Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature
Abstract
1. Introduction
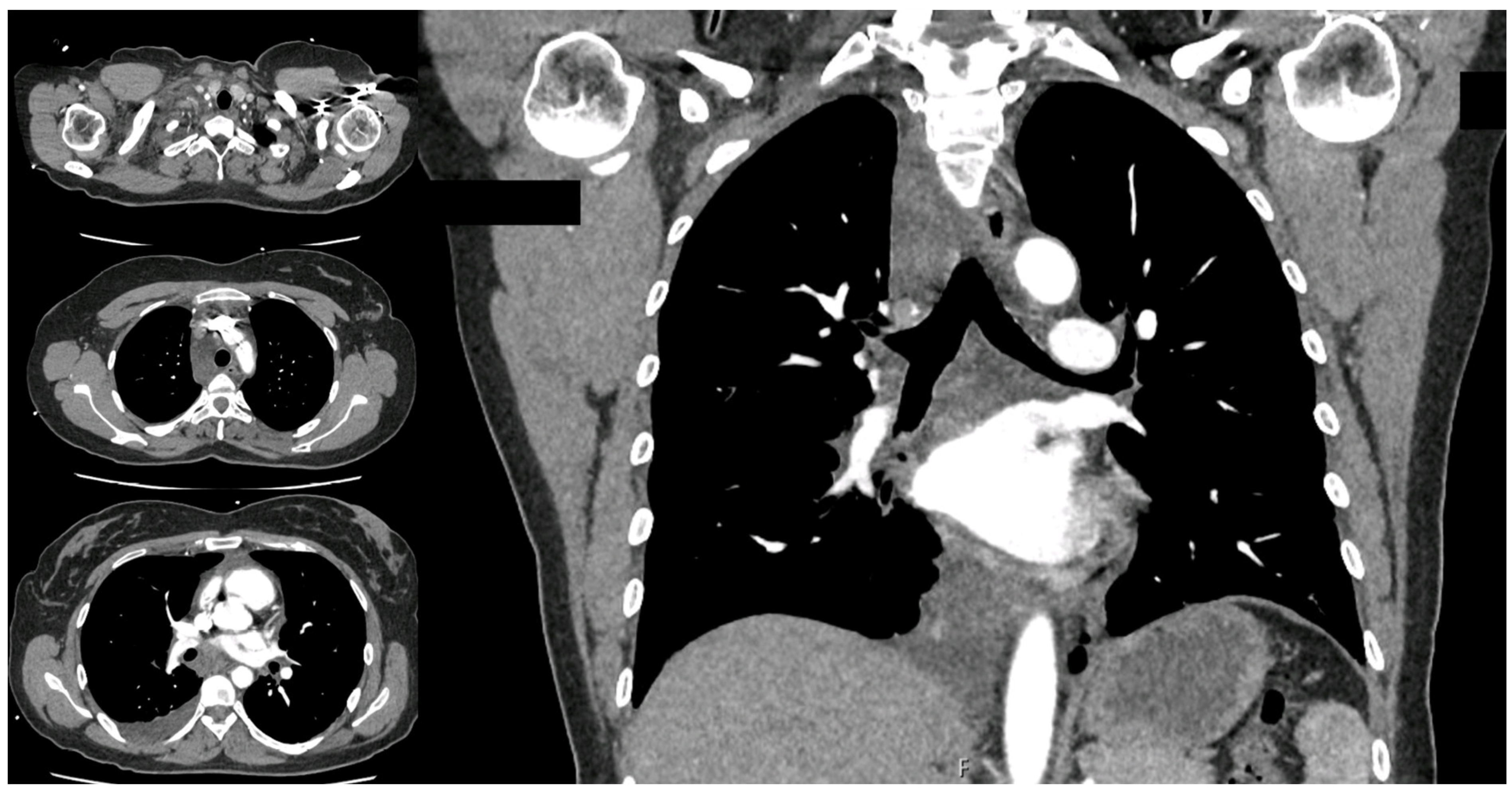
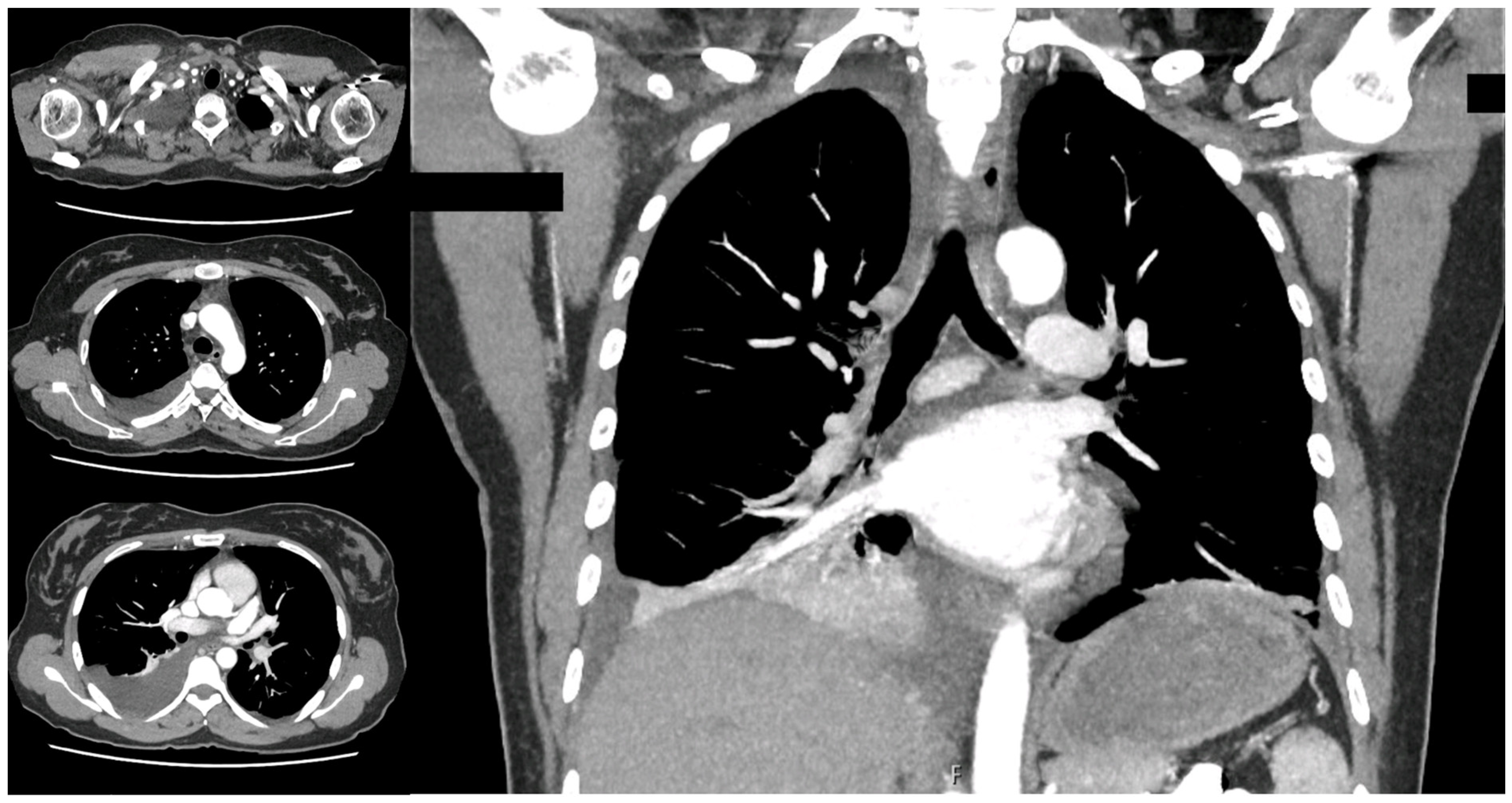
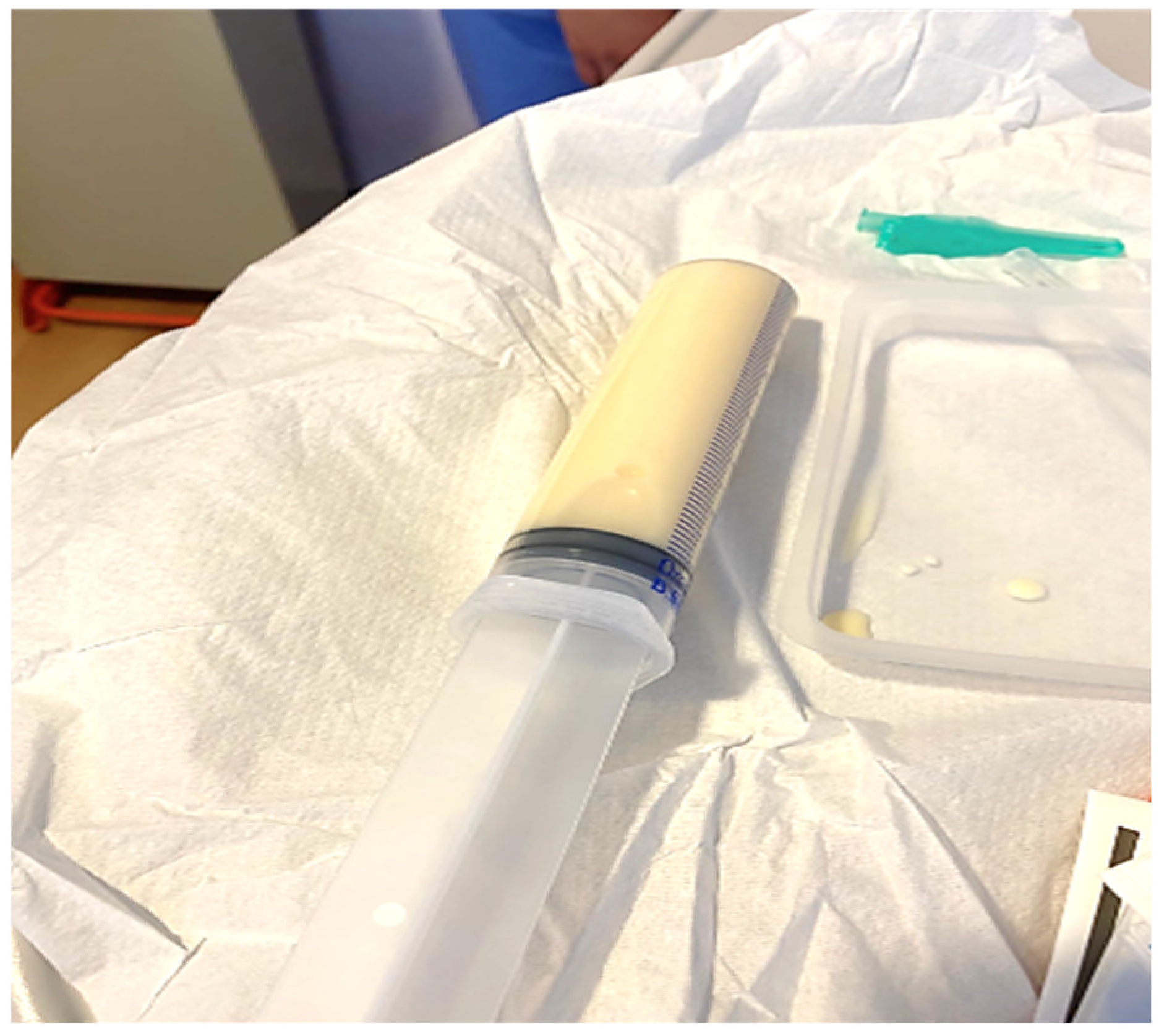
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Doerr, C.H.; Miller, D.L.; Ryu, J.H. Chylothorax. Semin. Respir. Crit. Care Med. 2001, 22, 617–626. [Google Scholar] [CrossRef] [PubMed]
- Doerr, C.H.; Allen, M.S.; Nicholas, F.C. Etiology of chylothorax in 203 patients. Mayo Clin. Proc. 2005, 80, 867. [Google Scholar] [CrossRef] [PubMed]
- Bender, B.; Murthy, V.; Chamberlin, R.S. The changing management of chylothorax in in the modern era. Eur. J. Cardiothorac. Surg. 2016, 49, 18–24. [Google Scholar] [CrossRef]
- Lama, A.; Ferreiro, L.; Toubes, M.E.; Golpe, A.; Gude, F.; Álvarez-Dobaño, J.M.; González-Barcala, F.J.; San José, E.; Rodríguez-Núñez, N.; Rábade, C.; et al. Characteristics of patients with pseudochylothorax—A systematic review. J. Thorac. Dis. 2016, 8, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- Sassoon, C.S.; Light, R.W. Chylothorax and pseudochylothorax. Clin. Chest Med. 1985, 6, 163–171. [Google Scholar] [CrossRef]
- McCray, S.P.C. Nutritional management of chyle leaks: An update. Pract. Gastroentrol. Ser. 2011, 94, 12–32. [Google Scholar]
- Huggins, J.T. Chylothorax and cholesterol pleural effusion. Semin. Respir. Crit. Care Med. 2010, 31, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Riley, L.E.; Ataya, A. Clinical approach and review of causes of chylothorax. Respir. Med. 2019, 157, 7–13. [Google Scholar] [CrossRef]
- Ferrari, P.A.; Fusaro, F.; Ferrari, A.; Tamburrini, A.; Grimaldi, G.; Santoru, M.; Zappadu, S.; Tanda, E.; Nemolato, S.; Comelli, S.; et al. Refractory Chylothorax Secondary to Sizeable Azygos Vein Hemangioma: Tailored Multimodal Treatment of a Challenging Case Report. Medicina 2022, 59, 91. [Google Scholar] [CrossRef]
