Scapular Asymmetries and Dyskinesis in Young Elite Swimmers: Evaluating Static vs. Functional Shoulder Alterations
Abstract
1. Introduction
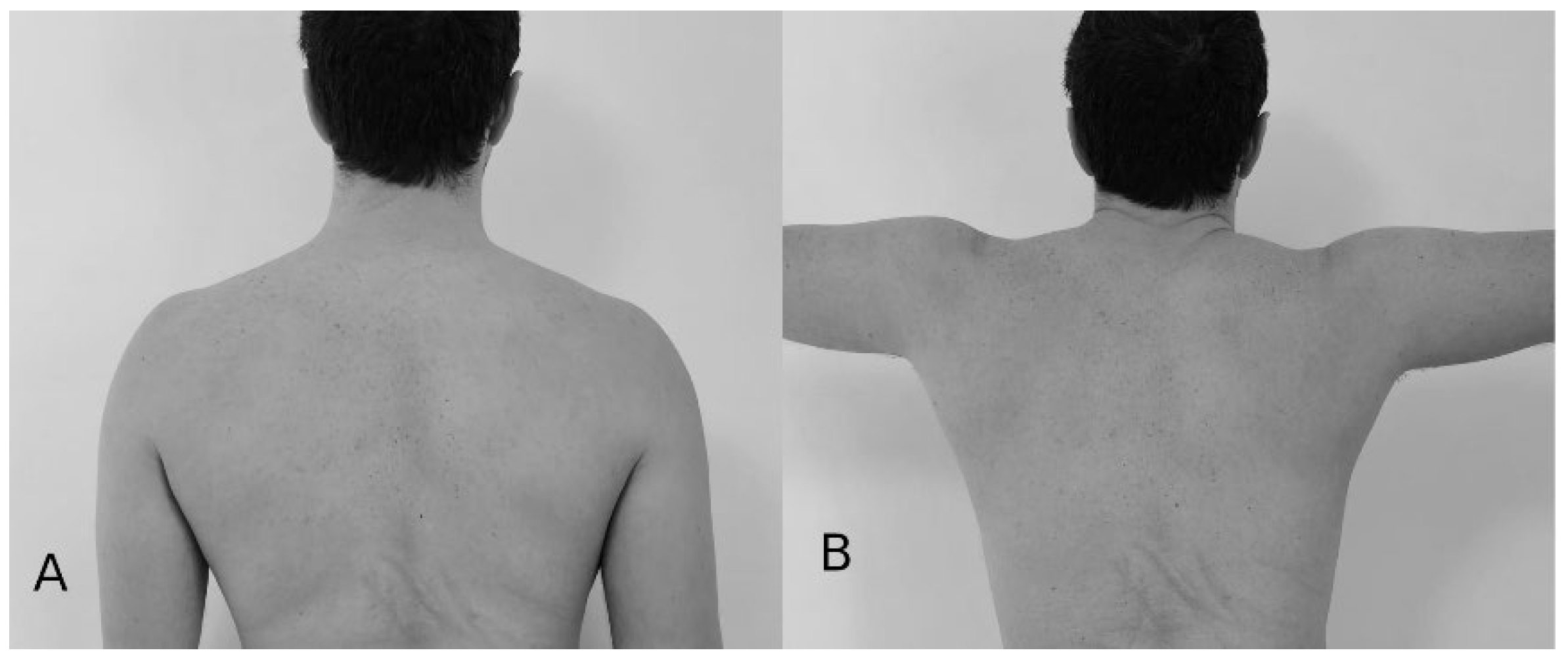
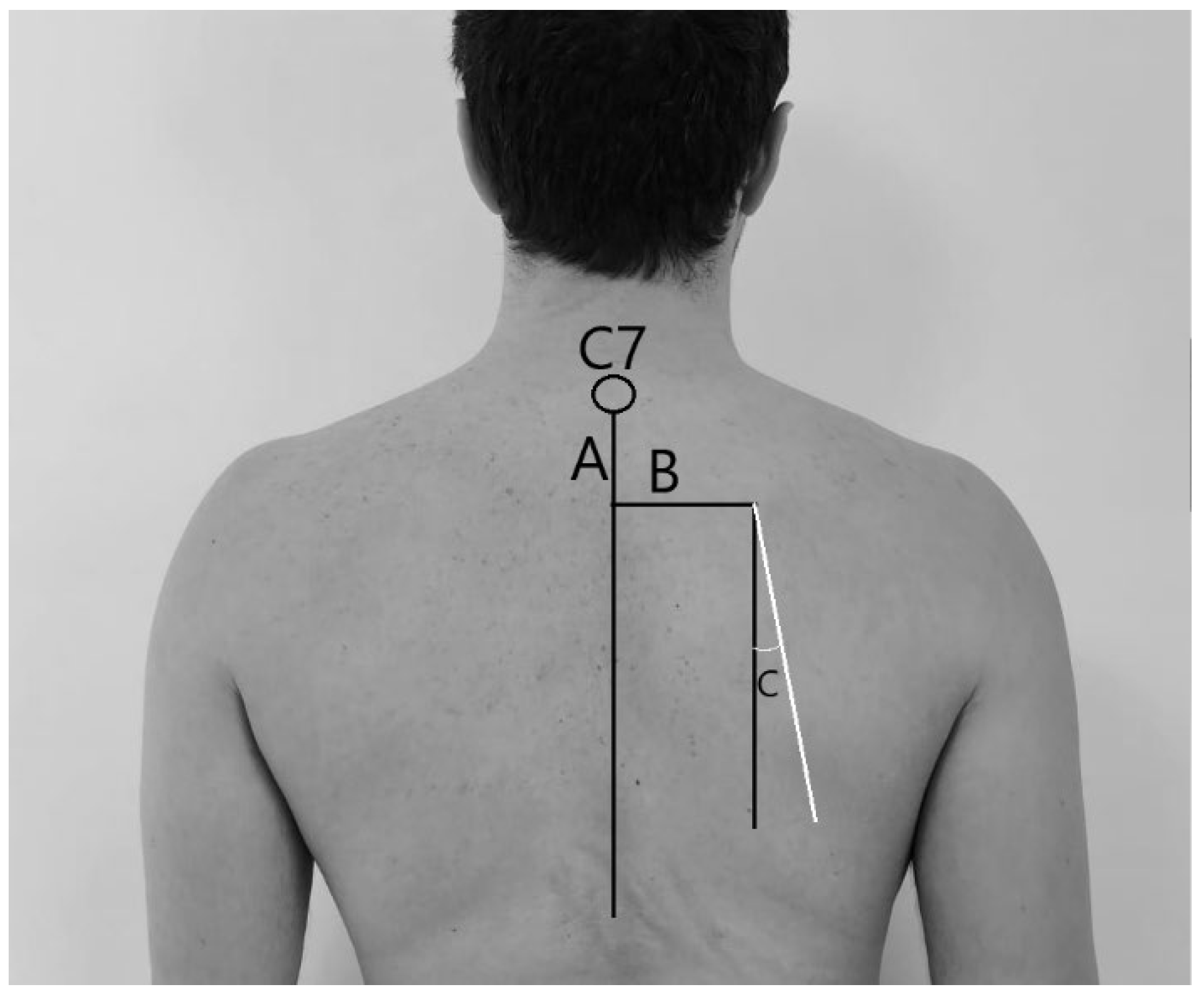
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SA | Scapular asymmetry |
| SD | Scapular dyskinesis |
| GIRD | Glenohumeral internal rotation deficit |
| ROM | Range of movement |
References
- Kibler, W.B. The role of the scapula in athletic shoulder function. Am. J. Sports Med. 1998, 26, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Bakshi, N.; Freehill, M.T. The Overhead Athletes Shoulder. Sports Med. Arthrosc. Rev. 2018, 26, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Lintner, D.; Noonan, T.J.; Kibler, W.B. Injury patterns and biomechanics of the athlete’s shoulder. Clin. Sports Med. 2008, 27, 527–551. [Google Scholar] [CrossRef]
- Shanley, E.; Thigpen, C.A.; Clark, J.; Wyland, D.J.; Hawkins, R.J.; Noonan, T.J.; Kissenberth, M.J. Changes in passive range of motion and development of glenohumeral internal rotation deficit (GIRD) in the professional pitching shoulder between spring training in two consecutive years. J. Shoulder Elb. Surg. 2012, 21, 1605–1612. [Google Scholar] [CrossRef]
- Kibler, B.W.; Sciascia, A.; Wilkes, T. Scapular Dyskinesis and Its Relation to Shoulder Injury. J. Am. Acad. Orthop. Surg. 2012, 20, 364–372. [Google Scholar] [CrossRef]
- Clarsen, B.; Bahr, R.; Andersson, S.H.; Munk, R.; Myklebust, G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: A prospective cohort study. Br. J. Sports Med. 2014, 48, 1327–1333. [Google Scholar] [CrossRef]
- Sciascia, A.; Ben Kibler, W. Current Views of Scapular Dyskinesis and its Possible Clinical Relevance. Int. J. Sports Phys. Ther. 2022, 17, 117–130. [Google Scholar] [CrossRef]
- Asker, M.; Brooke, H.L.; Waldén, M.; Tranaeus, U.; Johansson, F.; Skillgate, E.; Holm, L.W. Risk factors for, and prevention of, shoulder injuries in overhead sports: A systematic review with best-evidence synthesis. Br. J. Sports Med. 2018, 52, 1312–1319. [Google Scholar] [CrossRef] [PubMed]
