The Impact of ACLS Training in the Management of Cardiac Arrest: A Narrative Review
Abstract
1. Introduction
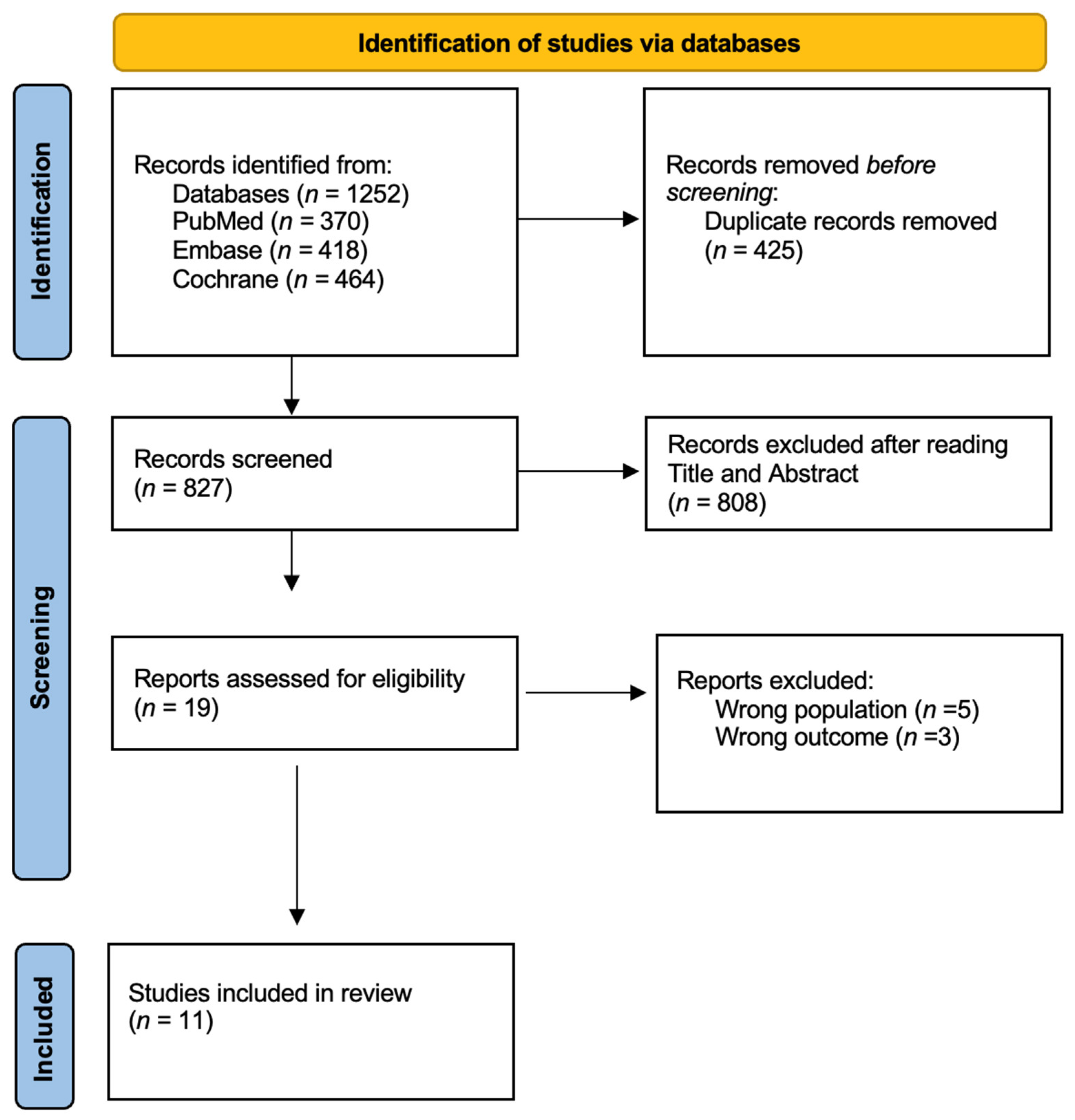
2. Materials and Methods
2.1. Research Concept
2.2. Inclusion and Exclusion Criteria
- Patients aged 18 years and older;
- Intrahospital setting (IHCA);
- Out-of-hospital setting (OHCA);
- Cardiac arrest.