- McGrath, E.E.; Blades, Z.; Anderson, P.B. Chylothorax: Aetiology, diagnosis and therapeutic options. Respir. Med. 2010, 104, 1–8. [Google Scholar] [CrossRef]
- Staats, B.A.; Ellefson, R.D.; Budahn, L.L.; Dines, D.E.; Prakash, U.B.; Offord, K. The lipoprotein profile of chylous and nonchylous pleural effusion. Mayo Clin. Proc. 1980, 55, 700–704. [Google Scholar]
- Madaniah, A.A. Spontaneous idiopathic chylothorax in adults. Saudi Med. J. 2005, 26, 145–146. [Google Scholar] [PubMed]
- Cholet, C.; Delalandre, C.; Monnier-Cholley, L.; Le Pimpec-Barthes, F.; El Mouhadi, S.; Arrivé, L. Nontraumatic Chylothorax: Nonenhanced MR Lymphography. Radiographics 2020, 40, 1554–1573. [Google Scholar] [CrossRef] [PubMed]
- Savla, J.J.; Itkin, M.; Rossano, J.W.; Dori, Y. Post-Operative Chylothorax in Patients with Congenital Heart Disease. J. Am. Coll. Cardiol. 2017, 69, 2410–2422. [Google Scholar] [CrossRef] [PubMed]
- Weissler, J.M.; Cho, E.H.; Koltz, P.F.; Carney, M.J.; Itkin, M.; Laje, P.; Levin, L.S.; Dori, Y.; Kanchwala, S.K.; Kovach, S.J. Lymphovenous Anastomosis for the Treatment of Chylothorax in Infants: A Novel Microsurgical Approach to a Devastating Problem. Plast. Reconstr. Surg. 2018, 141, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- Aalami, O.O.; Allen, D.B.; Organ, C.H., Jr. Chylous ascites: A collective review. Surgery 2000, 128, 761–778. [Google Scholar] [CrossRef] [PubMed]
- Breslin, J.W.; Yang, Y.; Scallan, J.P.; Sweat, R.S.; Adderley, S.P.; Murfee, W.L. Lymphatic vessel network structure and physiology. Compr. Physiol. 2018, 9, 207–299. [Google Scholar] [PubMed]
- Torrejais, J.C.; Rau, C.B.; de Barros, J.A.; Torrejais, M.M. Spontaneous chylothorax associated with light physical activity. J. Bras. Pneumol. 2006, 32, 599–602. [Google Scholar] [CrossRef] [PubMed]
