Abstract
Cannabis is a widely used substance among the youth population, with an estimated 2.8% currently smoking cannabis. Its popularity is growing due to the perception of its harmless nature and lack of dependence. However, this increase in use has been linked to mental health issues, especially since its partial decriminalisation in some part of the United States and Australia. The objective of this scoping review was to investigate the mental health impact of cannabis use among young people in Australia and the United States. A scoping review was conducted according to the Joanna Briggs Institute (JBI) protocol, and articles were searched from ProQuest Central and EBSCO Host (MEDLINE and CINAHL databases). A total of 24 articles were analysed, including systematic reviews, meta-analyses, and cohort, longitudinal, and cross-sectional studies. The findings indicate that cannabis use is associated with depression, psychosis, suicide, cannabis use disorder, dependence, decline in cognitive function, and the development of externalising behaviour, particularly attention deficit hyperactivity disorder. However, the relationship between cannabis use and anxiety is equivocal. Mental health issues were more prevalent with increased frequency, duration, intensity, and type of use. Female, minority, LGBTQI, African American, Aboriginal, and Torres Strait Islander youth and the age of onset of cannabis use were significant factors for the development of mental health problems. The increasing prevalence of cannabis use among high school and college students suggests the need for intervention by teachers, parents, and community health professionals to make them aware of its potential negative mental health outcomes. Moreover, policy-level interventions by the government are required to discourage young people from using cannabis.
Keywords:
adolescent; cannabis use; substance abuse; mental health; marijuana; psychosis; depression; dependence; scoping review 1. Introduction
Cannabis is a substance that has been used for centuries and is estimated to be currently used by around 2.8% of the young population worldwide, making it increasingly popular among youth [1,2]. In the United States, cannabis is the second-most used substance after alcohol, with an estimated 7.1% of youth using it [3]. In addition, cannabis is the most used substance among Australian youth, with around 34.8% of Australians aged 14 years and above using it at least once in their lifetime [4]. Among young Australian males of the Aboriginal and Torres Strait Islander population, this percentage increases to about 70%, and among females, it is 20% [5]. These numbers appear to be increasing, especially after the legalisation of cannabis for recreational use since 2012 [6,7]. The most common reasons for cannabis use among these groups are a decreased perception of harm, dependence, or addiction [8].
While cannabis has medicinal value for various conditions, including epilepsy, multiple sclerosis, Parkinson’s disease, arthritis, and anxiety, anecdotal evidence should not overshadow assessments of its immediate or long-term harm, especially concerning age of onset and chronic exposure [9,10]. The youth population, especially the adolescent group, is more prone to using cannabis because they go through several physical as well as psychological changes, which increase their vulnerability to environmental influences, involvement in risk-taking behaviour, peer pressure, family relations, and conflicting and variable views of cannabis use by medical, political, social, and ethical standpoints on cannabis-related issues [5,11,12]. In addition, self-control behaviour by adolescents against cannabis use is also an important predictor of the development of cannabis use disorders or other mental health issues [13]. It has been found that young people are equally susceptible to cannabis use, with both males and females being equally susceptible, but males are more prone to its chronic use, whereas females are more susceptible to developing mental health problems [14]. Among numerous strains of cannabis, Cannabis sativa is the most popular and widely used, derived from leaves or female flower buds. The common mode of delivery of herbal cannabis is usually through inhalation of smoke [5] and, in recent days, cannabis use with vaping has increased substantially [15]. The psychoactive compound, i.e., 9 delta tetrahydrocannabinol (THC) present in cannabis, is responsible for most of its effects, which are mediated through the CB1 receptor present in the brain and are responsible for the development of various mental health conditions such as psychosis, depression, cannabis use disorders, dependence, anxiety, mood disorders, and other mental health problems [5]. Another active component found in cannabis is cannabichromene (CBC), which interacts with the endocannabinoid system in ways that suggest potential anti-inflammatory, pain-relieving, and neuroprotective effects, but its impact on mental health is not yet clearly understood [16].
The selection of Australia and the US for this study reflects the similarities in the intricate and dynamic nature of cannabis legalisation in these regions. With certain states having already legalised cannabis for both recreational and medicinal use, and others still in the process of considering it, these two countries present a unique context for examining the effects of cannabis on the mental health of young individuals [17,18,19]. However, there is limited research conducted specific to young people in Australia and United States that explores the impact on mental health, which have a similar landscape in terms of variation of legalisation in state and federal level. Despite the growing concerns surrounding the mental health implications of cannabis use among young people, there is a noticeable lack of reviews that comprehensively assess this issue. To address this knowledge gap, we conducted a scoping review aimed at examining and synthesising the existing evidence on the mental health impact of cannabis use among young populations in Australia and the United States.
2. Materials and Methods
This scoping review was conducted according to the protocol that was prepared based on to the Joanna Briggs Institute (JBI) protocol for scoping reviews [20]. This protocol included specific steps for identifying and selecting relevant studies, extracting data, and analysing and reporting the results to answer the research question.
2.1. Research Question
What is the nature and extent of the mental health impact of cannabis use among young people in Australia and the United States?
2.2. Eligibility
Using modified versions of the Population, Interventions, Comparators and Outcomes (PICO) framework, we formulated the research question and selected the eligibility criteria for the study. Peer-reviewed journal articles published in the English language and conducted on human subjects were screened as per eligibility criteria, which are summarised in Table 1.

