1. Introduction
Bundle branch re-entrant ventricular tachycardia (BBRVT) is defined as a rare form of monomorphic ventricular tachycardia (VT) with wide QRS complexes caused by re-entrant tachycardia between both bundle branches [
1]. The prevalence of BBRVT is estimated at 6% [
2]. Patients with structural or functional heart disease and His–Purkinje system (HPS) conduction abnormalities may develop BBRVT; however, rare cases have been described in patients without apparent cardiomyopathy [
3,
4,
5,
6,
7]. Aortic valve surgery can elicit BBRVT, although this is rarely seen [
1,
5].
We present a case of a male patient with an ischemic cardiomyopathy and severe symptomatic aortic stenosis who underwent a minimal invasive aortic valve replacement (Yil-AVR) and coronary artery bypass graft (CABG). The patient developed BBRVT in the early postoperative setting, requiring additional catheter ablation of the right bundle branch (RBB).
2. Timeline
| 13 April 2017 | Out-of-hospital cardiac arrest |
| 13 April 2017 | Normal coronary angiography |
| 16 April 2017 | Delayed enhancement inferior apical wall on MRI |
| 18 April 2017 | ICD implantation |
| 2 December 2020 | Progressive impedance elevation of right ventricular lead |
| 12 January 2021 | Replacement right ventricular lead |
| 16 March 2021 | Progressive dyspnea due to severe aortic stenosis |
| 1 April 2021 | Coronary angiography with hemodynamically significant stenosis of left anterior descending artery and first diagonal branch artery |
| 2 April 2021 | Patient scheduled for Yil-AVR and CABG |
| 3 June 2021 | Yil-AVR and CABG |
| 7 June 2021 | Hospital discharge from cardiothoracic surgery ward |
| 10 June 2021 | Home monitoring revealed sustained VT |
| 10 June 2021 | Readmission on cardiology ward |
| 20 August 2021 | Follow-up cardiac check-up |
3. Clinical Case
A 62-year-old patient with arterial hypertension, diabetes mellitus type 2, dyslipidemia, obesity and paroxysmal atrial fibrillation presented at planned cardiac check-up with symptoms of progressive dyspnea. The patient had an extensive cardiac history that started in 2017 with out-of-hospital cardiac arrest following ventricular arrhythmia. Transthoracic echocardiography in 2017 showed a borderline normal systolic left ventricular ejection fraction of 50%. Coronary angiography at that time showed no high-grade stenoses; however, magnetic resonance imaging of the heart showed delayed enhancement of inferior apical wall suggestive of semi-recent myocardial infarction. Thus, the patient received subsequent implantation of an implantable cardioverter defibrillator (ICD). Thereafter, he was discharged on the following medical therapy: acetylsalicylic acid 80 milligrams once daily, bisoprolol 5 milligrams twice daily, perindopril 10 milligrams once daily and atorvastatin 40 milligrams once daily.
Control transthoracic echocardiography at current check-up showed a moderate reduced systolic left ventricular function with an ejection fraction of 42%. A progressive severe aortic stenosis with peak gradient of 66 mmHg and a mean gradient of 45 mmHg was documented for which the patient was electively admitted for pre-operative investigations. Repeat coronary angiography showed a moderate stenosis of 50% at left anterior descending coronary artery (LAD). Additional resting full-cycle ratio (RFR) of both coronary arteries was performed and showed hemodynamically significant lesions (RFR; respectively, 0.85 and 0.82). After reviewing the case at the heart team meeting, we opted for Yil-AVR and CABG with revascularization of LAD. The surgery went ahead without complications and the patient made a rapid postoperative recovery. Home monitoring of ICD revealed relapsing episodes of sustained monomorphic VT at 152 beats per minute (VT 1 zone) 3 days after discharge. Patient had no symptoms during this event. He was readmitted on the cardiology ward.
Figure 1 shows comparison of patient’s 12 lead electrocardiogram (ECG) in sinus rhythm and during BBRVT. QRS morphology during the episode of sustained VT was unchanged with apparent ventriculoatrial dissociation.