- Kolbaş, I.; Tezel, Y.; Coşgun, T.; Baysungur, V.; Tezel, C. Chylothorax Due to Weight Lifting: A Rare Etiology. South. Clin. Ist. Euras. 2020, 31, 75–77. [Google Scholar] [CrossRef]
- Akbar, S.; Advani, R.; Aggarwal, R. Bilateral spontaneous chylothorax presenting as a left-sided neck mass. BMJ Case Rep. 2021, 14, e240320. [Google Scholar] [CrossRef]
- Garcia-Aparicio, J.; Herrero-Herrero, J.-I.; Corral-Gudine, L.; Jorge-Sanchez, R.-J. Bilateral idiopathic chylothorax associated with light exercise. Resp. Med. CME 2009, 2, 68–69. [Google Scholar] [CrossRef][Green Version]
- Bottet, B.; Melki, J.; Levesque, H.; Baste, J.M.; Roussel, E.; Peillon, C. Stretching et chylothorax. Rev. Mal. Respir. 2019, 36, 742–746. [Google Scholar] [CrossRef] [PubMed]
- Bocquel, V.; Girard, P.; Fournel, P.; Vergnon, J.M. Spontaneous chylothorax. Apropos of a further case. Rev. Mal. Respir. 1997, 14, 395–396. [Google Scholar] [PubMed]
- Hematti, H.; Mehran, R.J. Anatomy of the thoracic duct. Thorac. Surg. Clin. 2011, 21, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Meade, R.H. Spontaneous chylothorax. Arch. Intern. Med. 1972, 90, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Reilly, K.M.; Tsou, F. Bilateral chylothorax: A case report following episodes of stretching. JAMA 1975, 233, 536–537. [Google Scholar] [CrossRef] [PubMed]
- Gullane, P.J.; Marsh, A.S. Bilateral spontaneous chylothorax presenting as a neck mass. J. Otolaryngol. 1984, 13, 4. [Google Scholar]
- Tankanow, L.B.; Petrozzi, C.; Ward, J.C.; Bower, G.C. Idiopathic Bilateral Chylothorax Presenting as a Left-Sided Neck Swelling. Henry Ford. Hosp. Med. J. 1986, 34, 130–131. [Google Scholar] [PubMed]
- Fehr, M.; Lehmann, T.; Kuhn, M. Idiopathic chylothorax while vacuum cleaning. Schweiz Med. Forum. 2007, 7, 630–632. [Google Scholar]
- Bellini, C.; Cabano, R.; De Angelis, L.C.; Bellini, T.; Calevo, M.G.; Gandullia, P.; Ramenghi, L.A. Octreotide for congenital and acquired chylothorax in newborns: A systematic review. J. Paediatr. Child. Health 2018, 54, 840–847. [Google Scholar] [CrossRef]
