Abstract
Background: The aim of this study is to compare the mid-term outcomes of primary tear of the anterior cruciate ligament (ACL) reconstruction via the use of peroneus longus tendon (PLT) and bone–patellar tendon–bone (BPTB) autografts. Methods: 53 patients (group 1) received ACL reconstruction via BPTB, whereas 55 patients (group 2) received arthroscopic ACL reconstruction using PLT autograft. Results: In group 1, the mean preoperative and postoperative scores on the Lysholm Knee Questionnaire (LKQ) scale resulted in 69.2 ± 10.7 points and −92.2 ± 6.4 points, respectively. The average preoperative and postoperative value on the International Knee Documentation Committee (IKDC) scale was 68.2 ± 10.6% and −90.1 ± 9.5%, respectively. For KT-1000, according to the results of surgical treatment, it is −3.7 ± 1.4 mm, and for the American Orthopaedic Foot & Ankle Society (AOSAF) it is −95.3 ± 4.5%. The autograft ruptured within 2 years after operation in 4 of 50 patients. In group 2, the mean score on the LKQ scale before the operation was 70.2 ± 11.6 points, after −94.3 ± 0.5 points. The average value on the IKDC scale before surgery was 68.6 ± 8.7%, after −91.5 ± 8.2%. KT-1000 −3.4 ± 1.2 mm. Conclusion: The results in both groups can be assessed as good; peroneus longus muscle tendon autograft is an alternative graft for the primary reconstruction of ACL, preserving the dynamic stabilizers of the knee and has no effect on the formation of flat feet and other disease in the postoperative period.
1. Introduction
A tear of the anterior cruciate ligament (ACL) is one of the most common injuries of the knee joint sustained by physically active individuals [1]. The history of ACL arthroscopic reconstruction dates back over 30 years [2,3]. Surgeons now have a wide range of surgical techniques, graft materials, and fixation methods available for use in a bone tunnel. Semitendinosus/gracilis tendon and bone–patellar tendon–bone (BPTB) grafts are the preferred graft materials for primary ACL reconstruction [4]. BPTB is one of the best graft choices because it allows bone-to-bone healing, which permits the effective incorporation of tunnel and graft, leading to a faster return to function and sports activity [5]. This characteristic is important in relation to professional athletes with ACL injuries. However, it carries the risk of patellar fracture, with an invasive approach and a large incision, fixed length and a weaker-than-native ACL, making it unsuitable for double-bundle reconstruction and anterior kneeling pain [5]. For instance, the use of BPTB grafts often leads to significant pain in the anterior knee and at the harvest site (present in 60% of cases) and poses a high risk for osteoarthrosis and ACL tears in the contralateral leg [6]. Conversely, harvesting hamstring autografts can result in a strength imbalance between tibial flexors and extensors, increasing the likelihood of ACL graft rupture [7,8].
The peroneus longus tendon (PLT) shows promise as an autograft material for ACL reconstruction. It can be easily and quickly harvested, possesses sufficient thickness, and does not affect the dynamic knee joint stabilizers, thereby preventing complications associated with autograft harvesting [9,10]. However, the potential of PLT autografts for arthroscopic ACL reconstruction and their impact on foot function remains not fully understood and requires further elucidation.
The purpose of this study was to compare the midterm outcomes of primary anterior cruciate ligament (ACL) reconstruction using peroneus longus tendon (PLT) autografts and bone–patellar tendon–bone (BPTB) autografts in microsurgical techniques.
2. Materials and Methods
2.1. Patients Selection
This prospective, monocentric, longitudinal and randomized comparative controlled study was conducted between 2017 and 2018. The study included a total of 108 patients who underwent arthroscopic reconstruction of the anterior cruciate ligament (ACL). Among them, 53 patients were assigned to the main group (group 1) and received an autograft harvested from the peroneus longus tendon, while 55 patients were assigned to the control group (group 2) and received a bone–patellar tendon–bone graft. The assignment of patients to the main and control groups was randomized using sealed envelopes. Surgical interventions were performed consecutively on both groups, and no specific criteria were applied to determine the choice of autograft type. During the follow-up period, 8 patients from the total cohort were unavailable for postoperative examinations. The surgical procedures were carried out by three experienced surgeons from the traumatology and orthopedics department, each with over 5 years of experience and performing a minimum of 200 ACL reconstructions per year.
The surgical technique, instruments, and disposables were standardized and consistent across both groups. Only autografts were used for ACL reconstruction, with no utilization of allo- or xenografts or repair techniques. Suture techniques were employed to repair different types of meniscal tears, including traumatic, ‘fresh’ para-capsular, RAMP, longitudinal, and bucket handle tears in the red-red zone. A partial meniscectomy was performed for degenerative or flap-type meniscal tears in areas with poor blood supply.
The study enrolled participants based on specific eligibility criteria: engagement in sports activities at least three times a week, absence of ankle joint injuries or instability (for group 1), age between 18 and 50 years, no previous knee joint surgeries, willingness to undergo preoperative MRI examination of the knee joint, no history of neurological or psychiatric disorders, and consent to complete medical questionnaires and participate in the study. Exclusion criteria included stage 3–4 bilateral flatfoot (for group 1), multiligament injury, full-thickness articular cartilage defect of the knee, and meniscal root tear.