Table 1.
Inclusion criteria adopted in the scoping review.
2.3. Search Strategy, Information Source, and Study Selection
The search strategy employed in this scoping review involved the databases ProQuest Central, CINAHL (via EBSCOhost), and MEDLINE (via EBSCOhost). The initial search was conducted using words found in the title and abstract of retrieved papers, as well as index terms used to describe the articles. Following this, a second search was conducted using the identified keywords and index terms across all databases, incorporating limiters such as article publication dates between 1 January 2012 and 1 November 2022, age range between 12 and 45 years, peer-reviewed studies conducted in English language, studies with human subjects, and studies from the United States and Australia.
Keywords employed in the search strategy included the following:
- Mental health: Anxiety OR depression OR bipolar mood disorder OR psychosis OR schizophrenia OR attention deficit hyperactive disorder OR ADHD OR PTSD OR Anti-sociality disorder OR conduct Disorder OR Panic attack OR Mental disorder OR Mental*;
- Cannabis: Marijuana OR Tetra hydro cannabidiol OR THC OR pot OR bong OR joint OR cannabis;
- Young population: Adolescence OR adolescent OR young adult OR youth OR young.
All the identified studies were uploaded to Mendeley Version 2.8 (Elsevier, Amsterdam, The Netherlands), a reference management tool, which was used to remove duplicates, and to screen and select studies for the data extraction process, as per PRISMA Extension for Scoping Reviews [21]. Two reviewers (A.B. and K.R.) independently assessed the titles and abstracts of the articles and determined their eligibility based on the criteria provided in Table 1. The studies that met the criteria were retrieved in full text and screened. Any disagreement was resolved through consensus or discussion with a third reviewer (R.C.).
2.4. Data Extraction
Data extraction was carried out following the Preferred Reporting Items for Systematic Review and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) Checklist [21]. All the data were collected electronically and was extracted in a pre-developed form using Microsoft Word version 16.7 software. The form was calibrated and pilot-tested by two reviewers (A.B. and K.R.), and all the items collected were verified by a third reviewer (R.C.). Disagreements were resolved by consensus and consultation with all reviewers. The extracted data included the author’s name, year of publication, study design, information about participants, study objective, and study outcomes.
2.5. Thematic Analysis and Charting
After completing the data extraction process following the PRISMA-ScR checklist, we conducted thematic analysis and charting to analyse and summarise the findings [21]. Thematic analysis involves identifying, analysing, and reporting the themes found in the data, while charting involves summarising the key findings of each article and organising them to facilitate comparison and synthesis of results. Through this process, we were able to identify the key themes and patterns in the data and synthesise the findings from the different studies [22]. This helped provide a broader understanding of the mental health impact of cannabis use among young people in Australia and the United States.
3. Results
The initial search retrieved a total of 692 articles from the electronic database search, as illustrated in Figure 1. Of these, 243 were from ProQuest Central, while 449 were obtained from EBSCOhost using 2 databases, which included CINAHL and MEDLINE, covering the period from 1 January 2012 to 1 November 2022. After removing 90 duplicates, 50 full-text studies were assessed, and 26 studies were subsequently excluded based on the eligibility criteria.
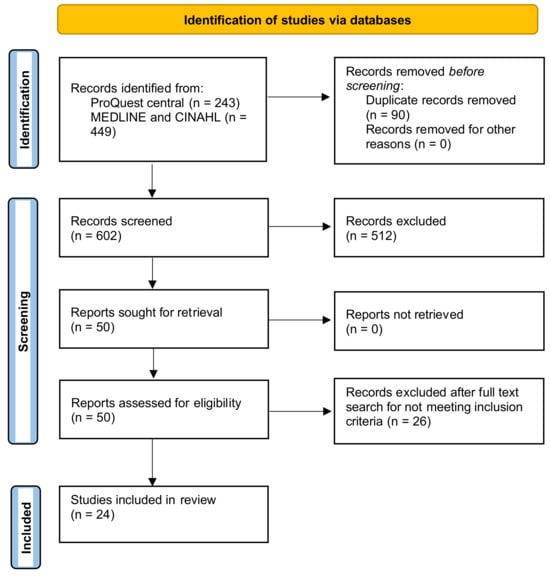
Figure 1.
PRISMA flow diagram illustrating identification of studies.
Out of the 24 articles included for data charting and thematic analysis, 3 were from Australia and 21 were from the United States, as shown in Table 2. Among them, three were systematic reviews and meta-analyses, seven were cohort studies, seven were longitudinal studies, and seven were cross-sectional studies.

Table 2.
Summary of the included studies.
3.1. Cannabis Use among Young Population and Depression and Depressive Symptoms
The relationship between cannabis use among young people and the development of depression and depressive symptoms was explored in 15 selected studies. A 2019 systematic review and meta-analysis conducted by Knopf et al. in the United States found 11 relevant articles, constituting individuals aged between 12 and 32 years, and concluded that teen cannabis users had 1.37 times higher risk of developing depression than non-users [25]. A similar trend was synthesised by another systematic review [41]. A cohort study conducted in Australia, consisting of participants from adolescence to young adulthood, found that weekly cannabis users were more prone to developing depression by 0.24 (95% CI: 0.18–0.30) compared to non-users and the strength of association was strongest among adolescents [27].
