Assessing Short- and Medium-Term Outcomes of Lung Transplantation in Elderly Recipients: A Comparative Age-Based Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Conception
2.2. Preoperative Evaluation
2.3. Surgical Approach and Postoperative Management
2.4. Statical Analysis
3. Results
3.1. Patient Characteristics
3.2. Surgical and Perioperative Outcomes
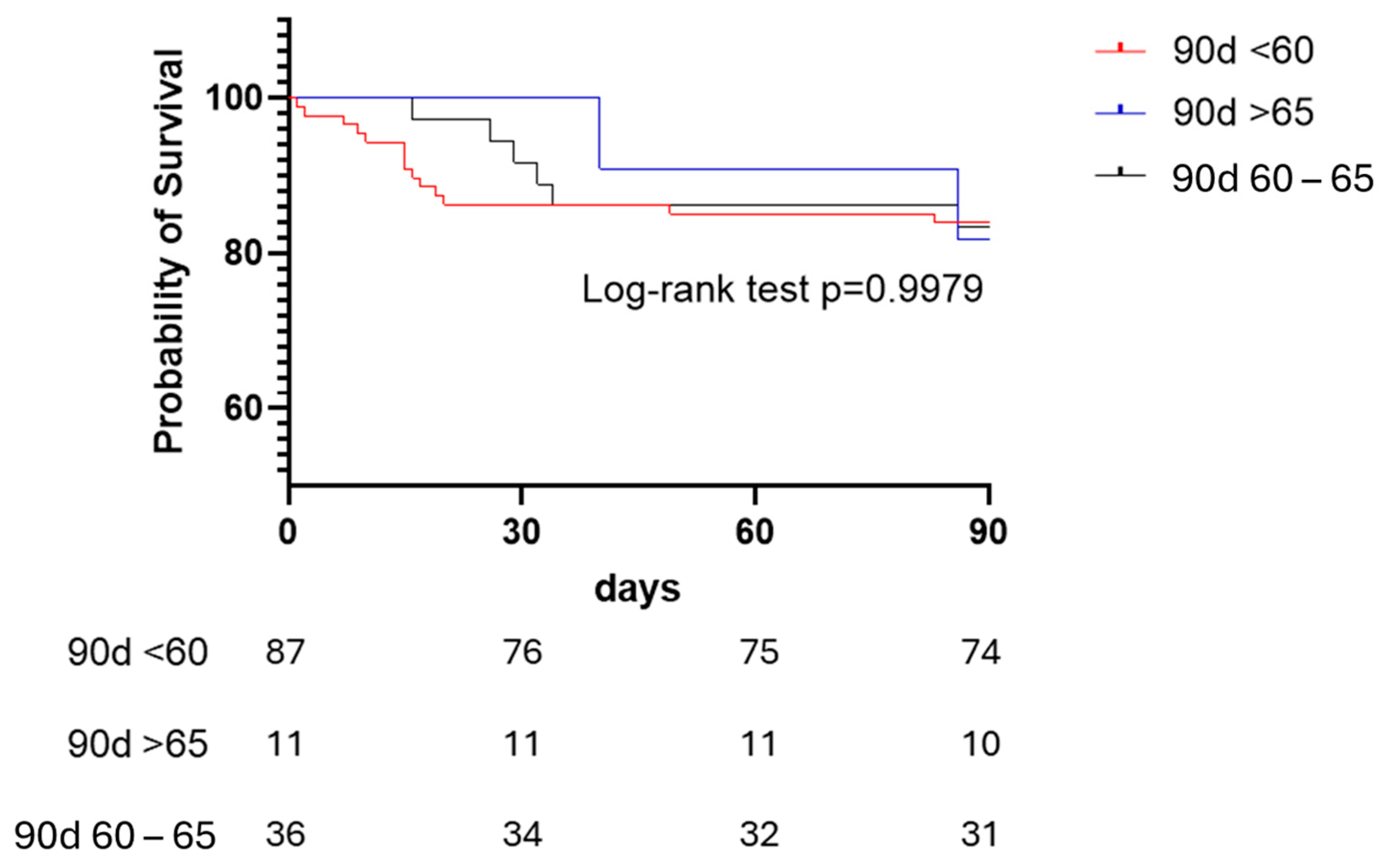
3.3. Survival and Outcome Correlation Analysis
4. Discussion
4.1. Age Difference, Disease Differences
4.2. Bilateral vs. Single Lung Transplant
4.3. Perioperative Complications, Recovery and Graft Survival
4.4. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ICU | Intensive Care Unit |
| IPF | Idiopathic Pulmonary Fibrosis |
| CLAD | Chronic Lung Allograft Dysfunction |
| COPD | Chronic Obstructive Pulmonary Disease |
| ECMO | Extracorporeal Membrane Oxygenation |
| OS | Overall Survival |
| PGD | Primary Graft Dysfunction |
| RRT | Renal Replacement Therapy |
References
- Courtwright, A.; Cantu, E. Lung transplantation in elderly patients. J. Thorac. Dis. 2017, 9, 3346–3351. [Google Scholar] [CrossRef] [PubMed]
- Orens, J.B.; Estenne, M.; Arcasoy, S.; Conte, J.V.; Corris, P.; Egan, J.J.; Egan, T.; Keshavjee, S.; Knoop, C.; Kotloff, R.; et al. International guidelines for the selection of lung transplant candidates: 2006 update—A consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2006, 25, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Valapour, M.; Lehr, C.J.; Schladt, D.P.; Smith, J.M.; Swanner, K.; Weibel, C.J.; Weiss, S.; Snyder, J.J. OPTN/SRTR 2022 Annual Data Report: Lung. Am. J. Transplant. 2024, 24 (Suppl. 1), S394–S456. [Google Scholar] [CrossRef]
- Leard, L.E.; Holm, A.M.; Valapour, M.; Glanville, A.R.; Attawar, S.; Aversa, M.; Campos, S.V.; Christon, L.M.; Cypel, M.; Dellgren, G.; et al. Consensus document for the selection of lung transplant candidates: An update from the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2021, 40, 1349–1379. [Google Scholar] [CrossRef]
- Catelli, C.; D’Alessandro, M.; Lloret Madrid, A.; Fossi, A.; Franchi, F.; Bennett, D.; Paladini, P.; Bargagli, E.; Luzzi, L. Donor-Recipient Mismatch in Lung Transplantation: The Role of Graft Sizing in Clinical Outcomes. Transpl. Int. 2025, 38, 14387. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Weingarten, N.; Mehta, A.C.; Budev, M.; Ahmad, U.; Yun, J.; McCurry, K.; Elgharably, H. Single vs Double Lung Transplantation in Older Adults: A Propensity-Matched Analysis. Chest 2025, 167, 518–528. [Google Scholar] [CrossRef] [PubMed]
- Ehrsam, J.P.; Benden, C.; Seifert, B.; Opitz, I.; Schneiter, D.; Weder, W.; Inci, I. Lung transplantation in the elderly: Influence of age, comorbidities, underlying disease, and extended criteria donor lungs. J. Thorac. Cardiovasc. Surg. 2017, 154, 2135–2141. [Google Scholar] [CrossRef]