- Age younger than 18 years;
- Trauma patients.
2.3. Research Strategy
3. Results
Main Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
| PUBMED | ((heart arrest [Title/Abstract]) OR (cardiac arrest[Title/Abstract]) OR (heart arrest[MeSH Terms]) OR (cardiopulmonary resuscitation[MeSH Terms]) OR (cardiopulmonary resuscitation[Title/Abstract]) OR (blue code[title/abstract])) AND ((ALS [title/abstract]) OR (Advance life support [title/abstract]) OR (ACLS [Title/Abstract]) OR (Advanced Cardiac Life Support[MeSH Terms]) OR (Advanced Cardiac Life Support[Title/Abstract])) AND ((mortality[Title/Abstract]) OR (mortality[MeSH Terms])) |
| EMBASE |
(‘heart arrest’: ti,ab OR ‘cardiac arrest’: ti,ab OR ‘heart arrest’/exp
OR ‘cardiopulmonary resuscitation’/exp OR ‘cardiopulmonary resuscitation’: ti,ab OR ‘blue code’: ti,ab) AND (‘als’: ti,ab OR ‘advance life support’: ti,ab OR ‘acls’: ti,ab OR ‘advanced cardiac life support’/exp OR ‘advanced cardiac life support’: ti,ab) AND (‘mortality’: ti,ab OR ‘mortality’/exp) |
| COCHRANE |
1-MeSH descriptor: [Heart Arrest] explode all trees 2882
2-‘heart arrest’: ti,ab OR ‘cardiac arrest’: ti,ab OR ‘cardiopulmonary resuscitation’: ti,ab OR ‘blue code’: ti,ab 6450 3-‘ALS’: ti,ab OR ‘Advance life support’: ti,ab OR ‘ACLS’: ti,ab OR ‘Advanced Cardiac Life Support’: ti,ab OR ‘ACLS’: ti,ab 3550 4-MeSH descriptor: [Mortality] explode all trees 21876 5-‘mortality’: ti,ab OR ‘death’: ti,ab OR ‘rosc’: ti,ab 135505 (#1 OR #2) AND (#3) AND (#4 OR #5) 143 |
References
- Lim, Z.J.; Ponnapa Reddy, M.; Afroz, A.; Billah, B.; Shekar, K.; Subramaniam, A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: A systematic review and meta-analysis. Resuscitation 2020, 157, 248–258. [Google Scholar] [CrossRef]
- Şener, A.; Pekdemir, M.; İslam, M.M.; Aksay, E.; Karahan, S.; Aksel, G.; Doğan, N.Ö.; Öztürk, B.; Hacımustafaoğlu, M.; Türkücü, Ç.; et al. Prospective, multicenter, Turkish out-of-hospital cardiac arrest study: TROHCA. Turk. J. Emerg. Med. 2024, 24, 133–144. [Google Scholar] [CrossRef]
- Lim, G.H.; Seow, E. Resuscitation for patients with out-of-hospital cardiac arrest: Singapore. Prehosp. Disaster Med. 2002, 17, 96–101. [Google Scholar] [CrossRef]
- Mayr, N.P.; Mayr, T.; Tassani, P.; Martin, K. Use of automated external defibrillators in the occupational setting in Germany: A pilot study. J. Occup. Environ. Med. 2012, 54, 789–791. [Google Scholar] [CrossRef] [PubMed]
- Villa, G.F.; Kette, F.; Balzarini, F.; Riccò, M.; Manera, M.; Solaro, N.; Pagliosa, A.; Zoli, A.; Migliori, M.; Sechi, G.M.; et al. Out-of-hospital cardiac arrest (OHCA) Survey in Lombardy: Data analysis through prospective short time period assessment. Acta Biomed. 2019, 90, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [PubMed]
- Savonitto, S.; De Luca, G.; Goldstein, P.; van T’ Hof, A.; Zeymer, U.; Morici, N.; Thiele, H.; Montalescot, G.; Bolognese, L. Antithrombotic therapy before, during and after emergency angioplasty for ST elevation myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 2017, 6, 173–190. [Google Scholar] [CrossRef]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef]
- Soar, J.; Böttiger, B.W.; Carli, P.; Couper, K.; Deakin, C.D.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation 2021, 161, 115–151. [Google Scholar] [CrossRef]
