Assessment of In-Hospital Pain Control after Childbirth and Its Correlation with Anxiety in the Postpartum Period: A Cross-Sectional Study at a Single Center in the USA
Abstract
1. Introduction
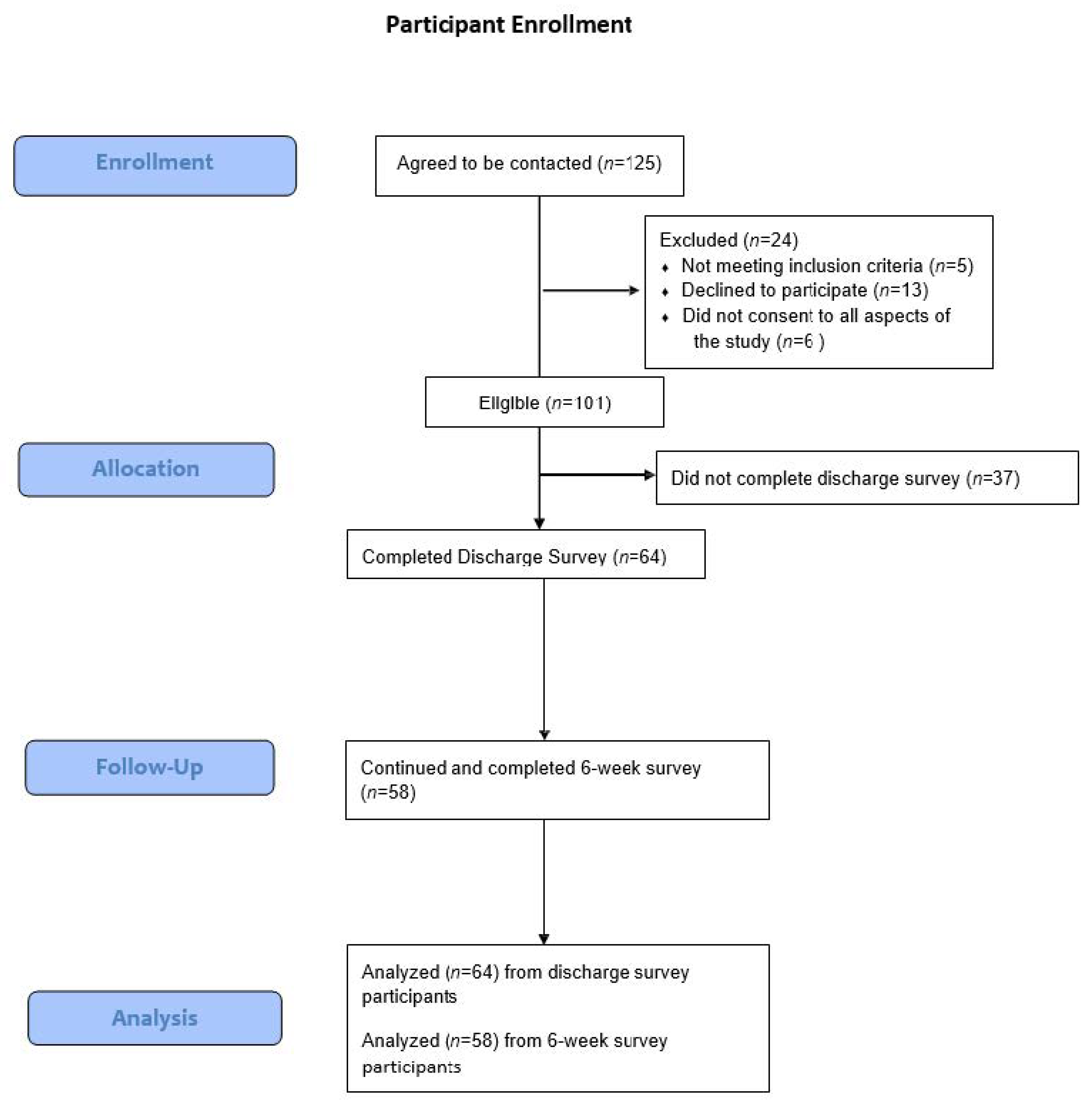
2. Materials and Methods
Statistical Analysis
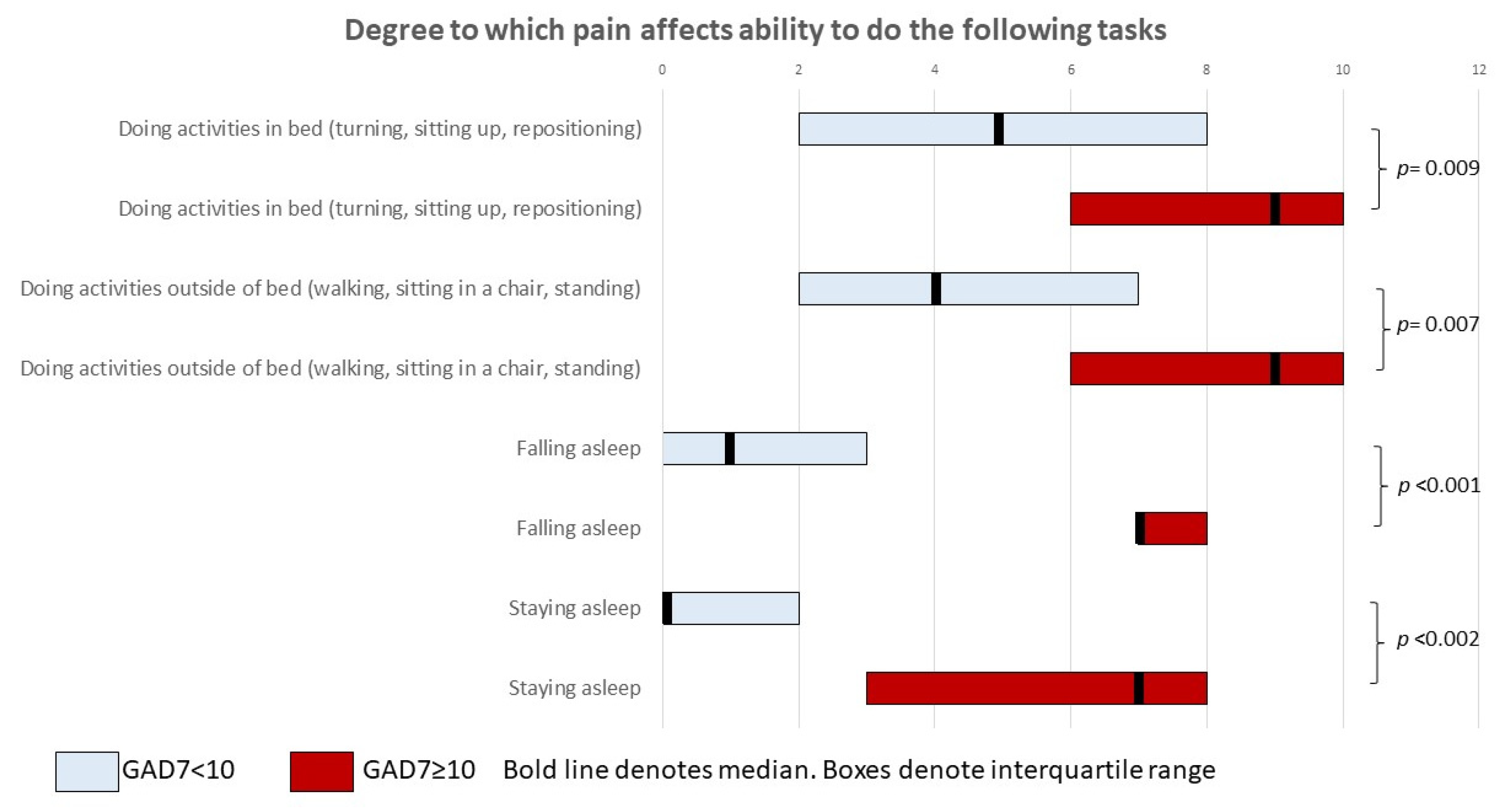
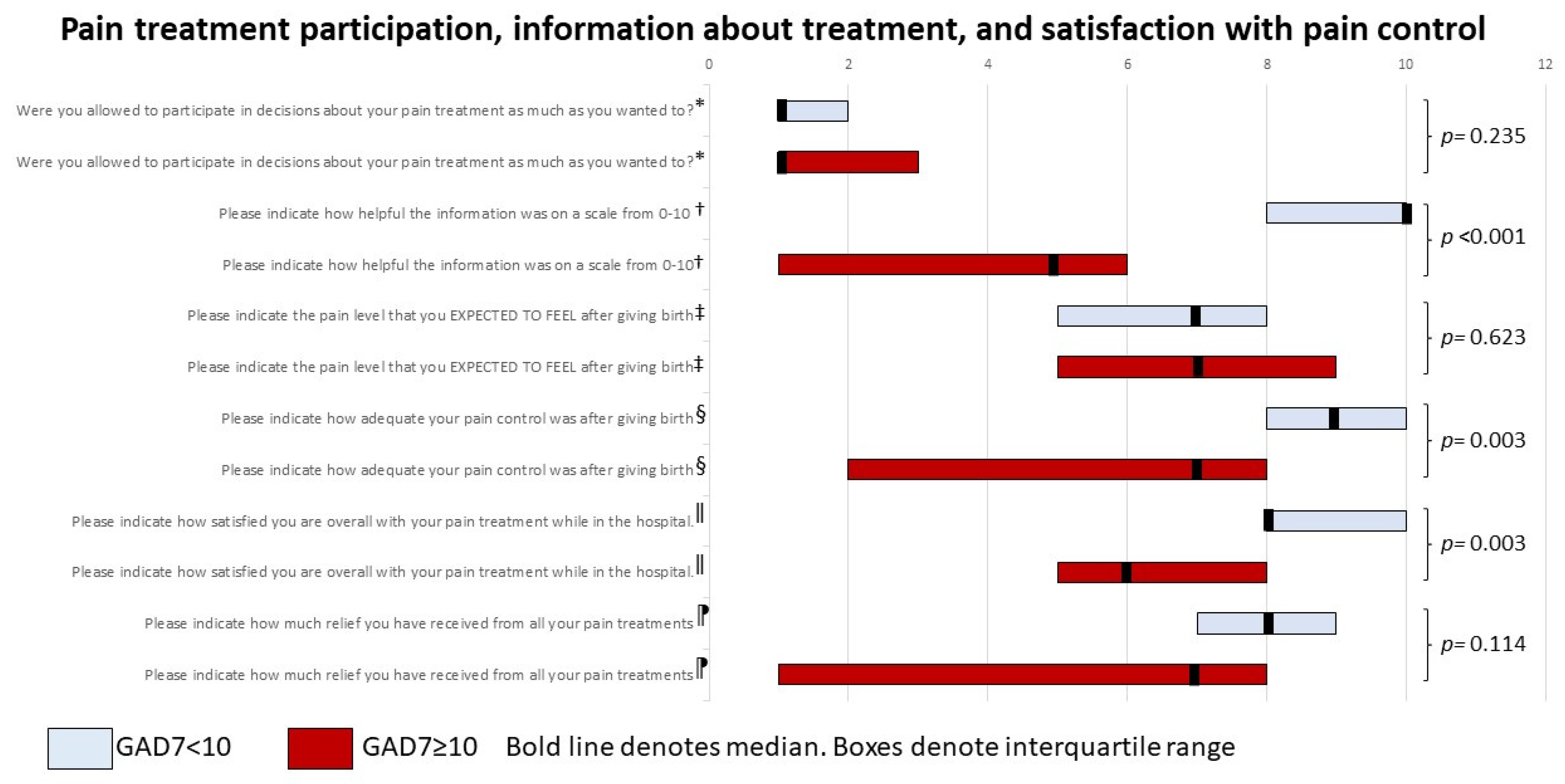
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bandelow, B.; Michaelis, S. Epidemiology of anxiety disorders in the 21st century. Dialog Clin. Neurosci. 2015, 17, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Radua, J.; Olivola, M.; Croce, E.; Soardo, L.; de Pablo, G.S.; Shin, J.I.; Kirkbride, J.B.; Jones, P.; Kim, J.H.; et al. Age at onset of mental disorders worldwide: Large-scale meta-analysis of 192 epidemiological studies. Mol. Psychiatry 2021, 27, 281–295. [Google Scholar] [CrossRef] [PubMed]
- Xiong, P.T.; Poehlmann, J.; Stowe, Z.N.; Antony, K.M. Anxiety, Depression, and Pain in the Perinatal Period: A Review for Obstetric Care Providers. Obstet. Gynecol. Surv. 2021, 76, 692–713. [Google Scholar] [CrossRef] [PubMed]
- Reck, C.; Noe, D.; Gerstenlauer, J.; Stehle, E. Effects of postpartum anxiety disorders and depression on maternal self-confidence. Infant Behav. Dev. 2012, 35, 264–272. [Google Scholar] [CrossRef]
- Field, T. Postnatal anxiety prevalence, predictors and effects on development: A narrative review. Infant Behav. Dev. 2018, 51, 24–32. [Google Scholar] [CrossRef]
- Ma, J.E.S.; Brack, G.A.; DiIorio, C. Prevalence and Predictors of Women’s Experience of Psychological Trauma During Childbirth. Birth 2003, 30, 36–46. [Google Scholar] [CrossRef]
- Qu, F.; Zhou, J. Electro-Acupuncture in Relieving Labor Pain. Evidence-Based Complement. Altern. Med. 2007, 4, 125–130. [Google Scholar] [CrossRef]
- Eisenach, J.C.; Pan, P.H.; Smiley, R.; Lavand’Homme, P.; Landau, R.; Houle, T. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain 2008, 140, 87–94. [Google Scholar] [CrossRef]
- Tzeng, Y.-L.; Yang, Y.-L.; Kuo, P.-C.; Lin, Y.-C.; Chen, S.-L. Pain, Anxiety, and Fatigue During Labor: A Prospective, Repeated Measures Study. J. Nurs. Res. 2017, 25, 59–67. [Google Scholar] [CrossRef]