- Faccioli, E.; Terzi, S.; Pangoni, A.; Lomangino, I.; Rossi, S.; Lloret, A.; Cannone, G.; Marino, C.; Catelli, C.; Dell’AMore, A. Extracorporeal membrane oxygenation in lung transplantation: Indications, techniques and results. World J. Transplant. 2021, 11, 290–302. [Google Scholar] [CrossRef]
- Tseng, S.C.; Gagne, S.M.; Hatabu, H.; Lin, G.; Sholl, L.M.; Nishino, M. Lung Cancer in Lung Transplant Recipients: Clinical, Radiologic, and Pathologic Characteristics and Treatment Outcome. J. Comput. Assist. Tomogr. 2023, 47, 590–597. [Google Scholar] [CrossRef]
- Catelli, C.; Faccioli, E.; Silvestrin, S.; Lorenzoni, G.; Luzzi, L.; Bennett, D.; Schiavon, M.; Campisi, A.; Bargagli, E.; Dell’amore, A.; et al. Lung Transplantation in Patients with Previous or Unknown Oncological Disease: Evaluation of Short- and Long-Term Outcomes. Cancers 2024, 16, 538. [Google Scholar] [CrossRef]
- Bisson, A.; Bonnette, P. A new technique for double lung transplantation. “Bilateral single lung” transplantation. J. Thorac. Cardiovasc. Surg. 1992, 103, 40–46. [Google Scholar] [CrossRef]
- Avramenko, A.; Etienne, H.; Weisenburger, G.; Mullaert, J.; Cerceau, P.; Pellenc, Q.; Roussel, A.; Morer, L.; Bunel, V.; Montravers, P.; et al. How safe is lung transplantation in patients of 65 years or older? A single-center retrospective cohort. Respir. Med. Res. 2024, 86, 101139. [Google Scholar] [CrossRef]
- Kuntz, C.L.; Hadjiliadis, D.; Ahya, V.N.; Kotloff, R.M.; Pochettino, A.; Lewis, J.; Christie, J.D. Risk factors for early primary graft dysfunction after lung transplantation: A registry study. Clin. Transplant. 2009, 23, 819–830. [Google Scholar] [CrossRef]
- Puri, V.; Patterson, G.A.; Meyers, B.F. Single versus bilateral lung transplantation: Do guidelines exist? Thorac. Surg. Clin. 2015, 25, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Munson, J.C.; Christie, J.D.; Halpern, S.D. The societal impact of single versus bilateral lung transplantation for chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2011, 184, 1282–1288. [Google Scholar] [CrossRef] [PubMed]
- Gulack, B.C.; Ganapathi, A.M.; Speicher, P.J.; Meza, J.M.; Hirji, S.A.; Snyder, L.D.; Davis, R.D.; Hartwig, M.G. What Is the Optimal Transplant for Older Patients With Idiopathic Pulmonary Fibrosis? Ann. Thorac. Surg. 2015, 100, 1826–1833. [Google Scholar] [CrossRef]
- Villavicencio, M.A.; Axtell, A.L.; Osho, A.; Astor, T.; Roy, N.; Melnitchouk, S.; D’aLessandro, D.; Tolis, G.; Raz, Y.; Neuringer, I.; et al. Single- Versus Double-Lung Transplantation in Pulmonary Fibrosis: Impact of Age and Pulmonary Hypertension. Ann. Thorac. Surg. 2018, 106, 856–863. [Google Scholar] [CrossRef]
