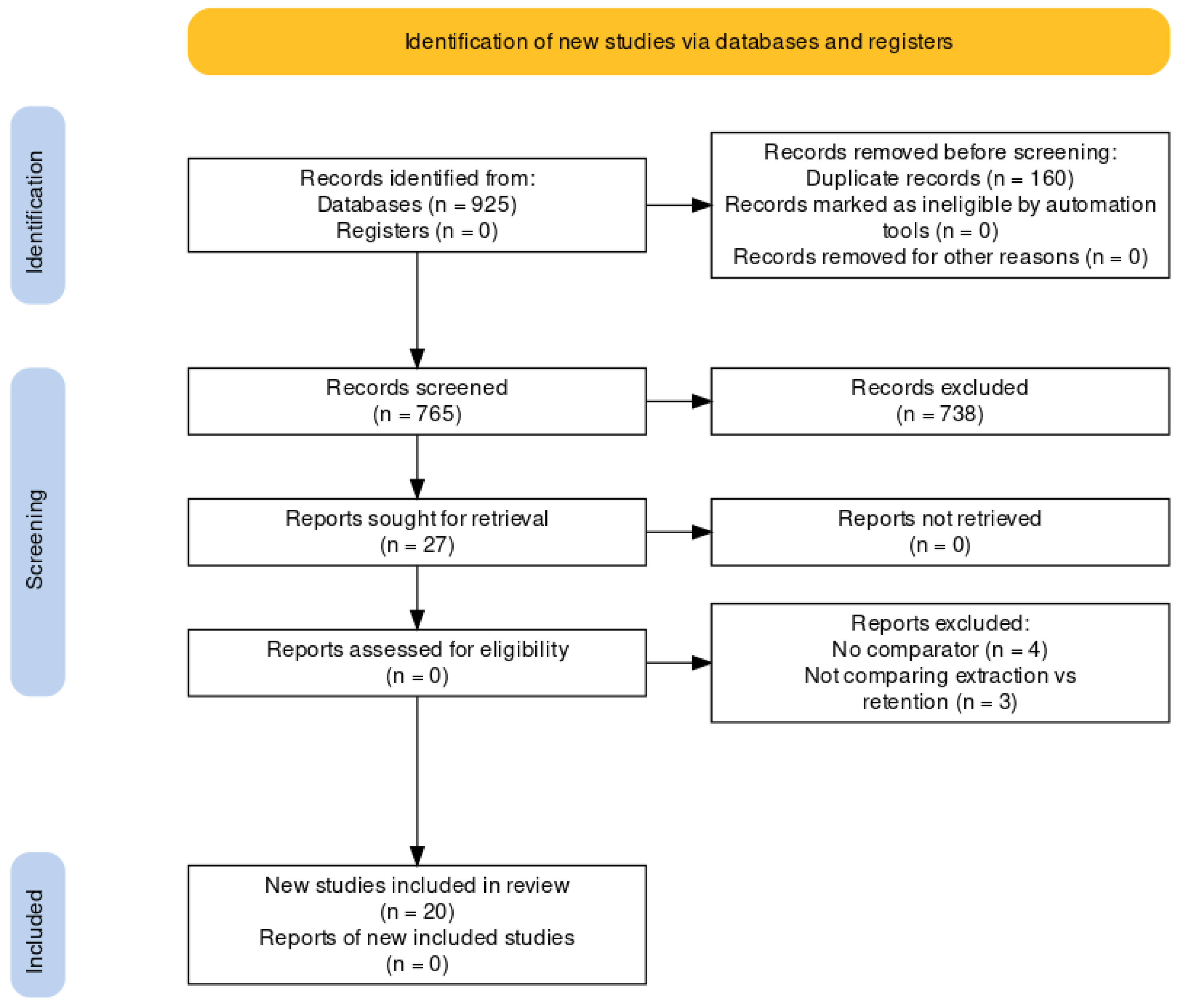
3. Electronic Search
4. Results
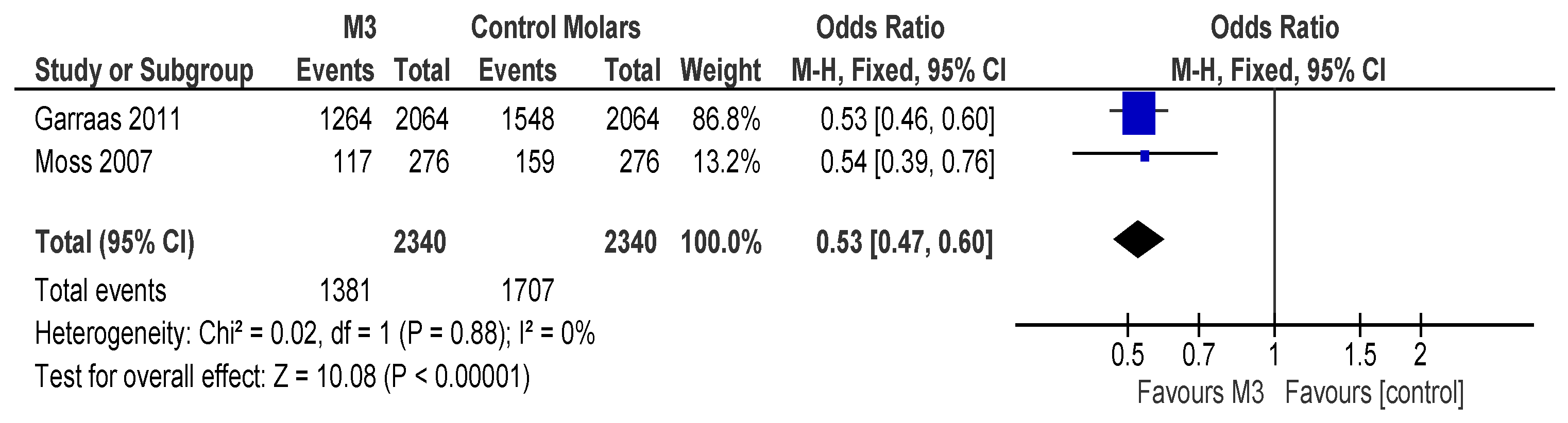
Description of Results from Literature Search
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anjrini, A.A.; Kruger, E.; Tennant, M. Cost effectiveness modelling of a “watchful monitoring strategy” for impacted third molars vs prophylactic removal under GA: An Australian perspective. Br. Dent. J. 2015, 219, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Avellaneda-Gimeno, V.; Figueiredo, R.; Valmaseda-Castellon, E. Quality of life after upper third molar removal: A prospective longitudinal study. Med. Oral Patol. Oral Cirugia Bucal 2017, 22, e759–e766. [Google Scholar] [CrossRef] [PubMed]
- Blakey, G.H.; Parker, D.W.; Hull, D.J.; White, R.P.; Offenbacher, S.; Phillips, C.; Haug, R.H. Impact of Removal of Asymptomatic Third Molars on Periodontal Pathology. J. Oral Maxillofac. Surg. 2009, 67, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Chou, Y.; Ho, P.; Ho, K.; Wang, W.; Hu, K. Association between the eruption of the third molar and caries and periodontitis distal to the second molars in elderly patients. Kaohsiung J. Med. Sci. 2017, 33, 246–251. [Google Scholar] [CrossRef]
- Chuang, S.-K.; Perrott, D.H.; Susarla, S.M.; Dodson, T.B. Risk Factors for Inflammatory Complications Following Third Molar Surgery in Adults. J. Oral Maxillofac. Surg. 2008, 66, 2213–2218. [Google Scholar] [CrossRef]
- Cotrin, P.; Freitas, K.M.S.; Freitas, M.R.; Valarelli, F.P.; Cançado, R.H.; Janson, G. Evaluation of the influence of mandibular third molars on mandibular anterior crowding relapse. Acta Odontol. Scand. 2020, 78, 297–302. [Google Scholar] [CrossRef]
- Liedholm, R.; Knutsson, K.; Norlund, A. Economic aspects of mandibular third molar surgery. Br. Dent. J. 2010, 208, 211. [Google Scholar] [CrossRef]
- Fernandes, M.J.; Ogden, G.R.; Pitts, N.B.; Ogston, S.A.; Ruta, D.A. Actuarial life-table analysis of lower impacted wisdom teeth in general dental practice. Community Dent. Oral Epidemiol. 2010, 38, 58–67. [Google Scholar] [CrossRef]