Moreover, cross-sectional research conducted in Baltimore, United States that included female participants of African American and white ethnicity aged between 18 and 30 years found that African American females were more likely to develop depression, with an odds ratio of 2.1 (95% CI: 1.08–3.93), and the relationship between cannabis use and depression did not differ by developmental stages [28]. A longitudinal study conducted in Australia among adolescents from age 15 to 19 years found that the rate of cannabis use increased from 7.5% at age 15 to 29.8% at age 19, which was four times more, and showed a 20% increase in depression between these ages [29]. A similar trend in the increase of cannabis use from adolescence to adulthood was found in the United States in one longitudinal research study conducted among 9816 individuals aged between 18 and 32 years [30]. However, there was an inverse relationship between the prevalence of depressive symptoms and the age of cannabis use, i.e., more among adolescents and less in emerging adulthood [29,30].
The frequency of cannabis use and the development of depression was directly related and twice as high among youth and did not significantly differ by age, as found in one cohort study conducted among 55,271 adolescents and young adults in the United States [31]. Depression was more common among regular non-blunt cannabis users as compared to blunt users in a cross-sectional study comprising participants from age 12 to 45 years [32]. However, one cohort study consisting of high school students and one longitudinal study consisting of young people in the United States found association with the development of depression in early adulthood, especially from 18–26 years [35,36]. This finding was consistent with another cross-sectional research conducted in 300 university students aged 18 to 25 years in Colorado, United States [38].
A longitudinal research study conducted in the United States from participants aged 12–32 years attempted to find the causal relationship between depression and cannabis use and found that it was bidirectional and more common among sexual minority groups such as LGBTQI groups [37]. This finding was supported by another cross-sectional study conducted in the United States consisting of 204,102 individuals aged 12–17 years [14].
3.2. Cannabis Use among Young Population and Anxiety
The relationship between cannabis use and anxiety in young people was explored in eight articles in this review. However, the results seem equivocal. For example, longitudinal research conducted among Australian secondary school students transitioning to young adulthood found that those who used cannabis were 20–30% more likely to have anxiety [29]. Another cohort study conducted in the United States with a sample of 55,271 individuals aged 12–32 years found that young people who used cannabis were twice as likely to develop anxiety, with the likelihood increasing with the intensity of use [31]. This finding is consistent with a longitudinal study conducted in the United States among individuals aged 18–45 years, with the highest prevalence observed in those aged 18–22 years [31,35]. Furthermore, a longitudinal study conducted in the United States with participants aged 12–32 years found that the relationship between cannabis use in adolescence and the development of anxiety in late adolescence/early adulthood is unidirectional and is more common among sexual minority groups such as LGBTQI individuals [37]. The relationship with cumulative cannabis use, regardless of status, was significant among young people aged 15–26 years in the United States [43].
However, a 2019 systematic review and meta-analysis that included 11 relevant articles found no statistically significant relationship between cannabis use among young people and the development of anxiety in the United States [41]. This finding was supported by a cross-sectional study conducted among university students aged 18–25 years in Colorado, United States [38]. Additionally, one longitudinal study consisting of 506 adolescent boys from Pittsburgh, United States, did not find a statistically significant outcome for depression among participants in their mid-30s across different subgroups of cannabis users, including early onset chronic users, late increasing users, adolescence-limited users, and low/non-users [33].
3.3. Cannabis Use among Young Population and Risk of Suicide, Suicidal Ideation, Plan, and Attempt
A study among high school students in the United States found that adolescents reporting a history of cannabis use were 2 to 5 times more likely to have had suicidal ideation, suicidal thought, and a suicidal plan in the last year [26]. This finding was also supported by a cohort study with a nationally representative sample in the United States [36]. A US cohort study on participants aged 18–34 found that past-year cannabis use disorder, daily cannabis use, and non-daily cannabis use were linked to higher rates of suicidal ideation, plan, and attempt [42]. The increase in prevalence was more significant among individuals with or without cannabis use disorder, with a higher prevalence observed among women (13.9% vs. 3.5%) than men (9.9% vs. 3.0%) [42]. Similarly, a systematic review and meta-analysis in 2019 found that teen cannabis users had a 1.5 times increased risk of developing suicidal ideation and were 3.46 times more likely to attempt suicide than non-users [41]. However, a longitudinal study consisting of adolescent boys from Pittsburgh, United States did not find a statistically significant outcome for suicide, suicidal plan, attempt, and ideation among participants in their mid-30s between different subgroups of cannabis users, i.e., from early onset chronic users, late increasing users, adolescence-limited users, and low/nonusers [33].
3.4. Cannabis Use among Young Population and Risk of Psychosis and Psychotic Symptoms
A longitudinal study conducted in the United States with 36,309 participants between the ages of 18 and 45 years found that the frequency of cannabis use and cannabis use disorder is directly proportional to the development of psychosis, with more prevalence between the ages of 18 and 23 and higher risk among females than males [35]. Additionally, a cohort study conducted in Boston, United States participants between the ages of 14 and 18 years found that cannabis use and the association of psychotic symptoms such as hallucination and paranoia are more common among youth with positive monthly or more frequent use of cannabis or cannabis use disorder as compared to use once or twice in the past year. However, cannabis use was also positively associated with psychotic symptoms, even with a single use [39].