- Meister, K. Injuries to the shoulder in the throwing athlete. Part two: Evaluation/treatment. Am. J. Sports Med. 2000, 28, 587–601. [Google Scholar] [CrossRef]
- Burkhart, S.S.; Morgan, C.D.; Kibler, W.B. The disabled throwing shoulder: Spectrum of pathology part I: Pathoanatomy and biomechanics. Arthrosc. J. Arthrosc. Relat. Surg. 2003, 19, 404–420. [Google Scholar] [CrossRef]
- Kibler, W.B.; Kuhn, J.E.; Wilk, K.; Sciascia, A.; Moore, S.; Laudner, K.; Ellenbecker, T.; Thigpen, C.; Uhl, T. The Disabled Throwing Shoulder: Spectrum of Pathology—10-Year Update. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 141–161.e26. [Google Scholar] [CrossRef]
- Kibler, W.B.; McMullen, J. Scapular dyskinesis and its relation to shoulder pain. J. Am. Acad. Orthop. Surg. 2003, 11, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.E.; Fullmer, J.A.; Nielsen, C.M.; Johnson, J.K.; Moorman, C.T. Glenohumeral Internal Rotation Deficit and Injuries: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2018, 6, 232596711877332. [Google Scholar] [CrossRef] [PubMed]
- Amin, N.H.; Ryan, J.; Fening, S.D.; Soloff, L.; Schickendantz, M.S.; Jones, M. The Relationship Between Glenohumeral Internal Rotational Deficits, Total Range of Motion, and Shoulder Strength in Professional Baseball Pitchers. J. Am. Acad. Orthop. Surg. 2015, 23, 789–796. [Google Scholar] [CrossRef]
- Holt, K.; Boettcher, C.; Halaki, M.; Ginn, K.A. Humeral torsion and shoulder rotation range of motion parameters in elite swimmers. J. Sci. Med. Sport 2017, 20, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Su, K.P.E.; Johnson, M.P.; Gracely, E.J.; Karduna, A.R. Scapular Rotation in Swimmers with and without Impingement Syndrome: Practice Effects. Med. Sci. Sports Exerc. 2004, 36, 1117–1123. [Google Scholar] [CrossRef]
- Preziosi Standoli, J.; Fratalocchi, F.; Candela, V.; Standoli, T.P.; Giannicola, G.; Bonifazi, M.; Gumina, S. Scapular Dyskinesis in Young, Asymptomatic Elite Swimmers. Orthop. J. Sports Med. 2018, 6, 232596711775081. [Google Scholar] [CrossRef]
- Bak, K.; Faunø, P. Clinical findings in competitive swimmers with shoulder pain. Am. J. Sports Med. 1997, 25, 254–260. [Google Scholar] [CrossRef]
