Rhabdomyosarcoma of the Paranasal Sinuses Initially Diagnosed as Acute Sinusitis
Abstract
:1. Introduction
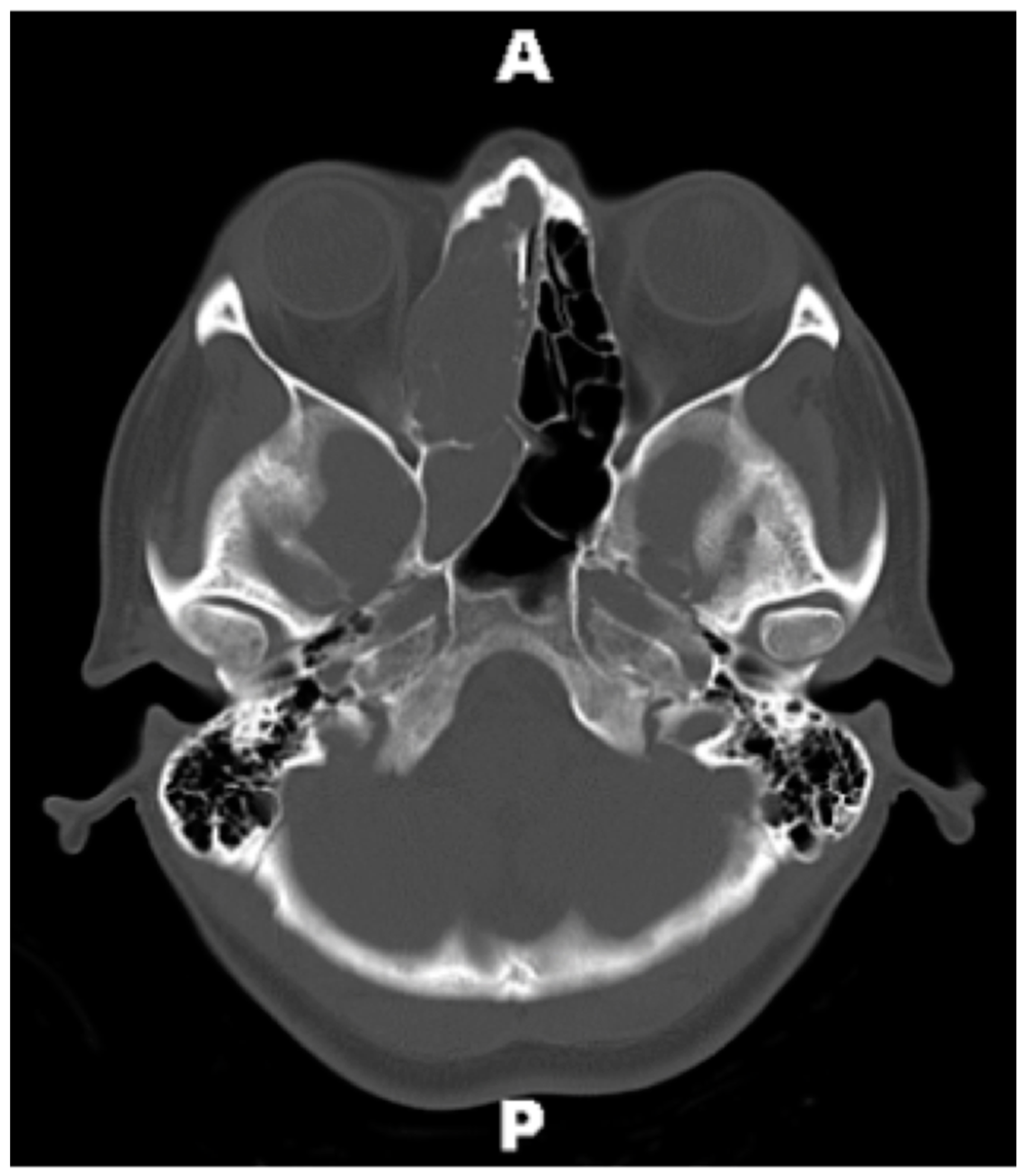
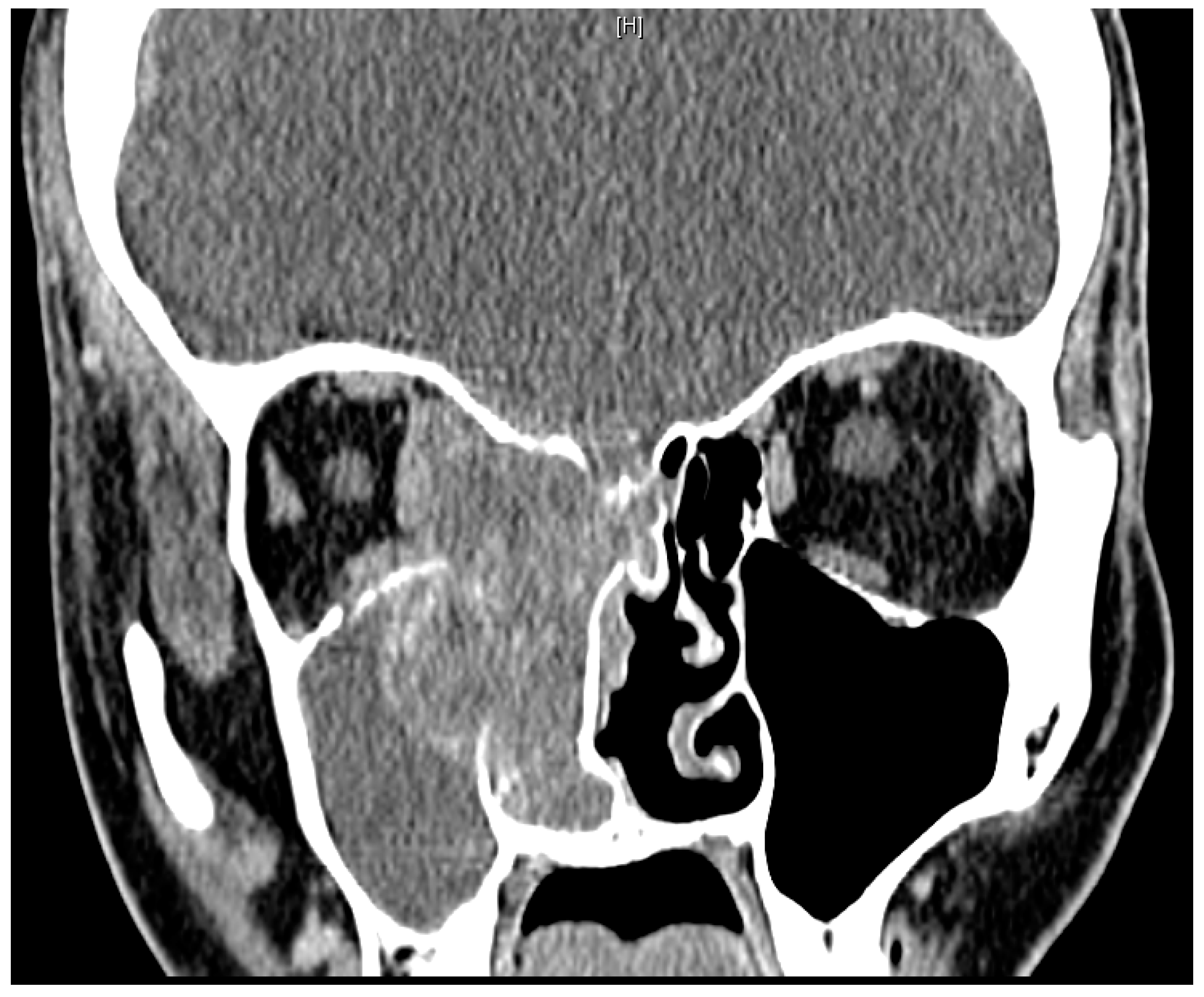
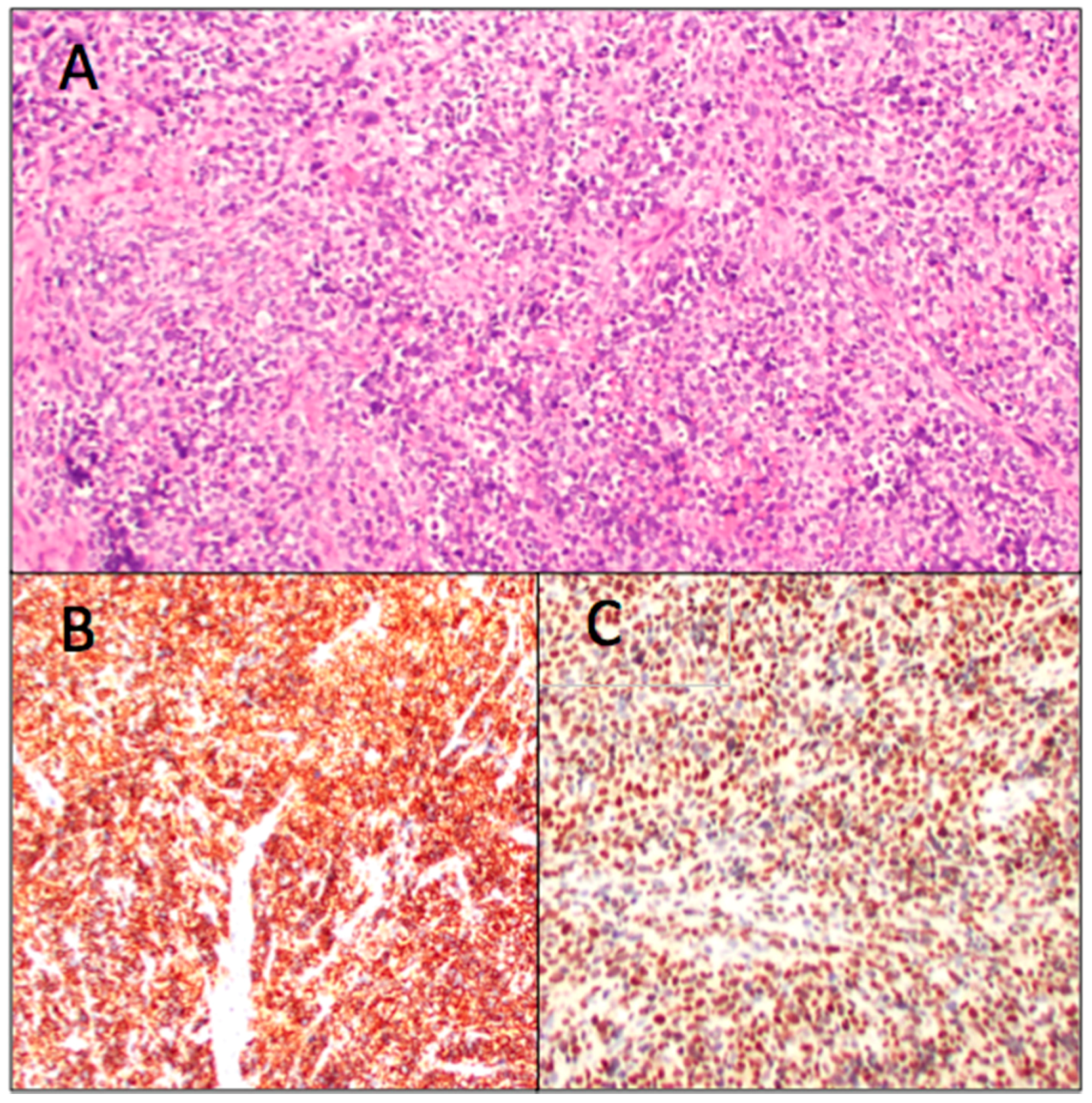
2. Case Report
3. Discussion
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Gonzalez-Gonzalez, R.; Bologna-Molina, R.; Molina-Frechero, N.; Domínguez-Malagon, H.R. Prognostic factors and treatment strategies for adult head and neck soft tissue sarcoma. Int. J. Oral Maxillofac. Surg. 2012, 41, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.E.; Chai, X.; Pollack, S.M.; Loggers, E.; Rodler, E.; Dillon, J.; Parvathaneni, U.; Moe, K.S.; Futran, N.; Jones, R.L. Analysis of clinical prognostic factors for adult patients with head and neck sarcomas. Otolaryngol. Head Neck Surg. 2014, 151, 976–983. [Google Scholar] [CrossRef] [PubMed]
- Tajudeen, B.A.; Fuller, J.; Lai, C.; Grogan, T.; Elashoff, D.; Abemayor, E.; John, M.S. Head and neck sarcomas: The UCLA experience. Am. J. Otolaryngol. 2014, 35, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Lindford, A.; McIntyre, B.; Marsh, R.; MacKinnon, C.A.; Davis, C.; Tan, S.T. Outcomes of the treatment of head and neck sarcomas in a tertiary referral center. Front. Surg. 2015, 2, 19. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.A.; Grogan, T.; Wang, M.B. Head and neck sarcomas: Analysis of the SEER database. Otolaryngol. Head Neck Surg. 2014, 151, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Mesa, C.; Goldberg, J.M.; Munoz, A.J.C.; Dumont, S.N.; Trent, J.C. Rhabdomyosarcoma in adults: New perspectives on therapy. Curr. Treat. Options Oncol. 2015, 16, 27. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.A.; Tsokos, M. Sinonasal rhabdomyosarcoma in children and young adults. Int. J. Surg. Pathol. 2007, 15, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.H.; Richmon, J.D. Head and neck rhabdomyosarcoma: A critical analysis of population-based incidence and survival data. Otolaryngol. Head Neck Surg. 2011, 145, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Callender, T.A.; Weber, R.S.; Janjan, N.; Benjamin, R.; Zaher, M.; Wolf, P.; El-Naggar, A. Rhabdomyosarcoma of the nose and paranasal sinuses in adults and children. Otolaryngol. Head Neck Surg. 1995, 112, 252–257. [Google Scholar] [CrossRef]
- Thompson, C.F.; Kim, B.J.; Lai, C.; Grogan, T.; Elashoff, D.; St John, M.A.; Wang, M.B. Sinonasal rhabdomyosarcoma: Prognostic factors and treatment outcomes. Int. Forum Allergy Rhinol. 2013, 3, 678–683. [Google Scholar] [CrossRef] [PubMed]
- Wharam, M.D., Jr. Rhabdomyosarcoma of Parameningeal Sites. Semin. Radiat. Oncol. 1997, 7, 212–216. [Google Scholar] [CrossRef]
