Highlights
What are the main findings?
- Diabetic ketoacidosis (DKA) requires hospitalization for aggressive fluid replacement, electrolyte management, and insulin therapy.
- The major precipitating factors for DKA include a new diagnosis of diabetes, non-adherence to insulin therapy, and infections such as sepsis in patients with diabetes.
- Patient education and appropriate insulin dosing are key to preventing recurrence. Special patient populations, such as those with pregnancy, renal failure, acute pancreatitis, or insulin pump users, should be carefully considered.
What is the implication of the main finding?
- Our review demonstrates that the management of DKA remains standard, even in special patient populations such as those with pregnancy, acute pancreatitis, and, to a certain extent, patients on renal replacement therapy or with congestive heart failure.
- Euglycemic DKA and ketonemia are on the rise with the increased use of Sodium–Glucose Cotransporter (SGLT) inhibitors. Patients are advised to follow the STICH protocol (STop SGLT inhibitor, Insulin administration, Carbohydrate consumption, Hydration).
- Patients with COVID-19 exhibit elevated levels of proinflammatory markers similar to those seen in DKA; however, no causal relationship has been established.
Abstract
Diabetic ketoacidosis (DKA) is the most common hyperglycemic emergency and causes the greatest risk for death that could be prevented in patients with diabetes mellitus. DKA occurs more commonly among patients with type-1 diabetes with a thirty percent of the cases take place in patients with type 2 diabetes. DKA is characterized by sever hyperglycemia, metabolic acidosis and ketosis. Proper management of DKA requires hospitalization for aggressive replacement and monitoring of fluids, electrolytes and insulin therapy. Management of DKA has been updated with guidelines, to help standardize care, and reduce mortality and morbidity. The major precipitating factors for DKA include new diagnosis of diabetes, non-adherence to insulin therapy as well as infection in patients with diabetes. Discharge plans should include appropriate selection of insulin dosing and regimens as well as patient education to prevent recurrence of DKA. Further, definition and management of euglycemic DKA in patients prescribed sodium-glucose co-transporter 2 inhibitors are discussed. Special consideration is reviewed for specific patient population including pregnancy, renal replacement, acute pancreatitis, and insulin pump users as well as patients with COVID-19.
1. Introduction
1.1. Diabetic Ketoacidosis (DKA)
DKA is characterized by uncontrolled hyperglycemia (>250 mg/dL), metabolic acidosis, and increased ketone concentration [1]. DKA incidence increased at annual rate of 6.3% most notably in persons aged <45 years with significant increase in hospitalization rate between 2008 and 2018 [2]. Nevertheless, overall in-hospital mortality rates declined during the study period from 1.1% to 0.4% [3]. DKA is a life-threatening, but preventable complication of type-1 diabetes with a thirty percent of the cases that could be attributed to type-2 diabetes. The major clinical difference between these two types of diabetes is a lesser degree of acidosis and absence of hyperkalemia in type 2 diabetes [4].
1.2. Pathophysiology of DKA
The pathophysiology of DKA is a multifactorial and driven by hyperglycemia, dehydration, ketosis, and electrolyte imbalance. As depicted in Figure 1, insulin deficiency triggers a cascade of maladaptive physiologic responses involving hormone-sensitive lipase which is activated such as lipoprotein lipase resulting in increased triglycerides and free fatty acids (FFA). In return, FFA triggers excessive ketone bodies formation in the liver leading to metabolic acidosis. Activation of counter regulatory hormones (cortisol, glucagon, growth hormone, and catecholamines) drive hyperglycemia via various mechanisms including increased glycogenolysis, gluconeogenesis resulting in progressive volume depletion and electrolyte loss (reviewed in [5]). Production of prostaglandins can contribute also to nausea, vomiting and abdominal pain [6]. Additional risk factors include infection, pancreatitis, myocardial infarction, stroke as well as secondary causes due to drugs such as steroid, thiazides, sympathomimetics.

Figure 1.
Schematic framework of the pathophysiology of diabetic ketoacidosis. In DKA, insulin insufficiency sets off a cascade of maladaptive physiologic responses involving activation of lipase, increased free fatty acids that triggers excessive ketone bodies leading to metabolic acidosis. Activation of counter regulatory hormones drive hyperglycemia via various mechanisms including increased glycogenolysis, gluconeogenesis resulting in progressive volume depletion and electrolyte loss.
1.3. DKA Presentation and Diagnosis
As a result of increased lipolysis and decreased lipogenesis, surplus free fatty acids are converted to ketone bodies: β-hydroxybutyrate (β-OHB) and acetoacetate. Majority of patients with DKA present with symptoms such as polyuria, polydipsia, weight loss, vomiting, dehydration, weakness, and mental status changes. Physical findings include poor skin turgor, Kussmaul (deep/labored) respirations, tachycardia and/or hypotension. Gastrointestinal symptoms can include nausea, vomiting and diffuse abdominal pain [1]. The American Diabetes Association diagnostic criteria for DKA include elevated serum glucose level above 250 mg/dL, arterial pH of ≤7.30, bicarbonate level of ≤18 mEq/L an elevated serum ketone level, a pH less than 7.3 and, a serum bicarbonate level less than 18 mEq per L (18 mmol per L) and adjusted for albumin anion gap of >10–12.3. Table 1, adopted from Kitabchi et al., 2009 [1] shows detailed diagnostic criteria for various stages of DKA based on the degree of acidosis. The detection of positive urine or serum ketones further confirm the diagnosis of DKA, however obtaining serum level of ketone bodies can be more laborious. Of note, the diagnosis of DKA could be challenging in patients with end stage renal disease, due to existing chronic metabolic acidosis or mixed acid-base disorders. Therefore, detection of anion gap of >20 usually is used to support the diagnosis of DKA in these patients [7].

Table 1.
Diagnostic criteria and deficits of electrolytes in different stages of diabetic ketoacidosis (DKA). Reprinted/adapted with permission from Kitabchi et al., 2009 “hyperglycemic crises in adult patients with diabetes” [1]. Copyright © 2009 by the American Diabetes Association.
