Early Impact of COVID-19 Pandemic on Burn Injuries, Admissions, and Care in a Statewide Burn Service
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Data Source
2.2. Data Management
2.3. Statistical Analysis
2.4. Ethics Approval
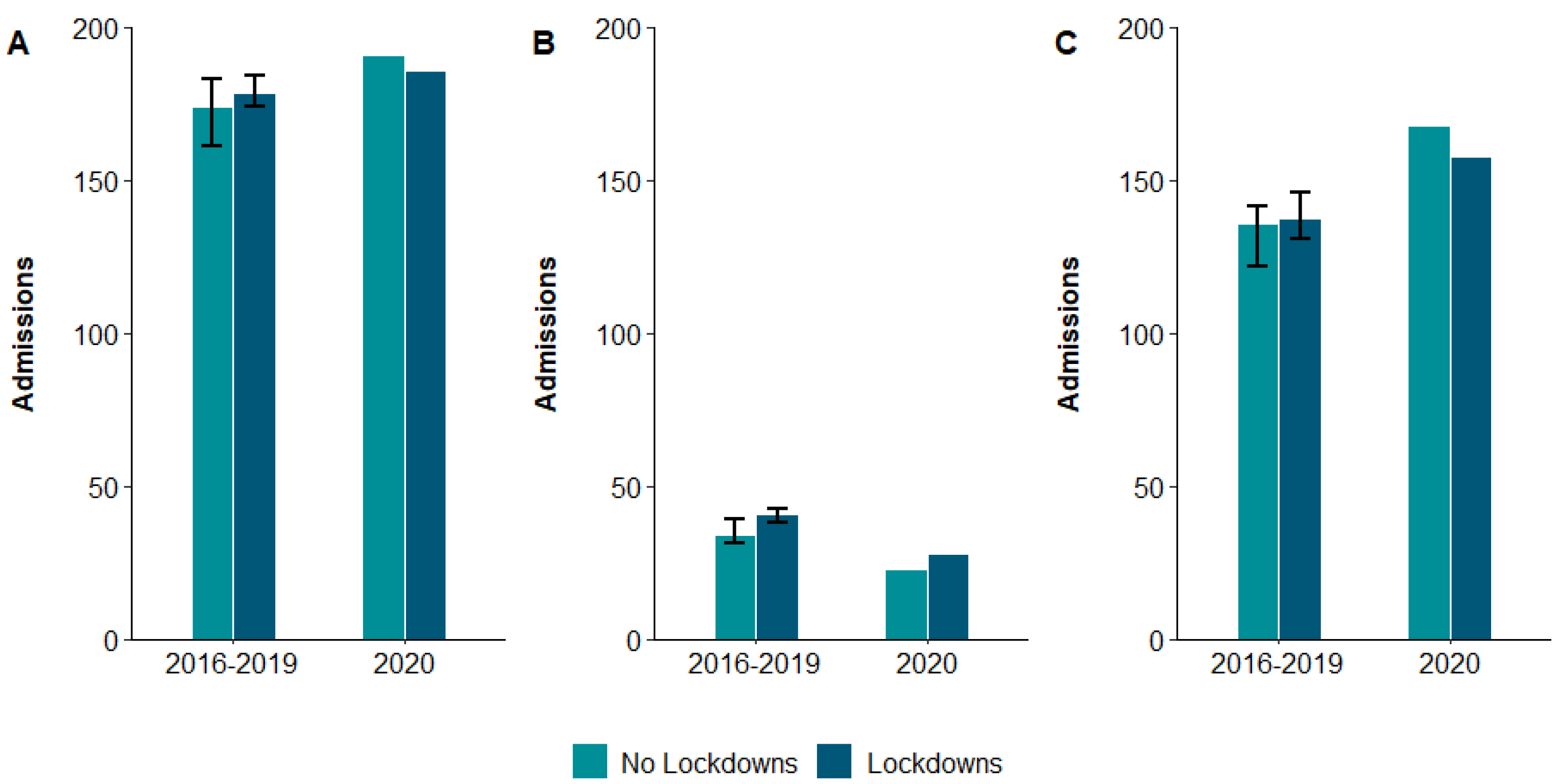
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Listings of WHO’s Response to COVID-19. 2020. Available online: https://www.who.int/news/item/29-06-2020-covidtimeline (accessed on 29 August 2022).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 29 August 2022).
