Babesiosis and Malaria in the United States: Epidemiology, Research Funding, Medical Progress, & Recommendations for Improvement
Abstract
1. Introduction
2. Methods
2.1. Epidemiologic Data
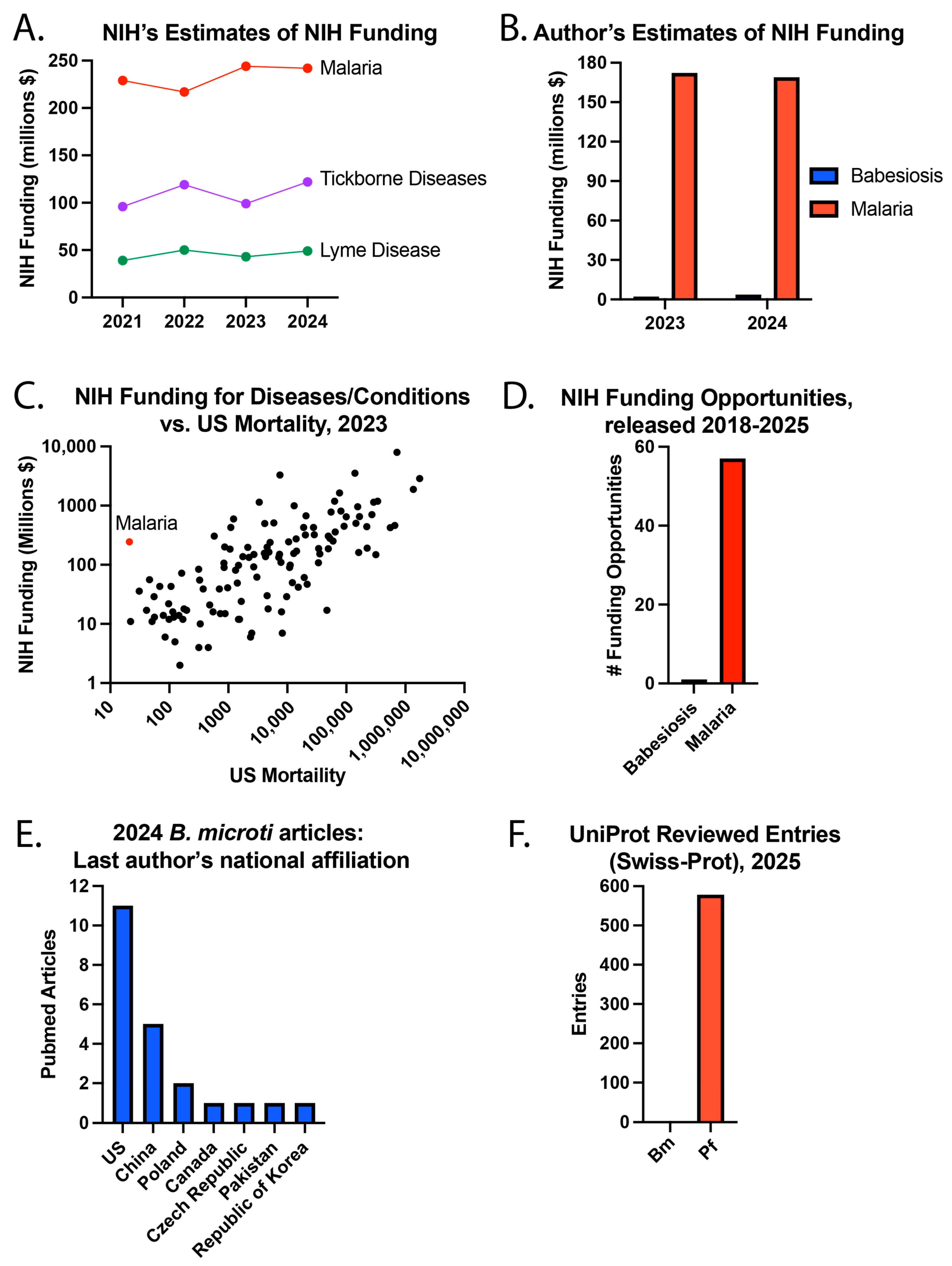
2.2. NIH Funding Estimates
2.3. Bm Articles on PubMed
3. Results
3.1. Recent US Public Health Efforts
3.2. Cases in the US
3.3. Deaths of US Residents
3.4. Funding Estimates and Published Articles
3.5. History
3.6. Medical Progress
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, Y.; Christie, J.; Köster, L.; Du, A.; Yao, C. Emerging Human Babesiosis with “Ground Zero” in North America. Microorganisms 2021, 9, 440. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Swanson, M.; Pickrel, A.; Williamson, J.; Montgomery, S. Trends in Reported Babesiosis Cases—United States, 2011–2019. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 273–277. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gray, E.B.; Herwaldt, B.L. Babesiosis Surveillance—United States, 2011–2015. MMWR Surveill Summ. 2019, 68, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Rogers, R.; Krause, P.J.; Norris, A.M.; Ting, M.H.; Nagami, E.H.; Cilley, B.; Vannier, E. Broad Antimicrobial Resistance in a Case of Relapsing Babesiosis Successfully Treated with Tafenoquine. Clin. Infect. Dis. 2022, 76, 741–744. [Google Scholar] [CrossRef]
- Krause, P.J. Human babesiosis. Int. J. Parasitol. 2019, 49, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Jajosky, R.P.; Jajosky, A.N.; Jajosky, P.G.; Stowell, S.R. Do Babesia microti Hosts Share a Blood Group System Gene Ortholog, Which Could Generate an Erythrocyte Antigen That Is Essential for Parasite Invasion? Trop. Med. Infect. Dis. 2024, 9, 195. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matz, J.M. Plasmodium’s bottomless pit: Properties and functions of the malaria parasite’s digestive vacuole. Trends Parasitol. 2022, 38, 525–543. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, P. Haemoprotozoa: Making biological sense of molecular phylogenies. Int. J. Parasitol. Parasites Wildl. 2017, 6, 241–256. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sojka, D.; Jalovecká, M.; Perner, J. Babesia, Theileria, Plasmodium and Hemoglobin. Microorganisms 2022, 10, 1651. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, W.-C.; Russell, B.; Rénia, L. Sticking for a Cause: The Falciparum Malaria Parasites Cytoadherence Paradigm. Front. Immunol. 2019, 10, 1444. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bourgeois, J.S.; You, S.S.; Clendenen, L.H.; Shrestha, M.; Petnicki-Ocwieja, T.; Telford, S.R.; Hu, L.T. Comparative reservoir competence of Peromyscus leucopus, C57BL/6J, and C3H/HeN for Borrelia burgdorferi B31. Appl. Environ. Microbiol. 2024, 90, e00822-24. [Google Scholar] [CrossRef] [PubMed]
- CDC. CDC WONDER 2025. Available online: https://wonder.cdc.gov/ (accessed on 1 August 2025).
- CDC. Babesiosis Case Definition. Available online: https://ndc.services.cdc.gov/case-definitions/babesiosis/ (accessed on 1 August 2025).
- CDC. Babesiosis (Babesia spp.) 2011 Case Definition: CDC. 2021. Available online: https://ndc.services.cdc.gov/case-definitions/babesiosis-2011/ (accessed on 1 August 2025).
- CDC. Malaria (Plasmodium spp.) 2014 Case Definition. Available online: https://ndc.services.cdc.gov/case-definitions/malaria-2014/ (accessed on 1 August 2025).
- CDC. NNDSS Event Codes & Other Surveillance Resources: CDC. 2025. Available online: https://ndc.services.cdc.gov/event-codes-other-surveillance-resources/ (accessed on 1 August 2025).
- NIH. NIH RePORT Funding: NIH. 2025. Available online: https://report.nih.gov/funding/categorical-spending#/ (accessed on 1 August 2025).
- NIH. NIH Reporter: 2025. 2025. Available online: https://reporter.nih.gov/advanced-search (accessed on 1 August 2025).