- Anger, M.; Hofmann, J.; Ruf, B.; Steinborn, M.; Reber, D.; Warncke, K.; Rieber, N. Cough-induced chylothorax in a two-year-old boy—case report and review of the literature. BMC Pediatr. 2023, 23, 416. [Google Scholar] [CrossRef] [PubMed]
- Madhavan, S.; Nakao, M. How efficacious are Octreotide and Somatostatin in the management of chylothorax in congenital cardiac surgical patients? Interact. Cardiovasc. Thorac. Surg. 2021, 33, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Al-Zubairy, S.A.; Al-Jazairi, A.S. Octreotide as a therapeutic option for management of chylothorax. Ann. Pharmacother. 2003, 37, 679–682. [Google Scholar] [CrossRef] [PubMed]
- Kalomenidis, I. Octreotide and chylothorax. Curr. Opin. Pulm. Med. 2006, 12, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Deng, X.F.; Duan, C.M.; Chen, C.; Xiang, J.L.; Lu, Y.L.; Ma, O.F. Somatostatin receptors SSTR2 and SSTR5 are expressed in the human thoracic duct. Lymphology 2011, 44, 21–28. [Google Scholar] [PubMed]
- Buettiker, V.; Hug, M.I.; Burger, R.; Baenziger, O. Somatostatin: A new therapeutic option for the treatment of chylothorax. Intensive Care Med. 2001, 27, 1083–1086. [Google Scholar] [CrossRef] [PubMed]
- Ismail, N.A.; Gordon, J.; Dunning, J. The use of octreotide in the treatment of chylothorax following cardiothoracic surgery. Interact. Cardiovasc. Thorac. Surg. 2015, 20, 848–854. [Google Scholar] [CrossRef]
- Mitchell, K.; Weiner, A.; Ramsay, P.; Sahni, M. Use of Propranolol in the Treatment of Chylous Effusions in Infants. Pediatrics 2021, 148, e2020049699. [Google Scholar] [CrossRef] [PubMed]
- Jindal, R.; Singh, J.; Garg, L.; Gupta, M. Diagnosis and management of traumatic bilateral chylothorax: A clinical conundrum. BMJ Case Rep. 2019, 12, e229400. [Google Scholar] [CrossRef] [PubMed]