- Struyf, F.; Tate, A.; Kuppens, K.; Feijen, S.; Michener, L.A. Musculoskeletal dysfunctions associated with swimmers’ shoulder. Br. J. Sports Med. 2017, 51, 775–780. [Google Scholar] [CrossRef]
- Preziosi Standoli, J.; Candela, V.; Bonifazi, M.; Gumina, S. Glenohumeral internal rotation deficit in young and asymptomatic elite swimmers. J. Athl. Train. 2023, 59, 731–737. [Google Scholar] [CrossRef]
- Hibberd, E.E.; Laudner, K.; Berkoff, D.J.; Kucera, K.L.; Yu, B.; Myers, J.B. Comparison of Upper Extremity Physical Characteristics Between Adolescent Competitive Swimmers and Nonoverhead Athletes. J. Athl. Train. 2016, 51, 65–69. [Google Scholar] [CrossRef]
- Beach, M.L.; Whitney, S.L.; Dickoff-Hoffman, S.A. Relationship of Shoulder Flexibility, Strength, and Endurance to Shoulder Pain in Competitive Swimmers. J. Orthop. Sports Phys. Ther. 1992, 16, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Riemann, B.L.; Witt, J.; Davies, G.J. Glenohumeral joint rotation range of motion in competitive swimmers. J. Sports Sci. 2011, 29, 1191–1199. [Google Scholar] [CrossRef]
- Hill, L.; Collins, M.; Posthumus, M. Risk factors for shoulder pain and injury in swimmers: A critical systematic review. Phys. Sportsmed. 2015, 43, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Burn, M.B.; McCulloch, P.C.; Lintner, D.M.; Liberman, S.R.; Harris, J.D. Prevalence of Scapular Dyskinesis in Overhead and Nonoverhead Athletes: A Systematic Review. Orthop. J. Sports Med. 2016, 4, 232596711562760. [Google Scholar] [CrossRef]
- Hickey, D.; Solvig, V.; Cavalheri, V.; Harrold, M.; Mckenna, L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 102–110. [Google Scholar] [CrossRef]
- Burkhart, S.S.; Morgan, C.D.; Ben Kibler, W. The disabled throwing shoulder: Spectrum of pathology part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthrosc. J. Arthrosc. Relat. Surg. 2003, 19, 641–661. [Google Scholar] [CrossRef] [PubMed]
- Carbone, S.; Moroder, P.; Runer, A.; Resch, H.; Gumina, S.; Hertel, R. Scapular dyskinesis after Latarjet procedure. J. Shoulder Elb. Surg. 2016, 25, 422–427. [Google Scholar] [CrossRef]