- Hunt, G. First Confirmed Case of Novel Coronavirus in Australia. 2020. Available online: https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/first-confirmed-case-of-novel-coronavirus-in-australia (accessed on 8 February 2022).
- Azzena, B.; Perozzo, F.A.G.; De Lazzari, A.; Valotto, G.; Pontini, A. Burn Unit admission and management protocol during COVID-19 pandemic. Burns 2021, 47, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Barret, J.P.; Chong, S.J.; Depetris, N.; Fisher, M.D.; Luo, G.; Moiemen, N.; Pham, T.; Qiao, L.; Wibbenmeyer, L.; Matsumura, H. Burn center function during the COVID-19 pandemic: An international multi-center report of strategy and experience. Burns 2020, 46, 1021–1035. [Google Scholar] [CrossRef] [PubMed]
- Farroha, A. Reduction in length of stay of patients admitted to a regional burn centre during COVID-19 pandemic. Burns 2020, 46, 1715. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Liu, T.; Chen, H.; Liao, J.; Li, H.; Luo, Q.; Song, H.; Xiang, F.; Tan, J.; Zhou, J.; et al. Management strategies for the burn ward during COVID-19 pandemic. Burns 2020, 46, 756–761. [Google Scholar] [CrossRef]
- Ma, S.; Yuan, Z.; Peng, Y.; Chen, J.; Li, H.; Luo, Q.; Song, H.; Xiang, F.; Tan, J.; Zhou, J.; et al. Experience and suggestion of medical practices for burns during the outbreak of COVID-19. Burns 2020, 46, 749–755. [Google Scholar] [CrossRef]
- Monte Soldado, A.; López-Masrramon, B.; Aguilera-Sáez, J.; Serracanta Domenech, J.; Collado Delfa, J.M.; Moreno Ramos, C.; Barret Nerin, J.P. Implementation and evaluation of telemedicine in burn care: Study of clinical safety and technical feasibility in a single burn center. Burns 2020, 46, 1668–1673. [Google Scholar] [CrossRef]
- Nischwitz, S.P.; Popp, D.; Sawetz, I.; Smolle, C.; Tuca, A.C.; Luze, H.; Kamolz, L.P. Burns in pandemic times—The Graz way towards COVID-19 and back. Burns 2021, 47, 234–239. [Google Scholar] [CrossRef]
- Saha, S.; Kumar, A.; Dash, S.; Singhal, M. Managing Burns During COVID-19 Outbreak. J. Burn. Care Res. 2020, 41, 1033–1036. [Google Scholar] [CrossRef]
- Tatar, R.; Enescu, D.M. The impact of COVID-19 pandemic on the activity of a pediatric burn center in Bucharest, Romania. Burns 2020, 46, 1977–1978. [Google Scholar] [CrossRef]
- Brewster, C.T.; Choong, J.; Thomas, C.; Wilson, D.; Moiemen, N. Steam inhalation and paediatric burns during the COVID-19 pandemic. Lancet 2020, 395, 1690. [Google Scholar] [CrossRef]
- Farroha, A. Effects of COVID-19 pandemic on burns epidemiology. Burns 2020, 46, 1466. [Google Scholar] [CrossRef] [PubMed]
