Abstract
Voice plays a prominent role in verbal communication and social interactions. Acute burn care often includes intubation, mechanical ventilation, and tracheostomy, which could potentially impact voice quality. However, the issue of long-term dysphonia remains underexplored. This study investigates long-term self-reported voice changes in individuals with burn injuries, focusing on the impact of acute burn care interventions. Analyzing data from a multicenter longitudinal database (2015–2023), self-reported vocal changes were examined at discharge and 6, 12, 24, and 60 months after injury. Out of 582 participants, 65 reported voice changes at 12 months. Changes were prevalent at discharge (16.4%) and persisted over 60 months (11.6–12.7%). Factors associated with voice changes included flame burn, inhalation injury, tracheostomy, outpatient speech-language pathology, head/neck burn, larger burn size, mechanical ventilation, and more ventilator days (p < 0.001). For those on a ventilator more than 21 days, 48.7% experience voice changes at 12 months and 83.3% had received a tracheostomy. The regression analysis demonstrates that individuals that were placed on a ventilator and received a tracheostomy were more likely to report a voice change at 12 months. This study emphasizes the need to understand the long-term voice effects of intubation and tracheostomy in burn care.
1. Introduction
Voice, from the Latin word vocem, plays a large role in verbal communication and social interactions [1,2]. The voice is the channel through which ideas, emotions, and personalities are communicated [2]. When injuries to the head and neck occur, patients may be left with vocal changes that can impact their communication and quality of lifelong term [3]. Although burn injury has a 96.8% survival rate, many survivors face long-term challenges [4,5,6]. Some of these challenges include physical and mental health deficits, impacting life satisfaction. Dysphonia, an impairment in voice, and dysphagia, a swallowing disorder, can persist through the acute stage of burn injury and manifest as chronic issues, especially in individuals who also have had an inhalation injury [6,7].
Studies have shown that some burn injuries result in long-term damage to laryngeal and pharyngeal structures [8,9,10,11]. Burns due to direct thermal contact caused by hot liquids, flames, or steam can directly damage the larynx and pharynx [12]. Likewise, the inhalation of superheated gases and toxic substances during a fire can lead to damage of the upper airway [13]. Delayed complications from burn injuries, such as infection and scarring, may also affect the larynx and pharynx [14]. Scar tissue formation (fibrosis) can cause long-term constriction or narrowing of the airway [14].
A systematic review noted that dysphagia and dysphonia were the most prevalent sequelae of patients diagnosed with laryngeal injuries [11]. Other studies have reported a decline in voice quality and some degree of hoarseness after burn and inhalation injury [9]. Early management plans for burn patients often include intubation, which may impact voice quality as well [8,15]. Airway swelling from burns affecting the face, neck, or upper chest can compromise breathing, making intubation necessary to maintain a clear airway, especially in cases of inhalation injury associated with extensive burns [16]. Additionally, intubation allows for mechanical ventilation, aiding oxygenation, and ventilation support [17]. The length of intubation and number of laryngeal procedures is associated with long-term laryngeal function [9,18,19,20,21].
Dysphagia and laryngeal status after a burn injury has been well documented, while the issue of long-term dysphonia remains underexplored. Thus, this study aims to describe the frequency with which burn survivors report vocal changes up to five years after injury and examine factors associated with voice changes.
2. Materials and Methods
2.1. Burn Model System National Database
This study used data from the Burn Model System (BMS) National Database, funded by the National Institute on Disability, Independent Living, and Rehabilitation Research. The BMS National Database was established in 1994 to explore the long-term physical and psychosocial outcomes of burn survivors and is one of the world’s most extensive longitudinal datasets of burn injury outcomes. Informed consent is obtained from all participants, and each BMS site’s Institutional Review Board oversees data collection. The sites included in this study were the Boston-Harvard Burn Injury Model System (BH-BIMS), Boston, MA, USA; North Texas Burn Rehabilitation Model System, Dallas, TX, USA; Northwest Regional Burn Model System, Seattle, WA, USA; and the University of Texas Medical Branch/Shriners Hospital Pediatric Burn Model System Galveston, TX, USA.