- Gumina, S.; Carbone, S.; Postacchini, F. Scapular Dyskinesis and SICK Scapula Syndrome in Patients with Chronic Type III Acromioclavicular Dislocation. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 40–45. [Google Scholar] [CrossRef]
- Kibler, W.B.; Uhl, T.L.; Maddux, J.W.Q.; Brooks, P.V.; Zeller, B.; McMullen, J. Qualitative clinical evaluation of scapular dysfunction: A reliability study. J. Shoulder Elb. Surg. 2002, 11, 550–556. [Google Scholar] [CrossRef]
- McClure, P.; Tate, A.R.; Kareha, S.; Irwin, D.; Zlupko, E. A Clinical Method for Identifying Scapular Dyskinesis, Part 1: Reliability. J. Athl. Train. 2009, 44, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Uhl, T.L.; Kibler, W.B.; Gecewich, B.; Tripp, B.L. Evaluation of Clinical Assessment Methods for Scapular Dyskinesis. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 1240–1248. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Porterfield, R.; Simpson, C.D.; Harker, P.; Paparesta, N.; Andrews, J.R. Correlation of Glenohumeral Internal Rotation Deficit and Total Rotational Motion to Shoulder Injuries in Professional Baseball Pitchers. Am. J. Sports Med. 2011, 39, 329–335. [Google Scholar] [CrossRef]
- Oyama, S.; Myers, J.B.; Wassinger, C.A.; Ricci, R.D.; Lephart, S.M. Asymmetric Resting Scapular Posture in Healthy Overhead Athletes. J. Athl. Train. 2008, 43, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Borsa, P.A.; Laudner, K.G.; Sauers, E.L. Mobility and Stability Adaptations in the Shoulder of the Overhead Athlete: A Theoretical and Evidence-Based Perspective. Sports Med. 2008, 38, 17–36. [Google Scholar] [CrossRef]
- Yeşilyaprak, S.S. Kinesiology of the shoulder complex. In Comparative Kinesiology of the Human Body; Academic Press: Cambridge, MA, USA, 2020; pp. 157–190. [Google Scholar] [CrossRef]
- Schenkman, M.; Rugo de Cartaya, V. Kinesiology of the shoulder complex. J. Orthop. Sports Phys. Ther. 1987, 8, 438–450. [Google Scholar] [CrossRef]
- Burkhart, S.S.; Morgan, C.D.; Kibler, W.B. The disabled throwing shoulder: Spectrum of Pathology Part II: Evaluation and treatment of SLAP lesions in throwers. Arthrosc. J. Arthrosc. Relat. Surg. 2003, 19, 531–539. [Google Scholar] [CrossRef]