3.5. Cannabis Use among Young Population and Risk of Cannabis Use Disorder and Dependence
A cohort study conducted in the United States with 55,271 participants aged between 12 and 45 years found that cannabis use disorder was directly proportional to the intensity of use. The disorder was more prevalent in heavy users (22.35%) compared to moderate (15.54%) and light users (10.10%). Additionally, recent users were more likely to report cannabis use disorder compared to non-users, with prevalence rates of 15.32% for the past 30 days, 11.62% for the past year, and 3.49% for lifetime use [31]. Similarly, a cohort study in the United States consisting of 281,650 individuals aged between 18 and 34 years found that individuals with past-year cannabis use disorder were associated with a higher prevalence of suicidal ideation, plan, and attempt [42]. Furthermore, another cohort study conducted in the United States found significant cannabis use disorder among participants, with 40% meeting the DSM IV criteria for cannabis dependence and 32% meeting the criteria for cannabis abuse. Additionally, adolescents with cannabis use disorder were more likely to develop alcohol and opioid abuse [8]. In addition to this, a cross-sectional research study conducted in the United States among participants aged between 12 and 45 years to determine the prevalence of cannabis use disorder and dependence among participants taking cannabis in different forms found that cannabis use disorder, abuse, and dependence increased most in blunt use, followed by dual cigar and blunt use, then non-blunt marijuana use [32]. A cross-sectional study conducted in the United States among 182,722 participants aged between 18 and 22 years found that there was an annual increase in marijuana use from 2002 to 2018 among college and non-college individuals by 0.46% vs. 0.37%, respectively. However, there was no statistically significant result for the development of cannabis use disorder [24].
3.6. Cannabis Use and Development of Other Mental Disorder
A meta-analysis with more than 650 study subjects and 5600 controls found that cannabis use was associated with the development of cognitive decline, as measured by a decrease in IQ by 2 points compared to non-users in the United States [40]. Another cohort study conducted in Boston, United States with participants between the ages of 12–24 years found that cannabis use was associated with an increased risk of developing externalising behaviours, especially attention deficit hyperactivity disorder, compared to non-users [34].
4. Discussion
This scoping review systematically synthesised evidence on the knowledge gaps in understanding the relationship between cannabis use among young individuals and its impact on mental health. Analysing 24 articles primarily from the United States and Australia, it revealed a consistent association between cannabis use and various adverse mental health outcomes, including depression, anxiety, suicide, psychosis, cannabis use disorder, dependence, lower cognitive function, and externalising behaviour. A consistent association between cannabis use and depression was synthesised from the included studies, and, additionally, we observed a higher prevalence of cannabis use among sexual minority groups, including LGBTQI youth, African American youth, and Aboriginal and Torres Strait Islander youth populations [5,13,28,37]. Such a trend can be explained through the mental health stigma and drug-related stigma in marginalised groups [44,45]. Nevertheless, cannabis use exhibited consistency between male and female youth, with males displaying a higher likelihood of chronic use, while females were more prone to developing adverse mental health outcomes [23,28,30,35]. Furthermore, non-blunt cannabis use was more consistently associated with the development of depression than blunt use, and adolescents and young adults aged between 18 and 26 years were found to be more susceptible to developing depression from cannabis use [32]. Previous global-scale studies have noted similar tendency as well [46]. The findings regarding the development of anxiety among young adults were ambivalent, as anxiety was directly related to intensity, past cumulative use, and age group. Additionally, it was more commonly observed among sexual minority groups [27,31,35,37,41]. Cannabis use was associated with the development of psychosis and psychotic symptoms, such as hallucinations and paranoia [35,39]. Cannabis use is associated with heightened risks of cannabis use disorder, suicide, substance problems, particularly among females and males, respectively, with conflicting findings possibly due to study limitations, while also correlating with decreased cognitive capacity and externalising behaviour [34,40].
The established relationship between cannabis use and a spectrum of mental health outcomes presents a discourse with significant implications for diverse stakeholders and particular relevance for medical practitioners, policymakers, and mental health professionals, including developmental psychologists [47,48,49]. Integrating this research into practice could offer valuable insights for medical practitioners, prompting us to consider cannabis use as a pertinent factor when addressing mental health issues in young people [50,51]. Furthermore, the age groups, gender differences, and vulnerable populations underscore the need for tailored interventions and preventive strategies demanded by the changing demographics of the population [52,53,54,55,56]. However, the critical discussion should acknowledge potential limitations within the research, such as variations in study methodologies and the influence of biases and confounders. This underscores the necessity for continued investigation and the application of an evidence-based approach in both clinical and policy settings to address the complex interplay between cannabis use and mental health outcomes [57].
The findings underscore the need for future research to focus on longitudinal studies examining the temporal relationship between cannabis use and mental health outcomes. This includes factors such as age of onset, frequency, and duration of use, as well as the impact of different strains, modes of delivery, and dosages on mental health [53,54,55,56]. Building on this research, policies should be evidence-based, balancing potential benefits with risks, with stricter regulations on availability and targeted interventions for vulnerable groups [56,57,58]. Prevention efforts should include comprehensive school-based programs to educate students about the risks of cannabis use and promote healthy coping strategies [59]. Healthcare provider training is also crucial to ensure professionals can screen for cannabis use, provide early interventions, and offer support to at-risk individuals [60]. Educational programs should aim to dispel misconceptions and stigma, while providing accurate information and promoting healthy coping strategies [59,60].