- Kruchevsky, D.; Arraf, M.; Levanon, S.; Capucha, T.; Ramon, Y.; Ullmann, Y. Trends in Burn Injuries in Northern Israel during the COVID-19 Lockdown. J. Burn. Care Res. 2020, 42, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.; Reid, G.; Sack, A.; Heryet, R.; Mackie, I.; Sen, S.K. Changes in burn referrals and injuries during CoVid-19. Burns 2020, 46, 1469–1470. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.; Rogers, M.; Kissmer, N.; Du Preez, A.; Dufourq, N. Impact of lockdown measures implemented during the Covid-19 pandemic on the burden of trauma presentations to a regional emergency department in Kwa-Zulu Natal, South Africa. Afr. J. Emerg. Med. 2020, 10, 193–196. [Google Scholar] [CrossRef]
- Sayed, M.A.; Walsh, K.; Sheikh, Z. COVID-19 and the rise of the full ‘Fitness’ friction burn. Burns 2020, 46, 1717. [Google Scholar] [CrossRef]
- Rogers, A.D.; Cartotto, R. The impact of COVID-19 on burn care at a major regional burn centre. J. Burn. Care Res. 2021, 42, 110–111. [Google Scholar] [CrossRef]
- Sciarrillo, A.; Stella, M.; Bogetti, P. Burns during the epidemic, what changed? Burns 2021, 47, 1213–1214. [Google Scholar] [CrossRef]
- Sethuraman, U.; Stankovic, C.; Singer, A.; Vitale, L.; Krouse, C.B.; Cloutier, D.; Donoghue, L.; Klein, J.; Kannikeswaran, N. Burn visits to a pediatric burn center during the COVID-19 pandemic and ‘Stay at home’ period. Burns 2020, 47, 491–492. [Google Scholar] [CrossRef]
- Hamill, J.K.; Sawyer, M.C. Reduction of childhood trauma during the COVID-19 Level 4 lockdown in New Zealand. ANZ J. Surg. 2020, 90, 1242–1243. [Google Scholar] [CrossRef]
- Harris, D.; Ellis, D.Y.; Gorman, D.; Foo, N.; Haustead, D. Impact of COVID-19 social restrictions on trauma presentations in South Australia. Emerg. Med. Australas. 2020, 33, 152–154. [Google Scholar] [CrossRef]
- Christey, G.; Amey, J.; Campbell, A.; Smith, A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N. Z. Med. J. 2020, 133, 81–88. [Google Scholar] [PubMed]
- Jacob, S.; Mwagiru, D.; Thakur, I.; Moghadam, A.; Oh, T.; Hsu, J. Impact of societal restrictions and lockdown on trauma admissions during the COVID-19 pandemic: A single-centre cross-sectional observational study. ANZ J. Surg. 2020, 90, 2227–2231. [Google Scholar] [CrossRef] [PubMed]
- Kam, A.W.; Chaudhry, S.G.; Gunasekaran, N.; White, A.J.; Vukasovic, M.; Fung, A.T. Fewer presentations to metropolitan emergency departments during the COVID-19 pandemic. Med. J. Aust. 2020, 213, 370–371. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.S.; Teague, W.J. Childhood injury and injury prevention during COVID-19 lockdown—Stay home, stay safe? Injury 2021, 52, 1105–1107. [Google Scholar] [CrossRef] [PubMed]
- Probert, A.C.; Sivakumar, B.S.; An, V.; Nicholls, S.L.; Shatrov, J.G.; Symes, M.J.; Ellis, A.M. Impact of COVID-19-related social restrictions on orthopaedic trauma in a level 1 trauma centre in Sydney: The first wave. ANZ J. Surg. 2020, 91, 68–72. [Google Scholar] [CrossRef]
- RMIT ABC Fact Check. Josh Frydenberg Says Melbourne Is the World’s Most Locked Down City. Is That Correct? Available online: https://www.abc.net.au/news/2021-10-25/fact-check-is-melbourne-most-locked-down-city/100560172 (accessed on 8 February 2022).