- Cope, C.; Kaiser, L.R. Management of unremitting chylothorax by percutaneous embolization and blockage of retroperitoneal lymphatic vessels in 42 patients. J. Vasc. Interv. Radiol. 2002, 13, 1139–1148. [Google Scholar] [CrossRef]
- Itkin, M.; Kucharczuk, J.C.; Kwak, A.; Trerotola, S.O.; Kaiser, L.R. Nonoperative thoracic duct embolization for traumatic thoracic duct leak: Experience in 109 patients. J. Thorac. Cardiovasc. Surg. 2010, 139, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Nadolski, G.J.; Itkin, M. Thoracic duct embolization for nontraumatic chylous effusion: Experience in 34 patients. Chest 2013, 143, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Boffa, D.J.; Sands, M.J.; Rice, T.W.; Murthy, S.C.; Mason, D.P.; Geisinger, M.A.; Blackstone, E.H. A critical evaluation of a percutaneous diagnostic and treatment strategy for chylothorax after thoracic surgery. Eur. J. Cardiothorac. Surg. 2013, 33, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Laslett, D.; Trerotola, S.O.; Itkin, M. Delayed complications following technically successful thoracic duct embolization. J. Vasc. Interv. Radiol. 2012, 23, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Kim, P.H.; Tsauo, J.; Shin, J.H. Lymphatic interventions for chylothorax: A systematic review and meta-analysis. J. Vasc. Interv. Radiol. 2018, 29, 194–202. [Google Scholar] [CrossRef]
- Pamarthi, V.; Stecker, M.S.; Schenker, M.P.; Baum, R.A.; Killoran, T.P.; Han, A.S.; O’Horo, S.K.; Rabkin, D.J.; Fan, C.M. Thoracic duct embolization and disruption for treatment of chylous effusions: Experience with 105 patients. J. Vasc. Interv. Radiol. 2014, 25, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Binkert, C.A.; Yucel, E.K.; Davison, B.D.; Sugarbaker, D.J.; Baum, R.A. Percutaneous treatment of high-output chylothorax with embolization or needle disruption technique. J. Vasc. Interv. Radiol. 2005, 16, 1257–1262. [Google Scholar] [CrossRef] [PubMed]