- CDC. How to Report a Case of Malaria. Available online: https://www.cdc.gov/malaria/php/case-reporting/index.html (accessed on 1 August 2025).
- CDC. About Mosquitoes in the United States 2024. Available online: https://www.cdc.gov/mosquitoes/about/about-mosquitoes-in-the-united-states.html (accessed on 1 August 2025).
- CDC. NCEZID Strategic Plan 2024. Available online: https://www.cdc.gov/ncezid/strategic-plan/index.html (accessed on 1 August 2025).
- CDC. National Notifiable Diseases Surveillance System (NNDSS): CDC. Available online: https://www.cdc.gov/nchs/hus/sources-definitions/nndss.htm (accessed on 1 August 2025).
- Ingram, D.; Crook, T. Rise in Babesiosis Cases, Pennsylvania, USA, 2005–2018. Emerg. Infect. Dis. 2020, 26, 1703–1709. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- CDC. National Notifiable Diseases Surveillance System (NNDSS) Annual Summary Data 2016–2022. 2025. Available online: https://wonder.cdc.gov/wonder/help/nndss.html# (accessed on 1 August 2025).
- CDC. Malaria Surveillance, United States. 2022. Available online: https://www.cdc.gov/malaria/php/surveillance-report/2022.html (accessed on 1 August 2025).
- WHO. World Malaria Report 2024. 2024. Available online: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2024 (accessed on 1 August 2025).
- Ixodes Scapularis Life Cycle: University of Wisconsin—Madison. 2011. Available online: https://wisconsin-ticks.russell.wisc.edu/ixodes-scapularis-life-cycle/ (accessed on 1 August 2025).
- Rocha, L.E.C.; Thorson, A.E.; Lambiotte, R. The Non-linear Health Consequences of Living in Larger Cities. J. Urban Health 2015, 92, 785–799. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- CDC. CDC WONDER Data Use Restrictions 2025. Available online: https://wonder.cdc.gov/datause.html# (accessed on 1 August 2025).
- FDA. Transfusion/Donation Fatalities. Available online: https://www.fda.gov/vaccines-blood-biologics/report-problem-center-biologics-evaluation-research/transfusiondonation-fatalities (accessed on 1 August 2025).
- FDA. Babesia microti NAT/Babesia microti NAT for Blood Screening. Available online: https://www.fda.gov/vaccines-blood-biologics/approved-blood-products/babesia-microti-natbabesia-microti-nat-blood-screening (accessed on 1 August 2025).
- Tonnetti, L.; Dodd, R.Y.; Foster, G.; Stramer, S.L. Babesia blood testing: The first-year experience. Transfusion 2022, 62, 135–142. [Google Scholar] [CrossRef] [PubMed]
- NIH. NIH Guide for Grants and Contracts. Available online: https://grants.nih.gov/funding/nih-guide-for-grants-and-contracts (accessed on 1 August 2025).
- CDC. Zika Cases in the United States 2025. Available online: https://www.cdc.gov/zika/zika-cases-us/index.html (accessed on 1 August 2025).
- Kretschmer, M.; Ruberto, I.; Townsend, J.; Zabel, K.; Will, J.; Maldonado, K.; Busser, N.; Damian, D.; Dale, A.P. Unprecedented Outbreak of West Nile Virus—Maricopa County, Arizona, 2021. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 452–457. [Google Scholar] [CrossRef] [PubMed]
- KFF. The President’s Malaria Initiative and Other U.S. Government Global Malaria Efforts 2025. Available online: https://www.kff.org/global-health-policy/fact-sheet/the-presidents-malaria-initiative-and-other-u-s-government-global-malaria-efforts/ (accessed on 1 August 2025).
- KFF. The Trump Administration’s Foreign Aid Review: Status of U.S. Support for the Global Fund to Fight AIDS, Tuberculosis and Malaria 2025. Available online: https://www.kff.org/global-health-policy/fact-sheet/the-trump-administrations-foreign-aid-review-status-of-u-s-support-for-the-global-fund-to-fight-aids-tuberculosis-and-malaria/ (accessed on 1 August 2025).