- Elliott, J.M.; Wang, T.K.M.; Gamble, G.D.; Williams, M.J.; Matsis, P.; Troughton, R.; Hamer, A.; Devlin, G.; Mann, S.; Richards, M.; et al. A decade of improvement in the management of New Zealand ST-elevation myocardial infarction (STEMI) patients: Results from the New Zealand Acute Coronary Syndrome (ACS) Audit Group national audits of 2002, 2007 and 2012. N. Z. Med. J. 2017, 130, 17–28. [Google Scholar]
- Descatha, A.; Dagrenat, C.; Cassan, P.; Jost, D.; Loeb, T.; Baer, M. Cardiac arrest in the workplace and its outcome: A systematic review and meta-analysis. Resuscitation 2015, 96, 30–36. [Google Scholar] [CrossRef]
- de Visser, M.; Bosch, J.; Bootsma, M.; Cannegieter, S.; van Dijk, A.; Heringhaus, C.; de Nooij, J.; Terpstra, N.; Peschanski, N.; Burggraaf, K. An observational study on survival rates of patients with out-of-hospital cardiac arrest in the Netherlands after improving the “chain of survival”. BMJ Open 2019, 9, e029254. [Google Scholar] [PubMed]
- Żuratyński, P.; Ślęzak, D.; Dąbrowski, S.; Krzyżanowski, K.; Mędrzycka-Dąbrowska, W.; Rutkowski, P. Use of Public Automated External Defibrillators in Out-of-Hospital Cardiac Arrest in Poland. Medicina 2021, 57, 298. [Google Scholar] [CrossRef] [PubMed]
- Gianni, A.; Botteri, M.; Stirparo, G.; Mattesi, G.; Zorzi, A.; Villa, G.F. The impact of the Italian law mandating an automatic external defibrillator in all sports venues on sudden cardiac arrest resuscitation rates. Eur. J. Prev. Cardiol. 2024, 31, e16–e18. [Google Scholar] [CrossRef] [PubMed]
- Panchal, A.R.; Berg, K.M.; Hirsch, K.G.; Kudenchuk, P.J.; Del Rios, M.; Cabañas, J.G.; Link, M.S.; Kurz, M.C.; Chan, P.S.; Morley, P.T.; et al. 2019 American Heart Association Focused Update on Advanced Cardiovascular Life Support: Use of Advanced Airways, Vasopressors, and Extracorporeal Cardiopulmonary Resuscitation During Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2019, 140, e881–e894. [Google Scholar] [CrossRef]
- Wyckoff, M.H.; Singletary, E.M.; Soar, J.; Olasveengen, T.M.; Greif, R.; Liley, H.G.; Zideman, D.; Bhanji, F.; Andersen, L.W.; Avis, S.R.; et al. 2021 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Neonatal Life Support; Education, Implementation, and Teams; First Aid Task Forces; and the COVID-19 Working Group. Resuscitation 2021, 169, 229–311. [Google Scholar] [CrossRef]
- Asken, M.J.; Shrimanker, I.; Bhattarai, S.; Hortian, V.; Slaven, V.; Nookala, V. Interns’ anticipatory anxiety about cardiopulmonary resuscitation: Reducing it while bolstering confidence with psychological skills training. Intern. Emerg. Med. 2021, 16, 2009–2011. [Google Scholar] [CrossRef]
- Semeraro, F.; Scapigliati, A.; Tammaro, G.; Olcese, U.; Cerchiari, E.L.; Ristagno, G. Advanced life support provider course in Italy: A 5-year nationwide study to identify the determinants of course success. Resuscitation 2015, 96, 246–251. [Google Scholar] [CrossRef]
- Nambiar, M.; Nedungalaparambil, N.M.; Aslesh, O.P. Is current training in basic and advanced cardiac life support (BLS & ACLS) effective? A study of BLS & ACLS knowledge amongst healthcare professionals of North-Kerala. World J. Emerg. Med. 2016, 7, 263–269. [Google Scholar] [CrossRef]
- Stirparo, G.; Di Fronzo, P.; Solla, D.; Bottignole, D.; Gambolò, L. Are Italian Newly Licensed Nurses Ready? A Study on Self-Perceived Clinical Autonomy in Critical Care Scenarios. Healthcare 2024, 12, 809. [Google Scholar] [CrossRef]
- Stirparo, G.; Gambolò, L.; Bottignole, D.; Solla, D.; Trapani, M.; Ristagno, G.; Pregliasco, F.; Signorelli, C. Enhancing Physicians’ Autonomy through Practical Trainings. Ann. Ig. 2024, 36, 652–659. [Google Scholar] [CrossRef]