- Garaas, R.; Moss, K.L.; Fisher, E.L.; Wilson, G.; Offenbacher, S.; Beck, J.D.; White, R.P. Prevalence of visible third molars with caries experience or periodontal pathology in middle-aged and older Americans. J. Oral Maxillofac. Surg. 2011, 69, 463–470. [Google Scholar] [CrossRef]
- Gelesko, S.; Blakey, G.H.; Partrick, M.; Hill, D.L.; White, R.P.; Offenbacher, S.; Phillips, C.; Haug, R.H. Comparison of Periodontal Inflammatory Disease in Young Adults with and Without Pericoronitis Involving Mandibular Third Molars. J. Oral Maxillofac. Surg. 2009, 67, 134–139. [Google Scholar] [CrossRef]
- Gursoytrak, B.; Kocaturk, O.; Koparal, M.; Gulsun, B. Assessment of Effect of Submucosal Injection of Dexmedetomidine on Postoperative Symptoms. J. Oral Maxillofac. Surg. 2020, 78, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Harradine, N.W.; Pearson, M.H.; Toth, B. The effect of extraction of third molars on late lower incisor crowding: A randomized controlled trial. Br. J. Orthod. 1998, 25, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Hounsome, J.; Pilkington, G.; Mahon, J.; Boland, A.; Beale, S.; Kotas, E.; Renton, T.; Dickson, R. Prophylactic removal of impacted mandibular third molars: A systematic review and economic evaluation. Health Technol. Assess. 2020, 24, 1–115. [Google Scholar] [CrossRef] [PubMed]
- Worrall, S.; Riden, K.; Haskell, R.; Corrigan, A.M. UK National Third Molar project: The initial report. Br. J. Oral Maxillofac. Surg. 1998, 36, 14–18. [Google Scholar] [CrossRef]
- Huang, G.J.; Cunha-Cruz, J.; Rothen, M.; Spiekerman, C.; Drangsholt, M.; Anderson, L.; Roset, G.A. A prospective study of clinical outcomes related to third molar removal or retention. Am. J. Public Health 2014, 104, 728–734. [Google Scholar] [CrossRef]
- Leechanavanichpan, P.; Rodanant, P.; Leelarungsun, R.; Wongsirichat, N. Postoperative Pain Perception and Patient’s Satisfaction After Mandibular Third Molar Surgery by Primary Closure with Distal Wedge Surgery. J. Clin. Med. Res. 2019, 11, 489–494. [Google Scholar] [CrossRef]
- Mann, A.; Scott, J. Coronectomy of mandibular third molars: A systematic literature review and case studies. Aust. Dent. J. 2021, 66, 136–149. [Google Scholar] [CrossRef]