- Goodman, J.H.; Watson, G.R.; Stubbs, B. Anxiety disorders in postpartum women: A systematic review and meta-analysis. J. Affect. Disord. 2016, 203, 292–331. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- McNeill, J.A.; Sherwood, G.D.; Starck, P.L.; Thompson, C.J. Assessing Clinical Outcomes: Patient Satisfaction with Pain Management. J. Pain Symptom Manag. 1998, 16, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Max, M.B.; Donovan, M.I.; Miaskowski, C.A.; Ward, S.E.; Gordon, D.B.; Bookbinder, M.; Cleeland, C.S.; Coyle, N.; Kiss, M.E.; Thaler, H.T.; et al. Quality Improvement Guidelines for the Treatment of Acute Pain and Cancer Pain. JAMA 1995, 274, 1874–1880. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Kupfer, D.J. Anxiety and DSM-5. Dialog Clin. Neurosci. 2015, 17, 245–246. [Google Scholar] [CrossRef]
- Pettersson, F.D.; Hellgren, C.; Nyberg, F.; Åkerud, H.; Sundström-Poromaa, I. Depressed mood, anxiety, and the use of labor analgesia. Arch. Women’s Ment. Health 2015, 19, 11–16. [Google Scholar] [CrossRef]
- Curzik, D.; Jokic-Begic, N. Anxiety sensitivity and anxiety as correlates of expected, experienced and recalled labor pain. J. Psychosom. Obstet. Gynecol. 2011, 32, 198–203. [Google Scholar] [CrossRef]
- Gorkem, U.; Togrul, C.; Şahiner, Y.; Yazla, E.; Gungor, T. Preoperative anxiety may increase post-cesarean delivery pain and analgesic consumption. Minerva Anestesiol. 2016, 82, 974–980. [Google Scholar]
- Bell, A.F.; Carter, C.S.; Davis, J.M.; Golding, J.; Adejumo, O.; Pyra, M.; Connelly, J.J.; Rubin, L.H. Childbirth and symptoms of postpartum depression and anxiety: A prospective birth cohort study. Arch. Women’s Ment. Health 2015, 19, 219–227. [Google Scholar] [CrossRef]
- Floris, L.; Irion, O. Association between anxiety and pain in the latent phase of labour upon admission to the maternity hospital: A prospective, descriptive study. J. Health Psychol. 2013, 20, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Poehlmann, J.R.; Stowe, Z.N.; Godecker, A.; Xiong, P.T.; Broman, A.T.; Antony, K.M. The impact of preexisting maternal anxiety on pain and opioid use following cesarean delivery: A retrospective cohort study. Am. J. Obstet. Gynecol. MFM 2022, 4, 100576. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, E.S.; Gibbons, R.D.; O’Hara, M.W.; Duffecy, J.; Maki, P.M. Depression and anxiety symptoms across pregnancy and the postpartum in low-income Black and Latina women. Arch. Women’s Ment. Health 2021, 24, 979–986. [Google Scholar] [CrossRef]