2. Management of DKA
2.1. Standard Treatment of DKA
Most patients with DKA present to the emergency room for the management of hyperglycemic crisis. Successful treatment of DKA requires correction of dehydration, hyperglycemia and electrolyte imbalances with frequent monitoring of clinical and metabolic parameters that support resolution of DKA [1]. Specific therapeutic goals of DKA management include optimization of (1) volume status; (2) hyperglycemia and ketoacidosis; (3) electrolyte abnormalities; and (4) potential precipitating factors.
As depicted in Figure 2, early steps of DKA management include: 1—collection of blood for metabolic profile before initiation of intravenous fluids; 2—infusion of 1-L of 0.9% sodium chloride over 1 h after drawing initial blood samples; 3—ensuring potassium level of >3.3 mEq/L before initiation of insulin therapy and 4—initiating insulin therapy only after execution of the initial steps [1,2,3].
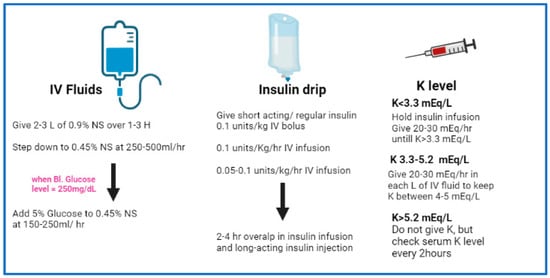
Figure 2.
Schematic representation of a simplified protocol/workflow for management of adult patients with DKA. Abbreviations: NS, normal saline, H, hour, Bl. blood, K potassium, IV intravenous.
2.2. Treatment–Fluid Therapy
Since DKA patients experience fluid loss of approximately 6–9 L, the goal of fluid resuscitation aims to replete that volume within 24–36 h with 50% of resuscitation fluid administered within first 8–12 h of presentation. Current DKA guidelines recommend initiating volume repletion with isotonic saline (0.9% NaCl) at 15–20 mL/kg/h followed by hypotonic saline solution (0.45% saline) at a rate of 4–14 mL/kg/h then re-evaluate. Fluid resuscitation continue as long as the patient is hemodynamically stable and the corrected serum sodium is normal to high. If not, corrected sodium level can dictate further volume repletion with a different type of IV fluid [8]. Fluid resuscitation will decrease hyperglycemia by stimulating osmotic diuresis if renal function is not severely compromised and restore peripheral action of insulin. Traditionally, hyperglycemia is corrected faster than ketoacidosis (6 and 12 h, respectively) [9]. Hence, when glucose levels fall below 200–250 mg/dL, intravenous fluids should be switched to dextrose-containing 0.45% NaCl solution to allow continued insulin administration until ketonemia and avoid hypoglycemia [9].
Due to hyperglycemia in DKA causing osmotic diuresis and severe dehydration, the mainstay of treatment is rehydration. Traditional treatment as mentioned above is “one bag protocol (1 L/bag)” with normal saline and supplemental electrolytes vs. “two bag protocol (1 L/bag)”. The two bags of fluids include one containing 1N saline (0.9% NaCl) and supplemental electrolytes and the other bag contains 0.45% NaCl solution with additional 10% dextrose. By changing the individual rates of Bag 1 and Bag 2 and hence, by changing the relative amounts of the two fluids will functionally change the final dextrose concentration to cope with glucose level. The change in percentages of fluids changes the sodium concentration as well. For instance, when the glucose level >300 mg/dL, the rate of Bag 1 will be 100% and Bag 2 will be zero and when glucose level <300 mg/dL and >200 mg, then the rate of Bag1 will be 50% and Bag 2 will be 50% and when the glucose level <150 mg then the rate of Bag 1 will be zero and Bag 2 will be 100%. Of note, each institution will modify and adopt the exact rate and type of fluids with the goal of maintaining glucose of 150–300. Published studies showed significant improvement of earlier closure of anion gap with “two bag protocol” (~10-h) compared to “one bag protocol” (~14-h) [10,11]. Hyperglycemia was also noted to improve faster in “two bag protocol” (7 h) compared to “one bag protocol” (9 h). On the other hand, there was no difference in the time to improve serum HCO3 level >18 mg/dL or the hospital length of stay differed between the two groups [11].
2.3. Treatment–Insulin Therapy
Randomized controlled studies in patients with DKA have shown that insulin therapy is effective regardless of the route of administration whether insulin is delivered via continuous intravenous infusion or by frequent subcutaneous or intramuscular injections [12,13]. Recently, inhaled insulin was used for management of DKA in a patient with subcutaneous insulin resistance syndrome [14]. However, IV continuous infusion with regular insulin remains the mainstay of treatment due to its short half-life and easy titration in comparison to other modes of administration [12,15]. Treatment algorithms recommended the administration of an initial intravenous dose of regular insulin (0.1 unit/kg) followed by infusion of (0.1 unit/kg/h). Other studies showed that an hourly insulin infusion of (0.14 units/kg body wt) would be sufficient without a bolus dose [16]. Monitor glucose (every 1 to 2 h) and expect decrease of 50 to 75 mg/dL/h. If the level did not drop, then infusion rate should be increased or bolus another dose of 0.14 unit/kg. When the plasma glucose reaches 200 mg/dL, the rate of insulin infusion should be decreased to 0.02–0.05 unit/kg/h. Continue close monitoring glucose to maintain glucose level at 150–200 mg/dL.
Other delivery methods of insulin delivery include subcutaneous rapid-acting insulin analogs in in non–intensive care unit (ICU) settings. Safety and efficacy of subcutaneous treatment with rapid-acting such as lispro and aspart every 1 or 2 h has been shown to be similar to the standard I.V regular insulin in the ICU settings [17]. The clinical parameters including the decline rate of blood glucose level and the correction of ketosis duration were similar among the two groups [17]. Additionally, review of literature of 5 randomized clinical trials in patients with DKA showed no significant difference between the use of subcutaneous rapid-acting insulin analogues versus intravenous regular insulin [18]. Incidence of hypoglycemic episodes was the main adverse effect for both regimens.
2.4. Treatment-Potassium
Despite total-body potassium depletion, patients with hyperglycemic crises can present with mild hyperkalemia that could be attributed to reduced glomerular filtration rate and/or extracellular shift of potassium. The later could be triggered by insulin deficiency, hypertonicity, or acidemia [19]. Occasionally, patients with DKA may present with significant hypokalemia as a result of correction of volume or metabolic acidosis and/or insulin therapy [1]. Hypokalemia can cause life-threatening arrhythmias and respiratory muscle weakness [20]. In such cases, potassium replacement should begin with fluid therapy, and insulin treatment should be delayed until potassium concentration is restored to >3.3 mEq/L. Generally, administration of 20–30 mEq potassium in each liter of infusion fluid is sufficient to maintain a serum potassium concentration within the normal range of 4–5 mEq/L.
