Workflow and Short-Term Functional Outcomes in Simultaneous Acute Code Stroke Activation and Stroke Reperfusion Therapy
Abstract
1. Introduction
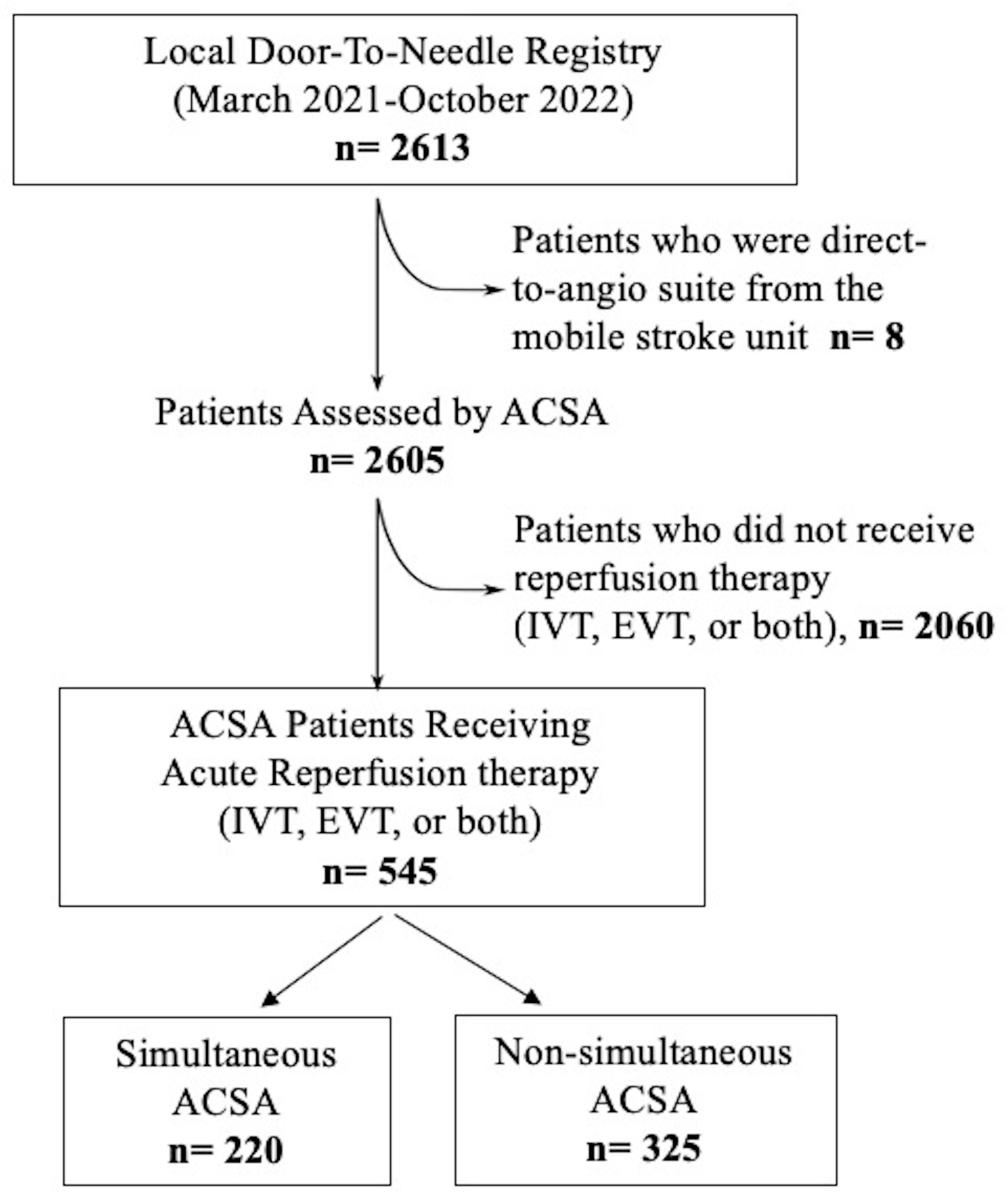
2. Materials and Methods
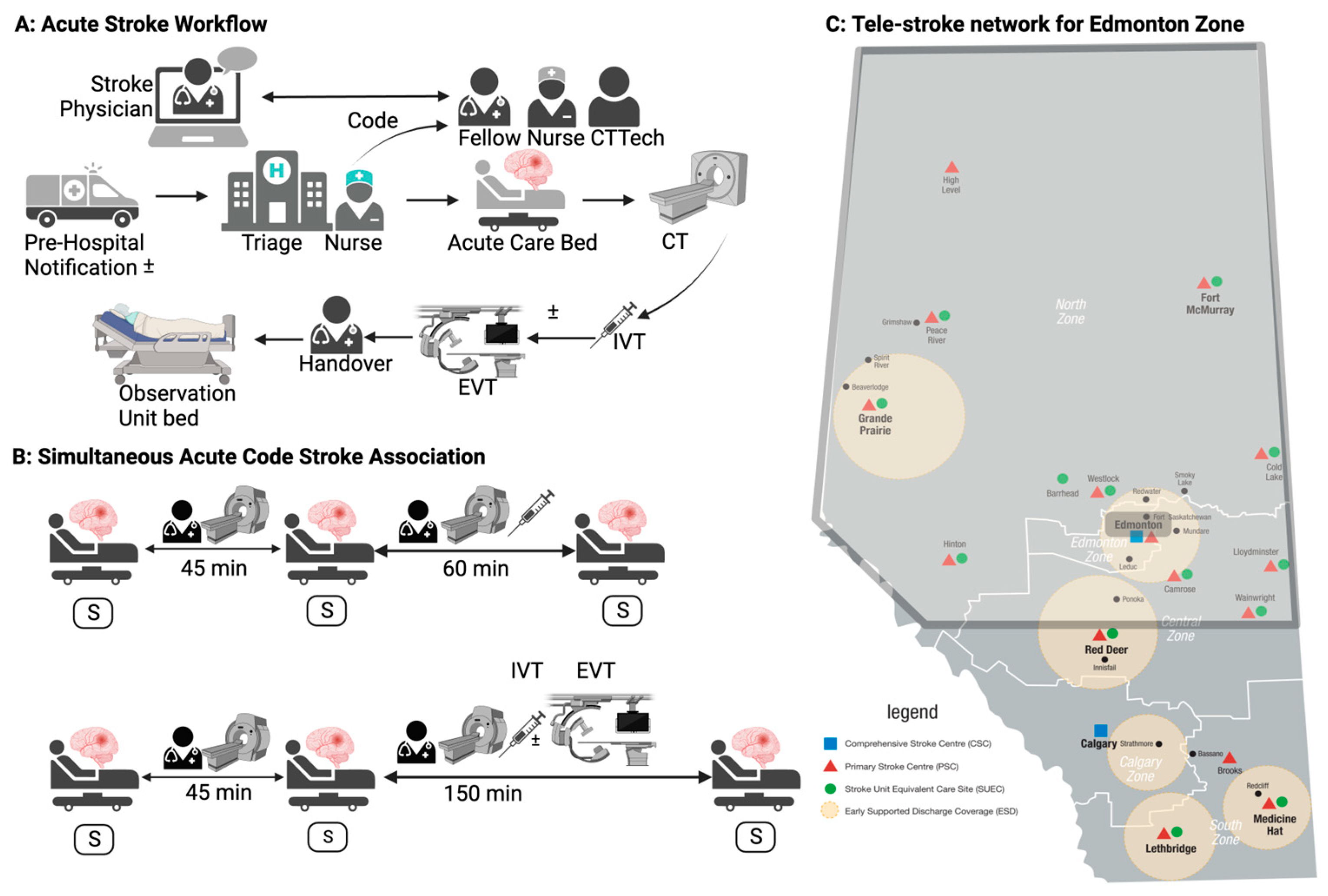
2.1. Study Design and Setting
2.2. Code Stroke Workflow
2.3. Study Definitions
2.4. Outcome Measures
2.5. Sample Size
2.6. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. Workflow Metrics
3.3. Threshold Analyses
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Saver, J.L.; Goyal, M.; van der Lugt, A.; Menon, B.K.; Majoie, C.B.L.M.; Dippel, D.W.; Campbell, B.C.; Nogueira, R.G.; Demchuk, A.; Tomasello, A.; et al. Time to Treatment With Endovascular Thrombectomy and Outcomes From Ischemic Stroke: A Meta-analysis. JAMA 2016, 316, 1279–1289. [Google Scholar] [CrossRef] [PubMed]
- Jovin, T.G.; Nogueira, R.G.; Lansberg, M.G.; Demchuk, A.M.; Martins, S.O.; Mocco, J.; Ribo, M.; Jadhav, A.P.; Ortega-Gutierrez, S.; Hill, M.D.; et al. Thrombectomy for anterior circulation stroke beyond 6 h from time last known well (AURORA): A systematic review and individual patient data meta-analysis. Lancet 2022, 399, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Alemseged, F.; Nguyen, T.N.; Alverne, F.M.; Liu, X.; Schonewille, W.J.; Nogueira, R.G. Endovascular Therapy for Basilar Artery Occlusion. Stroke 2023, 54, 1127–1137. [Google Scholar] [CrossRef]
- Janssen, P.M.; Venema, E.; Dippel, D.W.J. Effect of Workflow Improvements in Endovascular Stroke Treatment. Stroke 2019, 50, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Gao, F.; Ji, Y.; Zhai, T.; Tong, X.; Jia, B.; Wu, J.; Wu, J.; Zhang, Y.; Wei, C.; et al. Workflow Intervals and Outcomes of Endovascular Treatment for Acute Large-Vessel Occlusion During On-Vs. Off-hours in China: The ANGEL-ACT Registry. Front. Neurol. 2021, 12, 771803. [Google Scholar] [CrossRef]
- Heran, M.; Lindsay, P.; Gubitz, G.; Yu, A.; Ganesh, A.; Lund, R.; Arsenault, S.; Bickford, D.; Derbyshire, D.; Doucette, S.; et al. Canadian Stroke Best Practice Recommendations: Acute Stroke Management, 7th Edition Practice Guidelines Update, 2022. Can. J. Neurol. Sci./J. Can. Sci. Neurol. 2022, 51, 1–31. [Google Scholar] [CrossRef]