Most of the studies were observational studies, which can be affected by unmeasurable confounders. Therefore, future research needs to be more robust, such as systematic reviews and meta-analyses, translational qualitative studies, and controlled trials, to understand the causal relationship between cannabis use and the development of mental illness among young populations by adjusting potential non-measurable confounders [61,62]. Furthermore, the increasing prevalence of cannabis use among high school and college students, due to its perceived harmless nature and lack of dependence, suggests the need for intervention by integrating teachers, parents, courses, and community health professionals to make them aware of its potential negative mental health outcomes [63,64]. Additionally, policy-level interventions to discourage cannabis use among young populations are necessary [65]. Overall, this review emphasises the importance of understanding the potential mental health consequences of cannabis use among young people and suggests the need for more robust research and intervention strategies to prevent these outcomes.
This scoping review was conducted through a search of three databases from 2012 to 2022. Nevertheless, it is important to acknowledge certain limitations inherent in this approach. The reliance on three specific databases might result in overlooking relevant articles available on alternative platforms and the gray literature, potentially leading to a fractional representation of the existing literature. Furthermore, given that a majority of the included articles were observational studies, the research is susceptible to recall bias, selection bias, and unmeasurable confounders, introducing potential threats to the study’s internal validity [58,66]. Additionally, confining the search to the United States and Australia may cause limitations about the generalisability of the findings to other global regions, which may exhibit distinct geographical, political, cultural, and societal variations impacting the relationship between cannabis use and mental health outcomes. Therefore, it is crucial to interpret the results within the context of these limitations and consider the need for further research in diverse settings to enhance the robustness and generalisability of the findings of this scoping review.
5. Conclusions
This scoping review was conducted to identify the mental health impact of cannabis use among the young populations of Australia and the United States. It was found that cannabis use has been associated with the development of depression, psychosis, cannabis use disorder (CUD), dependence, externalising behaviour, attention deficit hyperactivity disorder (ADHD), and a decline in cognitive function. However, there were equivocal results regarding the development of anxiety. Additionally, the development of these disorders was associated with the age of cannabis use, intensity, and type of use, and was more common among females and in vulnerable populations. Most of the studies reviewed were observational; hence, a causal relationship between cannabis use and mental health outcomes requires more robust forms of research.
Author Contributions
A.B. and F.H. conceptualised the research questions for the review. A.B. developed the search strategy and drafted the initial manuscript under the guidance of F.H. K.R. critically revised the initial and final versions of the manuscript and validated the search and the data under supervision of R.C. All authors have read and agreed to the published version of the manuscript.
Funding
This review received no external funding. In-kind support and open access fee support has been provided by the Philanthropy Nepal (Paropakari Nepal) Research Collaboration.
Acknowledgments
The project was initially started by A.B. as an MPH capstone project supervised by F.H. and would like to acknowledge the team at Torrens University, Australia for their support. We would also like to acknowledge all the members of Philanthropy Nepal (Paropakari Nepal) Research Collaboration for their support and assistance in completing the project.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bauman, A.; Phongsavan, P. Epidemiology of substance use in adolescence: Prevalence, trends and policy implications. Drug Alcohol Depend. 1999, 55, 187–207. [Google Scholar] [CrossRef] [PubMed]
- Mansell, H. Selective Studies on the Challenges of Cannabis Use in Children, Youth and Young Adults; University of Saskatchewan: Saskatoon, SK, Canada, 2022. [Google Scholar]