- Douglas, J.G.; Arndt, C.A.; Hawkins, D.S. Delayed radiotherapy following dose intensive chemotherapy for parameningeal rhabdomyosarcoma (PM-RMS) of childhood. Eur. J. Cancer 2007, 43, 1045–1050. [Google Scholar] [CrossRef] [PubMed]
- Tefft, M.; Fernandez, C.; Donaldson, M.; Newton, W.; Moon, T.E. Incidence of meningeal involvement by rhabdomyosarcoma of the head and neck in children: A report of the Intergroup Rhabdomyosarcoma Study (IRS). Cancer 1978, 42, 253–258. [Google Scholar] [CrossRef]
- Persic, M.; Roberts, J.T. Alveolar rhabdomyosarcoma metastatic to the breast: Long-term survivor. Clin. Oncol. 1999, 11, 417–418. [Google Scholar] [CrossRef]
- Audino, A.N.; Setty, B.A.; Yeager, N.D. Rhabdomyosarcoma of the breast in adolescent and young adult (AYA) women. J. Pediatr. Hematol. Oncol. 2017, 39, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Kebudi, R.; Koc, B.S.; Gorgun, O.; Celik, A.; Kebudi, A.; Darendeliler, E. Breast metastases in children and adolescents with rhabdomyosarcoma: A large single-institution experience and literature review. J. Peadiatr. Hematol. Oncol. 2017, 39, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Habesoglu, T.E.; Habesoglu, M.; Surmeli, M.; Uresin, T.; Egeli, E. Unilateral sinonasal symptoms. J. Craniofac. Surg. 2010, 21, 2019–2022. [Google Scholar] [CrossRef] [PubMed]