- Chen, C.-H.; Tang, S.-C.; Tsai, L.-K.; Hsieh, M.-J.; Yeh, S.-J.; Huang, K.-Y.; Jeng, K.-Y. Stroke Code Improves Intravenous Thrombolysis Administration in Acute Ischemic Stroke. PLoS ONE. 2014, 9, e104862. [Google Scholar] [CrossRef]
- Reznek, M.A.; Murray, E.; Youngren, M.N.; Durham, N.T.; Michael, S.S. Door-to-Imaging Time for Acute Stroke Patients Is Adversely Affected by Emergency Department Crowding. Stroke 2017, 48, 49–54. [Google Scholar] [CrossRef]
- Kelen, G.D.; Wolfe, R.; D’Onofrio, G.; Mills, A.M.; Diercks, D.; Stern, S.A.; Wadman, M.C.; Sokolove, P.E. Emergency Department Crowding: The Canary in the Health Care System. NEJM Catal. 2021, 1–26. [Google Scholar] [CrossRef]
- Dalsania, A.K.; Kansagra, A.P. Simultaneous patient presentation for endovascular thrombectomy in acute ischemic stroke. J. Neurointerv. Surg. 2019, 11, 1201–1204. [Google Scholar] [CrossRef]
- Buck, B.H.; Akhtar, N.; Alrohimi, A.; Khan, K.; Shuaib, A. Stroke mimics: Incidence, aetiology, clinical features and treatment. Ann. Med. 2021, 53, 420–436. [Google Scholar] [CrossRef]
- Moskop, J.C.; Sklar, D.P.; Geiderman, J.M.; Schears, R.M.; Bookman, K.J. Emergency Department Crowding, Part 1—Concept, Causes, and Moral Consequences. Ann. Emerg. Med. 2009, 53, 605–611. [Google Scholar] [CrossRef] [PubMed]
- Ding, R.; McCarthy, M.L.; Desmond, J.S.; Lee, J.S.; Aronsky, D.; Zeger, S.L. Characterizing Waiting Room Time, Treatment Time, and Boarding Time in the Emergency Department Using Quantile Regression. Acad. Emerg. Med. 2010, 17, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Bullard, M.J.; Musgrave, E.; Warren, D.; Unger, B.; Skeldon, T.; Grierson, R.; van der Linde, E.; Swain, J. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) Guidelines 2016. Can. J. Emerg. Med. 2017, 19, S18–S27. [Google Scholar] [CrossRef]
- Dreyer, J.F.; McLeod, S.L.; Anderson, C.K.; Carter, M.W.; Zaric, G.S. Physician workload and the Canadian Emergency Department Triage and Acuity Scale: The Predictors of Workload in the Emergency Room (POWER) Study. CJEM 2009, 11, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Wrede, J.; Wrede, H.; Behringer, W. Emergency Department Mean Physician Time per Patient and Workload Predictors ED-MPTPP. J. Clin. Med. 2020, 9, 3725. [Google Scholar] [CrossRef]