- Ellenbecker, T.S.; Roetert, E.P.; Bailie, D.S.; Davies, G.J.; Brown, S.W. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med. Sci. Sports Exerc. 2002, 34, 2052–2056. [Google Scholar] [CrossRef]
- Salamh, P.A.; Hanney, W.J.; Boles, T.; Holmes, D.; McMillan, A.; Wagner, A.; Kolber, M.J. Is it Time to Normalize Scapular Dyskinesis? The Incidence of Scapular Dyskinesis in Those with and Without Symptoms: A Systematic Review of the Literature. Int. J. Sports Phys. Ther. 2023, 18, 558–576. [Google Scholar] [CrossRef]
- Matsuki, K.; Matsuki, K.O.; Mu, S.; Yamaguchi, S.; Ochiai, N.; Sasho, T.; Sugaya, H.; Toyone, T.; Wada, Y.; Takahashi, K.; et al. In vivo 3-dimensional analysis of scapular kinematics: Comparison of dominant and nondominant shoulders. J. Shoulder Elbow Surg. 2011, 20, 659–665. [Google Scholar] [CrossRef] [PubMed]
| dAngle | dDistance | dHeight | |
|---|---|---|---|
| Position 1 | Mean (St.Dev.) | Mean (St.Dev.) | Mean (St.Dev.) |
| Female | 2.53 (2.41) | 0.75 (0.57) | 0.69 (0.47) |
| Male | 2.51 (2.67) | 0.73 (0.52) | 0.73 (0.52) |
| Total | 2.52 (2.54) | 0.74 (0.54) | 0.71 (0.50) |
| dAngle | dDistance | dHeight | |
| Position 2 | Mean (St.Dev.) | Mean (St.Dev.) | Mean (St.Dev.) |
| Female | 3.51 (3.07) | 0.65 (0.63) | 0.65 (0.49) |
| Male | 3.37 (2.99) | 0.63 (0.52) | 0.73 (0.55) |
| Total | 3.44 (3.03) | 0.64 (0.58) | 0.69 (0.52) |
| Position 1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| dAngle | dDistance | dHeight | |||||||
| N | % | SE | N | % | SE | N | % | SE | |
| Right | 46 | 6.96 | 0.009 | 29 | 4.39 | 0.007 | 45 | 6.81 | 0.009 |
| Normal | 563 | 85.17 | 0.013 | 601 | 90.92 | 0.01 | 590 | 89.26 | 0.01 |
| Left | 52 | 7.87 | 0.010 | 31 | 4.69 | 0.008 | 26 | 3.93 | 0.007 |
| Position 2 | |||||||||
| dAngle | dDistance | dHeight | |||||||
| N | % | SE | N | % | SE | N | % | SE | |
| Right | 102 | 15.43 | 0.014 | 31 | 4.69 | 0.008 | 24 | 3.63 | 0.007 |
| Normal | 477 | 72.16 | 0.017 | 613 | 92.74 | 0.009 | 590 | 89.26 | 0.011 |
| Left | 82 | 12.41 | 0.012 | 17 | 2.57 | 0.006 | 47 | 7.11 | 0.01 |