- Poehlmann, J.R.; Avery, G.; Antony, K.M.; Broman, A.T.; Godecker, A.; Green, T.L. Racial disparities in post-operative pain experience and treatment following cesarean birth. J. Matern. Neonatal Med. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Soares, A.D.S.; Couceiro, T.C.D.M.; Lima, L.C.; Flores, F.L.L.; Alcoforado, E.M.B.; Filho, R.D.O.C. Association of Pain Catastrophizing with the Incidence and Severity of Acute and Persistent Perineal Pain after Natural Childbirth: Longitudinal Cohort Study. Braz. J. Anesthesiol. 2013, 63, 317–321. [Google Scholar] [CrossRef]
- Kuciel, N.; Sutkowska, E.; Biernat, K.; Hap, K.; Mazurek, J.; Demczyszak, I. Assessment of the level of anxiety and pain in women who do and do not attend childbirth classes during the SARS-CoV-2 pandemic. Risk Manag. Health Policy 2021, 14, 4489–4497. [Google Scholar] [CrossRef]
- Guszkowska, M. The effect of exercise and childbirth classes on fear of childbirth and locus of labor pain control. Anxiety Stress Coping 2013, 27, 176–189. [Google Scholar] [CrossRef]
- Russell, P.D.; Judkins, J.L.; Blessing, A.; Moore, B.; Morissette, S.B. Incidences of anxiety disorders among active duty service members between 1999 and 2018. J. Anxiety Disord. 2022, 91, 102608. [Google Scholar] [CrossRef]
- Ravangard, R.; Basiri, A.; Sajjadnia, Z.; Shokrpour, N. Comparison of the Effects of Using Physiological Methods and Accompanying a Doula in Deliveries on Nulliparous Women’s Anxiety and Pain. Health Care Manag. 2017, 36, 372–379. [Google Scholar] [CrossRef]
- Buglione, A.; Saccone, G.; Mas, M.; Raffone, A.; Di Meglio, L.; di Meglio, L.; Toscano, P.; Travaglino, A.; Zapparella, R.; Duval, M.; et al. Effect of music on labor and delivery in nulliparous singleton pregnancies: A randomized clinical trial. Arch. Gynecol. Obstet. 2020, 301, 693–698. [Google Scholar] [CrossRef]
- Smith, C.A.; Levett, K.M.; Collins, C.T.; Armour, M.; Dahlen, H.G.; Suganuma, M. Relaxation techniques for pain management in labour. Cochrane Database Syst. Rev. 2018, 2018, CD009514. [Google Scholar] [CrossRef]