Evaluation of knee joint function involved the use of multiple assessment methods. Anamnesis encompassed information on the mechanism of injury, previous conservative treatments and rehabilitation, and the type of sports activity. Clinical examination included tests such as the anterior drawer test, pivot-shift test, Lachman test, range of motion assessment, MacMurray test, and Apley compression tests. Preoperative instrumental diagnostic tests such as the KT-1000 (MED metric Corporation, KT 327, 000000443, San Diego, CA, USA) and PKS-01 (Los Angeles, CA, USA) were conducted. Additionally, patients completed questionnaires before surgery and at the 2-year follow-up, including the Lysholm Knee Questionnaire [11], IKDC-2000 [12], and American Orthopaedic Foot & Ankle Society (AOFAS) (main group only). For the main group, a computer-aided plantographic examination using the PKS-01 device was performed. This device utilizes an integrated camera and specialized software to analyze foot photos. Patient follow-up, as well as pre- and postoperative examinations, were conducted by the operating surgeons.
Ethical approval for the study was obtained from the local Academician B. V. Petrovsky (Moscow, Russia) ethics committee in 2017, with protocol number 11.
2.2. Surgical Technique
In both groups, ACL reconstruction was preceded by diagnostic and therapeutic arthroscopy, which included partial meniscectomy/meniscal repair if it was necessary, resection of the hypertrophic synovial plica, and preparation for bone tunnel formation. In the next step, the autograft was harvested, and ACL reconstruction was performed.
In the main group, the single-bundle technique was used, with an anteromedial portal for tunnel formation. The autograft was harvested from the peroneus longus tendon of the ipsilateral leg. The diameter of bone tunnels was determined by the diameter of the graft. The graft was fixed with biodegradable interference screws (a blend of polylactic acid and hydroxyapatite). The screw diameter equaled the tunnel size; the length of the femoral and tibial interference fixators was 25 mm and 30 mm, respectively.
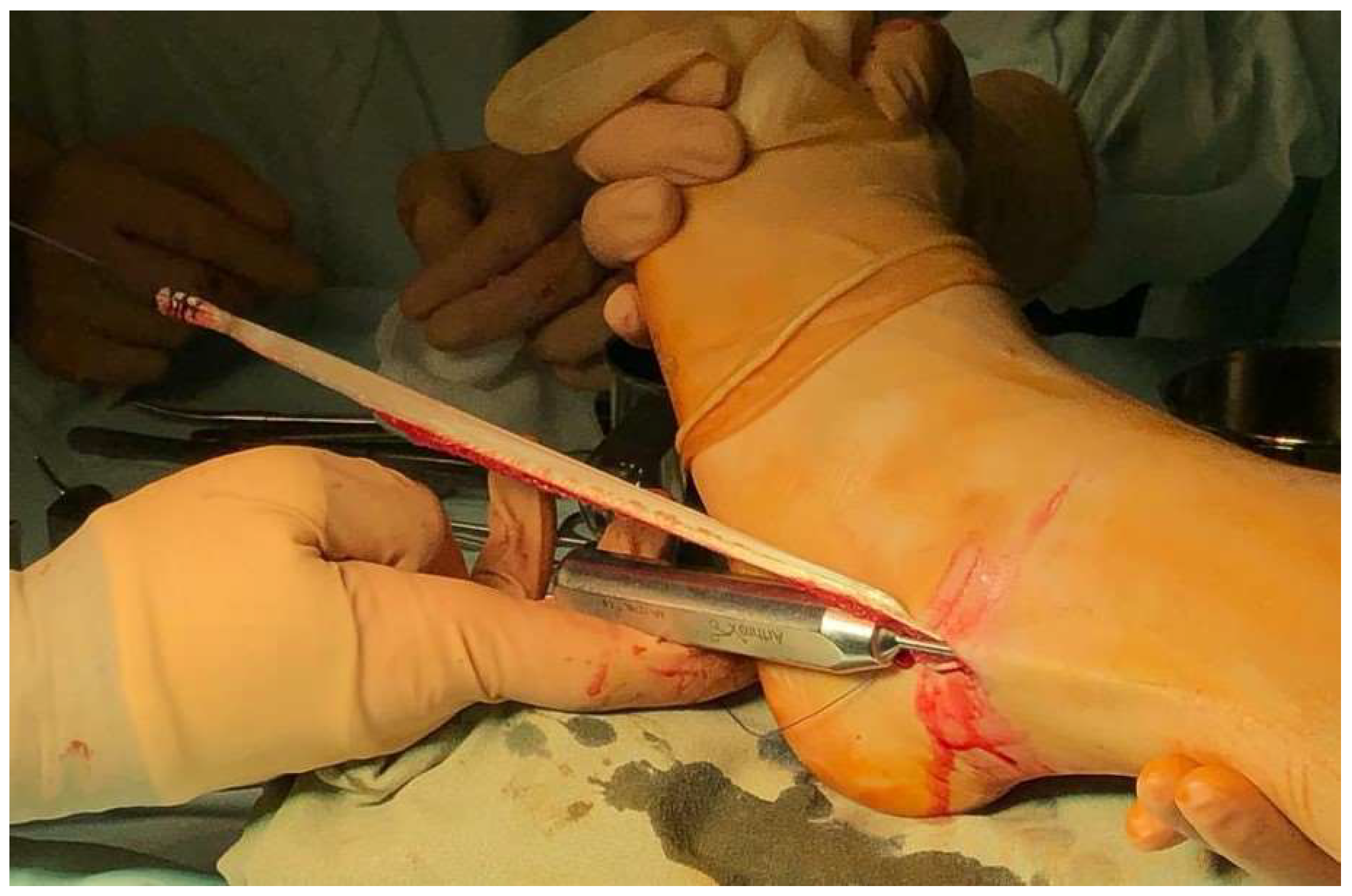
The course of the peroneus longus tendon was determined by putting the foot in the inverted position; then, a 2 cm skin incision was made along the PLT course over the posterior edge of the lateral malleolus (Figure 1).