Data from participants who were burned between 2015 and 2023, age greater than or equal to 18 years at the time of injury, alive at discharge, and consented to participate in the BMS National Database were included in this study. Current criteria for inclusion in the BMS National Database are those who require autografting or amputation surgery for wound closure and meet one of the following criteria: (1) 0–64 years of age with a burn injury ≥20% total body surface area (TBSA), (2) ≥65 years of age with a burn injury ≥10% TBSA, (3) any age with a burn injury to their face/neck, hands, or feet, (4) any age with a high-voltage electrical burn injury. The BMS database enrollment criteria have been modified over time, and these changes are detailed on the BMS National Data and Statistical Center’s website: https://burndata.washington.edu/ (accessed on 30 January 2023) [22,23].
2.2. Demographic and Clinical Characteristics
The following demographic and clinical characteristics were collected by medical record abstraction or self-report: age, race, Hispanic/Latino ethnicity, sex, education, employment, BMS site, alcohol and drug misuse history (both variables from the Cut down, Annoyed, Guilty, and Eye-opener (CAGE) Scale; the CAGE Scale is considered positive if the score is greater than or equal to 2; pre-injury recall collected at discharge) [24,25], burn size (percent total body surface area burned, TBSA), ventilator days (>1 day), burn etiology, inhalation injury (Y/N), tracheostomy (Y/N), outpatient speech-language pathology services (Y/N), head/neck burn, multiple trips to the operating room (≥2; Y/N), and mechanical ventilation. Alcohol and drug misuse were included because they have been shown to affect the vocal cords, potentially leading to inflammation, dehydration, and changes in vocal fold function [26,27,28].
2.3. Voice Outcomes
The primary outcome was the item, “Do you currently have change in voice?” (dichotomous response options: Y/N) in the Adult Review of Systems section of the BMS follow-up questionnaire at the 12-month time point. This item is also collected at discharge and at 6, 24, and 60 months after burn injury. The 12-month time point was chosen a priori by the authors because it is a sufficient time since injury to capture long-term voice outcomes; additionally, this time point ensured a more robust sample size given documented higher participant attrition rates at more distal time points [29].
2.4. Data Analysis
Demographic and clinical characteristics were summarized and compared for participants with and without voice change at 12 months. They were compared using non-parametric tests (Wilcoxon–Mann–Whitney) due to the non-normality of data for continuous variables and chi-square tests or Fisher’s exact (depending on sample size) for categorical variables; significance level was adjusted for multiple comparisons using Bonferroni’s method to p < 0.003. The frequency of voice change was examined at all follow-up time points: discharge, six months, 12 months, 24 months, and 60 months after burn injury. In addition, a subgroup analysis examined participants with repeated outcome measurements to examine the percentage of participants reporting voice change at discharge and at each follow-up time point (6, 12, 24, and 60 months).
An omnibus (chi-square) test was used to examine if there were statistically significant differences in the percent of burn survivors experiencing voice change by ventilator days (categories: 0, 1–10, 11–20, 21+ days). Likewise, the percentage of tracheostomies by ventilator days was at 12 months compared for those with and without a voice change. Tracheostomies are often considered after prolonged endotracheal intubation exceeding 21 days. Thus, different ventilator day durations were used to compare the percentage of those with a tracheostomy to those with voice change [30].
A logistic regression model assessed the association between voice change and demographic and clinical variables (age, sex, BMS site, burn size, etiology, inhalation injury, tracheostomy, ventilator (Y/N), burn location, and multiple operations) at 12 months, which was the primary outcome of this study. Robust standard errors accounted for heteroskedasticity, and the significance value was set to 0.05. Two additional analogous exploratory logistic regression models were conducted to assess the association between voice change at 24 and 60 months with demographic and clinical variables (age, sex, BMS site, burn size, etiology, inhalation injury, tracheostomy, ventilator (Y/N), burn location, and multiple operations). In addition, race, ethnicity, education, employment, history of alcohol and drug use (CAGE scale) were not significantly different between groups in the descriptive analysis thus, they were not included the regression model.