- Elden, H.; Gutke, A.; Kjellby-Wendt, G.; Fagevik-Olsen, M.; Ostgaard, H.-C. Predictors and consequences of long-term pregnancy-related pelvic girdle pain: A longitudinal follow-up study. BMC Musculoskelet. Disord. 2016, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Floris, L.; Irion, O.; Courvoisier, D. Influence of obstetrical events on satisfaction and anxiety during childbirth: A prospective longitudinal study. Psychol. Health Med. 2017, 22, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Austin, M.-P.; Tully, L.; Parker, G. Examining the relationship between antenatal anxiety and postnatal depression. J. Affect. Disord. 2007, 101, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Rousseau, S.; Katz, D.; Shlomi-Polachek, I.; Frenkel, T.I. Prospective risk from prenatal anxiety to post traumatic stress following childbirth: The mediating effects of acute stress assessed during the postnatal hospital stay and preliminary evidence for moderating effects of doula care. Midwifery 2021, 103, 103143. [Google Scholar] [CrossRef]
| Characteristic | GAD-7 < 10 (n = 57) | GAD-7 ≥ 10 (n = 7) | p-Value * | |
|---|---|---|---|---|
| Age, mean (SD) | 32.4 (3.3) | 33.9 (4.1) | 0.281 | |
| Race/Ethnicity, n (%) | Non-Hispanic White | 53 (93.0) | 5 (71.4) | 0.065 |
| Non-Hispanic Black or African American | 0 (0) | 0 (0) | ||
| Asian American | 4 (7.0) | 2 (28.6) | ||
| Latinx | 0 (0) | 0 (0) | ||
| Other/unknown | 0 (0) | 0 (0) | ||
| Married or partnered, n (%) | 54 (94.7) | 7 (100.0) | 0.534 | |
| Insurance, n (%) | Private insurance | 56 (98.2) | 5 (71.4) | <0.001 |
| Medicaid | 1 (1.8) | 0 (0) | ||
| Tricare | 0 (0) | 2 (28.6) | ||
| Education, n (%) | Less than high school | 0 (0) | 0 (0) | 0.810 |
| High school education | 1 (1.75) | 0 (0) | ||
| Some college | 3 (5.26) | 0 (0) | ||
| College degree | 3 (5.26) | 0 (0) | ||
| Masters degree or higher | 50 (87.7) | 7 (100) | ||
| Parity, n (%) | Primiparous | 31 (54.4) | 4 (57.1) | 0.890 |
| Multiparous | 26 (45.6) | 3 (42.9) | ||
| Prior miscarriage or abortion, n (%) | 12 (21.1) | 2 (28.6) | 0.650 | |