Figure 1.
Skin incision over the peroneus longus tendon of the left leg.
The skin incision was extended proximally and distally along the course of the tendon. The fascia was dissected, and PLT was exposed and grasped using Billroth’s forceps and a dissector (Figure 2).

Figure 2.
Isolation of PLT of the left leg.
The autograft was harvested in the ventral direction using a blunt-tipped instrument to avoid injury to the adjacent anatomical structures, including the sural nerve. PLT lies superficial to the peroneus brevis tendon. At the donor site, the peroneus brevis tendon is thin and has clearly visible, prominent muscle tissue. This helps to differentiate between peroneus tendons and to avoid a surgical error before the suturing step (Figure 3).
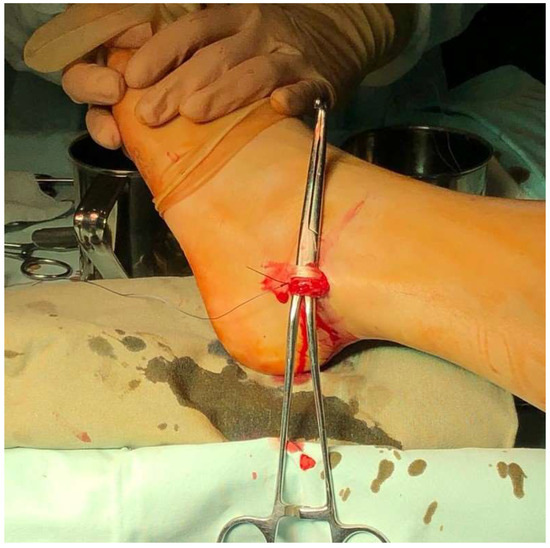
Figure 3.
Comparison of the peroneus longus and brevis tendons of the left.
After PLT was isolated, its proximal end (25 mm) was sutured using Krackow stitches, whereas its distal end was sutured using a biodegradable suture material. Then, the tendon was transected between the suture sites. Its distal end was sutured to the tendinous portion of the peroneus brevis tendon. The proximal portion of PLT was released from its muscular attachments using a stripper, and the autograft was harvested (Figure 4).
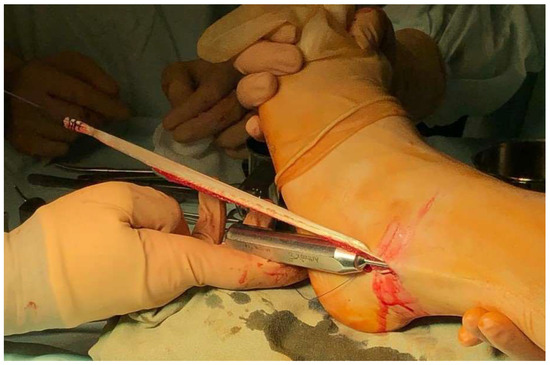
Figure 4.
Harvesting a PLT autograft from the left patient’s leg.
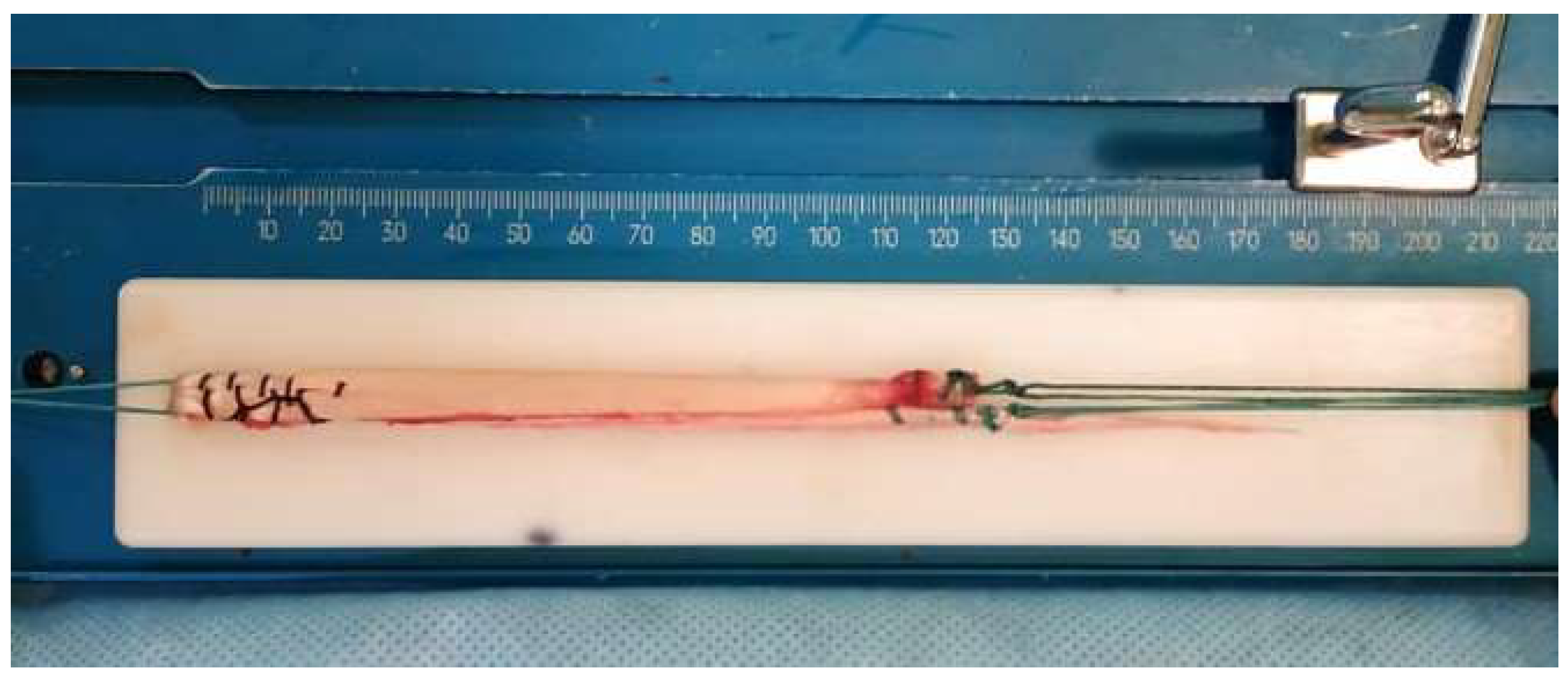
The fascia was closed with absorbable sutures; the skin incision was closed with a nonabsorbable suture material. Once the graft was harvested, it was prepared for further implantation by the surgeon’s assistant. Briefly, the tendon was cleared of muscle fibers, the graft was folded in two, and its distal ends were secured to the graft preparation station. The unsutured distal end of the graft (25 mm) was sutured using Krackow stitches. The proximal end (25 mm) was sutured using a biodegradable suture (Figure 5). Then, the diameter of the graft was measured using a graft sizer tool.
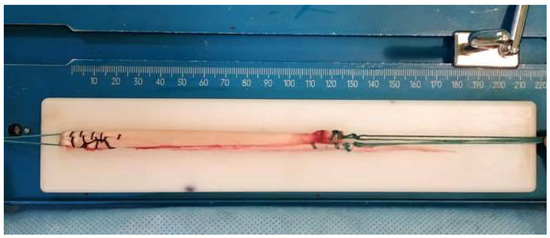
Figure 5.
A ready-for-use PLT graft.
While the graft was being prepared, the surgeon was forming bone tunnels as described above. Once ready, the graft was passed through the bone tunnels and fixed with biodegradable screws. The surgical technique used in the control group was the same as in the main group. The autograft for ACL reconstruction was a bone–patellar tendon–bone graft. Bone tunnels were 10 mm in diameter. The graft was fixed with biodegradable interference screws (a blend of polylactic acid and hydroxyapatite) of various lengths: 8 × 25 mm for the femoral tunnel and 8 × 30 mm for the tibial tunnel.
2.3. Postoperative Period