3. DKA in Special Population
3.1. DKA in Pregnancy
DKA in pregnancy is poorly understood condition due to limited published evidence of risk factors and outcomes. DKA in pregnancy is an obstetric and medical emergency for both the pregnant woman and the fetus and therefore requires prompt and aggressive treatment [21]. Fetal and neonatal morbidity can be the direct consequence of the extremely poor tolerance of the fetus to acidosis, resulting in intrauterine death or preterm delivery. DKA in pregnancy can occur at near normal levels of blood glucose (euglycemic DKA) and often progresses more rapidly as compared with nonpregnancy [22]. Prior studies identified number of risk factors that can lead to precipitating episodes of diabetic ketoacidosis in pregnant patients. The major risk factors are intractable vomiting and starvation (53%), inadequate insulin management (18%), and infection (27%) including pyelonephritis, respiratory, chorioamnionitis, ear infection, cellulitis, or tooth abscess. Additional common causes include the use of β-sympathomimetic drugs, steroid administration for fetal lung maturation) and diabetic gastroparesis [21]. Management of DKA during pregnancy is similar to DKA in non-pregnant patients. Initial fluid replacement starts with 0.9% sodium chloride (normal saline) at a rate of 15 to 20 mL/kg (−1–1.5 L) over the first hour then the rate and type of fluids are determined accordingly. The clinical assessment of the mother involves blood pressure, pulse, hydration, mental status, fluid input and urine output. Additionally, fetal heart rate monitoring is recommended for a gestational age of 24 weeks or more [23].
3.2. DKA in Renal Replacement
Diabetes is one of the major precipitating factors of end-stage renal disease (ESRD) in the US [24]. A normal renal function is integral to maintain insulin homeostasis including its secretion, clearance and level of sensitivity. Hence, impairment or loss of renal function presents multiple challenges in glycemic control for ESRD-patients. Driven mainly by accumulated uremic toxins, ESRD can increase hepatic gluconeogenesis reduce utilization of insulin peripherally and drive insulin resistance [25]. Interestingly, DKA is uncommon in ESRD-patients possibly because of the absence of glycosuria and osmotic diuresis. Clinical and biochemical lab presentation of DKA in ESRD-dialysis patients is different when compared to non-dialysis patients [26]. For instance, patients with ESRD present with higher admission blood glucose, volume overload and need for mechanical ventilation [27]. Interestingly, ESRD-patients have lower A1c, similar mortality, but longer length of stay and higher hospital costs [27].
Overall, ESRD dialysis patients maintain normal intracellular and extracellular volume. Therefore, they present with minimal volume depletion, and instead they might experience edema of lungs and lower extremities as well as elevated blood pressure; collectively signs of volume expansion. Traditionally, dialysis patients do not require intravenous fluids unless patients exhibit clinical signs of extracellular fluid loss such as vomiting or diarrhea. If needed, small boluses of normal saline (250 mL) would be administered under tight monitoring to maintain stable hemodynamic parameters. Hemodialysis is reserved for severe hyperkalemia and pulmonary edema and continues to be controversial in general. Hyperkalemia in ESRD can be life threatening and could be attributed to reduced glomerular filtration rate, lack of insulin, and hypertonicity [28]. Severe hyperkalemia requires close monitoring for signs of cardiac toxicity and detection of potassium level post hemodialysis.
3.3. DKA in Acute Pancreatitis and Islets Transplants
Acute pancreatitis (AP) is one of the common causes of acute abdominal pain related hospital admission with high morbidity and mortality [29]. AP is associated mostly with hyperlipidemia, uncontrolled diabetes, alcoholism and is seen more with patients with familial hyperlipidemia [30]. Several reports showed the incidence of severe DKA in patients with AP that was associated with hypertriglyceridemia [29,31,32,33,34]. It is difficult to establish a causal relationship whether DKA is the cause or the result of AP, DKA was managed using standard fluid resuscitation and insulin infusion in these patients.
With the success of organ transplants, wide use of immunosuppressants including tacrolimus can cause drug-induced pancreatic islet cell damage and subsequent decrease in insulin secretion [35]. This can lead to post-transplant diabetes mellitus and diabetic ketoacidosis [36]. Recent report documented a case of tacrolimus-induced acute pancreatitis in association with hypertriglyceridemia and DKA post-kidney transplant [37]. Pancreatic islet transplantation is becoming a potential approach to β-cell replacement therapy and the treatment of insulin-deficient diabetes in the setting of recurrent AP or chronic pancreatitis [38]. Additionally, recurrent episodes of DKA in patients with type-1 diabetes is one of the considerations for islet transplantation [39]. Islet auto-transplantation involves infusion of islets isolated from the diseased pancreas via the portal vein and intrahepatic engraftment. Tacrolimus remains one of the maintenance immunosuppression for islet transplant recipients with close monitoring for glucose levels and insulin secretions in these patients [40]. Despite the success of islet transplantation in improving insulin-requirements in type-1 diabetes, it comes with a list of limitations mainly associated with sustained use of immunosuppressants [38]. As such, it should be saved for patients with type-1 diabetes in whom other, less invasive current treatments have been repeatedly ineffective.
3.4. DKA and Sodium–Glucose Cotransporter (SGLT) Inhibitors
SGLT2 inhibitors including Canagliflozin, Dapagliflozin, Empagliflozin and Ertugliflozin are popular in the US and Europe as their use is approved in patients with type-2 diabetes as a first line therapy. Further, they have been studied and used off-label in combination with insulin therapy in patients with type 1 diabetes [41]. The use of SGLT2 inhibitors has been increasingly associated with an increased risk of DKA primarily in patients with type-1 diabetes and to a lesser extent in type-2 diabetes. Blocking SGLT2 transporter in the proximal tubule of the kidney results in glycosuria and natriuresis. SGLT-2 inhibition results in excretion of 50–60% of the filtered glucose, but also exerts a mild natriuretic effect that provide additional benefits including weight loss and reduction in systolic/diastolic blood pressure [42]. SGLT-2 inhibitors are potent cardioprotective and nephroprotective agents, offering reductions of up to 38% in cardiovascular mortality, 35% in heart failure hospitalization, 45% in progression of renal disease, and 30% in all-cause mortality (reviewed in [43]). The ability of SGLT2 inhibitors to induce osmotic diuresis allows the body to get rid of extra free water and supported potential use of SGLT2 inhibitors in cases of euvolemic hyponatremia [44,45]. While this particular use warrant further studies, a recent case review showed that SGLT2 inhibitors can cause hyponatremia as a potential, rare side effect and that the use of SGLT2 inhibitor should be evaluated or stopped in case of persistent hyponatremia [46].