- KFF. The Trump Administration’s Foreign Aid Review: Status of the President’s Malaria Initiative (PMI) 2025. Available online: https://www.kff.org/global-health-policy/the-trump-administrations-foreign-aid-review-status-of-the-presidents-malaria-initiative-pmi/ (accessed on 1 August 2025).
- Uniprot. Available online: https://www.uniprot.org/ (accessed on 1 August 2025).
- McCandless, P. Revolutionary fever: Disease and war in the Lower South, 1776–1783. Trans. Am. Clin. Climatol. Assoc. 2007, 118, 225–249. [Google Scholar] [PubMed] [PubMed Central]
- Mertens, J.E. A History of Malaria and Conflict. Parasitol Res. 2024, 123, 165. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tiwari, A.; Sinha, A. Etymologia: Falciparum. Emerg. Infect. Dis. 2021, 27, 470. [Google Scholar] [CrossRef]
- CDC. The History of Malaria in the United States. Available online: https://www.cdc.gov/malaria/history/index.html (accessed on 1 August 2025).
- Raju, T.N. The Nobel chronicles. 1946: Hermann Joseph Muller (1890-1967). Lancet 1999, 353, 1023. [Google Scholar] [CrossRef] [PubMed]
- Carson, R. Silent Spring; Houghton Mifflin Harcourt: Boston, USA, 1962. [Google Scholar]
- Gray, J.S.; Ogden, N.H. Ticks, Human Babesiosis and Climate Change. Pathogens 2021, 10, 1430. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ostfeld, R.S.; Brunner, J.L. Climate change and Ixodes tick-borne diseases of humans. Trans. R. Soc. B Biol. Sci. 2015, 370, 20140051. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stromdahl, E.Y.; A Feldman, K.; Nadolny, R.M.; Kennedy, A.C.; Bement, Z.J.; Buoni, M.; Rutz, H.; Broyhill, J.C.; Bernick, J.; Brinkerhoff, R.J.; et al. Emerging babesiosis in the mid-Atlantic: Autochthonous human babesiosis cases and Babesia microti (Piroplasmida: Babesiidae) in Ixodes scapularis (Acari: Ixodidae) and Ixodes keiransi (Acari: Ixodidae) ticks from Delaware, Maryland, Virginia, West Virginia, and the District of Columbia, 2009 to 2024. J. Med. Entomol. 2025, 62, 995–1008. [Google Scholar] [CrossRef] [PubMed]
- Tse, E.G.; Korsik, M.; Todd, M.H. The past, present and future of anti-malarial medicines. Malar. J. 2019, 18, 93. [Google Scholar] [CrossRef]
- Talapko, J.; Škrlec, I.; Alebić, T.; Jukić, M.; Včev, A. Malaria: The Past and the Present. Microorganisms 2019, 7, 179. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- CDC. Drug Resistance in the Malaria-Endemic World 2024. Available online: https://www.cdc.gov/malaria/php/public-health-strategy/drug-resistance.html (accessed on 1 August 2025).