The postoperative care protocol was standardized for both groups. Patients did not wear braces during the early postoperative period. Weight-bearing on the operated leg, walking, and painless knee flexion and extension exercises were initiated as early as the day following surgery. Patients were advised to take three weeks off work and rest at home before gradually resuming daily activities. By the sixth week, both groups achieved a minimum knee joint flexion angle of 90 degrees. For patients with meniscal sutures, knee flexion beyond 90 degrees was restricted for six weeks. Starting from the third month, patients were allowed to engage in gym workouts and run on a flat surface with straight-line tracks, avoiding sharp turns. Return to preoperative physical activity levels was recommended after complete recovery of femoral and tibial muscles, which typically took an average of eight months. Follow-up examinations were conducted at 14 and 30 days post-surgery, as well as at 3, 6, 12, and 24 months post-surgery (Table 1).

Table 1.
Follow-Up Assessment Methods After ACL Reconstruction.
2.4. Functional Assessment
The functional outcomes of foot and ankle surgeries in group 1 were evaluated using the AOFAS (American Orthopaedic Foot and Ankle Society) scale. Baseline assessments using the AOFAS scale were performed preoperatively to establish the initial functional status of patients in group 1. These assessments were conducted by trained healthcare professionals experienced in using the AOFAS scale to ensure consistency and accuracy of the measurements. Postoperative assessments using the AOFAS scale were conducted at specified time points, including 3 months, 6 months, and 1 year after the surgery, to track the functional improvement in group 1 patients. The follow-up assessments aimed to determine the long-term outcomes and evaluate the effectiveness of the surgical intervention.
2.5. Statistical Analysis
Data analysis was conducted using Excel and SPSS software. The significance level was set at p < 0.05 to determine statistical significance. The analysis included all participants in the study, including those who experienced complications during the postoperative period, such as autograft tear, ankle joint instability in the main group, or sural nerve injury in the main group.
For variables that followed a normal distribution with 95% confidence, such as Lysholm Knee Questionnaire scores, parametric statistical tests were employed. These included independent t-tests or analysis of variance (ANOVA) with post hoc tests for between-group comparisons. For variables that did not follow a normal distribution, non-parametric statistical tests were used. The Mann–Whitney U test was utilized to examine differences between groups.
Appropriate measures of central tendency (mean or median) and dispersion (standard deviation or interquartile range) were reported for continuous variables, while frequencies and percentages were used for categorical variables. Effect sizes were calculated where applicable to assess the magnitude of differences between groups.