| Pre-pregnancy maternal BMI †, mean ± SD | 30.1 (6.2) | 33.2 (8.2) | 0.227 | |
| Tobacco use, n (%) | 0 (0) | 0 (0) | NA | |
| Mood disorders, n (%) | Anxiety | 8 (14.0) | 1 (14.3) | 0.730 |
| Depression | 3 (5.3) | 0 (0) | ||
| Anxiety and depression | 8 (14.0) | 2 (28.6) | ||
| Neither | 38 (66.7) | 4 (57.1) | ||
| Delivery Characteristics | GAD-7 < 10 (n = 57) | GAD-7 ≥ 10 (n = 7) | p-Value * | |
|---|---|---|---|---|
| Mode of delivery, n (%) | Vaginal | 34 (59.7) | 1 (14.3) | 0.053 |
| Vacuum | 1 (1.8) | 1 (14.3) | ||
| Forceps | 0 (0) | 0 (0) | ||
| Scheduled cesarean | 9 (15.8) | 2 (28.6) | ||
| Urgent cesarean | 12 (21.1) | 2 (28.6) | ||
| Emergency cesarean | 1 (1.8) | 1 (14.3) | ||
| Cesarean birth analgesia, ‡ n (%) | Epidural | 9 (40.9) | 1 (20) | 0.552 |
| Spinal | 11 (50.0) | 3 (60.0) | ||
| Combined spinal/epidural | 1 (4.6) | 1 (20.0) | ||
| General anesthesia | 1 (4.6) | 0 (0) | ||
| Labor analgesia, n (%) | No pain medications | 3 (6.4) | 0 (0) | 0.055 |
| IV pain medications only | 2 (4.3) | 1 (25.0) | ||
| Epidural only | 28 (49.6) | 0 (0) | ||
| IV pain meds and epidural | 14 (29.8) | 3 (75.0) | ||
| Vaginal lacerations, ‡ n (%) | No laceration | 4 (11.4) | 0 (0) | 0.152 |
| 1st degree | 8 (22.9) | 0 (0) | ||
| 2nd degree | 21 (60.0) | 1 (50.0) | ||
| 3rd degree | 2 (5.7) | 1 (50.0) | ||
| 4th degree | 0 (0) | 0 (0) | ||
| Intraamniotic infection, n (%) | 1 (1.1) | 1 (14.3) | 0.015 | |
| Gestational age (weeks), mean (SD) | 39.0 (1.4) | 39.4 (0.8) | 0.399 | |
| Length of stay > 72 h, n (%) | 15 (26.32) | 5 (57.14) | 0.092 | |
| Preterm delivery, n (%) | 6 (10.5) | 0 (0) | 0.367 | |
| Fetal anomalies present, n (%) | 5 (8.8) | 0 (0) | 0.414 | |
| NICU § Admission, n (%) | 3 (5.4) | 0 (0) | 0.530 | |
| Variable | GAD-7 < 10 (n = 57) | GAD-7 ≥ 10 (n = 7) | p-Value * | |
|---|---|---|---|---|
| First 24 h post-delivery(n = 64) | Maximum pain score ≥ 7, n (%) * | 19 (33.3) | 5 (71.4) | 0.049 |
| % of time spent in severe pain, median (IQR) † | 10 (0–10) | 10 (10–60) | 0.007 | |
| 20% of time or more spent with severe pain, n (%) | 12 (21.0) | 3 (42.9) | 0.199 | |
| Lowest pain score ≤ 3, n (%) | 51 (89.5) | 3 (42.9) | 0.001 | |
| Second 24 h post-delivery | Maximum pain score ≥ 7, n (%) | 14 (24.6) | 5 (71.4) | 0.010 |