- Pasquini, E.; Sciarretta, V.; Farneti, G.; Modugno, G.C.; Ceroni, A.R. Inverted papilloma: Report of 89 cases. Am. J. Otolaryngol. 2004, 25, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Yoskovitch, A.; Braverman, I.; Nachtigal, D.; Frenkiel, S. Sinonasal schneiderian papilloma. J. Otolaryngol. 1998, 27, 122–126. [Google Scholar] [PubMed]

© 2017 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dilger, A.E.; Schneider, A.L.; Cramer, J.; Shintani Smith, S. Rhabdomyosarcoma of the Paranasal Sinuses Initially Diagnosed as Acute Sinusitis. Sinusitis 2017, 2, 2. https://doi.org/10.3390/sinusitis2010002
Dilger AE, Schneider AL, Cramer J, Shintani Smith S. Rhabdomyosarcoma of the Paranasal Sinuses Initially Diagnosed as Acute Sinusitis. Sinusitis. 2017; 2(1):2. https://doi.org/10.3390/sinusitis2010002
Chicago/Turabian StyleDilger, Amanda E., Alexander L. Schneider, John Cramer, and Stephanie Shintani Smith. 2017. "Rhabdomyosarcoma of the Paranasal Sinuses Initially Diagnosed as Acute Sinusitis" Sinusitis 2, no. 1: 2. https://doi.org/10.3390/sinusitis2010002
APA StyleDilger, A. E., Schneider, A. L., Cramer, J., & Shintani Smith, S. (2017). Rhabdomyosarcoma of the Paranasal Sinuses Initially Diagnosed as Acute Sinusitis. Sinusitis, 2(1), 2. https://doi.org/10.3390/sinusitis2010002