Development of euglycemic DKA and ketonemia remain the most dangerous side effects for patients who develop DKA while on SGLT inhibitor therapy [47]. SGLT2 inhibitors can induce a state of ketosis by increasing both urinary glucose excretion and reabsorption of ketone bodies. Precipitating factors include prolonged periods of fasting, reduced carbohydrate intake, excessive physical activity, infection, pregnancy or alcohol consumption [48]. These factors can accelerate lipolysis and increased free fatty acid levels that eventually trigger hepatic formation of ketone bodies (see Figure 3).
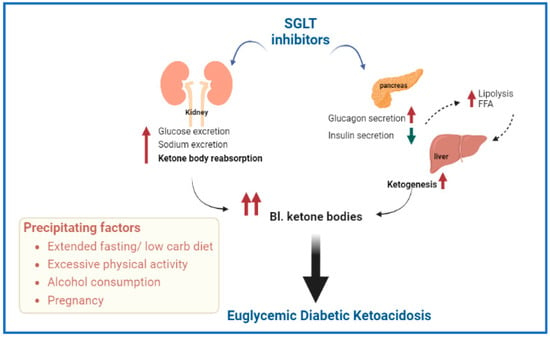
Figure 3.
Schematic representation of possible mechanisms involved in the development of euglycemic diabetic ketoacidosis (DKA) associated with sodium glucose transporter (SGLT) inhibitors. Precipitating factors are also included. Abbreviations—FFA: free fatty acids, Bl.: blood.
SGLT2 inhibitors are approved for type 1 diabetes in Europe and Japan, with off-label use in type-1 diabetes in the US [49]. Due to mild hyperglycemia associated with SGLT use, DKA diagnosis can be missed or delayed. Therefore, there is a need for patients to be educated regarding how to recognize and reduce elevated ketone levels. Development of unusual symptoms of physical sickness such as nausea, vomiting, abdominal pain, fatigue or malaise in these patients should be recognized. Recognizing these symptoms should prompt measuring ketones in the blood (preferred) or urine to evaluate for DKA [50]. A number of protocols have been developed to treat DKA for individuals who are treated with SGLT2 inhibitors. One of them is the STOP DKA protocol (Symptomatic to stop SGLT inhibitor, Test ketones and glucose, Oral ingestion of fluids and carbohydrates, Protocol instructions for insulin and carbohydrates) [50]. STOP DKA defines mild ketonemia as <1.0 mmol/L vs. 0.6 mmol/L in most of the other protocols. SGLT2 inhibitors should be stopped as soon as any symptoms of physical illness (e.g., lethargy, loss of appetite, nausea, or abdominal pain) or elevated ketone levels are detected and resumed only after ketone levels return to normal. Generally, patients should consume carbohydrates and give insulin in an attempt to lower ketone levels. If levels of ketones are elevated then the STICH (STop SGLT inhibitor, Insulin administration, Carbohydrate consumption, Hydration) protocol should be initiated [51]. After stopping SGLT2 inhibitor therapy, patients should receive rapid- or short-acting insulin and consume 15–30 g of rapidly absorbed carbohydrate such as juice, soda, or milk along with 300–500 mL of fluid. The level of ketones should be monitored every 3–4 h until resolution back to normal. Comparatively, the STOP DKA protocol provides specific insulin recommendations based on blood glucose and ketone levels, while the STICH protocol recommends that patients take 1.5 times their usual dose of insulin.
If symptoms of physical sickness or high ketone levels (>3.0 mmol/L) persist, patients should pursue medical help and hospitalization. Standard DKA treatment protocols are followed as described earlier (Section 2.1), with careful monitoring of ketone levels and allowing patients to consume carbohydrates. Of note, DKA related to SGLT2 inhibitors may result in glycosuria for at least 3 additional days after hospital admission in patients with either type 1 or type 2 diabetes [52], suggesting that the SGLT2 inhibitors require more time to clear after stopping the medication. Future studies are warranted to provide further information for DKA management in patients with SGLT2 inhibitors.
3.5. DKA in Patients with Congestive Heart Failure (CHF)
Similar to patients with chronic kidney disease, specific population considerations should be given to patients with CHF [10]. These patients tend to retain fluids; therefore, volume resuscitation should be carefully titrated in patient with CHF. A conservative fluid resuscitation is crucial in the management of the DKA patient with CHF. Minimal fluid bolus, such as (250–500 mL) is recommended in hypovolemic patients with subsequent monitoring for signs/symptoms of volume overload. Intravenous insulin is the main stay to improve acidosis by preventing ketone production [25]. Further, urine output monitoring is an important step in patients with hyperglycemic crises.
Recently, the SGLT2 inhibitors demonstrated significant cardiorenal benefits and they are now approved to reduce CV events/death, heart failure hospitalization [53], even in patients with no diabetes history. There is a higher possibility to exhibit euglycemia DKA [54]. Hence, similar consideration for these patients with CHF to be educated regarding how to recognize and treat euglycemic DKA and manage ketone levels as described earlier.
3.6. DKA and Insulin Pump Users
Early studies showed that insulin pump users commonly known as continuous subcutaneous insulin infusion are more prone to development of DKA [55]. Insulin pump users rely on rapid or short acting insulin, but not the long acting insulin. Hence, if the pump fails or the canula blocked or dislodged, the insulin delivery will be stopped and blood glucose levels rise triggering ketoacidosis to develop rapidly. The prevalence of DKA in users of insulin pump therapy is decreasing most likely due to significant improvements of technology [56]. Of note, impact of patient training and education is most evident by improved glycemic control, and fewer of episodes of hypoglycemia and DKA after 1-year of pump use [56].