- Jun, H.; Hur, S.; Jeong, Y.S.; Kang, C.H.; Lee, H. Thoracic duct embolization in treating postoperative chylothorax: Does bail-out retrograde access improve outcomes? Eur. Radiol. 2022, 32, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Higgins, M.C.; Park, A.W.; Angle, J.F. Chylothorax: Percutaneous Embolization of the Thoracic Duct. Oper. Tech. Thorac. Cardiovasc. Surg. 2015, 20, 402–412. [Google Scholar] [CrossRef]
- Pillay, T.G.; Singh, B. A review of traumatic chylothorax. Injury 2016, 47, 545–550. [Google Scholar] [CrossRef]
- Fernández Alvarez, J.R.; Kalache, K.D.; Graŭel, E.L. Management of spontaneous congenital chylothorax: Oral medium-chain triglycerides versus total parenteral nutrition. Am. J. Perinatol. 1999, 16, 0415–0420. [Google Scholar] [CrossRef] [PubMed]
- Seitelman, E.; Arellano, J.J.; Takabe, K.; Barrett, L.; Faust, G.; Angus, L.G. Chylothorax after blunt trauma. J. Thorac. Dis. 2012, 4, 327–330. [Google Scholar] [PubMed]
| Authors, Year | Subjects (n) | Supposed Cause | Location of Chyle Leakage | Intervention |
|---|---|---|---|---|
| Meade RH, 1972 [25] | 5 | Hyperextension of the spine | Unilateral chylothorax | N/A |
| Reilly et al., 1975 [26] | 1 | Hyperextension of the spine during stretching exercise and yawning | Bilateral chylothorax | Conservative |
| Gullane et al., 1984 [27] | 1 | Hyperextension of the spine while swimming | Bilateral chylothorax | Conservative |
| Tankanow et al., 1986 [28] | 1 | Hyperextension of the spine while climbing into a bathtub | Bilateral chylothorax | Conservative |
| Bocquel et al., 1997 [23] | 1 | Overstretch of subclavius and anterior scalenus muscle during stretching exercise | Unilateral chylothorax | Conservative |