| Position 1 | ||||||||||||
| dAngle | dDistance | dHeight | ||||||||||
| Right | Normal | Left | p-value | Right | Normal | Left | p-value | Right | Normal | Left | p-value | |
| Dominant Limb | ||||||||||||
| Left | 4 | 63 | 4 | 0.66 | 2 | 66 | 3 | 0.77 | 4 | 63 | 4 | 0.69 |
| Right | 42 | 500 | 48 | 27 | 535 | 28 | 41 | 527 | 22 | |||
| Position 2 | ||||||||||||
| dAngle | dDistance | dHeight | ||||||||||
| Right | Normal | Left | p-value | Right | Normal | Left | p-value | Right | Normal | Left | p-value | |
| Dominant Limb | ||||||||||||
| Left | 6 | 57 | 8 | 0.19 | 3 | 66 | 2 | 0.97 | 0 | 62 | 9 | 0.04 |
| Right | 96 | 420 | 74 | 28 | 547 | 15 | 24 | 528 | 38 |
| Position 1 | Subjects (N) | SD Present | SE | SD Absent | SE | p-Value |
| dHeight | 71 | 14 | 0.04 | 57 | 0.04 | <0.001 |
| dDistance | 62 | 10 | 0.04 | 52 | 0.04 | 0.016 |
| dAngle | 100 | 12 | 0.032 | 88 | 0.032 | >0.05 |
| Position 2 | Subjects (N) | SD Present | SE | SD Absent | SE | p-Value |
| dHeight | 72 | 7 | 0.035 | 65 | 0.035 | >0.05 |
| dDistance | 48 | 8 | 0.05 | 40 | 0.05 | 0.02 |
| dAngle | 184 | 23 | 0.02 | 161 | 0.02 | 0.014 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Preziosi Standoli, J.; Preziosi Standoli, T. Scapular Asymmetries and Dyskinesis in Young Elite Swimmers: Evaluating Static vs. Functional Shoulder Alterations. Osteology 2025, 5, 22. https://doi.org/10.3390/osteology5030022
Preziosi Standoli J, Preziosi Standoli T. Scapular Asymmetries and Dyskinesis in Young Elite Swimmers: Evaluating Static vs. Functional Shoulder Alterations. Osteology. 2025; 5(3):22. https://doi.org/10.3390/osteology5030022
Chicago/Turabian StylePreziosi Standoli, Jacopo, and Tiziano Preziosi Standoli. 2025. "Scapular Asymmetries and Dyskinesis in Young Elite Swimmers: Evaluating Static vs. Functional Shoulder Alterations" Osteology 5, no. 3: 22. https://doi.org/10.3390/osteology5030022
APA StylePreziosi Standoli, J., & Preziosi Standoli, T. (2025). Scapular Asymmetries and Dyskinesis in Young Elite Swimmers: Evaluating Static vs. Functional Shoulder Alterations. Osteology, 5(3), 22. https://doi.org/10.3390/osteology5030022