Confidence intervals were determined to provide estimates of the precision of the study findings. Additionally, appropriate adjustments for multiple comparisons were applied when necessary. All statistical analyses were conducted by a trained statistician following established guidelines and recommendations for analyzing clinical data.
3. Results
The main indicators are presented in Table 2. Mean values and confidence intervals were computed for the Lysholm Knee Questionnaire, IKDC-2000, and postoperative KT-1000 scores in both groups. The normality of the data distribution was assessed using the one-sample Kolmogorov–Smirnov test. To evaluate differences in the proportion of patients with an ACL graft tear between the main and control groups, a Z-test was employed. Pearson’s correlation coefficient was calculated to explore potential correlations between the diameter of the bone tunnel and patient characteristics such as weight, height, and age in the main group.

Table 2.
Main indicators of the study.
The Lysholm Knee Questionnaire (LCQ) scores before the operation range from 41 to 94, with an average value of 69.739 and a standard deviation of 10.8779. The median LKQ score is 70, indicating the middle value of the distribution. After the operation, the LKQ scores range from 54 to 100, with an average value of 93.24 and a standard deviation of 9.6422. The median LKQ score increases to 97.
The IKDC-2000 scores before surgery range from 0 to 87.4, with an average value of 65.661 and a standard deviation of 17.1084. The median IKDC-2000 score is 69.55. After the operation, the IKDC-2000 scores range from 0 to 100, with an average value of 89.89 and a standard deviation of 12.6649. The median IKDC-2000 score increases to 93.1.
The mode represents the most frequent value in the distribution. The mode for LKQ before the operation is 63, and for LKQ after the operation, it is 100.
In this case, at the 95% confidence level, only the LKQ data before the operation have a normal distribution. Since the remaining indicators are not distributed normally, the differences will be checked using nonparametric comparison methods. In this case, we will use the Mann–Whitney criterion. For the nonparametric comparison of independent samples, see Table 3. The average ranks of the groups in the control group in the sample exceed the studied one.

Table 3.
Mann–Whitney criterion.
As we can see, there are no significant differences between the study group and the control group at 95% confidence (to confirm significant differences, the indicators of asymptotic significance should not exceed 0.05 at a confidence level of 95%).
In our study, we assessed the differences in the proportions of patients with repeated ruptures between the study and control groups using the Z-criterion. We also examined the correlation between the bone canal diameter in the study group and anthropometric parameters like weight, height, and age using the Pearson correlation coefficient. All analyses were conducted using Excel 2019 and SPSS V 28.8, with a significance threshold set at p < 0.05.
All patients, including those who experienced postoperative complications such as autograft rupture and ankle joint instability in the study group or damage to the calf nerve branch, were included in the analyses. Interestingly, only the “Lysholm Knee Questionnaire before surgery” data followed a normal distribution at the 95% confidence level. For non-normally distributed data, we utilized nonparametric methods, specifically the Mann–Whitney criterion. Although the average ranks were higher in the control group, there were no significant differences between the groups at a 95% confidence level. Furthermore, the z-criterion did not show significant differences concerning repeated graft rupture cases between the groups.
3.1. Group 1
Of 53 patients included in group 1, only 50 showed up for follow-up examinations in the early and late postoperative periods. The mean age in group 1 was 33.4 ± 8.9 years; 72% of the patients in this group were male, and 28% were female. Of all the patients in group 1, we failed to contact three individuals in the postoperative period. By month 24 after surgery, 7 of 50 patients had started to notice swelling at the graft harvest site during physical exercise, which was resolved on the following day. Two patients sustained an intraoperative injury to the sural nerve during graft harvesting and developed a reduced sense of touch and paresthesia over the fifth metatarsal. By month 24, these neurological symptoms had regressed, but the patients still complained that their sense of touch in the operated leg was permanently reduced, compared with the same region of the contralateral leg. During the follow-up, examination conducted 24 months after surgery, 6 of 50 patients still had complaints of mild pain and discomfort (1–2 points on the visual analogue scale) in the operated knee joint during physical exercise.
Prior to surgery, the mean Lysholm Knee Questionnaire score in group 1 was 69.2 ± 10.7 points, whereas after surgery, it increased to 92.2 ± 6.4 points. The mean preoperative IKDC-2000 score was 68.2 ± 10.6 points, increasing to 90.1 ± 9.5 points after surgery. Postoperative KT-1000 was 3.7 ± 1.4 mm, and postoperative AOFAS was 95.3 ± 4.5%.
Within 2 years after surgery, an ACL graft tear occurred in 4 of 50 patients (8%). The tear was diagnosed during a follow-up examination; the diagnosis relied on clinical and instrumental tests (tibial displacement > 5 mm according to KT-1000), medical history and MRI findings. Preoperative planography revealed first and second degrees bilateral flatfoot (with fallen transverse and longitudinal arches) in 12 patients; 12 patients had high arches, and 26 had no foot deformities. Plantography performed 24 months after surgery showed no changes in foot arches. This means that autograft harvesting from the peroneus longus tendon had no effect on the progression of the pathology.
In addition to conducting clinical tests, we investigated possible correlations between the bone tunnel diameter (determined by the graft diameter) and the weight, age and height of our patients. The mean tunnel diameter was 7.9 mm and ranged from 7 mm to 10 mm.