- Kamal, N.; Jeerakathil, T.; Stang, J.; Liu, M.; Rogers, E.; Smith, E.E.; Demchuk, A.; Siddiqui, M.; Mann, B.; Bestard, J.; et al. Provincial Door-to-Needle Improvement Initiative Results in Improved Patient Outcomes Across an Entire Population. Stroke 2020, 51, 2339–2346. [Google Scholar] [CrossRef]
- Quinn, T.J.; Dawson, J.; Lees, J.S.; Chang, T.-P.; Walters, M.R.; Lees, K.R. Time Spent at Home Poststroke. Stroke 2008, 39, 231–233. [Google Scholar] [CrossRef]
- Saposnik, G.; Baibergenova, M.A.; O’Donnell, M.; Hill, M.D.; Kapral, M.K.; Hachinski, V. Hospital volume and stroke outcome Does it matter? Neurology 2007, 69, 1142–1151. [Google Scholar] [CrossRef]
- Groot, A.E.; van Schaik, I.N.; Visser, M.C.; Nederkoorn, P.J.; Limburg, M.; Aramideh, M.; de Beer, F.; Zwetsloot, C.P.; Halkes, P.; de Kruijk, J.; et al. Association between i.v. thrombolysis volume and door-to-needle times in acute ischemic stroke. J. Neurol. 2016, 263, 807–813. [Google Scholar] [CrossRef]
- Kim, B.M.; Baek, J.H.; Heo, J.H.; Kim, D.J.; Nam, H.S.; Kim, Y.D. Effect of Cumulative Case Volume on Procedural and Clinical Outcomes in Endovascular Thrombectomy. Stroke 2019, 50, 1178–1183. [Google Scholar] [CrossRef]
- Shim, D.H.; Kim, Y.; Roh, J.; Kang, J.; Park, K.P.; Cha, J.K.; Baik, S.K.; Kim, Y. Hospital volume threshold associated with higher survival after endovascular recanalization therapy for acute ischemic stroke. J. Stroke 2020, 22, 141–149. [Google Scholar] [CrossRef]
- Hahn, M.; Gröschel, S.; Tanyildizi, Y.; Brockmann, M.A.; Gröschel, K.; Uphaus, T. The Bigger the Better? Center Volume Dependent Effects on Procedural and Functional Outcome in Established Endovascular Stroke Centers. Front. Neurol. 2022, 13, 828528. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef]
- Augenstein, T.; Schneider, A.; Wehler, M.; Weigl, M. Multitasking behaviors and provider outcomes in emergency department physicians: Two consecutive, observational and multi-source studies. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 14. [Google Scholar] [CrossRef]