| % of time spent in severe pain, median (IQR) | 0 (0–10) | 10 (10–50) | 0.010 | |
| 20% of time or more spent with severe pain, n (%) | 10 (17.5) | 2 (28.6) | 0.481 | |
| Lowest pain score ≤ 3, n (%) | 54 (94.7) | 5 (71.4) | 0.030 | |
| Overall for hospitalization | Maximum pain score ≥ 7, n (%) | 24 (42.11) | 5 (71.43) | 0.141 |
| 20% of time or more spent with severe pain, n (%) | 15 (26.32) | 3 (42.86) | 0.358 | |
| Lowest pain score ≤ 3, n (%) | 56 (98.25) | 5 (71.43) | 0.002 | |
| Total doses of opioid medications, † | 0 (0–1) | 3 (0–17) | 0.022 | |
| Perceived adequacy of pain control, median (IQR) †‡ | 9 (8–10) | 7 (2–8) | 0.003 | |
| Satisfaction with pain control, median (IQR) †§ | 10 (8–10) | 6 (5–8) | 0.003 | |
| GAD-7 < 5 N = 44 | GAD-7 5–9 N = 13 | GAD-7 10–14 N = 5 | GAD-7 15–21 N = 2 | p | ||
|---|---|---|---|---|---|---|
| Any severe pain, n (%) | 17 (38.6) | 2 (15.4) | 3 (60.0) | 2 (100) | 0.067 | |
| First 24 hours postpartum | 20% of time or more spent with severe pain, n (%) | 10 (22.7) | 2 (15.4) | 2 (40.0) | 1 (50.0) | 0.566 |
| Lowest pain score ≤ 3, n(%) | 40 (90.9) | 11 (84.6) | 3 (60.0) | 0 (0) | 0.002 | |
| Any severe pain | 10 (22.7) | 4 (30.8) | 3 (60.0) | 2 (100.0) | 0.047 | |
| Second 24 hours postpartum | 20% of time or more spent with severe pain | 8 (18.2) | 2 (15.4) | 1 (20.0) | 1 (50.0) | 0.707 |
| Lowest pain score ≤ 3 | 42 (95.4) | 12 (92.3) | 4 (80.0) | 1 (50.0) | 0.085 |
| Characteristic | GAD-7 < 10 (n = 49) | GAD-7 ≥ 10 (n = 9) | p-Value * | |
|---|---|---|---|---|
| Age, mean (SD) | 32 (3.6) | 31.4 (2.8) | 0.366 | |
| Race/ethnicity, n (%) | Non-Hispanic White | 44 (89.8) | 8 (88.9) | 0.935 |
| Non-Hispanic Black or African American | 0 (0) | 0 (0) | ||
| Asian American | 5 (10.2) | 1 (11.1) | ||
| Latinx | 0 (0) | 0 (0) | ||
| Other/unknown | 0 (0) | 0 (0) | ||
| Married or partnered, n (%) | 47 (95.9) | 8 (88.9) | ||
| Insurance, n (%) | Private insurance | 47 (95.9) | 8 (88.9) | 0.361 |
| Medicaid | 1 (2.0) | 0 (0) | ||
| Tricare | 1 (2.0) | 1 (11.1) | ||
| Education, n (%) | Less than high school | 0 (0) | 0 (0) | 0.691 |
| High school education | 1 (2.0) | 0 (0) | ||
| Some college | 3 (6.10) | 0 (0) | ||
| College degree | 2 (4.1) | 1 (11.1) | ||