- Zimring, J.C.; Hudson, K.E. Cellular immune responses in red blood cell alloimmunization. Hematol. Am. Soc. Hematol. Educ. Program 2016, 2016, 452–456. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pirenne, F.; Floch, A.; Diop, S. Alloimmunisation against red blood cells in sickle cell disease: Transfusion challenges in high-income and low-income countries. Lancet Haematol. 2023, 10, e468–e476. [Google Scholar] [CrossRef] [PubMed]
- Jajosky, R.P.; Wu, S.-C.; Zheng, L.; Jajosky, A.N.; Jajosky, P.G.; Josephson, C.D.; Hollenhorst, M.A.; Sackstein, R.; Cummings, R.D.; Arthur, C.M.; et al. ABO blood group antigens and differential glycan expression: Perspective on the evolution of common human enzyme deficiencies. iScience 2023, 26, 105798. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yazdanbakhsh, K.; Ware, R.E.; Noizat-Pirenne, F. Red blood cell alloimmunization in sickle cell disease: Pathophysiology, risk factors, and transfusion management. Blood 2012, 120, 528–537. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Arthur, C.M.; Chonat, S.; Fasano, R.; Yee, M.E.; Josephson, C.D.; Roback, J.D.; Stowell, S.R. Examining the Role of Complement in Predicting, Preventing, and Treating Hemolytic Transfusion Reactions. Transfus. Med. Rev. 2019, 33, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Arthur, C.M.; Stowell, S.R. The Development and Consequences of Red Blood Cell Alloimmunization. Annu. Rev. Pathol. 2023, 18, 537–564. [Google Scholar] [CrossRef] [PubMed]
- Cserti, C.M.; Dzik, W.H. The ABO blood group system and Plasmodium falciparum malaria. Blood 2007, 110, 2250–2258. [Google Scholar] [CrossRef] [PubMed]
- Rowe, J.A.; Handel, I.G.; Thera, M.A.; Deans, A.-M.; Lyke, K.E.; Koné, A.; Diallo, D.A.; Raza, A.; Kai, O.; Marsh, K.; et al. Blood group O protects against severe Plasmodium falciparum malaria through the mechanism of reduced rosetting. Proc. Natl. Acad. Sci. USA 2007, 104, 17471–17476. [Google Scholar] [CrossRef]
- Wolf, J.; Blais-Normandin, I.; Bathla, A.; Keshavarz, H.; Chou, S.T.; Al-Riyami, A.Z.; Josephson, C.D.; Massey, E.; Hume, H.A.; Pendergrast, J.; et al. Red cell specifications for blood group matching in patients with haemoglobinopathies: An updated systematic review and clinical practice guideline from the International Collaboration for Transfusion Medicine Guidelines. Br. J. Haematol. 2025, 206, 94–108. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maier, C.L.; Jajosky, R.P.; Patel, S.R.; Verkerke, H.P.; Fuller, M.D.; Allen, J.W.; Zerra, P.E.; Fasano, R.M.; Chonat, S.; Josephson, C.D.; et al. Storage differentially impacts alloimmunization to distinct red cell antigens following transfusion in mice. Transfusion 2023, 63, 457–462. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jajosky, R.P.; Patel, S.R.; Wu, S.-C.; Patel, K.R.; Covington, M.L.; Vallecillo-Zúniga, M.L.; Ayona, D.; Bennett, A.; Luckey, C.J.; E Hudson, K.; et al. Prior immunization against an intracellular antigen enhances subsequent red blood cell alloimmunization in mice. Blood 2023, 141, 2642–2653. [Google Scholar] [CrossRef] [PubMed]
- Jajosky, R.P.; Covington, M.L.; Liu, J.; Chai, L.; Zerra, P.E.; Chonat, S.; Stowell, S.R.; Arthur, C.M. CD47 regulates antigen modulation and red blood cell clearance following an incompatible transfusion. Front. Immunol. 2025, 16, 1548548. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zerra, P.E.; Patel, S.R.; Jajosky, R.P.; Arthur, C.M.; McCoy, J.W.; Allen, J.W.L.; Chonat, S.; Fasano, R.M.; Roback, J.D.; Josephson, C.D.; et al. Marginal zone B cells mediate a CD4 T-cell-dependent extrafollicular antibody response following RBC transfusion in mice. Blood 2021, 138, 706–721. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mener, A.; Patel, S.R.; Arthur, C.M.; Chonat, S.; Wieland, A.; Santhanakrishnan, M.; Liu, J.; Maier, C.L.; Jajosky, R.P.; Girard-Pierce, K.; et al. Complement serves as a switch between CD4+ T cell-independent and -dependent RBC antibody responses. JCI Insight 2018, 3, e121631. