1. Introduction
The National Burn Care Review in 2001 led to reformatting of the delivery of burn care throughout Great Britain, with varying levels of specialist care offered throughout regional networks [
1,
2,
3]. Our trust was designated as a burns facility, providing the first tier of specialist burn care, i.e., up to 10% TBSA in adults, and up to 5% TBSA in children. More complex injuries, including major burns requiring intravenous fluid resuscitation, are escalated to burns unit or burns centre care as appropriate [
4].
Major burn injuries can have a significant number of sequelae, with respiratory compromise not least amongst them [
5]. This is one reason why burns units or centres must work closely with intensive care units (ICUs), as advanced respiratory support may be required [
2]. In some instances, however, the acute respiratory distress syndrome (ARDS) that results from some major burn injuries (for example from airway injuries, parenchymal injury or systemic toxicity) [
6] leaves patients requiring higher levels of support than many ICUs are able to provide. This support comes in the form of extracorporeal membrane oxygenation (ECMO), which was first established in our trust in 1989 [
7]. This service was initially set up for children but progressed to provide ECMO care to adults as well [
8].
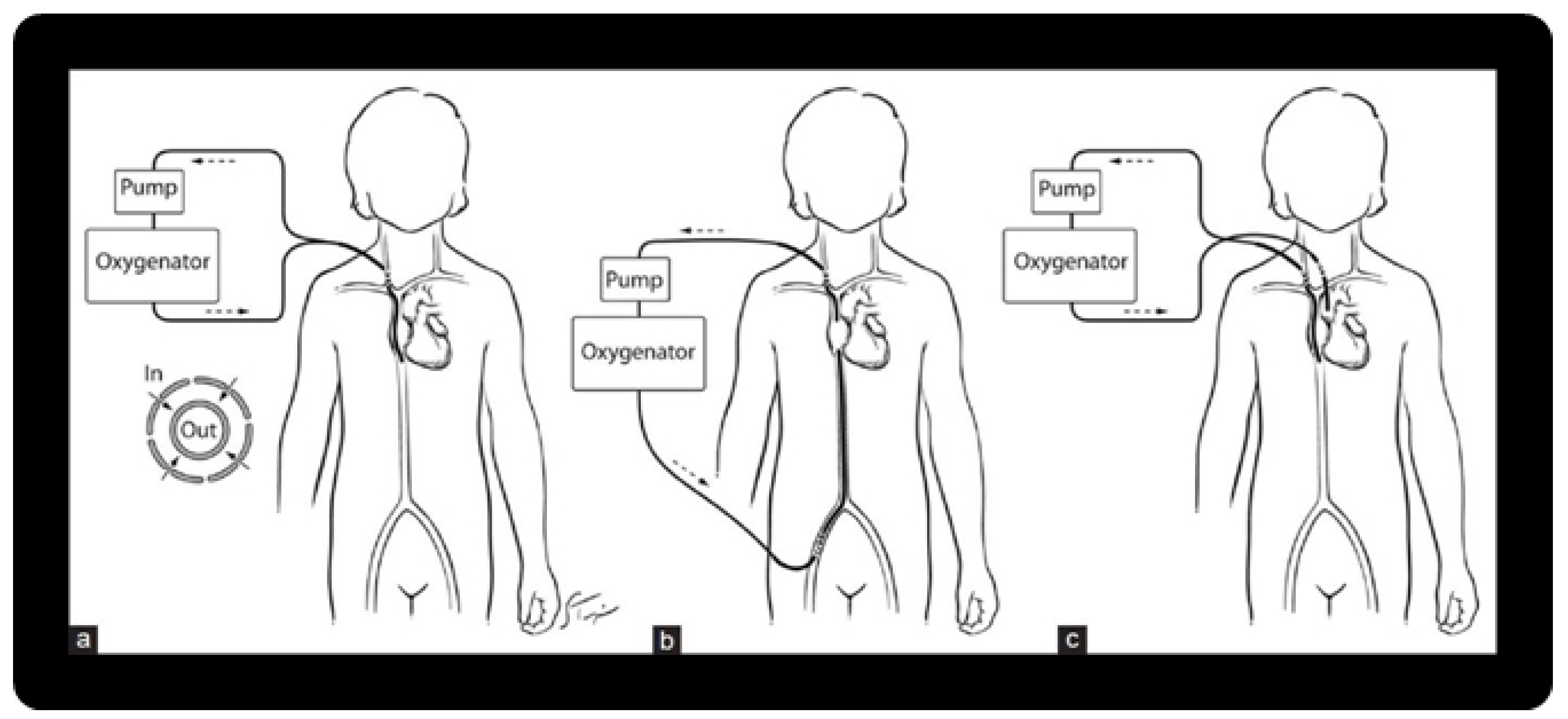
ECMO is a form of extracorporeal life support, with external respiratory support, with or without cardiac support. Veno-arterial ECMO bypasses the heart, providing support for both, as blood is removed from the body from a vein and returned in an artery. Veno-venous ECMO provides respiratory support only, as blood is removed and returned to the body via a vein. As such, veno-venous ECMO requires adequate cardiac function in the patient. A visual aid for this is shown in
Figure 1 [
9,
10].