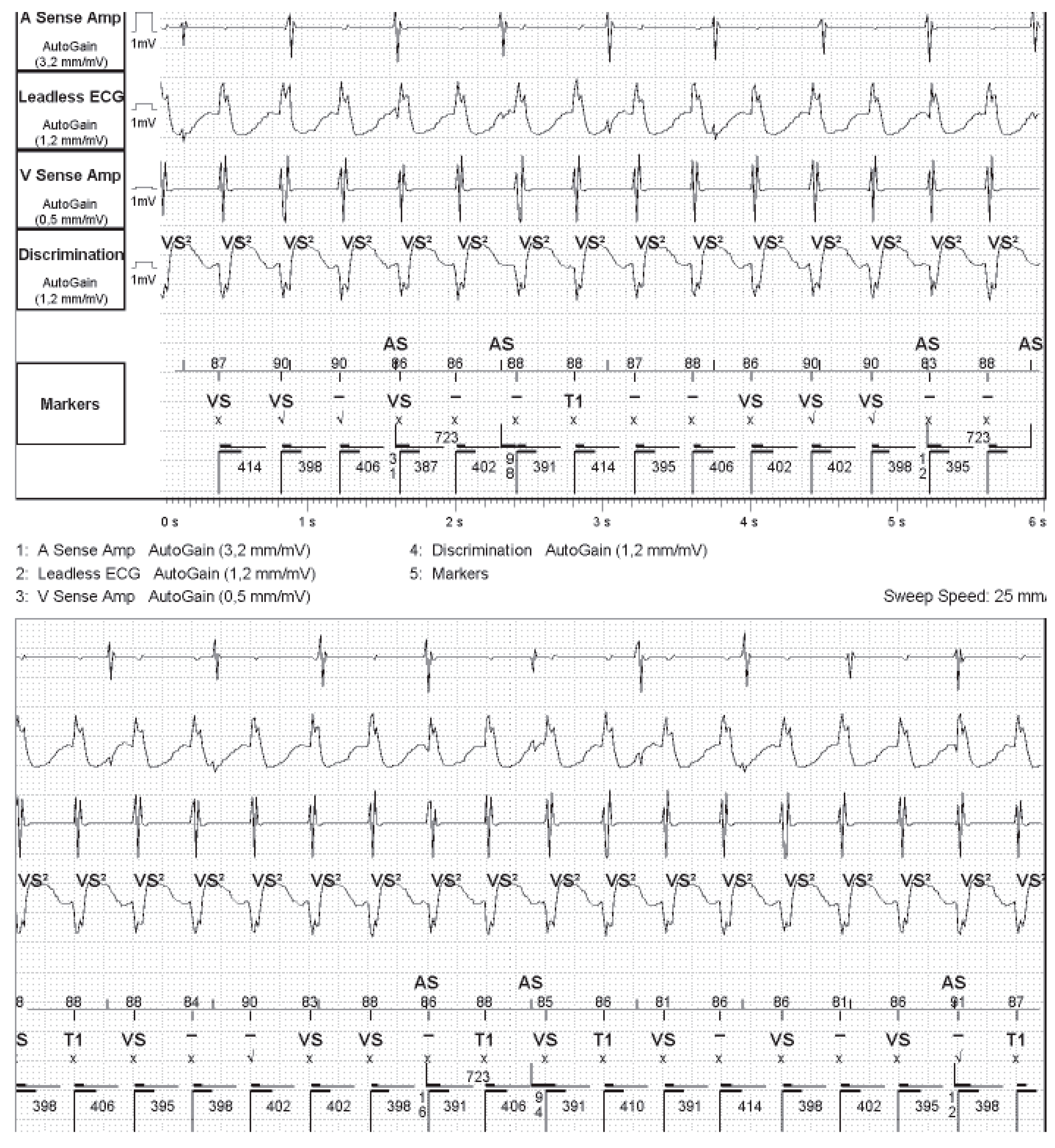
ICD analysis (
Figure 2) showed a sustained episode of VT within the VT-1 zone. No anti-tachycardia pacing or ICD shocks were needed due to spontaneous termination of VT. His antiarrhythmic drug therapy at discharge consisted of a maximal dose of beta blockers and amiodarone. Subsequent electrophysiological study was performed with successful catheter ablation of RBB. There was no ischemic VT inducible in the known inferolateral scar.
4. Discussion
We present a case of BBRVT in a patient with a non-dilated, moderately reduced functioning left ventricle after Yil-AVR and CABG.
BBRVT is a rare arrhythmia that can occur in patients with underlying structural or functional heart disease [
1,
2,
3]. In our case, BBRVT presented as a broad QRS tachycardia with LBBB morphology, resulting from antegrade conduction via RBB and retrograde conduction via LBB. A reverse re-entrant tachycardia with RBBB morphology is encountered less often. Our patient was asymptomatic; however, BBRVT can present with sudden syncope or cardiac death [
1,
2,
3]. Diagnosis of BBRVT was made by utilizing the diagnostic criteria as reported in previous papers [
8].
Sustained monomorphic VT in early postoperative setting after valve surgery is not common [
1]. Narasimhan et al. observed 29 patients with sustained monomorphic VT after valve surgery. BBRVT was diagnosed in one-third and occurred most frequently in the early postoperative setting with a median time of 10 days after surgery [
5]. Even case reports of BBRVT after transcatheter aortic valve replacement have been described [
9]. However, to our knowledge, this is the first time that BBRVT occurred after Yil-AVR.