- Department of Human Services. Trauma towards 2014: Review and Future Directions of the Victorian State Trauma System; Department of Human Services: Melbourne, Australia, 2009; Available online: https://www.health.vic.gov.au/sites/default/files/migrated/files/collections/policies-and-guidelines/t/trauma_towards_2014---pdf.pdf (accessed on 8 February 2022).
- Australian Bureau of Statistics. Socio-Economic Indexes for Areas (SEIFA). Available online: http://www.abs.gov.au/ausstats//mf/2039.0/.2013 (accessed on 8 February 2022).
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Wickham, H. Tidyverse: Easily Install and Load the ‘Tidyverse’, R Package Version 1.2.1. Available online: https://github.com/tidyverse/tidyverse (accessed on 27 January 2017).
- Grolemund, G.; Wickham, H. Dates and Times Made Easy with lubridate. J. Stat. Softw. 2011, 40, 1–25. [Google Scholar] [CrossRef]
- Yoshida, K.; Bartel, A. Tableone: Create ‘Table 1’ to Describe Baseline Characteristics with or without Propensity Score Weights. Available online: https://github.com/kaz-yos/tableone (accessed on 29 August 2022).
- Canty, A.; Ripley, B. Boot: Bootstrap R (S-Plus) Functions. R Package Version 1.3-25. Available online: https://cran.r-project.org/web/packages/boot/index.html (accessed on 29 August 2022).
- Davison, A.C.; Hinkley, D.V. Bootstrap Methods and Their Applications; Cambridge University Press: Cambridge, UK, 1997. [Google Scholar]
- Neuwirth, E. RColorBrewer: ColorBrewer Palettes, R Package Version 1.1-2. Available online: https://cran.r-project.org/web/packages/RColorBrewer/index.html (accessed on 29 August 2022).
- Wilke, C.O. Cowplot: Streamlined Plot Theme and Plot Annotations for ‘ggplot2’, R Package Version 0.9.4. Available online: https://cran.r-project.org/web/packages/cowplot/index.html (accessed on 22 August 2022).
- Mann, J.A.; Patel, N.; Bragg, J.; Roland, D. Did children ‘stay safe’? Evaluation of burns presentations to a children’s emergency department during the period of COVID-19 school closures. Arch. Dis. Child. 2020, 106, e18. [Google Scholar] [CrossRef]
- Williams, F.N.; Chrisco, L.; Nizamani, R.; King, B.T. COVID-19 related admissions to a regional burn center: The impact of shelter-in-place mandate. Burn. Open 2020, 4, 158–159. [Google Scholar] [CrossRef]
- Williams, F.N.; Nizamani, R.; Chrisco, L.; King, B.T. Increased Burn Center Admissions During COVID-19 Pandemic. J. Burn Care Res. 2020, 41, 1128. [Google Scholar] [CrossRef]
- Tracy, L.M.; Rosenblum, S.; Gabbe, B.J. Burns Registry of Australia and New Zealand (BRANZ) 2018/19 Annual Report; Department of Epidemiology and Preventive Medicine, Monash University: Melbourne, Australia, 2020. [Google Scholar]
- Cleland, H.; Greenwood, J.E.; Wood, F.M.; Read, D.J.; Wong She, R.; Maitz, P.; Castley, A.; Vandervord, J.G.; Simcock, J.; Adams, C.D.; et al. The Burns Registry of Australia and New Zealand: Progressing the evidence base for burn care. Med. J. Aust. 2016, 204, 195. [Google Scholar] [CrossRef]
- Moussa, A.; Lo, C.H.; Cleland, H. Burn wound excision within 24 h: A 9-year review. Burns 2021, 47, 1300–1307. [Google Scholar] [CrossRef] [PubMed]
- Stathakis, V.; Berecki-Gisolf, J. Epidemiological Profile of Hospitalised Unintentional Home Injuries Immediately Prior and during the COVID-19 Pandemic in Victoria, January 2019—December 2020. Hazard Edition 89; Victorian Injury Surveillance Unit, Monash University Accident Research Centre: Melbourne, Australia, 2021; Available online: https://www.monash.edu/__data/assets/pdf_file/0011/2754884/Hazard-89_FINALweb-v2.pdf (accessed on 1 April 2022).