| Masters degree or higher | 43 (87.8) | 8 (88.9) | ||
| Parity, n (%) | Primiparous | 27 (55.1) | 5 (55.6) | 0.980 |
| Multiparous | 22 (44.9) | 4 (44.4) | ||
| Prior miscarriage or abortion, n (%) | 8 (18.4) | 2 (22.2) | 0.786 | |
| Pre-pregnancy maternal BMI †, mean ±SD | 30.7 (6.5) | 30.6 (7.6) | 0.947 | |
| Tobacco use, n (%) | 0 (0) | 0 (0) | NA | |
| Mood disorders, n (%) | Anxiety | 6 (12.2) | 2 (22.2) | 0.696 |
| Depression | 2 (4.1) | 0 (0) | ||
| Anxiety and depression | 7 (14.3) | 1 (22.2) | ||
| Neither | 34 (69.4) | 5 (55.6) | ||
| Mode of delivery, n (%) | Vaginal | 29 (59.2) | 4 (44.4) | 0.397 |
| Vacuum | 1 (2.0) | 1 (11.1) | ||
| Forceps | 0 (0) | 0 (0) | ||
| Scheduled cesarean | 8 (16.3) | 1 (11.1) | ||
| Urgent cesarean | 10 (20.4) | 2 (22.2) | ||
| Emergency cesarean | 1 (2.0) | 1 (11.1) | ||
| Cesarean birth analgesia, † n (%) | Epidural | 7 (36.8) | 1 (25.0) | 0.015 |
| Spinal | 11 (57.9) | 1 (25.0) | ||
| Combined spinal/epidural | 0 (0) | 2 (50.0) | ||
| General anesthesia | 1 (5.3) | 0 (0) | ||
| Labor analgesia, n (%) | No pain medications | 3 (7.5) | 0 (0) | 0.404 |
| IV pain medications only | 3 (7.5) | 0 (0) | ||
| Epidural only | 23 (57.5) | 3 (42.9) | ||
| IV pain meds and epidural | 11 (27.5) | 4 (57.1) | ||
| Vaginal lacerations, ‡ n (%) | No laceration | 3 (10.0) | 1 (20.0) | 0.285 |
| 1st degree | 8 (26.7) | 0 (0) | ||
| 2nd degree | 18 (60.0) | 3 (60.0) | ||
| 3rd degree | 1 (3.3) | 1 (20.0) | ||
| 4th degree | 0 (0) | 0 (0) | ||
| Intraamniotic infection, n (%) | 2 (4.1) | 0 (0) | 0.748 | |
| Gestational age (weeks), mean (SD) | 39.0 (1.4) | 39.4 (0.98) | 0.356 | |
| Length of stay > 72 h, n (%) | 14 (28.6) | 3 (33.3) | 0.773 | |
| Preterm delivery, n (%) | 5 (10.2) | 0 (0) | 0.316 | |
| Fetal anomalies present, n (%) | 4 (8.2) | 0 (0) | 0.374 | |
| NICU § Admission, n (%) | 3 (6.3) | 0 (0) | 0.441 | |
| Variable | GAD-7 < 10 (n = 49) | GAD-7 ≥ 10 (n = 9) | p-Value * | |
|---|---|---|---|---|
| First 24 h post-delivery (n = 64) | Maximum pain score ≥ 7, n (%) * | 18 (36.7) | 4 (44.4) | 0.661 |
| % of time spent in severe pain, median (IQR) † | 10 (0–20) | 10 (0–10) | 0.706 | |
| 20% of time or more spent with severe pain, n (%) | 13 (26.5) | 1 (11.1) | 0.320 | |