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jajosky, R.P.; Ayona, D.; Mener, A.; Stowell, S.R.; Arthur, C.M. Dynamics of antibody engagement of red blood cells in vivo and in vitro. Front. Immunol. 2024, 15, 1475470. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jajosky, R.P.; Patel, K.R.; Allen, J.W.L.; Zerra, P.E.; Chonat, S.; Ayona, D.; Maier, C.L.; Morais, D.; Wu, S.-C.; Luckey, C.J.; et al. Antibody-mediated antigen loss switches augmented immunity to antibody-mediated immunosuppression. Blood 2023, 142, 1082–1098. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sullivan, H.C.; Gerner-Smidt, C.; Nooka, A.K.; Arthur, C.M.; Thompson, L.; Mener, A.; Patel, S.R.; Yee, M.; Fasano, R.M.; Josephson, C.D.; et al. Daratumumab (anti-CD38) induces loss of CD38 on red blood cells. Blood 2017, 129, 3033–3037. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chonat, S.; Jones, J.A.; Patel, S.R.; Briones, W.M.; Schoettler, M.L.; Maarouf, M.; Jeffers, L.A.; Adisa, O.; Tan, F.; Fields, E.; et al. Complement is activated in patients with acute chest syndrome caused by sickle cell disease and represents a therapeutic target. Sci. Transl. Med. 2025, 17, eadl4922. [Google Scholar] [CrossRef] [PubMed]
- Nickel, R.S.; Hendrickson, J.E.; Fasano, R.M.; Meyer, E.K.; Winkler, A.M.; Yee, M.M.; Lane, P.A.; Jones, Y.A.; Pashankar, F.D.; New, T.; et al. Impact of red blood cell alloimmunization on sickle cell disease mortality: A case series. Transfusion 2016, 56, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Dean, C.L.; Maier, C.L.; Roback, J.D.; Stowell, S.R. Multiple hemolytic transfusion reactions misinterpreted as severe vaso-occlusive crisis in a patient with sickle cell disease. Transfusion 2019, 59, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Dean, C.L.; Maier, C.L.; Chonat, S.; Chang, A.; Carden, M.A.; El Rassi, F.; McLemore, M.L.; Stowell, S.R.; Fasano, R.M. Challenges in the treatment and prevention of delayed hemolytic transfusion reactions with hyperhemolysis in sickle cell disease patients. Transfusion 2019, 59, 1698–1705. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.H.; Mason, S.J.; Dvorak, J.A.; McGinniss, M.H.; Rothman, I.K. Erythrocyte receptors for (Plasmodium knowlesi) malaria: Duffy blood group determinants. Science 1975, 189, 561–563. [Google Scholar] [CrossRef] [PubMed]
- Jajosky, R.P.; Wu, S.-C.; Jajosky, P.G.; Stowell, S.R. Plasmodium knowlesi (Pk) Malaria: A Review & Proposal of Therapeutically Rational Exchange (T-REX) of Pk-Resistant Red Blood Cells. Trop. Med. Infect. Dis. 2023, 8, 478. [Google Scholar] [CrossRef]
- Miller, L.H.; Mason, S.J.; Clyde, D.F.; McGinniss, M.H. The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy. N. Engl. J. Med. 1976, 295, 302–304. [Google Scholar] [CrossRef] [PubMed]
- Dame, J.B.; Williams, J.L.; McCutchan, T.F.; Weber, J.L.; Wirtz, R.A.; Hockmeyer, W.T.; Maloy, W.L.; Haynes, J.D.; Schneider, I.; Roberts, D.; et al. Structure of the Gene Encoding the Immunodominant Surface Antigen on the Sporozoite of the Human Malaria Parasite Plasmodium falciparum. Science 1984, 225, 593–599. [Google Scholar] [CrossRef]
- Trager, W.; Jensen, J.B. Human malaria parasites in continuous culture. Science 1976, 193, 673–675. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.G.; King, L.D.W.; Pulido, D.; Quinkert, D.; Lias, A.M.; Silk, S.E.; Ragotte, R.J.; Davies, H.; Barrett, J.R.; McHugh, K.; et al. Development of an improved blood-stage malaria vaccine targeting the essential RH5-CyRPA-RIPR invasion complex. Nat. Commun. 2024, 15, 4857. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- CDC. Clinical Care of Babesiosis 2024. Available online: https://www.cdc.gov/babesiosis/hcp/clinical-care/index.html (accessed on 1 August 2025).