- Nogueira, R.G.; Haussen, D.C.; Smith, E.E.; Sun, J.L.; Xian, Y.; Alhanti, B.; Blanco, R.; Mac Grory, B.; Doheim, M.F.; Bhatt, D.L.; et al. Higher Procedural Volumes Are Associated with Faster Treatment Times, Better Functional Outcomes, and Lower Mortality in Patients Undergoing Endovascular Treatment for Acute Ischemic Stroke. Ann. Neurol. 2023, 95, 146–155. [Google Scholar] [CrossRef]
| Non-Simultaneous ACSA (n = 325) | Simultaneous ACSA (n = 220) | p Value | |
|---|---|---|---|
| Age, years mean ± SD | 70.9 ± 13.7 | 70.5 ± 14.6 | 0.4 |
| Female Sex, n (%) | 143 (44%) | 107 (48.6%) | 0.2 |
| Prior disability, n (%) | 47 (14.5%) | 37 (16.8%) | 0.4 |
| Median (IQR) NIHSS | 13 (8–18) | 13 (8–18) | 0.5 |
| Risk Factors | |||
| Hypertension, n (%) | 209 (64.3%) | 141 (64.1%) | 0.9 |
| Diabetes Mellitus, n (%) | 72 (22.1%) | 53 (24.1%) | 0.6 |
| Dyslipidemia, n (%) | 125 (38.5%) | 81 (36.8%) | 0.6 |
| Atrial Fibrillation, n (%) | 53 (16.3%) | 44 (20%) | 0.3 |
| Coronary artery Disease, n (%) | 52 (16%) | 32 (14.5%) | 0.6 |
| Smoker, n (%) | 64 (19.7%) | 41 (18.6%) | 0.4 |
| Prior Stroke, n (%) | 65 (20%) | 35 (15.9%) | 0.2 |
| Acute Reperfusion Therapies | |||
| Intravenous Thrombolysis, n (%) | 210 (64.6%) | 128 (58.2%) | 0.1 |
| Endovascular Thrombectomy, n (%) | 174 (53.6%) | 138 (62.7%) | 0.03 |
| Short-Term Outcome | |||
| Median (IQR) length of Hospital Stay, Days | 13 (4, 45) | 17 (4, 49) | 0.6 |
| Median Home Time, Days | 54 (0, 85) | 58 (0, 84.5) | 0.7 |
| Mortality at 90 days, n (%) | 63 (19.4%) | 38 (17.2%) | 0.5 |
| Median (IQR) Workflow Times | Non-Simultaneous ACSA | Simultaneous ACSA | ||
|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | ||
| DTC, min | 15 (11, 21) n = 325 | 16 (11, 21) n = 148 | 15 (10.5, 22.5) n = 59 | 18 (13–28) * n = 13 |
| DTN, min | 39 (30, 55) n = 210 | 39 (30, 50.5) n = 92 | 39 (30, 57) n = 31 | 53 (30–56) n = 5 |
| DTP, min | 98.5 (82, 124) n = 174 | 101 (83, 127) n = 89 | 89.5 (69, 114) n = 38 | 121 (64, 188) * n = 11 |
| DTR, min | 149 (119, 177) n = 174 | 141 (114, 184) n = 89 | 119.5 (103, 156) n = 38 | 155 (108.5, 224.5) n = 11 |
| Home Time, days | 54 (0, 85) n = 325 | 54.5 (0, 84) n = 148 | 66 (2, 85.5) n = 59 | 61 (29, 84) n = 13 |
| Median (IQR) | Study Definition | Higher Threshold | Low Threshold | Very Low Threshold | ||||
|---|---|---|---|---|---|---|---|---|