Since then, a number of other ECMO centres have developed. Some of these are co-located with a burns and plastic surgery service within their trusts, and the majority of these are burns centres. Similarly, not all burns centres are co-located with an ECMO centre. Our trust is relatively unique in providing the highest level of respiratory support, but only the first tier of specialist burns care. Anecdotally, our service had been aware of major burns patients being transferred to our trust for ECMO, and our team cared for these whilst inpatients at our trust. As such, we set out to formally review this area, and assess if we were able to provide suitable care for these extreme cases.
2. Methods
Over a 10-year period (2011–2021), patients with cutaneous burns requiring ECMO were identified from the International Burn Injury Database (iBID) and the Extracorporeal Life Support Organization (ELSO) database, as well as departmental diaries. Case notes and letters for these patients were then reviewed and data was collated.
This provided us with a series of five patients, all adults. More patients with inhalational injuries were identified, but these were not included in this review as they had no cutaneous burns.
3. Results
3.1. Case 1
A 53-year-old female who suffered flame burns after her nightdress caught fire in 2011. The injury was calculated as 25% total body surface area (% TBSA) full thickness injury, and 22.5% TBSA partial thickness injury (overall 47.5% TBSA).
This patient was initially managed in a burns unit in the south of the country, with debridement and application of split-thickness skin grafts and allograft. Unfortunately, the patient underwent a respiratory decline, felt to be due to ARDS, or possibly sepsis originating from her chest. As a result of recurrent hypoxaemia, the patient was transferred to our trust on day 18. A trial of high frequency oscillatory ventilation (HFOV) provided limited benefit, and so the patient was commenced on veno-venous ECMO the following day.
After a slow progression, the patient was decannulated on day 43 after injury and repatriated a few days later. Unfortunately, the patient subsequently deteriorated again, developing respiratory failure, felt to be due to a lower respiratory tract infection. At this stage a second run of ECMO was considered futile, due to the prolonged initial course, and the patient passed away.