3. Results
3.1. Study Sample and Comparison of Characteristics between Groups
This study included 582 persons with a burn injury (65 self-reported a change in voice and 517 reported no change in voice at 12 months). The group with reported voice changes at 12 months had larger burn size (31.1% vs. 15.5% TBSA; p < 0.001) and greater ventilator days (25.9 ± 25.6 vs. 12.9 ± 21.2 days, p < 0.001). Additionally, the group with voice changes were more likely to have a flame burn etiology (83.1% vs. 52.7%, p < 0.001), inhalation injury (32.8% vs. 8.7%, p < 0.001), tracheostomy (29% vs. 4.3%, p < 0.001), outpatient speech-language pathology services (7.7% vs. 1%, p < 0.001), head/neck burn (78.5% vs. 45.4%, p < 0.001), multiple trips to the operating room (76.9% vs. 48.7%, p < 0.001), and require mechanical ventilation (67.2% vs. 19.7%, p < 0.001). Age, race, ethnicity, sex, education, employment, BMS site, and alcohol and drug misuse history were not statistically different between groups. A comparison of demographic and clinical characteristics between groups is presented in Table 1.

Table 1.
Comparison of demographic and clinical variables between participants with and without voice changes at 12 months (n = 582).
3.2. Self-Reported Voice Outcomes over Time
Self-report change in voice was most commonly reported at discharge (16.4%) and persisted over the follow-up time points (11.2–12.7%). The information presented in Table 2 is cross-sectional, resulting in varying sample sizes at each time point. Additionally, it excludes individuals whose data collection periods had not commenced (for instance, the 60-month data point excludes participants who sustained burn injuries after 2019).

Table 2.
Self-reported change in voice at each follow-up time point after burn injury.
The frequency of voice changes for participants with repeated measures at discharge and follow-up time points is summarized in Table 3. Participants with repeated measures reported change in voice at discharge at 15.8–19.6% and change in voice at follow-up time points ranged from 10.7% to 17.1%.

Table 3.
Frequency of “change in voice” at discharge and each follow-up among those with repeated measures.
3.3. Association of Voice Changes with Ventilator Days and Tracheostomy
At 12 months, self-reported changes in voice were observed to increase with more ventilator days. For participants with 21+ days on a ventilator, 48.7% reported a change in voice at 12 months. Similarly, the percentage of tracheostomies increased with more ventilator days. For participants with 21+ days on a ventilator, 83.3% had a tracheostomy. The relationship between voice change, tracheostomy status and ventilator days at 12 months is illustrated in Figure 1.
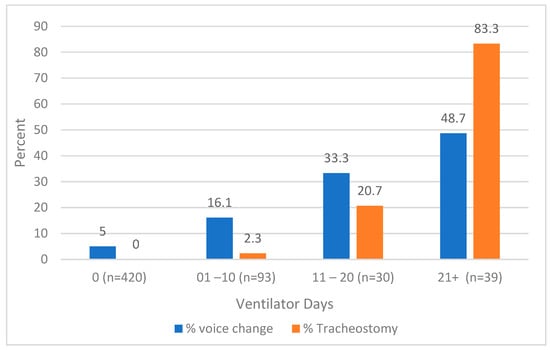
Figure 1.
Histogram of the association between voice change and tracheostomy status by ventilator days. Voice change and tracheostomy status are associated with ventilator days at 12 months (p < 0.001). Differences were examined using the omnibus (chi-square) test.
3.4. Factors Associated with Voice Change
The logistic regression analysis examined the association between self-reported voice changes at 12 months and demographic and clinical factors (Table 4). Results showed that participants with a tracheostomy were 184% (p = 0.027) more likely to report change in voice at 12 months, and those participants on a ventilator were 331% (p < 0.001) more likely to report change in voice when controlling for demographic and other clinical factors. Additionally, an exploratory logistic regression investigated the correlation between self-reported voice changes at 24 months and various demographic and clinical factors. It demonstrated that age (OR: 1.05, p < 0.001) and tracheostomy (OR: 39.75, p < 0.001) increased the odds of reporting a voice change. Another exploratory regression model was not conducted for the 60-month time point due to the small sample size for analysis.