The values of the correlation coefficient did not exceed 0.3 in all cases, suggesting that there was no convincing correlation between the diameter of the autograft and the age, weight or height of the patients. So, we conclude that these anthropometric parameters cannot be used to predict the diameter of an autograft for ACL reconstruction.
The majority of patients experienced little worsening in their AOFAS scores after the operation. There was no serious negative effect on the foot and ankle joints in the postoperative period.
3.2. Group 2
Of 55 patients included in group 2, only 50 showed up for follow-up examinations in the early and late postoperative periods. The mean age in this group was 27.9 ± 7.4 years; 78% of the patients were male, and 22% were female. We were unable to reach 5 of 55 patients in group 2. By month 24 after surgery, 14 of 50 patients still had complaints of mild pain and discomfort (1–2 points on the visual analogue scale) in the anterior knee joint during physical exercise.
The patients completed the Lysholm Knee Questionnaire and the IKDC-2000 form before and after surgery. Twenty-four months after surgery, the residual Lachman sign was measured using KT-1000.
The mean preoperative Lysholm Knee Questionnaire score was 70.2 ± 11.6 points, increasing to 94.3 ± 5 points postoperatively. The mean preoperative IKDC-2000 score was 68.6 ± 8.7 points; after surgery, it increased to 91.5 ± 8.2 points. Postoperative KT-1000 was 3.4 ± 1.2 mm. Within 2 years after surgery, an ACL graft tear occurred in 3 (6%) out of 50 patients in group 2.
3.3. Outcomes Evaluation
Summing up, the outcomes of arthroscopic ACL reconstruction were good in both groups. Statistically, there were no significant differences in outcomes between the groups, suggesting that a PLT autograft is an alternative to traditional autografts in primary ACL reconstruction that allows preserving the dynamic stabilizers of the knee joint. No tendency to flatfoot formation was observed in the main group.
Patients in group 1 experienced less pain and discomfort compared to patients in group 2 (p-value = 0.4) at the last follow-up (24 months). Patients in group 1 have an incidence of ACL graft tear within 2 years, similar to patients in group 2. These data were not statistically significant (p-value = 0.69). p-value was calculated with a chi-square test.
4. Discussion
The surgical technique, mechanical properties of hamstring and BPTB autografts for ACL reconstruction, and the long-term outcomes of this surgical intervention are well studied. This makes ACL reconstruction a successful therapeutic procedure with predictable outcomes [5,13,14]. However, some aspects of postoperative knee joint biomechanics require elucidation. For example, it is reported that using knee joint stabilizers as autografts can negatively affect the function of the knee joint and the lower leg compartment: weakened tibial flexors and extensors might impair the knee joint function in the postoperative period; there is also a risk of autograft injury [15,16]. Indeed, the anatomical tunnel position and postoperative rehabilitation reduce the likelihood of complications, but alternative types of autografts might also make their contribution to reducing the risks related to the knee joint biomechanics [16]. We think that the peroneus longus tendon is an underrated alternative to traditional autografts. Although it was first introduced into surgical practice over 10 years ago, it has not since gained wide recognition. There are only scarce research studies of this autograft type. Some of them attempted to evaluate the mid-term outcomes of using PLT for arthroscopic ACL reconstruction in different groups of patients [9,10,11,12,17]. The outcomes were interpreted as good and excellent; the patients were very satisfied with the results. No negative impact on the foot and ankle joint functions was reported in the postoperative period. Therefore, those studies recommended using a PLT autograft for primary ACL reconstruction. However, a study by Angthong et al. [18] reported changes to the foot and ankle joint functions that had a negative effect on the patients’ quality of life. Consequently, PLT was recommended as an alternative for revision ACL reconstruction but not as a first-choice option for primary ACL reconstruction. In our study, there were no postoperative changes affecting the ankle joint or foot functions, including instability of the ankle joint and flatfoot. The most common complaint was edema at the harvest site, which, in most cases, resolved within a year following ACL reconstruction. It is believed that PLT harvesting does not promote ankle joint instability because PLT is not an ankle joint stabilizer. PLT partially retains its function if its distal end is sutured to the peroneus brevis tendon. Colleagues who have been using PLT grafts for ALC reconstruction since 1997 analyzed the regenerative potential of PLT; based on the MRI scans of the ankle joint and tibia, they concluded that the tendon was able to regenerate partially in the late postoperative period [19]. In another study, Song X et al. analyzed the correlations between the diameter of a folded PLT graft, which was 8.3 mm on average, and some anthropometric parameters of their patients. The authors found that the anthropometric data could be successfully used to reliably predict the graft diameter and, therefore, obtain a good-quality graft [20]. In another study, the mean PLT graft diameter was 8.56 mm; the authors proposed a method for predicting the graft diameter at the preoperative stage [21]. In our patients, the mean diameter of the folded PLT graft was about 7.9 mm, but we did not find any correlations between the diameter of the graft and the age, weight and height of our patients, and the graft diameter cannot be predicted based on these parameters. Still, the graft diameter might depend on how physically active the patient is (the more active the patient, the thicker the graft). The harvesting technique we used was simple and rapid; it did not result in prolonged surgery duration.
Our findings indicate that the PLT offers a promising alternative to the traditional BPTB graft. Importantly, the PLT autograft extraction did not compromise the dynamic stabilizers of the knee joint, addressing some of the complications seen with other graft types. This aligns with the recent thrust in orthopedic research seeking solutions that uphold the integrity and function of the knee joint postoperatively.