- Haberstick, B.C.; Young, S.E.; Zeiger, J.S.; Lessem, J.M.; Hewitt, J.K.; Hopfer, C.J. Prevalence and correlates of alcohol and cannabis use disorders in the United States: Results from the national longitudinal study of adolescent health. Drug Alcohol Depend. 2014, 136, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Livingston, M.; Holmes, J.; Oldham, M.; Vashishtha, R.; Pennay, A. Trends in the sequence of first alcohol, cannabis and cigarette use in Australia, 2001–2016. Drug Alcohol Depend. 2020, 207, 107821. [Google Scholar] [CrossRef]
- Iede, M.A.; Nunn, K.; Milne, B.; Fitzgerald, D.A. The consequences of chronic cannabis smoking in vulnerable adolescents. Paediatr. Respir. Rev. 2017, 24, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Hall, W.; Lynskey, M. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction 2016, 111, 1764–1773. [Google Scholar] [CrossRef] [PubMed]
- Rotermann, M. What has changed since cannabis was legalized? Health Rep. 2020, 31, 11–20. [Google Scholar]
- Zaman, T.; Malowney, M.; Knight, J.; Boyd, J.W. Co-Occurrence of Substance-Related and Other Mental Health Disorders Among Adolescent Cannabis Users. J. Addict. Med. 2015, 9, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Mandelbaum, D.E.; de la Monte, S.M. Adverse structural and functional effects of marijuana on the brain: Evidence reviewed. Pediatr. Neurol. 2017, 66, 12–20. [Google Scholar] [CrossRef]
- Grotenhermen, F.; Müller-Vahl, K. Medicinal uses of marijuana and cannabinoids. Crit. Rev. Plant Sci. 2016, 35, 378–405. [Google Scholar] [CrossRef]
- Sellers, C.M.; McRoy, R.G.; O’Brien, K.H.M. Substance use and suicidal ideation among child welfare involved adolescents: A longitudinal examination. Addict. Behav. 2019, 93, 39–45. [Google Scholar] [CrossRef]
- White, C.T.; Shamim, H.; Al Shouli, R.; Habbal, A.B.; Mohammed, L. Cannabis use and the development of depression in adolescents: Is there an established linear relationship between the two? Cureus 2022, 14, e27394. [Google Scholar] [CrossRef]
- Pahl, K.; Brook, J.S.; Lee, J.Y. Adolescent self-control predicts joint trajectories of marijuana use and depressive mood into young adulthood among urban African Americans and Puerto Ricans. J. Behav. Med. 2014, 37, 675–682. [Google Scholar] [CrossRef][Green Version]
- Weinberger, A.H.; Zhu, J.; Lee, J.; Anastasiou, E.; Copeland, J.; Goodwin, R.D. Cannabis use among youth in the United States, 2004–2016: Faster rate of increase among youth with depression. Drug Alcohol Depend. 2020, 209, 107894. [Google Scholar] [CrossRef]
- Knopf, A. MTF: Cannabis use with vaping goes up, cannabis smoking down. Brown Univ. Child. Adolesc. Psychopharmacol. Update 2022, 24, 5. [Google Scholar] [CrossRef]
- Khalsa, J.H.; Bunt, G.; Blum, K.; Maggirwar, S.B.; Galanter, M.; Potenza, M.N. Review: Cannabinoids as Medicinals. Curr. Addict. Rep. 2022, 9, 630–646. [Google Scholar] [CrossRef]
- Chiu, V.; Hall, W.; Chan, G.; Hides, L.; Leung, J. A Systematic Review of Trends in US Attitudes toward Cannabis Legalization. Subst. Use Misuse 2022, 57, 1052–1061. [Google Scholar] [CrossRef]
- Kaur, N.; Keyes, K.M.; Hamilton, A.D.; Chapman, C.; Livingston, M.; Slade, T.; Swift, W. Trends in cannabis use and attitudes toward legalization and use among Australians from 2001–2016: An age-period-cohort analysis. Addiction 2021, 116, 1152–1161. [Google Scholar] [CrossRef] [PubMed]
- Single, E.; Christie, P.; Ali, R. The Impact of Cannabis Decriminalisation in Australia and the United States. J. Public Health Policy 2000, 21, 157–186. [Google Scholar] [CrossRef] [PubMed]
- Khalil, H.; Peters, M.; Godfrey, C.M.; McInerney, P.; Soares, C.B.; Parker, D. An evidence-based approach to scoping reviews. Worldviews Evid.-Based Nurs. 2016, 13, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Dennhardt, S.; Apramian, T.; Lingard, L.; Torabi, N.; Arntfield, S. Rethinking research in the medical humanities: A scoping review and narrative synthesis of quantitative outcome studies. Med. Educ. 2016, 50, 285–299. [Google Scholar] [CrossRef]
- Moller, C.I.; Tait, R.J.; Byrne, D.G. Self-harm, substance use and psychological distress in the Australian general population. Addiction 2013, 108, 211–220. [Google Scholar] [CrossRef]
- McCabe, S.E.; Arterberry, B.J.; Dickinson, K.; Evans-Polce, R.J.; Ford, J.A.; Ryan, J.E.; Schepis, T.S. Assessment of Changes in Alcohol and Marijuana Abstinence, Co-Use, and Use Disorders Among US Young Adults From 2002 to 2018. JAMA Pediatr. 2021, 175, 64–72. [Google Scholar] [CrossRef]
- Knopf, A. Teen cannabis use increases risk of suicidality and depression during young adulthood. Brown Univ. Child Adolesc. Behav. Lett. 2019, 35, 3–4. [Google Scholar] [CrossRef]
- Wong, S.S.; Zhou, B.; Goebert, D.; Hishinuma, E.S. The risk of adolescent suicide across patterns of drug use: A nationally representative study of high school students in the United States from 1999 to 2009. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 1611–1620. [Google Scholar] [CrossRef]