Table 4.
Logistic regression analysis examining associations between self-reported changes in voice at 12-months and demographics and clinical characteristics.
4. Discussion
Self-reported voice changes are common among people experiencing burn injuries and can persist for up to five years after injury [31]. This study found that approximately one in six participants reported voice changes at acute hospital discharge, and one in nine reported changes up to five years after injury. In addition, those who were treated with a ventilator and received a tracheostomy showed a higher likelihood of reporting voice changes at one year. These findings may inform the longitudinal care of burn patients regarding voice issues and a growing understanding of the long-term implications of acute interventions, such as mechanical ventilation and tracheostomy.
This study provides evidence that dysphonia is a long-term complication, which contributes to understanding burns as a chronic condition [6]. Other research supports that dysphonia ‘s chronicity can affect all ages and genders with a higher prevalence in patients who use their voice more frequently due to work-related responsibilities [7,32,33]. Additionally, dysphonia negatively impacts quality of life, including social interactions, work performance, and pain [34]. A scoping review examining the long-term laryngotracheal complications after inhalation injury noted that dysphonia was a frequent sequela after injury [35]. Close monitoring and timely interventions to address dysphonia are important. The authors suggest providers include questions about voice during the follow-up evaluations to screen for dysphonia. For symptomatic patients, referrals to otolaryngologists for further evaluation and speech language pathologists for voice rehabilitation should be considered. A possible area for further exploration involves developing long-term care models that address prevalent changes in vocal quality among people living with burn injuries along with patient-reported outcome measures that capture the impact of voice changes on daily tasks.
At 12 months after injury, individuals living with burn injury exhibited higher odds of reporting a change in voice if they were on a ventilator and had received a tracheostomy. Studies have shown that prolonged intubation can exacerbate the risk of vocal cord injury, thus emphasizing the potential benefits of minimizing the duration of intubation to mitigate voice quality complications [16]. Over the last two decades, many have debated the proper timing of tracheostomy for patients with prolonged mechanical ventilation [16,18,35]. The American College of Chest Physicians guidelines recommend considering a tracheostomy in patients receiving mechanical ventilation for more than 21 days [36,37]. The data from this study provide additional detail on the long-term implications of prolonged mechanical ventilation and tracheostomy as this practice was associated with increased odds of experiencing voice changes 12 months after injury.
There are multiple limitations in this study. There was less voice change data at more distal time points due to loss to follow-up, and some participants had not yet reached that follow-up period. Nonetheless, patterns regarding the frequency of self-reported voice changes emerged by examining all data cross-sectionally (Table 2) and cohorts with repeated measures (Table 4). Given that the BMS database inclusion criteria select those with more severe burn injuries, this introduces selection bias; additionally, follow-up data may be affected by response bias [36]. However, prior work has noted that the BMS database is representative of the national burn population [38]. In this study, there are likely confounding factors involved in the inhalation injury, intubation, and tracheostomy data contributing to these results. The BMS database does not include days from tracheostomy to decannulation or duration of overlap between tracheostomy and ventilation. Therefore, the dataset is not able to assess if duration of tracheostomy or overlap in tracheostomy and ventilator is related to subsequent dysphonia. Thus, this study cannot conclusively assess if the timing of transitioning from endotracheal intubation to tracheostomy impacts voice outcomes. A study comparing dysphonia and dysphagia outcomes of early tracheostomy (at 14 days) versus current guidelines (21 days) would be an important future study.
It is important to note that the voice change data in this dataset were based on participant self-report without formal speech therapy assessment or validated voice outcome measures, and it also lacks information on the nature and frequency of voice interventions received by burn survivors, potentially affecting the course of their voice symptoms. It is possible that some burn survivors experienced voice changes as a result of other health issues unrelated to their burn injury. To address these limitations, future studies may utilize objective standardized measures of voice function and anatomy with Speech-Language Pathology and Otolaryngology assessments to capture the severity and physiology of vocal impairments. Despite these limitations of the dataset and study design, this study is one of the first to examine long term self-reported dysphonia outcomes after burns in a multicenter database and therefore is a starting point in better understanding these outcomes.