For the management of possible DKA associated with insulin pump therapy, first the pump-related problem should be identified and rectified. For example, re-calibrating the pump, re-siting the cannula, and changing the tubing should be part of patient education. Switching insulin pump to alternative insulin such as an intravenous infusion can be useful because of altered insulin absorption and tissue perfusion [57]. If a pump user develops DKA, insulin pump should be immediately discontinued and standard DKA treatment started. Once DKA has resolved, insulin pump therapy can be restarted at the patient’s usual basal rate along with transitional dose of intravenous insulin infusion until a bolus is given via pump [58].
3.7. DKA in Patients with COVID-19
During the SARS-CoV-2 commonly referred to as COVID-19 pandemic, it has been established that diabetes is a frequent comorbidity and DKA has been documented in patients with COVID-19 in both patients with T1D and patients with T2D [59]. There is evidence that support a possible bidirectional relationship between SARS-CoV2 infection and diabetes, with infection being associated with worsening of hyperglycemia in preexisting diabetes and new-onset hyperglycemia [60]. Nevertheless, there are insufficient data to determine if DKA is more prevalent in COVID-19 and if the SARS-CoV-2 virus poses an increased risk over other severe infectious diseases. To date, only 1 study has described the prevalence of acidosis and ketoacidosis in 658 hospitalized patients with confirmed COVID-19 [61]. In the same study, patients with ketosis were about twice as likely to have diabetes at baseline, and the 3 individuals who developed DKA had underlying diabetes (1 with T1D, 2 with T2D). Ketosis was also associated with higher mortality. A more recent metanalysis showed that DKA is not uncommon in COVID-19 patients with diabetes mellitus and results in a mortality rate of 25.9% [62]. The major determinants of mortality in DKA patients with COVID-19 infection are pre-existing diabetes mellitus type 2, older age [≥60 years old], male gender, BMI ≥ 30, blood glucose level > 1000 mg/dL, and anion gap ≥ 30 mEq/L [62].
One of the important and common finding among COVID-19 patients is that severe disease is accompanied by high levels of inflammatory markers, which are also elevated in the setting of DKA independent of accompanying illness. IL-6 has been highlighted as likely playing a role in a maladaptive immune response to the SARS-CoV-2 virus and has been proposed as a possible treatment target [63]. Interestingly, IL-6 has also been also found to be elevated in patients with DKA and is thought to be mostly a driver of ketosis rather than a result [64]. Future studies are warranted to explore the role of inflammation in DKA and COVID-19 in relation to clinical outcomes.
4. Summary and Conclusions
DKA is the most common hyperglycemic emergency and causes the greatest risk for mortality in patients with diabetes mellitus. Epidemiological studies showed more prevalence of DKA among patients with type-1 diabetes, yet almost a third of the cases occur among those with type 2 diabetes. DKA is characterized by hyperglycemia, metabolic acidosis and ketosis. Patients with diabetes in general, and those with type-1 diabetes would benefit from being educated to recognize and reduce early signs of DKA. Standard management of DKA requires hospitalization and involves aggressive intravenous fluids, insulin therapy, electrolyte replacement. It is also clear that special patient population requires additional tweaking of DKA management as detailed above. With the wide use of SGLT2 inhibitors due to cardio- and reno-protective effects, incidence of euglycemic DKA has been increasing. Euglycemic DKA patients present with milder hyperglycemia, which makes early detection and intervention harder. Detection of ketonemia is the key for DKA risk mitigation along with consumption of oral carbohydrates and fluid and insulin for successful management. Future studies are warranted to continue to streamline and provide exact tweaks on the management of DKA in special patient population.
Funding
Self-funded.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Figures were created by BioRender.com, the online software.
Conflicts of Interest
ABE is listed as an inventor on patents relating to targeting p75NTR, which are assigned to the VA Medical Center. ABE is the Founder of Nour Therapeutics LLC with interest to develop therapeutics for diabetic complications.
References
- Kitabchi, A.E.; Umpierrez, G.E.; Miles, J.M.; Fisher, J.N. Hyperglycemic crises in adult patients with diabetes. Diabetes Care 2009, 32, 1335–1343. [Google Scholar] [CrossRef] [PubMed]
- Kichloo, A.; El-Amir, Z.; Wani, F.; Shaka, H. Hospitalizations for ketoacidosis in type 1 diabetes mellitus, 2008 to 2018. Bayl. Univ. Med. Cent. Proc. 2022, 35, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Benoit, S.R.; Zhang, Y.; Geiss, L.S.; Gregg, E.W.; Albright, A. Trends in Diabetic Ketoacidosis Hospitalizations and In-Hospital Mortality—United States, 2000–2014. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 362–365. [Google Scholar] [CrossRef] [PubMed]