| Torrejais et al., 2006 [18] | 1 | Hyperextension of the neck during light physical activity at a fitness center | Bilateral neck swelling and bilateral chylothorax | Conservative |
| Fehr et al., 2007 [29] | 1 | Hyperextension of the neck and overstretch of thoracic outlet during routine vacuum cleaning | Left-sided neck swelling and bilateral chylothorax | Conservative |
| Garcìa-Aparicio et al., 2009 [21] | 1 | Hyperextension of the neck during light physical activity | Bilateral chylothorax | Conservative |
| Bottet et al., 2019 [22] | 1 | Overstretch of subclavius and anterior scalenus muscle during stretching exercise | Bilateral chylothorax | Conservative |
| Kolbas et al., 2020 [19] | 1 | Overstretch of subclavius and anterior scalenus muscle while lifting 40 kg at a fitness center | Left-sided chylothorax | Conservative |
| Akbar et al., 2021 [20] | 1 | Hyperextension of the spine during stretching exercise | Left-sided neck swelling and bilateral chylothorax | Conservative |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hunduma, G.; Ferrari, P.A.; Alreshaid, F.; Kiran, T.; Alzetani, A.; Tamburrini, A. Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature. Surgeries 2024, 5, 288-296. https://doi.org/10.3390/surgeries5020026
Hunduma G, Ferrari PA, Alreshaid F, Kiran T, Alzetani A, Tamburrini A. Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature. Surgeries. 2024; 5(2):288-296. https://doi.org/10.3390/surgeries5020026
Chicago/Turabian StyleHunduma, Gabriel, Paolo Albino Ferrari, Farouk Alreshaid, Tayyeba Kiran, Aiman Alzetani, and Alessandro Tamburrini. 2024. "Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature" Surgeries 5, no. 2: 288-296. https://doi.org/10.3390/surgeries5020026
APA StyleHunduma, G., Ferrari, P. A., Alreshaid, F., Kiran, T., Alzetani, A., & Tamburrini, A. (2024). Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature. Surgeries, 5(2), 288-296. https://doi.org/10.3390/surgeries5020026