5. Conclusions
The study found that self-reported voice changes are common and often persist for up to five years in the hospitalized burn population. Notably, factors such as mechanical ventilation and tracheostomy are associated with persistent voice changes after injury. Nonetheless, the findings of this study should be considered in the context of its limitations, which notably included self-reported voice changes without comprehensive speech therapy or otolaryngology assessments. Future studies should examine voice outcomes utilizing standardized assessments as well as the impact of speech-language pathology and other interventions on those with long-term dysphonia after burns.
Author Contributions
Conceptualization, K.L.C., E.S., K.M., L.J.S., C.T.-H., A.T.C., C.A., C.M.O., C.M.R. and J.C.S.; Data curation, K.M.; Formal analysis, K.M.; Investigation, K.L.C., C.T.-H., C.M.R. and J.C.S.; Methodology, K.L.C., E.S., K.M., L.J.S., C.T.-H., A.T.C., C.A., C.M.O., C.M.R. and J.C.S.; Project administration, C.M.R. and J.C.S.; Supervision, C.M.R. and J.C.S.; Visualization, C.M.R. and J.C.S.; Writing—original draft, K.L.C.; Writing—review and editing, K.L.C., E.S., K.M., L.J.S., C.T.-H., A.T.C., H.A.Y., C.A., C.M.O., C.M.R. and J.C.S. All authors have read and agreed to the published version of the manuscript.
Funding
The contents of this article were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant numbers 90DPBU0005, 90DPBU0007, 90DPBU0008 and 90DPBU0009). The NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this article do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government. Partial support was obtained from Shriners Hospitals for Children (Grant #79136-BOS-23 and 79138-BOS-23).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Mass General Brigham (protocol code 2011P001264 and 6/15/2015).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The Burn Injury Model System National Database is a prospective, longitudinal, multi-center research data repository that contains measures of functional and psychosocial outcomes following burns. The data are free and publicly available at https://burndata.washington.edu/ (accessed on 30 January2023).
Conflicts of Interest
Ryan received financial support from MediWound for contracted research. This funding did not directly or indirectly impact this work. The remaining authors have no relevant financial or non-financial interests to disclose.
References
- Holavanahalli, R.; Quayle, B.K. Model Systems Knowledge Translation Center. Social Interaction after Burn Injury. Model Systems Knowledge Translation Center. Available online: https://msktc.org/sites/default/files/2022-06/SI-After-Burn-508_0.pdf (accessed on 25 May 2023).
- Tiwari, M.; Tiwari, M. Voice—How humans communicate? J. Nat. Sci. Biol. Med. 2012, 3, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers. 2020, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- American Burn Association. 2016 National Burn Repository. Report of Data from 2006–2015 [Internet]; American Burn Association: Chicago, IL, USA, 2017; Available online: https://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/ (accessed on 1 June 2023).