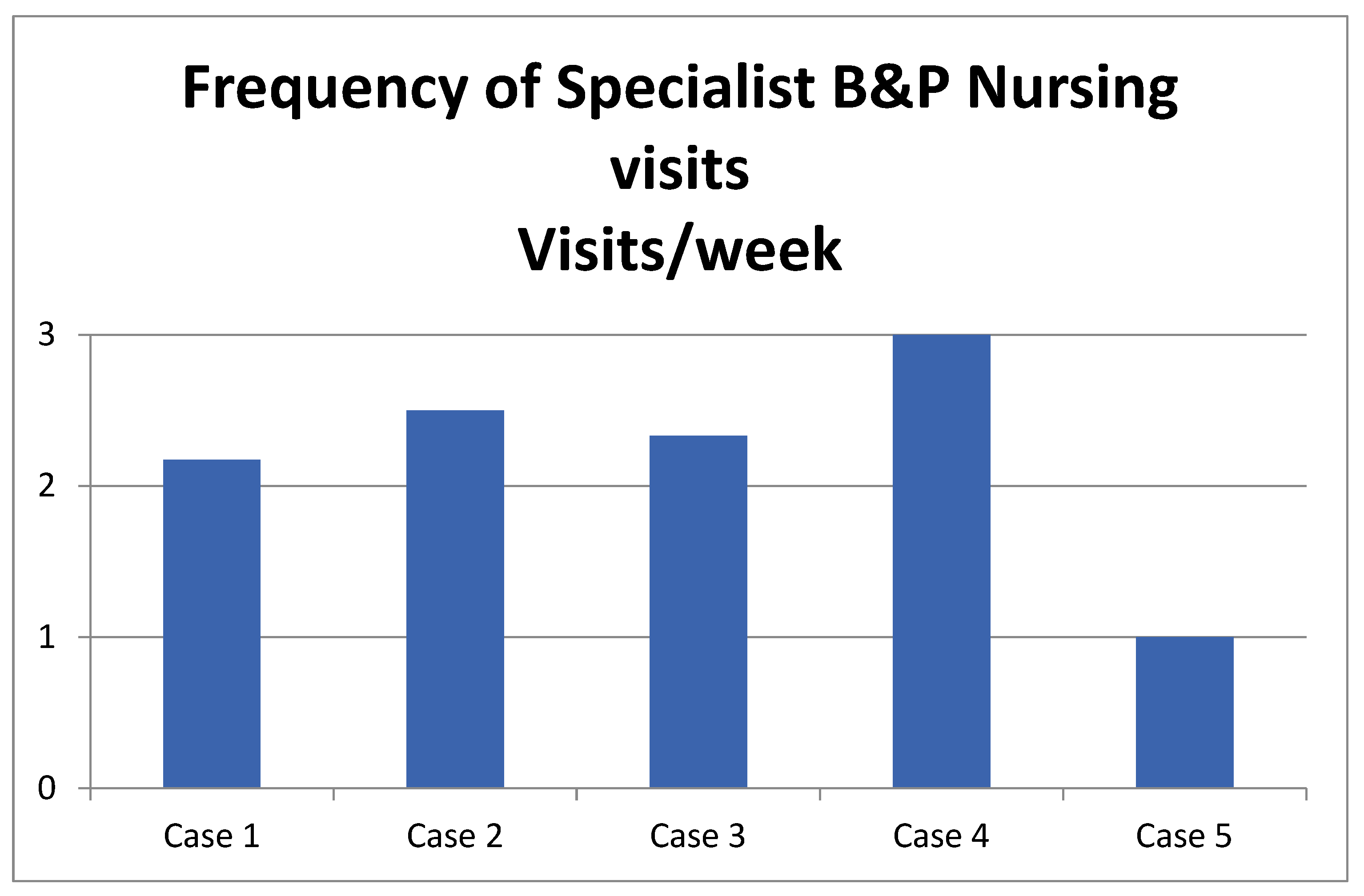
During her 29-day inpatient stay, this patient received nine reviews by specialist burns and plastic surgery nurses. Dressing changes took between 2 and 3 h each time. Generally, this would require two specialist nurses. Close contact was kept with the referring centre for discussion regarding wound healing and dressing choices.
3.2. Case 2
A 23-year-old male suffered flame burns in a house fire in 2012. The injury was calculated as 30% TBSA deep-dermal and full-thickness injuries.
The patient was first admitted and managed in a burn centre in the northwest of the country and had wound cleansing and dressing changes in an operating theatre twice. This patient developed ARDS, as a result of either smoke inhalation or direct thermal airway injury, with rapid respiratory decline, and was transferred to our trust for veno-venous ECMO on day 3 after the injury. The patient initially improved, however a trial off ECMO was unsuccessful. Further deterioration necessitated conversion to veno-arterial ECMO, during which the patient had a short cardiac arrest. Unfortunately, the patient developed an acute abdomen, which was felt to be a pre-terminal event, and care was withdrawn on day 17 after injury. The patient passed away shortly after.
During a 14-day inpatient stay, this patient received five reviews by specialist burns and plastic surgery nurses, and each dressing change took between 2 to 3 h, with two specialist nurses.
3.3. Case 3
A 46-year-old male who suffered flame burns after being caught in a car fire. On assessment, the injury was calculated at 9% TBSA full-thickness, and 6% TBSA partial-thickness injuries (overall 15% TBSA).
Initial management was undertaken at the burns unit in the midlands, who instigated HFOV for ARDS with rapid respiratory decline. There was minimal improvement from this, and so the patient was transferred to our trust for veno-venous ECMO on day 2 after the injury. Despite enduring an episode of suspected sepsis, the patient did improve, and was de-cannulated on day 17 after the injury, and successfully repatriated the following day.