A pivotal observation was that only the “Lysholm Knee Questionnaire before surgery” data adhered to a normal distribution, compelling us to employ nonparametric testing methods for the other variables. Utilizing the Mann–Whitney criterion, it was discerned that although the average ranks in the control group were marginally higher, the difference was not statistically significant. This infers that both PLT and BPTB grafts could potentially be equally effective in ACL reconstruction. Nonetheless, the advantage of fewer complications with PLT suggests its superiority in specific patient cohorts.
While the results of our study are promising, they echo the findings of prior literature, which suggests the efficacy of non-traditional grafts in ACL reconstruction [22,23]. The PLT’s ability to be harvested without disrupting knee dynamics presents a clear advantage, particularly when compared to grafts that might result in strength imbalances or other complications. It is noteworthy to mention that our study did present certain limitations. The research was monocentric, potentially limiting the generalizability of the findings. Additionally, the sample size, while significant, could be expanded in future studies to validate these findings further. One intriguing observation was regarding the lack of significant differences concerning repeated graft rupture cases between the groups. These challenges the commonly held belief about the robustness of the BPTB graft and opens up a new avenue of investigation into the long-term durability and resilience of the PLT graft.
The AOFAS score in the study aimed to evaluate the functional outcomes and quality of life of patients who underwent ACL reconstruction with an autograft harvested from the peroneus longus tendon. This measure provides valuable information on the effectiveness of the surgical technique and graft choice in terms of foot and ankle function. It is important to note that the AOFAS score was specific to the main group (group 1) in this study, as the control group (group 2) received a bone–patellar tendon–bone graft and did not require assessment using the AOFAS score.
Study Limitations
Our groups of patients were heterogeneous in terms of age, sex, anthropometric characteristics, and coexisting knee joint pathology. The choice of surgical treatment for meniscal pathology (meniscectomy vs. meniscal repair) could have affected the residual Lachman sign. The types of autografts, their mechanical properties and methods for graft attachment were also different between the groups, which might have affected the outcomes. Further research should be conducted in patient groups homogenous in terms of meniscal pathology, hypermobility and other parameters.
5. Conclusions
Our results demonstrated that ACL reconstruction with the peroneus longus tendon autograft yielded comparable outcomes to the bone–patellar tendon–bone graft in terms of knee stability, functional performance, and patient-reported outcomes. We did not observe any negative effects of PLT harvesting on the ankle joint function and the progression of flatfoot during the 24-month follow-up. The clinical and functional assessment measures, including the Lachman test, pivot shift test, Lysholm Knee Questionnaire, IKDC-2000, and AOFAS score (main group), consistently showed no significant differences between the two graft types. Further studies with larger sample sizes and longer-term follow-up are warranted to validate these findings and assess the durability of the peroneus longus tendon autograft over time.
Author Contributions
Conceptualization, E.N.G., O.A.K., E.N.B., A.A.V., N.G.G., M.E.R. and N.M.; methodology, E.N.G., O.A.K. and E.N.B.; validation, E.N.G., N.G.G., M.E.R. and N.M.; formal analysis, E.N.G., O.A.K., R.N., E.N.B., A.A.V. and N.M.; investigation, E.N.G., R.N., O.A.K. and E.N.B.; writing—original draft preparation, E.N.G., O.A.K. and M.E.R.; writing, review and editing, N.G.G., M.E.R. and N.M.; visualization, E.N.G., O.A.K. and E.N.B.; supervision, N.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics committee of the (2017, protocol number 11).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sanders, T.L.; Maradit, K.H.; Bryan, A.J.; Larson, D.R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am. J. Sports Med. 2016, 44, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- Chambat, P.; Guier, C.; Sonnery-Cottet, B.; Fayard, J.M.; Thaunat, M. The evolution of ACL reconstruction over the last fifty years. Int. Orthop. 2013, 37, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Davarinos, N.; O’Neill, B.J.; Curtin, W. A brief history of anterior cruciate ligament reconstruction. Adv. Orthop. Surg. 2014, 1, 706042. [Google Scholar] [CrossRef]
- Samuelsen, B.T.; Webster, K.E.; Johnson, N.R.; Hewett, T.E.; Krych, A.J. Hamstring Autograft versus Patellar Tendon Autograft for ACL Reconstruction: Is There a Difference in Graft Failure Rate? A Meta-analysis of 47,613 Patients. Clin. Orthop. Relat. Res. 2017, 475, 2459–2468. [Google Scholar] [CrossRef]