| NS-ACSA (n = 325) | S-ACSA (n = 220) | NS-ACSA (n = 291) | S-ACSA (n = 254) | NS-ACSA (n = 364) | S-ACSA (n = 181) | NS-ACSA (n = 405) | S-ACSA (n = 140) | |
| DTC (min) | 15 (11, 21) | 16 (11, 22.5) | 15 (11, 21) | 16 (11, 23) | 15 (11, 21) | 16 (11, 23) | 15 (11, 21) | 17 (12, 25) |
| DTN (min) | 39 (30, 55) | 39 (30.5, 53) | 39 (29, 55) | 39 (30.5, 52) | 38 (30, 55) | 40 (31, 53) | 38 (30, 52) | 40 (31, 53) |
| DTP (min) | 98.5 (82, 124) | 98.5 (79, 125) | 97 (811, 123) | 101 (80, 126) | 98.5 (81, 124.5) | 98.5 (79.5, 125) | 98.5 (81, 122.5) | 98.5 (79.5, 130) |
| DTR (min) | 149 (119, 177) | 140.5 (110, 167.5) | 147 (121, 173) | 141 (112, 168) | 147 (120, 173.5) | 140 (111, 161) | 147 (116, 172) | 141.5 (113, 173) |
| Home Time (days) | 54 (0, 85) | 58 (0, 84.5) | 55 (0, 85) | 56 (0, 84) | 55 (0, 85) | 57 (0, 84) | 55 (0, 85) | 61 (3.5, 84.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarmiento, R.J.; Wagner, A.; Sheriff, A.; Taralson, C.; Moniz, N.; Opsahl, J.; Jeerakathil, T.; Buck, B.; Sevcik, W.; Shuaib, A.; et al. Workflow and Short-Term Functional Outcomes in Simultaneous Acute Code Stroke Activation and Stroke Reperfusion Therapy. NeuroSci 2024, 5, 291-300. https://doi.org/10.3390/neurosci5030023
Sarmiento RJ, Wagner A, Sheriff A, Taralson C, Moniz N, Opsahl J, Jeerakathil T, Buck B, Sevcik W, Shuaib A, et al. Workflow and Short-Term Functional Outcomes in Simultaneous Acute Code Stroke Activation and Stroke Reperfusion Therapy. NeuroSci. 2024; 5(3):291-300. https://doi.org/10.3390/neurosci5030023
Chicago/Turabian StyleSarmiento, Robert Joseph, Amanda Wagner, Asif Sheriff, Colleen Taralson, Nadine Moniz, Jason Opsahl, Thomas Jeerakathil, Brian Buck, William Sevcik, Ashfaq Shuaib, and et al. 2024. "Workflow and Short-Term Functional Outcomes in Simultaneous Acute Code Stroke Activation and Stroke Reperfusion Therapy" NeuroSci 5, no. 3: 291-300. https://doi.org/10.3390/neurosci5030023
APA StyleSarmiento, R. J., Wagner, A., Sheriff, A., Taralson, C., Moniz, N., Opsahl, J., Jeerakathil, T., Buck, B., Sevcik, W., Shuaib, A., & Kate, M. (2024). Workflow and Short-Term Functional Outcomes in Simultaneous Acute Code Stroke Activation and Stroke Reperfusion Therapy. NeuroSci, 5(3), 291-300. https://doi.org/10.3390/neurosci5030023