- Turner, L.; Diaz, T.N.d.V.; Raghavan, S.S.R.; Kana, I.H.; Lyimo, E.; Reitzel, C.; Wang, C.W.; Berube, E.; Jensen, R.W.; Loeffler, J.R.; et al. Identification of broadly inhibitory anti-PfEMP1 antibodies by mass spectrometry sequencing of plasma IgG from a malaria-exposed child. Proc. Natl. Acad. Sci. USA 2025, 122, e2508744122. [Google Scholar] [CrossRef]
- Molina-Franky, J.; Patarroyo, M.E.; Kalkum, M.; Patarroyo, M.A. The Cellular and Molecular Interaction Between Erythrocytes and Plasmodium falciparum Merozoites. Front. Cell. Infect. Microbiol. 2022, 12, 816574. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fuller, L. Continuous in vitro propagation of Babesia microti. Infect. Immun. 2024, 92, e0048123. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zabala, G.A.; Lever, R.; Chan, X.H.; Bristowe, H.; Kilbride, E.; Richards, D.; Daly, M.; Brown, M.; Johnson, N.; Nabarro, L.E.; et al. Autochthonous Human Babesia divergens Infection, England. Emerg. Infect. Dis. 2024, 30, 2165–2168. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jajosky, R.; Jajosky, A.; Jajosky, P. Optimizing exchange transfusion for patients with severe Babesia divergens babesiosis: Therapeutically-Rational Exchange (T-REX) of M antigen-negative and/or S antigen-negative red blood cells should be evaluated now. Transfus. Clin. Biol. 2019, 26, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Jajosky, R.P.; O’bRyan, J.; Spichler-Moffarah, A.; Jajosky, P.G.; Krause, P.J.; Tonnetti, L. The impact of ABO and RhD blood types on Babesia microti infection. PLoS Negl. Trop. Dis. 2023, 17, e0011060. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tyagi, R.K.; Tandel, N.; Deshpande, R.; Engelman, R.W.; Patel, S.D.; Tyagi, P. Humanized Mice Are Instrumental to the Study of Plasmodium falciparum Infection. Front. Immunol. 2018, 9, 2550. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- $1 Million Grant Awarded to Study Babesiosis 2009. Available online: https://ysph.yale.edu/news-article/1-million-grant-awarded-to-study-babesiosis/ (accessed on 21 October 2025).
- Kavanagh, P.L.; Fasipe, T.A.; Wun, T. Sickle Cell Disease: A Review. JAMA 2022, 328, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Hale, R.C.; Morais, D.; Chou, J.; Stowell, S.R. The role of glycosylation in clinical allergy and immunology. J. Allergy Clin. Immunol. 2024, 153, 55–66. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- CDC. Life Expectancy. Available online: https://www.cdc.gov/nchs/fastats/life-expectancy.htm (accessed on 1 August 2025).
- Rare and Orphan Diseases: Cleveland Clinic; 2024. Available online: https://my.clevelandclinic.org/health/diseases/rare-and-orphan-diseases (accessed on 1 August 2025).