- Moss, K.L.; Beck, J.D.; Mauriello, S.M.; Offenbacher, S.; White, R.P. Third Molar Periodontal Pathology and Caries in Senior Adults. J. Oral Maxillofac. Surg. 2007, 65, 103–108. [Google Scholar] [CrossRef]
- Nunn, M.; Fish, M.D.; Garcia, R.; Kaye, E.; Figueroa, R.; Gohel, A.; Ito, M.; Lee, H.; Williams, D.; Miyamoto, T. Retained Asymptomatic Third Molars and Risk for Second Molar Pathology. J. Dent. Res. 2013, 92, 1095–1099. [Google Scholar] [CrossRef]
- Passarelli, P.C.; Lopez, M.A.; Desantis, V.; Piccirillo, G.B.; Rella, E.; Giovannini, V.; Speranza, A.; De Leonardis, M.; Manicone, P.F.; Casale, M.; et al. Quality of life of patients with mandibular third molars and mild pericoronitis. A comparison between two different treatments: Extraction or periodontal approach. Antibiotics 2020, 9, 222. [Google Scholar] [CrossRef]
- Petsos, H.; Fleige, J.; Korte, J.; Eickholz, P.; Hoffmann, T.; Borchard, R. Five-Years Periodontal Outcomes of Early Removal of Unerupted Third Molars Referred for Orthodontic Purposes. J. Oral Maxillofac. Surg. 2021, 79, 520–531. [Google Scholar] [CrossRef] [PubMed]
- Queral-Godoy, E.; Figueiredo, R.; Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Frequency and evolution of lingual nerve lesions following lower third molar extraction. J. Oral Maxillofac. Surg. 2006, 64, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Rajasuo, A.; Meurmarr, J.H.; Murtomaa, H. Periodontopathic bacteria and salivary microbes before and after extraction of partly erupted third molars. Eur. J. Oral Sci. 1993, 101, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Rood, J.P.; Shehab, B.A.A.N. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br. J. Oral Maxillofac. Surg. 1990, 28, 20–25. [Google Scholar] [CrossRef]
- Song, F.; Wilson, M.P.; Golder, S.; Kleijnen, J. The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth Rapid review. In HTA Health Technology Assessment NHS R&D HTA Programme Health Technology Assessment; National Institute for Health and Care Research: Nottingham, UK, 2000; Volume 4. [Google Scholar]
- Tomás, I.; Pereira, F.; Llucián, R.; Poveda, R.; Diz, P.; Bagán, J. Prevalence of bacteraemia following third molar surgery. Oral Dis. 2008, 14, 89–94. [Google Scholar] [CrossRef]