| Pre-COVID-19 Period (2016–2019) | COVID-19 Lockdowns (2020) | p | |
|---|---|---|---|
| Number of patients | 155 | 28 | |
| Age, median (IQR) years | 2 (1–7) | 2 (1–11) | 0.95 |
| Male | 99 (64%) | 16 (57%) | 0.64 |
| Primary cause | 0.005 | ||
| Scald | 83 (54%) | 17 (61%) | |
| Flame | 26 (17%) | 10 (36%) | |
| Other cause | 45 (29%) | <5 | |
| Activity when injury occurred | 0.56 | ||
| Near person preparing food | 46 (32%) | 11 (41%) | |
| Playing | 58 (41%) | 11 (41%) | |
| Other activity | 39 (27%) | 5 (18%) | |
| IRSAD quintile | 0.45 | ||
| 1 (most disadvantaged) | 40 (26%) | ||
| 2 | 36 (23%) | ||
| 3 | 23 (15%) | ||
| 4 | 27 (18%) | ||
| 5 (least disadvantaged) | 27 (18%) | ||
| Injury occurred in home | 118 (78%) | 22 (79%) | 0.99 |
| Unintentional injury | 152 (98%) | 27 (96%) | 0.99 |
| Time to admission, median (IQR) hours | 49 (3–281) | 2 (1–32) | <0.001 |
| Admission source | 0.003 | ||
| Scene via ambulance | 35 (22%) | 15 (54%) | |
| Other hospital | 46 (30%) | 5 (18%) | |
| Outpatient department | 60 (39%) | <5 | |
| Other source | 14 (9%) | <5 | |
| TBSA burned, median (IQR)% | 6 (2–8) | 9 (5–16) | 0.002 |
| TBSA group | 0.003 | ||
| 0–4.9% | 68 (44%) | 7 (25%) | |
| 5–9.9% | 56 (37%) | 9 (33%) | |
| 10–19.9% | 23 (15%) | 6 (21%) | |
| ≥20% | 6 (4%) | 6 (21%) | |
| Deep dermal or FT burn | 78 (70%) | 20 (70%) | 0.79 |
| Inhalation injury | <5 | 5 (18%) | <0.001 |
| Burn wound management in theatre | 114 (74%) | 21 (75%) | 0.99 |
| Time to first procedure, median (IQR) days | 7 (2–15) | 1 (0–3) | <0.001 |
| Received skin graft | 67 (59%) | 7 (33%) | 0.06 |
| Time to first skin graft, median (IQR) days | 15 (9–18) | 16 (13–17) | 0.58 |
| Admitted to ICU | 9 (6%) | 9 (32%) | <0.001 |
| ICU LOS, median (IQR) hours | 111 (89–231) | 589 (130–1080) | 0.12 |
| Discharged to home/usual residence | 148 (96%) | 23 (82%) | 0.03 |
| Hospital LOS, median (IQR) days) | 2 (1–5) | 8 (2–16) | <0.001 |
| Pre-COVID-19 Period (2016–2019) | COVID-19 Lockdowns (2020) | p | |
|---|---|---|---|
| Number of patients | 540 | 160 | |
| Age, median (IQR) years | 41 (27–57) | 40 (27–54) | 0.64 |
| Male | 399 (74%) | 122 (76%) | 0.62 |
| Primary cause | 0.005 | ||
| Scald | 126 (23%) | 39 (25%) | |
| Flame | 320 (60%) | 102 (64%) | |
| Other cause | 90 (17%) | 18 (11%) | |
| Activity when injury occurred | 0.003 | ||
| Cooking and/or preparing food/drink | 89 (17%) | 28 (19%) | |
| Leisure or sports activity | 86 (17%) | 17 (11%) | |
| Other household duties/maintenance | 71 (14%) | 20 (14%) | |
| Sleeping or resting | 60 (11%) | 10 (7%) | |