- Kwiatkowski, D.P. How malaria has affected the human genome and what human genetics can teach us about malaria. Am. J. Hum. Genet. 2005, 77, 171–192. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gaudinski, M.R.; Berkowitz, N.M.; Idris, A.H.; Coates, E.E.; Holman, L.A.; Mendoza, F.; Gordon, I.J.; Plummer, S.H.; Trofymenko, O.; Hu, Z.; et al. A Monoclonal Antibody for Malaria Prevention. N. Engl. J. Med. 2021, 385, 803–814. [Google Scholar] [CrossRef] [PubMed]
- Kayentao, K.; Ongoiba, A.; Preston, A.C.; Healy, S.A.; Hu, Z.; Skinner, J.; Doumbo, S.; Wang, J.; Cisse, H.; Doumtabe, D.; et al. Subcutaneous Administration of a Monoclonal Antibody to Prevent Malaria. N. Engl. J. Med. 2024, 390, 1549–1559. [Google Scholar] [CrossRef]
- Naidoo, K.; Oliver, S.V. Gene drives: An alternative approach to malaria control? Gene Therapy 2025, 32, 25–37. [Google Scholar] [CrossRef]
- Ross, J.J.; Carlile, N.; Ard, K.L. Increasing Length of the Babesia Season in New England in the Climate Change Era. Open Forum. Infect. Dis. 2025, 12, ofaf458. [Google Scholar] [CrossRef]
- Acosta, A.L.; Castro, M.C.; Laporta, G.Z.; Conn, J.E.; Sallum, M.A.M. Future global distribution and climatic suitability of Anopheles stephensi. Sci. Rep. 2025, 15, 22268. [Google Scholar] [CrossRef] [PubMed]


| Bm Babesiosis | Pf Malaria | |
|---|---|---|
| Endemic in US | Yes (and spreading geographically) | No (eliminated in 1951) |
| 1st human case acquired & reported in the US | 1969 | Colonial times |
| High risk for severe disease | Elderly, asplenic, immunocompromised | Children, those with certain blood types |
| Most human cases in the world | US | Nigeria [26] |
| Foreign significance | As many as ~300 symptomatic human cases in China [1] | Hundreds of millions of cases globally and hundreds of thousands of deaths |
| Key mammalian hosts | Mice | Humans |
| Vectors (definitive hosts) | Ticks | Mosquitoes |
| Parasite stages in humans | Erythrocytic | Hepatic & Erythrocytic |
| Free CDC testing after diagnosis | No | Yes |
| Led to drug development & approval | No | Yes (e.g., quinine, chloroquine, artesunate, artemether, etc.) |
| Drug resistant strains | Yes | Yes |
| Chemoprophylaxis for humans | No | Yes |
| Vaccines | None for humans | RTS,S & R21 |
| Blood donor precautions | Babesia NAT testing | Foreign travel & residence deferrals |
| Impact of RBC antigens on disease | Very few studies [85] | Extensively studied |
| UniProt reviewed entries (Swiss-Prot) | 0 entries | 578 entries |
| Parasite ligand & RBC receptor pairs | No pairs identified | Many pairs identified (e.g., PfRh5 and basigin) |
| Continuous in vitro cultures in human RBCs | Published in 2024 [82] | Published in 1976 [77] |
| Small animal models of disease | B. microti naturally infects mice | Pf can infect humanized mice [86] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jajosky, R.P.; Li, W.; Jajosky, A.N.; Jajosky, P.G.; Stowell, S.R. Babesiosis and Malaria in the United States: Epidemiology, Research Funding, Medical Progress, & Recommendations for Improvement. Epidemiologia 2025, 6, 76. https://doi.org/10.3390/epidemiologia6040076
Jajosky RP, Li W, Jajosky AN, Jajosky PG, Stowell SR. Babesiosis and Malaria in the United States: Epidemiology, Research Funding, Medical Progress, & Recommendations for Improvement. Epidemiologia. 2025; 6(4):76. https://doi.org/10.3390/epidemiologia6040076
Chicago/Turabian StyleJajosky, Ryan P., Wenhui Li, Audrey N. Jajosky, Philip G. Jajosky, and Sean R. Stowell. 2025. "Babesiosis and Malaria in the United States: Epidemiology, Research Funding, Medical Progress, & Recommendations for Improvement" Epidemiologia 6, no. 4: 76. https://doi.org/10.3390/epidemiologia6040076
APA StyleJajosky, R. P., Li, W., Jajosky, A. N., Jajosky, P. G., & Stowell, S. R. (2025). Babesiosis and Malaria in the United States: Epidemiology, Research Funding, Medical Progress, & Recommendations for Improvement. Epidemiologia, 6(4), 76. https://doi.org/10.3390/epidemiologia6040076