- Horwood, L.J.; Fergusson, D.M.; Coffey, C.; Patton, G.C.; Tait, R.; Smart, D.; Letcher, P.; Silins, E.; Hutchinson, D.M. Cannabis and depression: An integrative data analysis of four Australasian cohorts. Drug Alcohol. Depend. 2012, 126, 369–378. [Google Scholar] [CrossRef]
- Floyd Campbell, L. Depression and Marijuana Use among a Sample of Urban Females: Is Stage of Development Important? Subst. Use Misuse 2018, 53, 1008–1014. [Google Scholar] [CrossRef]
- Scholes-Balog, K.E.; Hemphill, S.A.; Patton, G.C.; Toumbourou, J.W. Cannabis use and related harms in the transition to young adulthood: A longitudinal study of Australian secondary school students. J. Adolesc. 2013, 36, 519–527. [Google Scholar] [CrossRef]
- Wilkinson, A.L.; Halpern, C.T.; Herring, A.H.; Shanahan, M.; Ennett, S.T.; Hussey, J.M.; Harris, K.M. Testing Longitudinal Relationships Between Binge Drinking, Marijuana Use, and Depressive Symptoms and Moderation by Sex. J. Adolesc. Health 2016, 59, 681–687. [Google Scholar] [CrossRef]
- Richter, L.; Pugh, B.S.; Ball, S.A. Assessing the risk of marijuana use disorder among adolescents and adults who use marijuana. Am. J. Drug Alcohol Abus. 2017, 43, 247–260. [Google Scholar] [CrossRef]
- Cohn, A.; Johnson, A.; Ehlke, S.; Villanti, A.C. Characterizing substance use and mental health profiles of cigar, blunt, and non-blunt marijuana users from the National Survey of Drug Use and Health. Drug Alcohol. Depend. 2016, 160, 105–111. [Google Scholar] [CrossRef]
- Bechtold, J.; Simpson, T.; White, H.R.; Pardini, D. Chronic adolescent marijuana use as a risk factor for physical and mental health problems in young adult men. Psychol. Addict. Behav. 2015, 29, 552–563. [Google Scholar] [CrossRef]
- Welsh, J.W.; Knight, J.R.; Hou, S.S.; Malowney, M.; Schram, P.; Sherritt, L.; Boyd, J.W. Association Between Substance Use Diagnoses and Psychiatric Disorders in an Adolescent and Young Adult Clinic-Based Population. J. Adolesc. Health 2017, 60, 648–652. [Google Scholar] [CrossRef]
- Leadbeater, B.J.; Ames, M.E.; Linden-Carmichael, A.N. Age-varying effects of cannabis use frequency and disorder on symptoms of psychosis, depression and anxiety in adolescents and adults. Addiction 2019, 114, 278–293. [Google Scholar] [CrossRef]
- Chadi, N.; Li, G.; Cerda, N.; Weitzman, E.R. Depressive Symptoms and Suicidality in Adolescents Using e-Cigarettes and Marijuana: A Secondary Data Analysis From the Youth Risk Behavior Survey. J. Addict. Med. 2019, 13, 362–365. [Google Scholar] [CrossRef]
- London-Nadeau, K.; Rioux, C.; Parent, S.; Vitaro, F.; Côté, S.M.; Boivin, M.; Tremblay, R.E.; Séguin, J.R.; Castellanos-Ryan, N. Longitudinal associations of cannabis, depression, and anxiety in heterosexual and LGB adolescents. J. Abnorm. Psychol. 2021, 130, 333–345. [Google Scholar] [CrossRef]
- Phillips, K.T.; Phillips, M.M.; Duck, K.D. Factors Associated With Marijuana use and Problems Among College Students in Colorado. Subst. Use Misuse 2018, 53, 477–483. [Google Scholar] [CrossRef]
- Levy, S.; Weitzman, E.R. Acute Mental Health Symptoms in Adolescent Marijuana Users. JAMA Pediatr. 2019, 173, 185–186. [Google Scholar] [CrossRef]
- Power, E.; Sabherwal, S.; Healy, C.; O’ Neill, A.; Cotter, D.; Cannon, M. Intelligence quotient decline following frequent or dependent cannabis use in youth: A systematic review and meta-analysis of longitudinal studies. Psychol. Med. 2021, 51, 194–200. [Google Scholar] [CrossRef]
- Gobbi, G.; Atkin, T.; Zytynski, T.; Wang, S.; Askari, S.; Boruff, J.; Ware, M.; Marmorstein, N.; Cipriani, A.; Dendukuri, N.; et al. Association of Cannabis Use in Adolescence and Risk of Depression, Anxiety, and Suicidality in Young Adulthood: A Systematic Review and Meta-analysis. JAMA Psychiatry 2019, 76, 426–434. [Google Scholar] [CrossRef]
- Han, B.; Compton, W.M.; Einstein, E.B.; Volkow, N.D. Associations of Suicidality Trends With Cannabis Use as a Function of Sex and Depression Status. JAMA Netw. Open 2021, 4, e2113025. [Google Scholar] [CrossRef]
- Meier, M.H.; Beardslee, J.; Pardini, D. Associations between Recent and Cumulative Cannabis Use and Internalizing Problems in Boys from Adolescence to Young Adulthood. J. Abnorm. Child Psychol. 2020, 48, 771–782. [Google Scholar] [CrossRef]
- Chimoriya, R.; Mohammad, Y.; Thomson, R.; Webster, C.; Dunne, R.; Aibangbee, M.; Ip, D.; Slewa-Younan, S. Mental illness stigma and associated factors among Arabic-speaking refugee and migrant populations in Australia. Int. J. Ment. Health Syst. 2023, 17, 11. [Google Scholar] [CrossRef]
- Douglass, C.H.; Win, T.M.; Goutzamanis, S.; Lim, M.S.C.; Block, K.; Onsando, G.; Hellard, M.; Higgs, P.; Livingstone, C.; Horyniak, D. Stigma Associated with Alcohol and Other Drug Use Among People from Migrant and Ethnic Minority Groups: Results from a Systematic Review of Qualitative Studies. J. Immigr. Minor. Health 2023, 25, 1402–1425. [Google Scholar] [CrossRef]