During his 18-day inpatient stay, this patient received eight reviews by specialist burns and plastic surgery nurses. This did include two “outreach” reviews by the specialist nursing team from the referring trust attending in person to support dressing changes. Each dressing change took between 2 and 3 h, requiring two specialist nurses.
3.4. Case 4
A 40-year-old female sustained flame burns after being exposed to a house fire caused by an explosion. The patient was assessed as having 2% TBSA full thickness, and 40% TBSA partial thickness burns (overall 42% TBSA).
The patient was initially managed at the burns centre in the north of the country, where the blisters were debrided, and wounds cleansed. Day 4 after injury saw the patient deteriorate with severe hypoxia, felt to be due to an inhalational injury. Local interventions were unsuccessful, and so the patient was transferred to our trust for veno-venous ECMO on day 5. Fortunately, the patient recovered quickly, and on day 9 was decannulated and subsequently repatriated.
During her 6-day inpatient stay, this patient was reviewed three times by specialist burns and plastic surgery nurses. Dressing changes for this patient required two specialist nurses and took around 2 to 3 h each time.
3.5. Case 5
A 57-year-old male sustained flame burns from a pan for deep-fat frying potatoes. The patient was assessed as having 37% TBSA full thickness, and 2% TBSA partial thickness burns (overall 39% TBSA).
This patient was initially managed at the burns centre in the midlands, where he underwent tangential excision and split thickness skin grafting from day 2 after the injury. By day 8, the patient developed a ventilator-associated pneumonia (VAP), superimposed on ARDS. The patient was transferred to our trust for veno-venous ECMO on day 11. The patient recovered quickly, and was decannulated on day 16, before repatriation to the burns unit in the midlands on day 18. He was subsequently repatriated to our trust for physiotherapy and rehabilitation, as he is a local resident. He has since been discharged to the community.
During his 7-day inpatient stay in the ECMO unit, this patient received one review by the specialist burns and plastic surgery nursing team. A subsequent dressing change was due to take place on day 7, but the patient was transferred out of the trust, and dressings attended to following discharge. His dressing change took between 2 and 3 h, and required two specialist nurses, as well as specialist nurses outreaching in person from the regional burns unit. He has healed well.
Of our patients, three survived to hospital discharge (60%), one survived until repatriation, but passed away before discharge home (20%) and one patient did not survive (20%).
The frequency of nursing visits is shown in
Figure 2. A summary of the details and variables of each case is shown in
Table 1.
4. Discussion
A systematic review and meta-analysis were conducted in 2012 by Asmussen et al. on a low number of studies with small patient cohorts. The salient points of this were a rate of 0.542 burn injury patients who survived hypoxaemic respiratory failure on ECMO therapy, with a range from 0.404 to 0.641. In addition, an ECMO run time of less than 200 h conferred a greater chance of survival compared to over 200 h. No difference in mortality was identified between patients who had PaO
2/FiO
2 ratios of more or less than 60 mmHg at the time of initiation of ECMO. Scald burns seem to show a higher tendency for survival compared to flame burns [
11]. This correlates to a number of other papers published over the last 25 years, from a variety of settings, quoting survival rates of 28% to 87.5% in adults. These were all small volume cohorts [
12,
13,
14,
15,
16,
17,
18,
19,
20,
21].
One paper by Hsu et al. reported an overall survival rate of 16.7% in six patients following battlefield explosion injuries. All mortalities had over 90% TBSA injuries. The single survivor had an injury covering a TBSA of 50% [
22].
Kennedy et al. described two burn patients requiring ECMO for ARDS. Both patients survived [
23]. Thompson et al. also described two similar patients surviving [
24].
A report by O’Toole et al. from our trust in 1998 described two paediatric cases requiring ECMO. One smoke inhalation only, the other with smoke inhalation in addition to cutaneous burns. Both patients survived to full recovery [
25]. Lessin et al. reported two paediatric major burn patients requiring ECMO surviving to discharge [
26].
For paediatric cases, similar papers have been published, quoting survival rates between 53% and 67% [
27,
28,
29,
30].
In a review of 39 burn centres in North America, Hebert et al. found that 79.5% reported the use of ECMO in any capacity for their burn patients, and 51.3% utilised it for ARDS or respiratory failure. Of those using ECMO for respiratory compromise, only 20% of centres utilised ECMO in more than one patient a year. They explain that limited evidence for ECMO use in burn patients, in addition to few suitable patients and lack of experience, were the most commonly reported barriers to more widespread utilisation of ECMO in the care of severe burn patients. As a result, they conclude that an improvement in collaboration and communication would be required to allow standardization of patient care, as well as to drive research [
31].