| Lowest pain score ≤ 3, n (%) | 43 (87.8) | 6 (66.7) | 0.108 | |
| Second 24 h post-delivery | Maximum pain score ≥ 7, n (%) | 13 (26.5) | 4 (44.4) | 0.278 |
| % of time spent in severe pain, median (IQR) | 10 (0–10) | 10 (0–10) | 0.991 | |
| 20% of time or more spent with severe pain, n (%) | 10 (20.4) | 1 (11.1) | 0.513 | |
| Lowest pain score ≤ 3, n (%) | 45 (91.8) | 8 (88.9) | 0.772 | |
| Overall for hospitalization | Maximum pain score ≥ 7, n (%) | 23 (46.9) | 4 (44.4) | 0.890 |
| 20% of time or more spent with severe pain, n (%) | 16 (32.6) | 1 (11.1) | 0.192 | |
| Lowest pain score ≤ 3, n (%) | 47 (95.9) | 8 (88.9) | 0.381 | |
| Total doses of opioid medications, † | 0 (0–1) | 0 (0–3) | 0.643 | |
| Perceived adequacy of pain control, median (IQR) †‡ | 9 (8–10) | 8 (5–9) | 0.090 | |
| Satisfaction with pain control, median (IQR) †§ | 10 (8–10) | 8 (5–10) | 0.049 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olson, C.G.; Soehl, J.R.; Stowe, Z.N.; Antony, K.M. Assessment of In-Hospital Pain Control after Childbirth and Its Correlation with Anxiety in the Postpartum Period: A Cross-Sectional Study at a Single Center in the USA. Reprod. Med. 2022, 3, 334-348. https://doi.org/10.3390/reprodmed3040026
Olson CG, Soehl JR, Stowe ZN, Antony KM. Assessment of In-Hospital Pain Control after Childbirth and Its Correlation with Anxiety in the Postpartum Period: A Cross-Sectional Study at a Single Center in the USA. Reproductive Medicine. 2022; 3(4):334-348. https://doi.org/10.3390/reprodmed3040026
Chicago/Turabian StyleOlson, Clara G., John R. Soehl, Zachary N. Stowe, and Kathleen M. Antony. 2022. "Assessment of In-Hospital Pain Control after Childbirth and Its Correlation with Anxiety in the Postpartum Period: A Cross-Sectional Study at a Single Center in the USA" Reproductive Medicine 3, no. 4: 334-348. https://doi.org/10.3390/reprodmed3040026
APA StyleOlson, C. G., Soehl, J. R., Stowe, Z. N., & Antony, K. M. (2022). Assessment of In-Hospital Pain Control after Childbirth and Its Correlation with Anxiety in the Postpartum Period: A Cross-Sectional Study at a Single Center in the USA. Reproductive Medicine, 3(4), 334-348. https://doi.org/10.3390/reprodmed3040026