- Sudhanshu, S.; Jevalikar, G.; Das, P.K.; Singh, P.K.; Bhatia, E.; Bhatia, V. Acute Respiratory Distress Syndrome: A Rare Complication in Pediatric Diabetic Ketoacidosis. Indian J. Pediatr. 2016, 83, 463–465. [Google Scholar] [CrossRef] [PubMed]
- Gosmanov, A.R.; Gosmanova, E.O.; Dillard-Cannon, E. Management of adult diabetic ketoacidosis. Diabetes Metab. Syndr. Obes. 2014, 7, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Chatzipanteli, K.; Head, C.; Megerman, J.; Axelrod, L. The relationship between plasma insulin level, prostaglandin production by adipose tissue, and blood pressure in normal rats and rats with diabetes mellitus and diabetic ketoacidosis. Metabolism 1996, 45, 691–698. [Google Scholar] [CrossRef]
- Tzamaloukas, A.H.; Rohrscheib, M.; Ing, T.S.; Siamopoulos, K.C.; Qualls, C.; Elisaf, M.S.; Vanderjagt, D.J.; Spalding, C.T. Serum potassium and acid-base parameters in severe dialysis-associated hyperglycemia treated with insulin therapy. Int. J. Artif. Organs 2005, 28, 229–236. [Google Scholar] [CrossRef]
- Nyenwe, E.A.; Kitabchi, A.E. Evidence-based management of hyperglycemic emergencies in diabetes mellitus. Diabetes Res. Clin. Pract. 2011, 94, 340–351. [Google Scholar] [CrossRef]
- Umpierrez, G.E.; Jones, S.; Smiley, D.; Mulligan, P.; Keyler, T.; Temponi, A.; Semakula, C.; Umpierrez, D.; Peng, L.; Ceron, M.; et al. Insulin analogs versus human insulin in the treatment of patients with diabetic ketoacidosis: A randomized controlled trial. Diabetes Care 2009, 32, 1164–1169. [Google Scholar] [CrossRef]
- Islam, T.; Sherani, K.; Surani, S.; Vakil, A. Guidelines and controversies in the management of diabetic ketoacidosis—A mini-review. World J. Diabetes 2018, 9, 226–229. [Google Scholar] [CrossRef]
- Munir, I.; Fargo, R.; Garrison, R.; Yang, A.; Cheng, A.; Kang, I.; Motabar, A.; Xu, K.; Loo, L.K.; Kim, D.I. Comparison of a ‘two-bag system’ versus conventional treatment protocol (‘one-bag system’) in the management of diabetic ketoacidosis. BMJ Open Diabetes Res. Care 2017, 5, e000395. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.N.; Shahshahani, M.N.; Kitabchi, A.E. Diabetic ketoacidosis: Low-dose insulin therapy by various routes. N. Engl. J. Med. 1977, 297, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Hockaday, T.D.; Turner, R.C. Small doses of intramuscular insulin in the treatment of diabetic “coma”. Lancet 1973, 2, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Gupta, M.; Gunn, S. Use of Inhaled Insulin in a Patient with Subcutaneous Insulin Resistance Syndrome: A Rare Condition. AACE Clin. Case Rep. 2019, 5, e187–e191. [Google Scholar] [CrossRef] [PubMed]
- Kitabchi, A.E.; Umpierrez, G.E.; Fisher, J.N.; Murphy, M.B.; Stentz, F.B. Thirty years of personal experience in hyperglycemic crises: Diabetic ketoacidosis and hyperglycemic hyperosmolar state. J. Clin. Endocrinol. Metab. 2008, 93, 1541–1552. [Google Scholar] [CrossRef]
- Kitabchi, A.E.; Murphy, M.B.; Spencer, J.; Matteri, R.; Karas, J. Is a priming dose of insulin necessary in a low-dose insulin protocol for the treatment of diabetic ketoacidosis? Diabetes Care 2008, 31, 2081–2085. [Google Scholar] [CrossRef]
- Umpierrez, G.E.; Latif, K.; Stoever, J.; Cuervo, R.; Park, L.; Freire, A.X.; Kitabchi, A.E. Efficacy of subcutaneous insulin lispro versus continuous intravenous regular insulin for the treatment of patients with diabetic ketoacidosis. Am. J. Med. 2004, 117, 291–296. [Google Scholar] [CrossRef]
- Andrade-Castellanos, C.A.; Colunga-Lozano, L.E.; Delgado-Figueroa, N.; Gonzalez-Padilla, D.A. Subcutaneous rapid-acting insulin analogues for diabetic ketoacidosis. Cochrane Database Syst. Rev. 2016, 2016, CD011281. [Google Scholar] [CrossRef]
- Eledrisi, M.S.; Beshyah, S.A.; Malik, R.A. Management of diabetic ketoacidosis in special populations. Diabetes Res. Clin. Pract. 2021, 174, 108744. [Google Scholar] [CrossRef]
- Kitabchi, A.E.; Umpierrez, G.E.; Murphy, M.B.; Kreisberg, R.A. Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association. Diabetes Care 2006, 29, 2739–2748. [Google Scholar] [CrossRef]
- Sibai, B.M.; Viteri, O.A. Diabetic ketoacidosis in pregnancy. Obstet. Gynecol. 2014, 123, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Diguisto, C.; Strachan, M.W.J.; Churchill, D.; Ayman, G.; Knight, M. A study of diabetic ketoacidosis in the pregnant population in the United Kingdom: Investigating the incidence, aetiology, management and outcomes. Diabet. Med. 2022, 39, e14743. [Google Scholar] [CrossRef] [PubMed]
- ohan, M.; Baagar, K.A.M.; Lindow, S. Management of diabetic ketoacidosis in pregnancy. Obstet. Gynaecol. 2017, 19, 55–62. [Google Scholar] [CrossRef]
- Koye, D.N.; Magliano, D.J.; Nelson, R.G.; Pavkov, M.E. The Global Epidemiology of Diabetes and Kidney Disease. Adv. Chronic Kidney Dis. 2018, 25, 121–132. [Google Scholar] [CrossRef]
- Seddik, A.A.; Bashier, A.; Alhadari, A.K.; AlAlawi, F.; Alnour, H.H.; Bin Hussain, A.A.; Frankel, A.; Railey, M.J. Challenges in management of diabetic ketoacidosis in hemodialysis patients, case presentation and review of literature. Diabetes Metab. Syndr. 2019, 13, 2481–2487. [Google Scholar] [CrossRef]