Of the five patients presented here, one died while receiving ECMO, while another died after repatriation. The other three patients (60%) survived to discharge.
The ECMO centre and the burns service in our trust are located at different sites which, though they are nearby, provides an added complication when supporting the care of these patients. In addition, due to our designation as a burns facility, the care of larger burns such as these would not normally fall within our remit, and hence is not accounted for when planning the routine commitments of our team members. As a result, when these cases do occur, it introduces a “surge” requirement on our staff, both in time and skills.
The specialist burns and plastic surgery nurse practitioners in our trust have undertaken extra qualifications, to ensure we are providing the highest level of care we can. 100% of the burns and plastics specialist nursing team has undertaken a post registration certified qualification in burns and plastics at degree or masters level. In addition to this, 70% have undertaken the Emergency Management of Severe Burns course (as delivered by the British Burns Association). Our burns service may be at facility level; however, the expertise of the nursing and therapy teams enabled us to care for these complex patients on the ECMO unit.
5. Conclusions
ARDS is a well-recognised sequela of major burn injuries. The use of ECMO in managing this has been reviewed in various set-ups internationally for many years and is a valid treatment option that may improve survival in patients who fail to respond to other forms of respiratory or ventilatory support. The complexity of these patients, however, should prompt a multidisciplinary approach to their intensive management to agree upon those patients who are appropriate. As seen by Hsu et al., substantial % TBSA injuries can reduce the survival rate of cutaneous burn patients receiving ECMO [
22]. Such variety in survival rates should be considered during the multidisciplinary team discussions and management of these patients, and may warrant further investigation in the future, to perhaps better quantify this relationship.
Our trust is relatively unique in providing the highest level of respiratory support (ECMO), with co-location of a specialised burn service, albeit at facility level, for both adult and paediatric patients. Our department can conclude that such patients are uncommon, but that provision of satisfactory specialist burns care was achieved. The difficulties encountered were primarily due to the cross-site cover and requirements beyond regular clinical commitments, which often meant changes in nurses’ commitment schedules. As such, adjustments or “surge-planning” will continue to be considered in case of similar eventualities in the future, to ensure optimum care is maintained in future patients. The support of our regional burns network by surgeons and specialist nurses was invaluable in preserving ideal care in these cases.
Given the highly specialised nature of burn care, as well as provision of ECMO, and the limited number of units providing this, formal review of these set-ups within the Great Britain should be undertaken, to allow for a consensus on how, and where, these patients would be most appropriately managed. Suitable training to the members of burns teams co-located with ECMO centres should be ensured. Coordination between the ECMO & burns networks, to explore training, assistance and, perhaps, outreach of the ECMO service to the higher-level burn centre should be discussed, so agreements can be made and policies put in place in preparation for such patients presenting in the future.
Formal review, on a national level, of the delivery of ECMO care in patients with cutaneous burns would also be of benefit, to allow more accurate comments on the impact on outcomes, including survival, infections, scarring, and psychological state. Such a review could also assess the impact of other organ support, such as renal replacement therapy, that is administered concurrently.
Author Contributions
Conceptualization, S.F., A.D. and R.A.; methodology, S.F., L.D., C.P. and R.A.; software, L.D.; validation, S.F., L.D., C.P. and R.A.; formal analysis, S.F.; investigation, S.F.; resources, S.F.; data curation, S.F.; writing—original draft preparation, S.F.; writing—review and editing, S.F., L.D., C.P., A.D. and R.A.; visualization, S.F. and R.A.; supervision, R.A.; project administration, S.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank the ECMO unit at Glenfield Hospital, Leicester, for their assistance in acquiring and accessing notes for data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- National Burn Care Review Committee. Standards and Strategy for Burn Care: A Review of Burn Care in the British Isles; UK, 2001; Available online: https://www.britishburnassociation.org/national-burn-care-review/ (accessed on 15 December 2021).
- NHS Commissioning Board. NHS Standard Contract for Specialised Burns Care (All Ages); UK, 2013; Available online: https://www.england.nhs.uk/wp-content/uploads/2014/04/d06-spec-burn-care-0414.pdf (accessed on 15 December 2021).