- Abouzeid, C.A.; Wolfe, A.E.; Ni, P.; Carrougher, G.J.M.; Gibran, N.S.; Hammond, F.M.; Holavanahalli, R.; McMullen, K.A.; Roaten, K.; Suman, O.; et al. Are burns a chronic condition? Examining patient reported outcomes up to 20 years after burn injury—A Burn Model System National Database investigation. J. Trauma Acute Care Surg. 2022, 92, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- Kelter, B.M.; Holavanahalli, R.; Suman, O.E.; Ryan, C.M.; Schneider, J.C. Recognizing the long-term sequelae of burns as a chronic medical condition. Burns 2020, 46, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Clayton, N.A.; Ward, E.C.; Rumbach, A.F.; Cross, R.R.; Kol, M.R.; Maitz, P.K. Influence of Inhalation Injury on Incidence, Clinical Profile and Recovery Pattern of Dysphagia Following Burn Injury. Dysphagia 2020, 35, 968–977. [Google Scholar] [CrossRef] [PubMed]
- Casper, J.K.; Clark, W.R.; Kelley, R.T.; Colton, R.H. Laryngeal and phonatory status after burn/inhalation injury: A long-term follow-up study. J. Burn Care Rehabil. 2002, 23, 235–243. [Google Scholar] [CrossRef]
- Clayton, N.; Kennedy, P.; Maitz, P. The severe burns patient with tracheostomy: Implications for management of dysphagia, dysphonia and laryngotracheal pathology. Burns 2010, 36, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Kelly, E.; Hirschwald, J.; Clemens, J.; Regan, J. Persistent Features of Laryngeal Injury Following Endotracheal Intubation: A Systematic Review. Dysphagia 2023, 38, 1333–1341. [Google Scholar] [CrossRef] [PubMed]
- Andriolo, B.N.; Andriolo, R.B.; Saconato, H.; Atallah, Á.N.; Valente, O. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst. Rev. 2015, 1, CD007271. [Google Scholar] [CrossRef]
- Khashaba, H.A.; Al-Fadhli, A.N.; Al-Tarrah, K.S.; Wilson, Y.T.; Moiemen, N. Epidemiology and outcome of burns at the Saud Al Babtain Burns, Plastic Surgery and Reconstructive Center, Kuwait: Our experience over five years (from 2006 to 2010). Ann. Burn. Fire Disasters 2012, 25, 178–187. [Google Scholar]
- Mlcak, R.P.; Suman, O.E.; Herndon, D.N. Respiratory management of inhalation injury. Burns 2007, 33, 2–13. [Google Scholar] [CrossRef] [PubMed]
- Carney, B.C.; Bailey, J.K.; Powell, H.M.; Supp, D.M.; Travis, T.E. Scar Management and Dyschromia: A Summary Report from the 2021 American Burn Association State of the Science Meeting. J. Burn Care Res. 2023, 44, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Moshrefi, S.; Sheckter, C.C.; Shepard, K.; Pereira, C.; Davis, D.J.; Karanas, Y.; Rochlin, D.H. Preventing Unnecessary Intubations: A 5-Year Regional Burn Center Experience Using Flexible Fiberoptic Laryngoscopy for Airway Evaluation in Patients with Suspected Inhalation or Airway Injury. J. Burn Care Res. 2019, 40, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, T.L.; Caruso, D.M.; Foster, K.N.; Cairns, B.A.; Peck, M.D.; Gamelli, R.L. Effect of inhalation injury on fluid resuscitation requirements after thermal injury. Crit. Care 2009, 13, R47. [Google Scholar]
- American Burn Association. Burn Resuscitation Guidelines. 2008. Available online: https://ameriburn.org/wp-content/uploads/2017/05/burn_resuscitation.pdf (accessed on 22 December 2023).
- Brodsky, M.B.; Levy, M.J.; Jedlanek, E.; Pandian, V.P.; Blackford, B.M.; Price, C.M.; Cole, G.D.; Hillel, A.T.; Best, S.R.; Akst, L.M. Laryngeal Injury and Upper Airway Symptoms After Oral Endotracheal Intubation with Mechanical Ventilation during Critical Care: A Systematic Review. Crit. Care Med. 2018, 46, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- Gaissert, H.A.; Lofgren, R.H.; Grillo, H.C. Upper airway compromise after inhalation injury. Complex strictures of the larynx and trachea and their management. Ann. Surg. 1993, 218, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Roy, N.; Merrill, R.M.; Gray, S.D.; Smith, E.M. Voice disorders in the general population: Prevalence, risk factors, and occupational impact. Laryngoscope 2005, 115, 1988–1995. [Google Scholar] [CrossRef]