- Gerbase, M.W.; Spiliopoulos, A.; Rochat, T.; Archinard, M.; Nicod, L.P. Health-related quality of life following single or bilateral lung transplantation: A 7-year comparison to functional outcome. Chest 2005, 128, 1371–1378. [Google Scholar] [CrossRef]
- Hadjiliadis, D.; Davis, R.D.; Palmer, S.M. Is transplant operation important in determining posttransplant risk of bronchiolitis obliterans syndrome in lung transplant recipients? Chest 2002, 122, 1168–1175. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, M.P.; Meyers, B.F. Bilateral versus single lung transplantation: Are two lungs better than one? J. Thorac. Dis. 2018, 10, 4588–4601. [Google Scholar] [CrossRef]
- Wilson, M.E.; Vakil, A.P.; Kandel, P.; Undavalli, C.; Dunlay, S.M.; Kennedy, C.C. Pretransplant frailty is associated with decreased survival after lung transplantation. J. Heart Lung Transplant. 2016, 35, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Hayanga, A.J.; Aboagye, J.K.; Hayanga, H.E.; Morrell, M.; Huffman, L.; Shigemura, N.; Bhama, J.K.; D’Cunha, J.; Bermudez, C.A. Contemporary analysis of early outcomes after lung transplantation in the elderly using a national registry. J. Heart Lung Transplant. 2015, 34, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Biswas Roy, S.; Alarcon, D.; Walia, R.; Chapple, K.M.; Bremner, R.M.; Smith, M.A. Is There an Age Limit to Lung Transplantation? Ann. Thorac. Surg. 2015, 100, 443–451. [Google Scholar] [CrossRef]
- Henricksen, E.J.; Wayda, B.; Teuteberg, J.J.; Luikart, H.; Njoroge, J.; Guenthart, B.A.; Khush, K.K. Trends in heart transplant outcomes for patients over the age of 70 years in the United States: An analysis of the scientific registry of transplant recipients database. J. Heart Lung Transplant. 2025, 44, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Zhou, A.L.; Karius, A.K.; Ruck, J.M.; Shou, B.L.; Larson, E.L.; Casillan, A.J.; Ha, J.S.; Shah, P.D.; Merlo, C.A.; Bush, E.L. Outcomes of Lung Transplant Candidates Aged ≥70 Years During the Lung Allocation Score Era. Ann. Thorac. Surg. 2024, 117, 725–732. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Variables | Group Y (<60) (n = 88) | Group M (60–65) (n = 36) | Group O (>65) (n = 11) | p Value |
|---|---|---|---|---|
| Age (years) | 47.0 (10.4) | 62.3 (1.6) | 65.5 (0.4) | <0.001 |
| Male sex, n (%) | 50 (56.8%) | 25 (69.4%) | 8 (72.7%) | 0.307 |
| End-stage disease, n (%) | <0.001 | |||
| IPF | 19 (22%) | 18 (50%) | 9 (82%) | |
| COPD | 14 (16%) | 11 (30%) | 2 (18%) | |
| Cystic Fibrosis | 24 (27%) | 0 (0%) | 0 (0%) | |
| Other | 31 (35%) | 7 (19%) | 0 (0%) | |
| Body Mass Index, kg/m2 | 23.1 (4.5) | 26.1 (4.5) | 24.5 (4.1) | 0.008 |
| Smoker | 38 (43%) | 25 (69%) | 9 (82%) | 0.003 |
| Comorbidities, n (%) | ||||
| Cardiopathy | 7 (8%) | 3 (8%) | 2 (18%) | 0.650 |
| Dyslipidemia | 20 (23%) | 18 (50%) | 4 (36%) | <0.001 |