- National Network for Burn Care. National Burn Care Standards; UK, 2013; Available online: https://www.mcctn.org.uk/publications.html (accessed on 15 December 2021).
- Clinical Advisory Group (CAG) of Midland Burn ODN. Midland Burn ODN Referral Guidelines; UK, 2019; Available online: https://www.mcctn.org.uk/emergency-care.html (accessed on 15 December 2021).
- Australia and New Zealand Burns Association. Emergency Management of Severe Burns Course Manual, 16th ed.; Australia and New Zealand, 2016; Available online: https://anzba.org.au/education/emsb/ (accessed on 9 December 2021).
- Jones, S.W.; Williams, F.N.; Cairns, B.A.; Cartotto, R. Inhalation Injury: Pathophysiology, Diagnosis, and Treatment. Clin. Plast. Surg. 2017, 44, 505–511. [Google Scholar] [CrossRef]
- Czapran, A.; Steel, M.; Barrett, N.A. Extra-corporeal membrane oxygenation for severe respiratory failure in the UK. J. Intensive Care Soc. 2019, 21, 247–255. [Google Scholar] [CrossRef] [PubMed]
- NHS England. Extra Corporeal Membrane Oxygenation (ECMO) for Respiratory Failure in Adults—Service Specification; 2019; Available online: https://www.england.nhs.uk/wp-content/uploads/2019/02/Adult-ECMO-Service-Specification.pdf (accessed on 15 December 2021).
- Extracorporeal Life Support Organization. What Is ECMO? 2021. Available online: https://www.elso.org/Resources/WhatisECMO.aspx (accessed on 8 September 2021).
- Extracorporeal Life Support Organization. Types of ECMO. 2021. Available online: https://www.elso.org/Resources/TypesofECMO.aspx (accessed on 8 September 2021).
- Asmussen, S.; Maybauer, D.M.; Fraser, J.F.; Jennings, K.; George, S.; Keiralla, A.; Maybauer, M.O. Extracorporeal membrane oxygenation in burn and smoke inhalation injury. Burns 2013, 39, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.-J.; Ma, H.; Liao, W.-C.; Shih, Y.-C.; Chen, M.-C.; Shih, C.-C.; Chen, T.-W.; Perng, C.-K. Extracorporeal membrane oxygenation support may be a lifesaving modality in patients with burn and severe acute respiratory distress syndrome: Experience of Formosa Water Park dust explosion disaster in Taiwan. Burns 2018, 44, 118–123. [Google Scholar] [CrossRef]
- Burke, C.R.; Chan, T.; McMullan, D.M. Extracorporeal Life Support Use in Adult Burn Patients. J. Burn. Care Res. 2017, 38, 174–178. [Google Scholar] [CrossRef]
- Ainsworth, C.R.; Dellavolpe, J.; Chung, K.K.; Cancio, L.C.; Mason, P. Revisiting extracorporeal membrane oxygenation for ARDS in burns: A case series and review of the literature. Burns 2018, 44, 1433–1438. [Google Scholar] [CrossRef]
- Szentgyorgyi, L.; Shepherd, C.; Dunn, K.W.; Fawcett, P.; Barker, J.M.; Exton, P.; Maybauer, M.O. Extracorporeal membrane oxygenation in severe respiratory failure resulting from burns and smoke inhalation injury. Burns 2018, 44, 1091–1099. [Google Scholar] [CrossRef]
- Dadras, M.; Wagner, J.M.; Wallner, C.; Huber, J.; Buchwald, D.; Strauch, J.; Harati, K.; Kapalschinski, N.; Behr, B.; Lehnhardt, M. Extracorporeal membrane oxygenation for acute respiratory distress syndrome in burn patients: A case series and literature update. Burn. Trauma 2019, 7, 28. [Google Scholar] [CrossRef] [Green Version]
- Eldredge, R.S.; Zhai, Y.; Cochran, A. Effectiveness of ECMO for burn-related acute respiratory distress syndrome. Burns 2019, 45, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Soussi, S.; Gallais, P.; Kachatryan, L.; Benyamina, M.; Ferry, A.; Cupaciu, A.; Chaussard, M.; Maurel, V.; Chaouat, M.; Mimoun, M.; et al. Extracorporeal membrane oxygenation in burn patients with refractory acute respiratory distress syndrome leads to 28% 90-day survival. Intensive Care Med. 2016, 42, 1826–1827. [Google Scholar] [CrossRef]