- Bellini, L.; Fagoni, N.; Andreassi, A.; Sechi, G.M.; Bonora, R.; Stirparo, G. Effectiveness of Cardiopulmonary Resuscitation at the Workplace. Med. Lav. Work Environ. Health 2023, 114, e2023010. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Kurz, M.C.; Schmicker, R.H.; Leroux, B.; Nichol, G.; Aufderheide, T.P.; Cheskes, S.; Grunau, B.; Jasti, J.; Kudenchuk, P.; Vilke, G.M.; et al. Advanced vs. Basic Life Support in the Treatment of Out-of-Hospital Cardiopulmonary Arrest in the Resuscitation Outcomes Consortium. Resuscitation 2018, 128, 132–137. [Google Scholar] [CrossRef]
- Grunau, B.; Kawano, T.; Scheuermeyer, F.; Tallon, J.; Reynolds, J.; Besserer, F.; Barbic, D.; Brooks, S.; Christenson, J. Early advanced life support attendance is associated with improved survival and neurologic outcomes after non-traumatic out-of-hospital cardiac arrest in a tiered prehospital response system. Resuscitation 2019, 135, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Kette, F.; Pellis, T.; Pordenone Cardiac Arrest Cooperative Study Group (PACS). Increased survival despite a reduction in out-of-hospital ventricular fibrillation in north-east Italy. Resuscitation 2007, 72, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Honarmand, K.; Mepham, C.; Ainsworth, C.; Khalid, Z. Adherence to advanced cardiovascular life support (ACLS) guidelines during in-hospital cardiac arrest is associated with improved outcomes. Resuscitation 2018, 129, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Moretti, M.A.; Cesar, L.A.M.; Nusbacher, A.; Kern, K.B.; Timerman, S.; Ramires, J.A.F. Advanced cardiac life support training improves long-term survival from in-hospital cardiac arrest. Resuscitation 2007, 72, 458–465. [Google Scholar] [CrossRef]
- McEvoy, M.D.; Field, L.C.; Moore, H.E.; Smalley, J.C.; Nietert, P.J.; Scarbrough, S.H. The effect of adherence to ACLS protocols on survival of event in the setting of in-hospital cardiac arrest. Resuscitation 2014, 85, 82–87. [Google Scholar] [CrossRef]
- Kourek, C.; Greif, R.; Georgiopoulos, G.; Castrén, M.; Böttiger, B.; Mongardon, N.; Hinkelbein, J.; Carmona-Jiménez, F.; Scapigliati, A.; Marchel, M.; et al. Healthcare professionals’ knowledge on cardiopulmonary resuscitation correlated with return of spontaneous circulation rates after in-hospital cardiac arrests: A multicentric study between university hospitals in 12 European countries. Eur. J. Cardiovasc. Nurs. 2020, 19, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Camp, B.N.; Parish, D.C.; Andrews, R.H. Effect of advanced cardiac life support training on resuscitation efforts and survival in a rural hospital. Ann. Emerg. Med. 1997, 29, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, M.L.; Robinson, N.E.; Kuska, B.M.; Stone, H.L.; Fryback, D.G.; Rose, J.H. Effect of advanced cardiac life-support training in rural, community hospitals. Crit. Care Med. 1994, 22, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Pareek, M.; Parmar, V.; Badheka, J.; Lodh, N. Study of the impact of training of registered nurses in cardiopulmonary resuscitation in a tertiary care centre on patient mortality. Indian J. Anaesth. 2018, 62, 381–384. [Google Scholar] [CrossRef]
- Larribau, R.; Deham, H.; Niquille, M.; Sarasin, F.P. Improvement of out-of-hospital cardiac arrest survival rate after implementation of the 2010 resuscitation guidelines. PLoS ONE 2018, 13, e0204169. [Google Scholar] [CrossRef]