We hypothesize that our patient with ischemic and valvular heart disease had pre-existing HPS conduction abnormalities due to ventricular dysfunction and calcification of the degenerated aortic annulus. Because of the close anatomical proximity of the aortic annulus near the conduction system, surgical manipulation during Yil-AVR could have worsened these conduction abnormalities, thus leading to onset of BBRVT. Postoperative edema or hemorrhagic lesions near HPS in combination with a higher atrial ectopic burden due to postoperative elevated adrenergic state could induce BBRVT [
5].
BBRVT is often resistant to pharmacologic antiarrhythmic therapy. However, pre-emptive use of amiodarone could have theoretical benefit in reducing atrial burden in postoperative settings and, thus, reduce the onset of BBRVT. Radiofrequency catheter ablation of a bundle branch is regarded as a first line therapy for BBRVT [
10]. Most commonly, ablation of the RBB is performed [
11].
Long-term prognosis of patients with BBRVT is understudied, but mainly depends on the underlying cardiac disease. Progressive heart failure in patients with reduced left ventricular function and BBRVT is a common cause of death. Hence, implantation of an ICD, and according to established criteria, the addition of a CRT, should be considered within this population of patients.
5. Conclusions
Patients with known cardiomyopathy can develop BBRVT early after cardiac surgery. To our knowledge, this is the first time that BBRVT occurred after Yil-AVR. It also highlights the importance of home monitoring.
Author Contributions
V.V.: conception, literature review, drafting of manuscript; P.T.J.: treating heart failure physician, review of manuscript; T.P.: electrophysiologist, review of manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from subject involved in the study.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Eckart, R.E.; Hruczkowski, T.W.; Tedrow, U.B.; Koplan, B.A.; Epstein, L.M.; Stevenson, W.G. Sustained ventricular tachycardia associated with corrective valve surgery. Circulation 2007, 116, 2005–2011. [Google Scholar] [CrossRef]
- Balasundaram, R.; Rao, H.B.; Kalavakolanu, S.; Narasimhan, C. Catheter ablation of bundle branch reentrant ventricular tachycardia. Heart Rhythm 2008, 5, S68–S72. [Google Scholar] [CrossRef] [PubMed]
- Caceres, J.; Jazayeri, M.; McKinnie, J.; Avitall, B.; Denker, S.T.; Tchou, P.; Akhtar, M. Sustained bundle branch reentry as a mechanism of clinical tachycardia. Circulation 1989, 79, 256–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, P.S.; Fleck, R.P.; Calisi, C.M.; Kozina, J.A.; Feld, G.K. Macroreentrant ventricular tachycardia and coronary artery disease in cerebrotendinous xanthomatosis. Am. J. Cardiol. 1989, 64, 680–682. [Google Scholar] [CrossRef]
- Narasimhan, C.; Jazayeri, M.R.; Sra, J.; Dhala, A.; Deshpande, S.; Biehl, M.; Akhtar, M.; Blanck, Z. Ventricular tachycardia in valvular heart disease: Facilitation of sustained bundle-branch reentry by valve surgery. Circulation 1997, 96, 4307–4313. [Google Scholar] [CrossRef] [PubMed]
- Hongwu, C.; Linsheng, S.; Bing, Y.; Weizhu, J.; Fengxiang, Z.; Gang, Y.; Kai, G.; Mingfang, L.; Kejiang, C.; Feifan, O.; et al. Electrophysiological characteristics of bundle branch reentry ventricular tachycardia in patients without structural heart disease. Circulation 2018, 11, e006049. [Google Scholar]
- Phlips, T.; Ramchurn, H.; De Roy, L. Reverse BBRVT in a structurally normal heart. Acta Cardiol. 2012, 67, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, B.; Tang, M.; Chun, K.R.; Antz, M.; Tilz, R.R.; Metzner, A.; Koektuerk, B.; Xie, P.; Kuck, K.H.; Ouyang, F. Left bundle branch-Purkinje system in patients with bundle branch reentrant tachycardia: Lessons from catheter ablation and electroanatomic mapping. Heart Rhythm 2009, 6, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Lahiri, M.; Khan, A.; Schuger, C. Bundle branch reentrant ventricular tachycardia after transcatheter aortic valve replacement. Heart Rhythm 2017, 3, 177–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cronin, E.M.; Bogun, F.M.; Maury, P.; Peichl, P.; Chen, M.; Namboodiri, N.; Aguinaga, L.; Leite, L.R.; Al-Khatib, S.M.; Anter, E.; et al. HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Heart Rhythm 2020, 17, e2–e154. [Google Scholar] [CrossRef] [PubMed]
- Blank, Z.; Dhala, A.; Deshpande, S.; Sra, J.; Jazayeri, M.; Akhtar, M. Bundle branch reentrant ventricular tachycardia: Cumulative experience in 48 patients. J. Cardiovasc. Electrophysiol. 1993, 4, 253–262. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).