- GBD 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry 2018, 5, 987–1012. [Google Scholar] [CrossRef]
- Mahone, I.H.; Farrell, S.; Hinton, I.; Johnson, R.; Moody, D.; Rifkin, K.; Moore, K.; Becker, M.; Barker, M.R. Shared decision making in mental health treatment: Qualitative findings from stakeholder focus groups. Arch. Psychiatr. Nurs. 2011, 25, e27–e36. [Google Scholar] [CrossRef]
- Tiruneh, Y.M.; Elliott, K.S.; Oyer, L.; Elueze, E.; Casanova, V. Addressing Substance Use and Misuse in East Texas: Stakeholder-Driven Needs and Priorities. Int. J. Environ. Res. Public. Health 2022, 19, 5215. [Google Scholar] [CrossRef]
- Aarons, G.A.; Wells, R.S.; Zagursky, K.; Fettes, D.L.; Palinkas, L.A. Implementing Evidence-Based Practice in Community Mental Health Agencies: A Multiple Stakeholder Analysis. Am. J. Public Health 2009, 99, 2087–2095. [Google Scholar] [CrossRef]
- Haller, D.M.; Meynard, A.; Lefebvre, D.; Hasselgård-Rowe, J.; Broers, B.; Narring, F. Excessive substance use among young people consulting family doctors: A cross-sectional study. Fam. Pract. 2015, 32, 500–504. [Google Scholar] [CrossRef][Green Version]
- Turner, S.D.; Spithoff, S.; Kahan, M. Approach to cannabis use disorder in primary care: Focus on youth and other high-risk users. Can. Fam. Physician 2014, 60, 801–808.e423-832. [Google Scholar]
- Shi, L.; Stevens, G.D. Vulnerable Populations in the United States; John Wiley & Sons: Hoboken, NJ, USA, 2021. [Google Scholar]
- Steinberg, K.L.; Roffman, R.A.; Carroll, K.M.; Kabela, E.; Kadden, R.; Miller, M.; Duresky, D.; Marijuana Treatment Project Research Group. Tailoring cannabis dependence treatment for a diverse population. Addiction 2002, 97, 135–142. [Google Scholar] [CrossRef]
- Hyshka, E. Applying a social determinants of health perspective to early adolescent cannabis use–An overview. Drugs Educ. Prev. Policy 2013, 20, 110–119. [Google Scholar] [CrossRef]
- Rana, K.; Shrestha, V.; Chimoriya, R. The effect of housing on health and challenges of demographic changes. Glob. J. Sci. Front. Res. 2020, 20, 75–82. [Google Scholar]
- Amanda, R.; Rana, K.; Saunders, P.; Tracy, M.; Bridges, N.; Poudel, P.; Arora, A. Evaluation of the usability, content, readability and cultural appropriateness of online alcohol and other drugs resources for Aboriginal and Torres Strait Islander Peoples in New South Wales, Australia. BMJ Open 2023, 13, e069756. [Google Scholar] [CrossRef]
- Connery, H.S.; McHugh, R.K.; Reilly, M.; Shin, S.; Greenfield, S.F. Substance use disorders in global mental health delivery: Epidemiology, treatment gap, and implementation of evidence-based treatments. Harv. Rev. Psychiatry 2020, 28, 316. [Google Scholar] [CrossRef]
- Johnson, L.L. Design of observational studies. In Principles and Practice of Clinical Research; Elsevier: London, UK, 2018; pp. 231–248. [Google Scholar]
- Faggiano, F.; Vigna-Taglianti, F.D.; Versino, E.; Zambon, A.; Borraccino, A.; Lemma, P. School-based prevention for illicit drugs use: A systematic review. Prev. Med. 2008, 46, 385–396. [Google Scholar] [CrossRef]
- Van Boekel, L.C.; Brouwers, E.P.M.; van Weeghel, J.; Garretsen, H.F.L. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug Alcohol Depend. 2013, 131, 23–35. [Google Scholar] [CrossRef]
- Rana, K.; Poudel, P.; Chimoriya, R. Qualitative Methodology in Translational Health Research: Current Practices and Future Directions. Healthcare 2023, 11, 2665. [Google Scholar] [CrossRef]
- Norberg, M.M.; Kezelman, S.; Lim-Howe, N. Primary prevention of cannabis use: A systematic review of randomized controlled trials. PLoS ONE 2013, 8, e53187. [Google Scholar] [CrossRef]
- Popova, L.; McDonald, E.A.; Sidhu, S.; Barry, R.; Richers Maruyama, T.A.; Sheon, N.M.; Ling, P.M. Perceived harms and benefits of tobacco, marijuana, and electronic vaporizers among young adults in Colorado: Implications for health education and research. Addiction 2017, 112, 1821–1829. [Google Scholar] [CrossRef]
- Robertson, E.B.; David, S.L.; Rao, S.A. Preventing Drug Use among Children and Adolescents: A Research-Based Guide for Parents, Educators, and Community Leaders; National Institute on Drug Abuse (NIDA): North Bethesda, MD, USA, 2003. [Google Scholar]
- Choi, S.; Hong, S.; Gatanaga, O.; Yum, A.; Lim, S.; Neighbors, C.; Yi, S. Substance Use and Treatment Disparities Among Asian Americans, Native Hawaiians, and Pacific Islanders: A Systematic Review. Drug Alcohol Depend. 2024, 256, 111088. [Google Scholar] [CrossRef] [PubMed]
- Radosevich, D. Designing an outcomes research study. In Understanding Health Care Outcomes Research, 2nd ed.; Jones and Bartlett: Sudbury, MA, USA, 2006; pp. 23–58. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).