- Tracy, L.F.; Shehan, J.; Grillone, G.A. Upper Airway Burn Injury. Oper. Tech. Otolaryngol.-Head Neck Surg. 2020, 31, 295–300. [Google Scholar] [CrossRef]
- Goverman, J.; Mathews, K.; Holavanahalli, R.K.; Vardanian, A.; Herndon, D.N.; Meyer, W.J.; Kowalske, K.; Fauerbach, J.; Gibran, N.S.; Carrougher, G.J.; et al. The National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Twenty Years of Contributions to Clinical Service and Research. J. Burn Care Res. 2017, 38, e240–e253. [Google Scholar] [CrossRef]
- Amtmann, D.; McMullen, K.; Bamer, A.; Fauerbach, J.A.; Gibran, N.S.; Herndon, D.; Schneider, J.C.; Kowalske, K.; Holavanahalli, R.; Miller, A.C. National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Review of Program and Database. Arch. Phys. Med. Rehabil. 2020, 101, S5–S15. [Google Scholar] [CrossRef]
- Ewing, J.A. Detecting Alcoholism: The CAGE Questionnaire. JAMA 1984, 252, 1905–1907. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.L.; Rounds, L.A. Conjoint screening questionnaires for alcohol and other drug abuse: Criterion validity in a primary care practice. Wis. Med. J. 1995, 94, 135–140. [Google Scholar] [PubMed]
- Reid, A.; Ha, J.F. Inhalational injury and the larynx: A review. Burns 2019, 45, 1266–1274. [Google Scholar] [CrossRef] [PubMed]
- Behlau, M.; Madazio, G.; Oliveira, G.; Pontes, P. Evaluation of vocal abuse: Interdisciplinary analysis of 107 cases. J. Voice 2008, 22, 682–689. [Google Scholar]
- Hamdan, A.L. The effects of drugs on the larynx. J. Voice 2016, 30, 461.e13–461.e19. [Google Scholar]
- Bamer, A.M.; McMullen, K.; Gibran, N.; Holavanahalli, R.; Schneider, J.C.; Carrougher, G.J.; Wiechman, S.; Wolfe, A.; Amtmann, D. Factors Associated with Attrition of Adult Participants in a Longitudinal Database: A National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System Study. J. Burn Care Res. 2020, 41, 270–279. [Google Scholar] [CrossRef]
- American College of Chest Physicians. Guidelines for the management of adult patients with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Chest 2005, 128, 221–235. [Google Scholar]
- Beck, I.; Tapking, C.; Haug, V.; Nolte, S.; Böcker, A.; Stoppe, C.; Kneser, U.; Hirche, C.; Hundeshagen, G. Short- and long term hyposmia, hypogeusia, dysphagia and dysphonia after facial burn injury—A prospective matched cohort study. Burns 2023, 49, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Neighbors, C.; Song, S.A. Dysphonia. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK565881/ (accessed on 22 December 2023).
- Smith, E.; Taylor, M.; Mendoza, M.; Barkmeier, J.; Lemke, J.; Hoffman, H. Spasmodic dysphonia and vocal fold paralysis: Outcomes of voice problems on work-related functioning. J. Voice 1998, 12, 223–232. [Google Scholar] [CrossRef]
- Rouhani, M.J.; Clunie, G.; Thong, G.; Lovell, L.; Roe, J.; Ashcroft, M.; Holroyd, A.; Sandhu, G.; Al Yaghchi, C. A Prospective Study of Voice, Swallow, and Airway Outcomes Following Tracheostomy for COVID-19. Laryngoscope 2021, 131, E1918–E1925. [Google Scholar] [CrossRef]
- Zhen, E.; Misso, D.; Rea, S.; Vijayasekaran, S.; Fear, M.; Wood, F. Long-Term Laryngotracheal Complications After Inhalation Injury: A Scoping Review. J. Burn Care Res. 2023, 44, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Plummer, A.L.; Gracey, D.R. Consensus conference on artificial airways in patients receiving mechanical ventilation. Chest 1989, 96, 178–180. [Google Scholar] [CrossRef] [PubMed]
- Khammas, A.H.; Dawood, M.R. Timing of Tracheostomy in Intensive Care Unit Patients. Int. Arch. Otorhinolaryngol. 2018, 22, 437–442. [Google Scholar] [CrossRef]
- Lezotte, D.C.; Hills, R.A.; Heltshe, S.L.; Holavanahalli, R.K.; Fauerbach, J.A.; Blakeney, P.; Klein, M.B.; Engrav, L.H. Assets and liabilities of the Burn Model System data model: A comparison with the National Burn Registry. Arch. Phys. Med. Rehabil. 2007, 88 (Suppl. S2), S7–S17. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).