- Tzamaloukas, A.H.; Ing, T.S.; Siamopoulos, K.C.; Rohrscheib, M.; Elisaf, M.S.; Raj, D.S.; Murata, G.H. Body fluid abnormalities in severe hyperglycemia in patients on chronic dialysis: Review of published reports. J. Diabetes Its Complicat. 2008, 22, 29–37. [Google Scholar] [CrossRef]
- Galindo, R.J.; Pasquel, F.J.; Fayfman, M.; Tsegka, K.; Dhruv, N.; Cardona, S.; Wang, H.; Vellanki, P.; Umpierrez, G.E. Clinical characteristics and outcomes of patients with end-stage renal disease hospitalized with diabetes ketoacidosis. BMJ Open Diabetes Res. Care 2020, 8, e000763. [Google Scholar] [CrossRef]
- Tzamaloukas, A.H.; Ing, T.S.; Siamopoulos, K.C.; Raj, D.S.; Elisaf, M.S.; Rohrscheib, M.; Murata, G.H. Pathophysiology and management of fluid and electrolyte disturbances in patients on chronic dialysis with severe hyperglycemia. Semin. Dial. 2008, 21, 431–439. [Google Scholar] [CrossRef]
- Mathuram Thiyagarajan, U.; Ponnuswamy, A.; Chung, A. An enigmatic triad of acute pancreatitis, diabetic ketoacidosis and hypertriglyceridaemia: Who is the culprit? BMJ Case Rep. 2019, 12, e217272. [Google Scholar] [CrossRef]
- Scherer, J.; Singh, V.P.; Pitchumoni, C.S.; Yadav, D. Issues in hypertriglyceridemic pancreatitis: An update. J. Clin. Gastroenterol. 2014, 48, 195–203. [Google Scholar] [CrossRef]
- Wang, Y.; Attar, B.M.; Hinami, K.; Jaiswal, P.; Yap, J.E.; Jaiswal, R.; Devani, K.; Simons-Linares, C.R.; Demetria, M.V. Concurrent Diabetic Ketoacidosis in Hypertriglyceridemia-Induced Pancreatitis: How Does It Affect the Clinical Course and Severity Scores? Pancreas 2017, 46, 1336–1340. [Google Scholar] [CrossRef]
- Nair, S.; Yadav, D.; Pitchumoni, C.S. Association of diabetic ketoacidosis and acute pancreatitis: Observations in 100 consecutive episodes of DKA. Am. J. Gastroenterol. 2000, 95, 2795–2800. [Google Scholar] [CrossRef] [PubMed]
- Singla, A.A.; Ting, F.; Singla, A. Acute pancreatitis secondary to diabetic ketoacidosis induced hypertriglyceridemia in a young adult with undiagnosed type 2 diabetes. JOP. J. Pancreas 2015, 16, 201–204. [Google Scholar] [CrossRef]
- Ravindran, D.; Mugunthan, R.S.R.; Shruthi, T.K.; Jayaraman, D. Severe diabetic ketoacidosis and autoimmune pancreatitis with SIRS in an adolescent with LRBA deficiency—A rare complication of a common primary immunodeficiency disease. J. Fam. Med. Prim. Care 2022, 11, 1552–1554. [Google Scholar] [CrossRef]
- Yilmaz-Yalcin, Y.; Bascil-Tutuncu, N.; Baysan-Cebi, H.P.; Verdi, H.; Erol, S.; Kaymaz, F.F.; Atac, F.B. A Lipotoxic Medium Decreases the Number of Lipid Droplets in beta Cells: One Possible Explanation of the beta-Cell Failure in Patients with Hyperlipidemia Receiving Tacrolimus. Exp. Clin. Transplant. epub before print. 2022. [Google Scholar] [CrossRef]
- Porrini, E.L.; Diaz, J.M.; Moreso, F.; Delgado Mallen, P.I.; Silva Torres, I.; Ibernon, M.; Bayes-Genis, B.; Benitez-Ruiz, R.; Lampreabe, I.; Lauzurrica, R.; et al. Clinical evolution of post-transplant diabetes mellitus. Nephrol. Dial. Transplant. 2016, 31, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Mazumder, M.A.; Gulati, S.; Narula, A.S.; Shehwar, D.; Mir, I.M. Tacrolimus-induced acute pancreatitis and diabetic ketoacidosis (DKA) in pediatric kidney transplant recipient. Pediatr. Transplant. 2022, 26, e14194. [Google Scholar] [CrossRef]
- Rickels, M.R.; Robertson, R.P. Pancreatic Islet Transplantation in Humans: Recent Progress and Future Directions. Endocr. Rev. 2019, 40, 631–668. [Google Scholar] [CrossRef]
- Rickels, M.R.; Stock, P.G.; de Koning, E.J.P.; Piemonti, L.; Pratschke, J.; Alejandro, R.; Bellin, M.D.; Berney, T.; Choudhary, P.; Johnson, P.R.; et al. Defining outcomes for beta-cell replacement therapy in the treatment of diabetes: A consensus report on the Igls criteria from the IPITA/EPITA opinion leaders workshop. Transpl. Int. 2018, 31, 343–352. [Google Scholar] [CrossRef]
- Hering, B.J.; Clarke, W.R.; Bridges, N.D.; Eggerman, T.L.; Alejandro, R.; Bellin, M.D.; Chaloner, K.; Czarniecki, C.W.; Goldstein, J.S.; Hunsicker, L.G.; et al. Phase 3 Trial of Transplantation of Human Islets in Type 1 Diabetes Complicated by Severe Hypoglycemia. Diabetes Care 2016, 39, 1230–1240. [Google Scholar] [CrossRef]
- Lyons, S.K.; Hermann, J.M.; Miller, K.M.; Hofer, S.E.; Foster, N.C.; Rami-Merhar, B.M.; Aleppo, G.; Seufert, J.; DiMeglio, L.A.; Danne, T.; et al. Use of Adjuvant Pharmacotherapy in Type 1 Diabetes: International Comparison of 49,996 Individuals in the Prospective Diabetes Follow-up and T1D Exchange Registries. Diabetes Care 2017, 40, e139–e140. [Google Scholar] [CrossRef]
- Sarafidis, P.; Loutradis, C.; Ferro, C.J.; Ortiz, A. SGLT-2 Inhibitors to Treat Hyponatremia Associated with SIADH: A Novel Indication? Am. J. Nephrol. 2020, 51, 553–555. [Google Scholar] [CrossRef] [PubMed]
- Loutradis, C.; Papadopoulou, E.; Angeloudi, E.; Karagiannis, A.; Sarafidis, P. The Beneficial Hemodynamic Actions of SGLT-2 Inhibitors beyond the Management of Hyperglycemia. Curr. Med. Chem. 2020, 27, 6682–6702. [Google Scholar] [CrossRef] [PubMed]