- Tomaszewska, A.; Sikora, M. The incidence and extraction causes of third molars among young adults in Poland. Anthr. Rev. 2019, 82, 253–263. [Google Scholar] [CrossRef]
- Türköz, Ç.; Ulusoy, Ç. Effect of premolar extraction on mandibular third molar impaction in young adults. Angle Orthod. 2013, 83, 572–577. [Google Scholar] [CrossRef]
- Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Inferior alveolar nerve damage after lower third molar surgical extraction: A prospective study of 1117 surgical extractions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2001, 92, 377–383. [Google Scholar] [CrossRef]
- van Wijk, A.; Kieffer, J.M.; Lindeboom, J.H. Effect of Third Molar Surgery on Oral Health-Related Quality of Life in the First Postoperative Week Using Dutch Version of Oral Health Impact Profile-14. J. Oral Maxillofac. Surg. 2009, 67, 1026–1031. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Louizakis, A.; Tatsis, D.; Grivas, T.; Tilaveridou, S.; Tilaveridis, I.; Kyrgidis, A. Prophylactic and Therapeutic Indications for Third Molar Extractions as Compared to Observation and Conservative Management: A Systematic Review and Meta-Analysis. Surgeries 2025, 6, 37. https://doi.org/10.3390/surgeries6020037
Louizakis A, Tatsis D, Grivas T, Tilaveridou S, Tilaveridis I, Kyrgidis A. Prophylactic and Therapeutic Indications for Third Molar Extractions as Compared to Observation and Conservative Management: A Systematic Review and Meta-Analysis. Surgeries. 2025; 6(2):37. https://doi.org/10.3390/surgeries6020037
Chicago/Turabian StyleLouizakis, Alexandros, Dimitris Tatsis, Theodoros Grivas, Sofia Tilaveridou, Ioannis Tilaveridis, and Athanassios Kyrgidis. 2025. "Prophylactic and Therapeutic Indications for Third Molar Extractions as Compared to Observation and Conservative Management: A Systematic Review and Meta-Analysis" Surgeries 6, no. 2: 37. https://doi.org/10.3390/surgeries6020037
APA StyleLouizakis, A., Tatsis, D., Grivas, T., Tilaveridou, S., Tilaveridis, I., & Kyrgidis, A. (2025). Prophylactic and Therapeutic Indications for Third Molar Extractions as Compared to Observation and Conservative Management: A Systematic Review and Meta-Analysis. Surgeries, 6(2), 37. https://doi.org/10.3390/surgeries6020037