- Rhatomy, S.; Asikin, A.I.Z.; Wardani, A.E.; Rukmoyo, T.; Lumban-Gaol, I.; Budhiparama, N.C. Peroneus longus autograft can be recommended as a superior graft to ham-string tendon in single-bundle ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3552–3559. [Google Scholar] [CrossRef]
- Thompson, S.M.; Salmon, L.J.; Waller, A.; Linklater, J.; Roe, J.P.; Pinczewski, L.A. Twenty-Year Outcome of a Longitudinal Prospective Evaluation of Isolated Endoscopic Anterior Cruciate Ligament Reconstruction with Patellar Tendon or Hamstring Autograft. Am. J. Sports Med. 2016, 44, 3083–3094. [Google Scholar] [CrossRef] [PubMed]
- Goncharov, E.N.; Koval, O.A.; Bezuglov, E.N.; Goncharov, N.G. Anatomical features and significance of the anterolateral liga-ment of the knee. Int. Orthop. (SICOT) 2018, 42, 2859–2864. [Google Scholar] [CrossRef] [PubMed]
- Yamanashi, Y.; Mutsuzaki, H.; Iwai, K.; Ikeda, K.; Kinugasa, T. Failure risks in anatomic single-bundle anterior cruciate ligament reconstruction via the outside-in tunnel technique using a hamstring autograft. J. Orthop. 2019, 16, 504–507. [Google Scholar] [CrossRef]
- Goncharov, E.N.; Koval, O.A.; Dubrov, V.E.; Bezuglov, E.N.; Alekhin, A.A.; Goncharov, N.G. Mid-Term Results of Simultaneous Reconstruction of Anterior Cruciate and Anterolateral Ligaments in Athletes. Traumatol. Orthop. Russ. 2020, 26, 62–71. [Google Scholar] [CrossRef]
- Goncharov, E.N.; Koval, O.A.; Dubrov, V.E.; Bezuglov, E.N.; Filimonova, A.M.; Goncharov, N.G. Clinical experience with combined reconstruction of the anterior cruciate and anterolateral ligaments of the knee in sportsmen. Int. Orthop. (SICOT) 2019, 43, 2781–2788. [Google Scholar] [CrossRef]
- Briggs, K.K.; Lysholm, J.; Tegner, Y.; Rodkey, W.G.; Kocher, M.S.; Steadman, J.R. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am. J. Sports Med. 2009, 37, 890–897. [Google Scholar] [CrossRef] [PubMed]
- Irrgang, J.J.; Anderson, A.F.; Boland, A.L.; Harner, C.D.; Kurosaka, M.; Neyret, P.; Richmond, J.C.; Shelborne, K.D. Development and validation of the international knee documentation committee subjective knee form. Am. J. Sports Med. 2001, 29, 600–613. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.H.S.; Lau, B.P.H.; Krishna, L. Outcomes of Anterior Cruciate Ligament Reconstruction in Females Using Patellar-Tendon-Bone versus Hamstring Autografts: A Systematic Review and Meta-Analysis. J. Knee Surg. 2019, 32, 770–787. [Google Scholar] [CrossRef]
- Ciccotti, M.C.; Secrist, E.; Tjoumakaris, F.; Ciccotti, M.G.; Freedman, K.B. Anatomic Anterior Cruciate Ligament Reconstruction via Independent Tunnel Drilling: A Systematic Review of Randomized Controlled Trials Comparing Patellar Tendon and Hamstring Autografts. Arthroscopy 2017, 33, 1062–1071.e5. [Google Scholar] [CrossRef] [PubMed]
- Bregenhof, B.; Jørgensen, U.; Aagaard, P.; Nissen, N.; Creaby, M.W.; Thorlund, J.B.; Jensen, C.; Torfing, T.; Holsgaard-Larsen, A. The effect of targeted exercise on knee-muscle function in patients with persistent hamstring deficiency following ACL reconstruction—Study protocol for a randomized controlled trial. Trials 2018, 19, 75. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N.; Ortenzi, V.; Naccarato, G.A.; Perrini, P. Angioleiomyoma of the knee: An uncommon cause of leg pain. A systematic review of the literature. Interdiscip. Neurosurg. 2020, 22, 100877. [Google Scholar] [CrossRef]
- Rhatomy, S.; Wicaksono, F.H.; Soekarno, N.R.; Setyawan, R.; Primasara, S.; Budhiparama, N.C. Eversion and First Ray Plantarflexion Muscle Strength in Anterior Cruciate Ligament Reconstruction Using a Peroneus Longus Tendon Graft. Orthop. J. Sports Med. 2019, 7, 2325967119872462. [Google Scholar] [CrossRef]
- Goncharov, E.N.; Goncharov, N.G.; Bezuglov, E.N.; Vetoshkin, A.A.; Rezunenko, I.A.; Oganesyan, S.K.; Koval, O.A. Comparison of results of the anterior cruciate ligament reconstruction of the knee joint using peroneus longus tendon auto-graft or patellar tendon autograft with two bone blocks. Genij Ortop. 2022, 28, 53–61. [Google Scholar] [CrossRef]
- Kerimoрlu, S.; Koşucu, P.; Livaoрlu, M.; Yükünç, I.; Turhan, A.U. Magnetic resonance imagination of the peroneus longus tendon after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 35–39. [Google Scholar] [CrossRef]
- Song, X.; Li, Q.; Wu, Z.; Xu, Q.; Chen, D.; Jiang, Q. Predicting the graft diameter of the peroneus longus tendon for anterior cruciate ligament reconstruction. Medicine 2018, 97, e12672. [Google Scholar] [CrossRef]
- Rhatomy, S.; Tanzil, H.; Setyawan, R.; Amanda, C.; Phatama, K.Y.; Andrianus, J.; Rukmoyo, T.; Kisworo, B. Influence of anthropometric features on peroneus longus graft diameter in Anterior Cruciate Ligament reconstruction: A cohort study. Ann. Med. Surg. 2019, 48, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.K.; Subramaniam, A.G.; Ebert, J.R.; Radic, R. Quadriceps Tendon Versus Hamstring Tendon Autografts for Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2022, 50, 3974–3986. [Google Scholar] [CrossRef] [PubMed]
- Mo, Z.; Li, D.; Yang, B.; Tang, S. Comparative Efficacy of Graft Options in Anterior Cruciate Ligament Reconstruction: A Systematic Review and Network Meta-Analysis. Arthrosc. Sports Med. Rehabil. 2020, 2, e645–e654. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).