| Arterial Hypertension | 25 (28%) | 14 (39%) | 6 (55%) | 0.158 |
| Osteoporosis | 56 (64%) | 18 (50%) | 10 (91%) | 0.123 |
| Diabetes | 37 (42%) | 8 (17%) | 3 (27%) | 0.025 |
| Pulmonary hypertension | 16 (18%) | 16 (44%) | 2 (18%) | 0.005 |
| MV/ECMO bridge n (%) | 19 (22%) | 0 (0%) | 0 (%) | 0.003 |
| Admitted before transplant, n (%) | 24 (27%) | 1 (3%) | 0 (0%) | 0.002 |
| Time on waiting list (days) | 356 (410) | 382 (408) | 294 (202) | 0.516 |
| Variables | Group Y (<60) (n = 88) | Group M (60–65) (n = 36) | Group O (>65) (n = 11) | p Value |
|---|---|---|---|---|
| Bilateral transplant | 80 (91%) | 22 (61%) | 4 (36%) | <0.001 |
| Minimum ischemia time (min) | 302 (130) | 284 (89) | 236 (76) | 0.280 |
| Maximum ischemia time (min) | 425 (161) | 350 (120) | 315 (140) | 0.048 |
| In-hospital stay (day) | 48 (47) | 40 (18) | 44 (25) | 0.900 |
| ICU stay (days) | 18 (18) | 13 (12) | 15 (17) | 0.290 |
| CRRT | 20 (23%) | 4 (11%) | 2 (18%) | 0.358 |
| PGD | 0.869 | |||
| 0 | 21 (24%) | 8 (22%) | 3 (27%) | |
| 1 | 20 (22%) | 6 (17%) | 1 (9%) | |
| 2 | 21 (24%) | 12 (33%) | 4 (36%) | |
| 3 | 26 (29%) | 10 (28%) | 3 (27%) | |
| Tracheostomy | 29 (33%) | 11 (31%) | 2 (18%) | 0.609 |
| CLAD development | 29 (33%) | 16 (44%) | 3 (27%) | 0.400 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Catelli, C.; Lloret Madrid, A.; Bennett, D.; D’Alessandro, M.; Guerrieri, M.; Rizzo, M.; Marianello, D.; Fossi, A.; Paladini, P.; Bargagli, E.; et al. Assessing Short- and Medium-Term Outcomes of Lung Transplantation in Elderly Recipients: A Comparative Age-Based Analysis. Transplantology 2025, 6, 28. https://doi.org/10.3390/transplantology6030028
Catelli C, Lloret Madrid A, Bennett D, D’Alessandro M, Guerrieri M, Rizzo M, Marianello D, Fossi A, Paladini P, Bargagli E, et al. Assessing Short- and Medium-Term Outcomes of Lung Transplantation in Elderly Recipients: A Comparative Age-Based Analysis. Transplantology. 2025; 6(3):28. https://doi.org/10.3390/transplantology6030028
Chicago/Turabian StyleCatelli, Chiara, Andrea Lloret Madrid, David Bennett, Miriana D’Alessandro, Marco Guerrieri, Marianna Rizzo, Daniele Marianello, Antonella Fossi, Piero Paladini, Elena Bargagli, and et al. 2025. "Assessing Short- and Medium-Term Outcomes of Lung Transplantation in Elderly Recipients: A Comparative Age-Based Analysis" Transplantology 6, no. 3: 28. https://doi.org/10.3390/transplantology6030028
APA StyleCatelli, C., Lloret Madrid, A., Bennett, D., D’Alessandro, M., Guerrieri, M., Rizzo, M., Marianello, D., Fossi, A., Paladini, P., Bargagli, E., & Luzzi, L. (2025). Assessing Short- and Medium-Term Outcomes of Lung Transplantation in Elderly Recipients: A Comparative Age-Based Analysis. Transplantology, 6(3), 28. https://doi.org/10.3390/transplantology6030028