- Stirparo, G.; Bellini, L.; Ristagno, G.; Bonora, R.; Pagliosa, A.; Migliari, M.; Andreassi, A.; Signorelli, C.; Sechi, G.M.; Fagoni, N. The Impact of COVID-19 on Lombardy Region ST-Elevation Myocardial Infarction Emergency Medical System Network-A Three-Year Study. J. Clin. Med. 2022, 11, 5718. [Google Scholar] [CrossRef]
- Stirparo, G.; Fagoni, N.; Bellini, L.; Oradini-Alacreu, A.; Migliari, M.; Villa, G.F.; Botteri, M.; Signorelli, C.; Sechi, G.M.; Zoli, A. Cardiopulmonary resuscitation missed by bystanders: Collateral damage of coronavirus disease 2019. Acta Anaesthesiol. Scand. 2022, 66, 1124–1129. [Google Scholar] [CrossRef]
- Sarboozi-Hosseinabadi, S.; Sharifzadeh, G.; Hosseini, S.M. Evaluating CPR training: Simulation vs. webinars for Iranian emergency medical technicians during COVID-19. BMC Emerg. Med. 2024, 24, 46. [Google Scholar] [CrossRef]
| First Author, Year, Country | Journal | Type of the Study | Setting | Sample | Outcomes | Main Results |
|---|---|---|---|---|---|---|
| Kourek, 2020, European Union [32] | European Journal of Cardiovascular Nursing | Observational, cross-sectional multicenter study | IHCA | -- | Correlation between ACLS guidelines knowledge and ROSC rates in the selected hospitals | Correlation between cardiopulmonary resuscitation knowledge and ROSC rates of patients with IHCA demonstrated that each additional correct answer on the advanced life support score results in a further increase in return of spontaneous circulation rates. |
| Kurz, 2018, USA [26] | Resuscitation | Retrospective study | OHCA | 35,065 patients | Survival to hospital discharge; prehospital ROSC; 24-h survival, and favorable neurological survival defined as a modified Rankin score ≤ 3 At hospital discharge | ALS care with or without initial BLS care was independently associated with increased adjusted ROSC and survival to hospital discharge unless delivered greater than 6 min after BLS arrival (BLS + late ALS). |
| Grunau, 2019, Canada [27] | Resuscitation | Secondary analysis of consecutive adult OHCAs | OHCA | 12,722 patients | Survival and favorable neurological outcomes (modified Rankin scale ≤ 3) at hospital discharge | ALS response interval (per minute) was associated with decreased survival and a favorable neurological outcome. ALS response ≤ 10 min was associated with improved survival and favorable neurological outcomes. Earlier ALS arrival was associated with improved survival and favorable neurological outcomes. |
| Larribau, 2018, Switzerland [36] | PloS One | Retrospective observational study | OHCA | 795 patients | Survival to hospital discharge; ROSC | The prognosis of patient survival at the time of hospital discharge rose from 10.33% in 2009–2010 to 17.01% in 2011–2012 (p = 0.007). Survival rate for OHCA patients improved significantly in 2011–2012. These data suggest that it was probably the improvement in the quality of care provided during CPR and post-cardiac arrest care that contributed to the increase in survival rates at the time of hospital discharge. |
| Honarmand, 2018, Canada [29] | Resuscitation | Retrospective study | IHCA | 160 patients | ROSC and survival to hospital discharge | There were fewer deviations during events that led to survival to hospital discharge compared to those where the patient did not survive to hospital discharge. A higher number of deviations from ACLS guidelines during resuscitation events was associated with a lower likelihood of not only ROSC, but also survival to hospital discharge. |