- Refardt, J.; Imber, C.; Sailer, C.O.; Jeanloz, N.; Potasso, L.; Kutz, A.; Widmer, A.; Urwyler, S.A.; Ebrahimi, F.; Vogt, D.R.; et al. A Randomized Trial of Empagliflozin to Increase Plasma Sodium Levels in Patients with the Syndrome of Inappropriate Antidiuresis. J. Am. Soc. Nephrol. 2020, 31, 615–624. [Google Scholar] [CrossRef]
- Yeoh, S.E.; Docherty, K.F.; Jhund, P.S.; Petrie, M.C.; Inzucchi, S.E.; Kober, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; et al. Relationship of Dapagliflozin with Serum Sodium: Findings From the DAPA-HF Trial. JACC Heart Fail. 2022, 10, 306–318. [Google Scholar] [CrossRef]
- Dhanasekaran, M.; Narayanan, S.; Mastoris, I.; Mehta, S. Canagliflozin-associated severe hyponatremia: A rare and potentially adverse effect? Endocrinol. Diabetes Metab. Case Rep. 2022, 2022, 21-0035. [Google Scholar] [CrossRef] [PubMed]
- Branco, A.; Fatima, R.; Liblik, K.; Jackson, R.; Payne, D.; El-Diasty, M. Euglycemic Diabetic Ketoacidosis Associated with Sodium-Glucose Cotransporter-2 Inhibitors After Cardiac Surgery: A Review of Current Literature. J. Cardiothorac. Vasc. Anesthesia 2022, 36, 3877–3886. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, W.; Sakaguchi, K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors. J. Diabetes Investig. 2016, 7, 135–138. [Google Scholar] [CrossRef]
- Teng, R.; Kurian, M.; Close, K.L.; Buse, J.B.; Peters, A.L.; Alexander, C.M. Comparison of Protocols to Reduce Diabetic Ketoacidosis in Patients with Type 1 Diabetes Prescribed a Sodium-Glucose Cotransporter 2 Inhibitor. Diabetes Spectr. 2021, 34, 42–51. [Google Scholar] [CrossRef]
- Goldenberg, R.M.; Gilbert, J.D.; Hramiak, I.M.; Woo, V.C.; Zinman, B. Sodium-glucose co-transporter inhibitors, their role in type 1 diabetes treatment and a risk mitigation strategy for preventing diabetic ketoacidosis: The STOP DKA Protocol. Diabetes Obes. Metab. 2019, 21, 2192–2202. [Google Scholar] [CrossRef]
- Klocker, A.A.; Phelan, H.; Twigg, S.M.; Craig, M.E. Blood beta-hydroxybutyrate vs. urine acetoacetate testing for the prevention and management of ketoacidosis in Type 1 diabetes: A systematic review. Diabet. Med. 2013, 30, 818–824. [Google Scholar] [CrossRef]
- Westcott, G.P.; Segal, A.R.; Mitri, J.; Brown, F.M. Prolonged glucosuria and relapse of diabetic ketoacidosis related to SGLT2-inhibitor therapy. Endocrinol. Diabetes Metab. 2020, 3, e00117. [Google Scholar] [CrossRef] [PubMed]
- Ekanayake, P.; Hupfeld, C.; Mudaliar, S. Sodium-Glucose Cotransporter Type 2 (SGLT-2) Inhibitors and Ketogenesis: The Good and the Bad. Curr. Diabetes Rep. 2020, 20, 74. [Google Scholar] [CrossRef] [PubMed]
- Blau, J.E.; Tella, S.H.; Taylor, S.I.; Rother, K.I. Ketoacidosis associated with SGLT2 inhibitor treatment: Analysis of FAERS data. Diabetes Res. Rev. 2017, 33, e2924. [Google Scholar] [CrossRef]
- Weissberg-Benchell, J.; Antisdel-Lomaglio, J.; Seshadri, R. Insulin pump therapy: A meta-analysis. Diabetes Care 2003, 26, 1079–1087. [Google Scholar] [CrossRef]
- Ramirez-Rincon, A.; Hincapie-Garcia, J.; Arango, C.M.; Aristizabal, N.; Castillo, E.; Hincapie, G.; Zapata, E.; Cuesta, D.P.; Delgado, M.; Abad, V.; et al. Clinical Outcomes after 1 Year of Augmented Insulin Pump Therapy in Patients with Diabetes in a Specialized Diabetes Center in Medellin, Colombia. Diabetes Technol. Ther. 2016, 18, 713–718. [Google Scholar] [CrossRef]
- Alshami, A.; Purewal, T.; Douedi, S.; Alazzawi, M.; Hossain, M.A.; Ong, R.; Sen, S.; Cheng, J.; Patel, S. Effect of Insulin Pump Use on Diabetic Ketoacidosis in Type 1 Diabetes Mellitus: A Matched Cohort Study. J. Clin. Med. 2021, 10, 898. [Google Scholar] [CrossRef] [PubMed]
- Evans, K. Diabetic ketoacidosis: Update on management. Clin. Med. 2019, 19, 396–398. [Google Scholar] [CrossRef]
- Chee, Y.J.; Ng, S.J.H.; Yeoh, E. Diabetic ketoacidosis precipitated by COVID-19 in a patient with newly diagnosed diabetes mellitus. Diabetes Res. Clin. Pract. 2020, 164, 108166. [Google Scholar] [CrossRef]
- Kazakou, P.; Paschou, S.A.; Psaltopoulou, T.; Gavriatopoulou, M.; Korompoki, E.; Stefanaki, K.; Kanouta, F.; Kassi, G.N.; Dimopoulos, M.A.; Mitrakou, A. Early and late endocrine complications of COVID-19. Endocr. Connect. 2021, 10, R229–R239. [Google Scholar] [CrossRef]
- Li, J.; Wang, X.; Chen, J.; Zuo, X.; Zhang, H.; Deng, A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes. Metab. 2020, 22, 1935–1941. [Google Scholar] [CrossRef]
- Alhumaid, S.; Al Mutair, A.; Al Alawi, Z.; Rabaan, A.A.; Alomari, M.A.; Al Salman, S.A.; Al-Alawi, A.S.; Al Hassan, M.H.; Alhamad, H.; Al-Kamees, M.A.; et al. Diabetic ketoacidosis in patients with SARS-CoV-2: A systematic review and meta-analysis. Diabetol. Metab. Syndr. 2021, 13, 120. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhao, B.; Qu, Y.; Chen, Y.; Xiong, J.; Feng, Y.; Men, D.; Huang, Q.; Liu, Y.; Yang, B.; et al. Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated with Drastically Elevated Interleukin 6 Level in Critically Ill Patients with Coronavirus Disease 2019. Clin. Infect. Dis. 2020, 71, 1937–1942. [Google Scholar] [CrossRef] [PubMed]
- Stentz, F.B.; Umpierrez, G.E.; Cuervo, R.; Kitabchi, A.E. Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises. Diabetes 2004, 53, 2079–2086. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).