| Other activity | 131 (25%) | 55 (37%) | |
| IRSAD quintile | 0.08 | ||
| 1 (most disadvantaged) | 88 (17%) | 26 (17%) | |
| 2 | 97 (18%) | 37 (24%) | |
| 3 | 118 (23%) | 24 (15%) | |
| 4 | 103 (20%) | 41 (27%) | |
| 5 (least disadvantaged) | 114 (22%) | 27 (17%) | |
| Injury occurred in home | 290 (57%) | 110 (73%) | <0.001 |
| Unintentional injury | 511 (95%) | 148 (93%) | 0.42 |
| Time to admission, median (IQR) hours | 9 (2–63) | 5 (2–21) | 0.03 |
| Admission source | 0.43 | ||
| Scene via ambulance | 198 (37%) | 62 (39%) | |
| Other hospital | 250 (46%) | 75 (47%) | |
| Outpatient department | 21 (4%) | < 5 | |
| Other source | 71 (13%) | 21 (13%) | |
| TBSA burned, median (IQR)% | 4 (2–8) | 5 (2–10) | 0.007 |
| TBSA group | 0.03 | ||
| 0–4.9% | 297 (55%) | 73 (46%) | |
| 5–9.9% | 131 (24%) | 37 (23%) | |
| 10–19.9% | 64 (12%) | 33 (21%) | |
| ≥20% | 46 (9%) | 15 (10%) | |
| Deep dermal or FT burn | 297 (56%) | 89 (56%) | 0.95 |
| Inhalation injury | 24 (5%) | 14 (9%) | 0.05 |
| Burn wound management in theatre | 387 (72%) | 122 (76%) | 0.23 |
| Time to first procedure, median (IQR) days | 3 (1–6) | 2 (1–5) | 0.05 |
| Received skin graft | 299 (78%) | 96 (79%) | 0.83 |
| Time to first skin graft, median (IQR) days | 5 (3–8) | 4 (3–8) | 0.56 |
| Admitted to ICU | 83 (15%) | 42 (26%) | 0.002 |
| ICU LOS, median (IQR) hours | 46 (23–169) | 145 (34–336) | 0.03 |
| Discharged to home/usual residence | 290 (54%) | 85 (53%) | 0.90 |
| Hospital LOS, median (IQR) days) | 7 (3–13) | 9 (5–17) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tracy, L.M.; Lo, C.H.; Cleland, H.J.; Teague, W.J.; Gabbe, B.J. Early Impact of COVID-19 Pandemic on Burn Injuries, Admissions, and Care in a Statewide Burn Service. Eur. Burn J. 2022, 3, 447-456. https://doi.org/10.3390/ebj3030039
Tracy LM, Lo CH, Cleland HJ, Teague WJ, Gabbe BJ. Early Impact of COVID-19 Pandemic on Burn Injuries, Admissions, and Care in a Statewide Burn Service. European Burn Journal. 2022; 3(3):447-456. https://doi.org/10.3390/ebj3030039
Chicago/Turabian StyleTracy, Lincoln M., Cheng Hean Lo, Heather J. Cleland, Warwick J. Teague, and Belinda J. Gabbe. 2022. "Early Impact of COVID-19 Pandemic on Burn Injuries, Admissions, and Care in a Statewide Burn Service" European Burn Journal 3, no. 3: 447-456. https://doi.org/10.3390/ebj3030039
APA StyleTracy, L. M., Lo, C. H., Cleland, H. J., Teague, W. J., & Gabbe, B. J. (2022). Early Impact of COVID-19 Pandemic on Burn Injuries, Admissions, and Care in a Statewide Burn Service. European Burn Journal, 3(3), 447-456. https://doi.org/10.3390/ebj3030039