| Pareek, 2018, India [35] | Indian Journal of Anaesthesia | Retrospective study | IHCA | 632 patients | ROSC and survival to discharge | During the pre-BLS/ACLS training period of the 294 Cardiac arrest patients, 58 patients (19.7%), had ROSC, while during the post-BLS/ACLS training period, 102 patients (30.1%) of the 338 patients who had cardiac arrest had ROSC (p = 0.003). |
| McEvoy, USA, 2013 [31] | Resuscitation | Retrospective study | IHCA | 149 patients | ROSC | The percentage of correct steps performed was positively correlated with ROSC from an IHCA (p < 0.01), and the number of errors of commission and omission were both negatively correlated with ROSC from an IHCA (p < 0.01). |
| Kette, 2007, Italy [28] | Resuscitation | Prospective, multicenter study | OHCA | 194 patients | Survival to hospital discharge | Compared results of two studies of the same research group (1994–2003), the rate of VF or pulseless VT as presenting rhythm reduced with a rate of return of spontaneous circulation of 69.2% and survival to hospital discharge of 41%. Hospital discharge for asystole or pulseless electrical activity remained drab (3.1% and 1.7%). |
| Moretti, 2007, Brazil [30] | Resuscitation | Multicenter, prospective cohort study | IHCA | 156 patients | ROSC; survival to hospital discharge, survival to 30 days, and survival to 1 year | The presence of an ACLS-trained team member at an in-hospital resuscitation event increases ROSC, short-term, and long-term survival following cardiac arrest. |
| Camp, 1997, USA [33] | Annals of Emergency Medicine | Retrospective study | IHCA | 236 patients | Survival to hospital discharge | There was a three-period study. Before, during, and after the organization of an ACLS teaching program. There were 893 total death events in the early period and 485 in the final period. After widespread ACLS training, there was a decrease in death events. |
| Birnbaum, 1994, USA [34] | Critical care medicine | Case–controlled, retrospective study | IHCA | 869 patients | Nurses and physicians’ behaviors; mortality rate | Rates of successful attainment of the terminal behavior objectives by physicians and nurses were 84.0% and 78.8%, respectively. The mortality rates decreased from 17.4% in the period before the training to 13.1% after the ACLS course. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Fronzo, P.; Gaetti, G.; Marcassa, D.; Gervasi, V.; Dardour, O.; Pedretti, A.; Gambolò, L. The Impact of ACLS Training in the Management of Cardiac Arrest: A Narrative Review. Epidemiologia 2025, 6, 61. https://doi.org/10.3390/epidemiologia6040061
Di Fronzo P, Gaetti G, Marcassa D, Gervasi V, Dardour O, Pedretti A, Gambolò L. The Impact of ACLS Training in the Management of Cardiac Arrest: A Narrative Review. Epidemiologia. 2025; 6(4):61. https://doi.org/10.3390/epidemiologia6040061
Chicago/Turabian StyleDi Fronzo, Pasquale, Giovanni Gaetti, Daniel Marcassa, Valeria Gervasi, Oumaiema Dardour, Andrea Pedretti, and Luca Gambolò. 2025. "The Impact of ACLS Training in the Management of Cardiac Arrest: A Narrative Review" Epidemiologia 6, no. 4: 61. https://doi.org/10.3390/epidemiologia6040061
APA StyleDi Fronzo, P., Gaetti, G., Marcassa, D., Gervasi, V., Dardour, O., Pedretti, A., & Gambolò, L. (2025). The Impact of ACLS Training in the Management of Cardiac Arrest: A Narrative Review. Epidemiologia, 6(4), 61. https://doi.org/10.3390/epidemiologia6040061