- Chou, N.-K.; Chen, Y.-S.; Ko, W.-J.; Huang, S.-C.; Chao, A.; Jan, G.-J.; Lin, F.-Y.; Wang, S.-S.; Chu, S.-H. Application of Extracorporeal Membrane Oxygenation in Adult Burn Patients. Artif. Organs 2001, 25, 622–626. [Google Scholar] [CrossRef]
- Nosanov, L.B.; McLawhorn, M.M.; Cruz, M.V.; Chen, J.H.; Shupp, J.W. A National Perspective on ECMO Utilization Use in Patients with Burn Injury. J. Burn. Care Res. 2017, 39, 10–14. [Google Scholar]
- Zhang, Y.H.; Guo, G.H.; Shen, G.L.; Han, W.; Zhao, X.Y.; Lin, W.; Huang, C.H.; Xu, J.; Fan, S.W.; Qian, H.G. Analysis on treatment of extremely severe burn patients with severe inhalation injury in August 2nd Kunshan factory aluminum dust explosion accident. Chin. J. Burn. 2018, 34, 455–458. [Google Scholar]
- Hsu, P.-S.; Tsai, Y.-T.; Lin, C.-Y.; Chen, S.-G.; Dai, N.-T.; Chen, C.-J.; Chen, J.-L.; Tsai, C.-S. Benefit of extracorporeal membrane oxygenation in major burns after stun grenade explosion: Experience from a single military medical center. Burns 2017, 43, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J.D.; Thayer, W.; Beuno, R.; Kohorst, K.; Kumar, A.B. ECMO in major burn patients: Feasibility and considerations when multiple modes of mechanical ventilation fail. Burn. Trauma 2017, 5. [Google Scholar] [CrossRef] [Green Version]
- Thompson, J.T.; Molnar, J.A.; Hines, M.H.; Chang, M.C.; Pranikoff, T. Successful management of adult smoke inhalation with extracorporeal membrane oxygenation. J. Burn Care Rehabil. 2005, 26, 62–66. [Google Scholar] [CrossRef]
- O’Toole, G.; Peek, G.; Jaffe, W.; Ward, D.; Henderson, H.; Firmin, R.K. Extracorporeal membrane oxygenation in the treatment of inhalation injuries. Burns 1998, 24, 562–565. [Google Scholar] [CrossRef]
- Lessin, M.S.; el-Eid, S.E.; Klein, M.D.; Cullen, M.L. Extracorporeal membrane oxygenation in pediatric respiratory failure secondary to smoke inhalation injury. J. Pediatr. Surg. 1996, 31, 1285–1287. [Google Scholar] [CrossRef]
- Askegard-Giesmann, J.R.; Besner, G.E.; Fabia, R.; Caniano, D.A.; Preston, T.; Kenney, B.D. Extracorporeal membrane oxygenation as a lifesaving modality in the treatment of pediatric patients with burns and respiratory failure. J. Pediatr. Surg. 2010, 45, 1330–1335. [Google Scholar] [CrossRef] [PubMed]
- Kane, T.D.; Greenhalgh, D.G.; Warden, G.D.; Goretsky, M.J.; Ryckman, F.C.; Warner, B.W. Pediatric burn patients with respiratory failure: Predictors of outcome with the use of extracorporeal life support. J. Burn Care Rehabil. 1999, 20, 145–150. [Google Scholar] [CrossRef]
- Goretsky, M.J.; Greenhalgh, D.G.; Warden, G.D.; Ryckman, F.C.; Warner, B.W. The use of extracorporeal life support in pediatric burn patients with respiratory failure. J. Pediatr. Surg. 1995, 30, 620–623. [Google Scholar] [CrossRef]
- Pierre, E.J.; Zwischenberger, J.B.; Angel, C.; Upp, J.; Cortiella, J.; Sankar, A.; Herndon, D.N. Extracorporeal membrane oxygenation in the treatment of respiratory failure in pediatric patients with burns. J. Burn Care Rehabil. 1998, 19, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Hebert, S.; Erdogan, M.; Green, R.S.; Rasmussen, J. The Use of Extracorporeal Membrane Oxygenation in Severely Burned Patients: A Survey of North American Burn Centers. J. Burn Care Res. 2021, irab103. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).