Community Response to Burn Injuries: Examples from Dhading District of Nepal
Abstract
:1. Background
2. Materials and Methods
3. Results
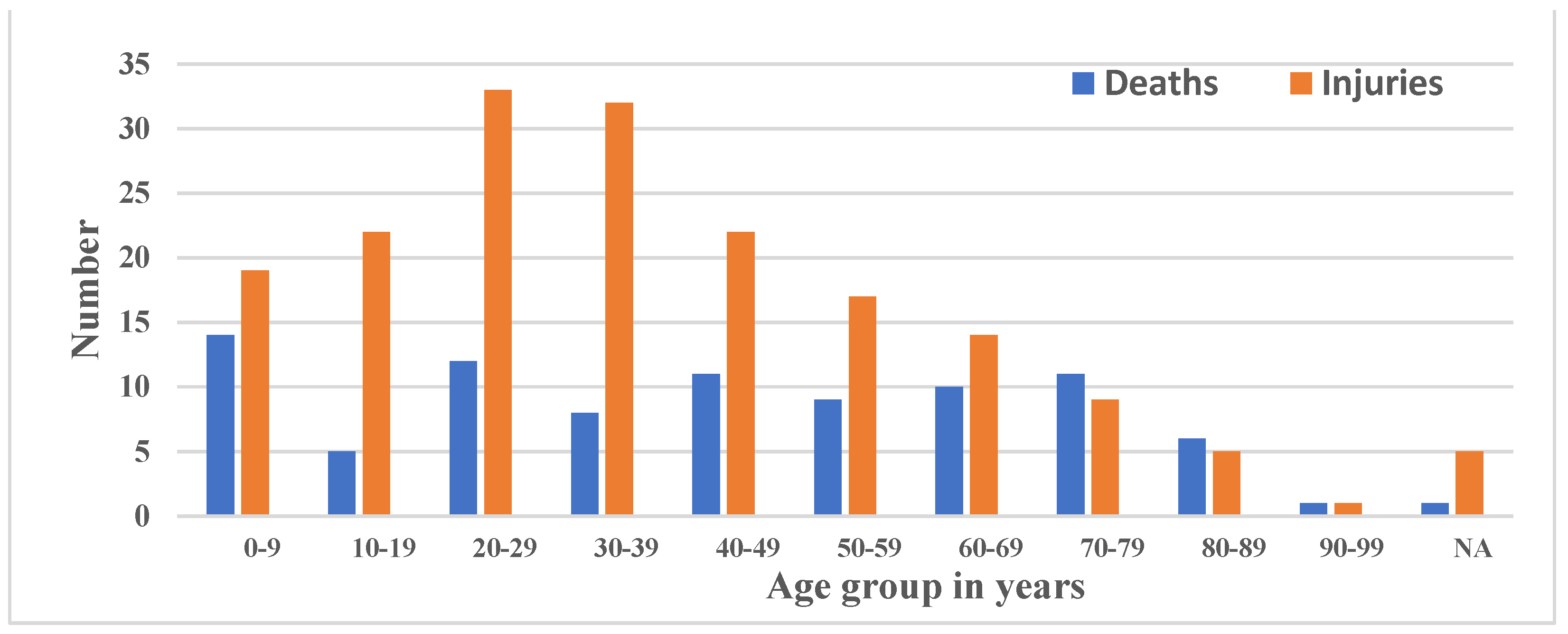
3.1. Situation of Burn Injuries and Deaths in Nepal
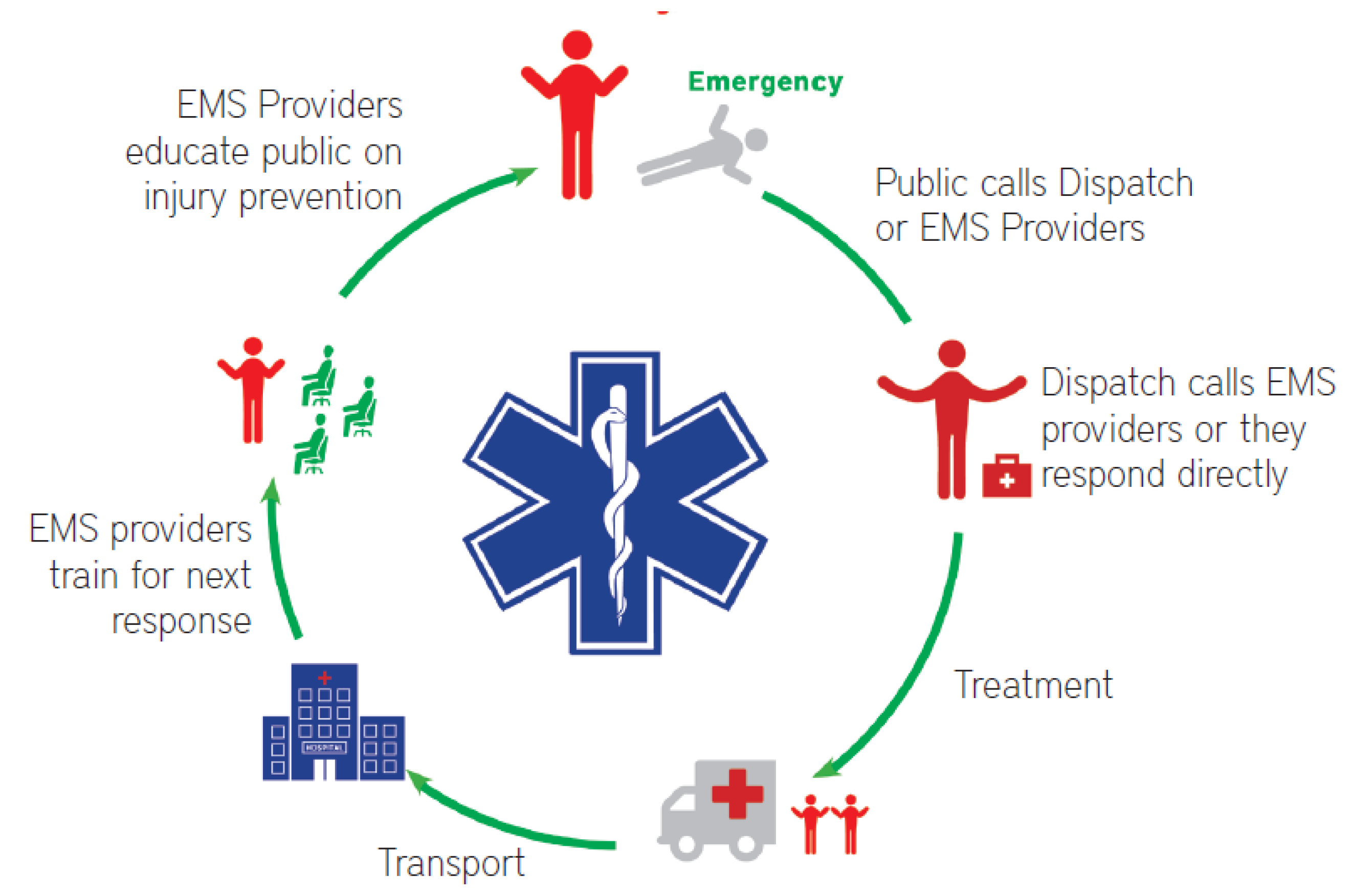
3.2. Emergency Medical Services (EMS)
3.2.1. Training for RFR
| Day 1, 8 h |
| Lesson 1: Introduction, Objectives, Emergency Communication Center, Pre-test, First Aid, RFR, EMS, Patients’ communication, and Roles and Responsibilities of RFR. |
| Lesson 2: Patient Assessment System, Hands-on Approach, and Practical Skills. |
| Lesson 3: Life Threats, triage, hemorrhage control, shock, Airway issues, Rescue Breathing, CPR, and day conclusion, Life Threats, Open Pneumothorax, Tension Pneumothorax, and Seizures. |
| Day 2, 8 h |
| Lesson 4: Musculoskeletal Injury, Head Injury, Spinal Injury, Muscle & Ligament Injury, Bone, Burns, Blisters, Crush Injury, Eye Injuries, and Dental Emergencies. |
| Lesson 5: Medical Illness, Cardiac Illness, Stroke, Respiratory Illness, Abdominal Problems, Constipation, Diarrhea, Nausea & Vomiting, Allergic, Reaction, Diabetes, Hypoglycemia & Hypoglycemia, Scenario, and Day’s Conclusion. |
| Day 3, 8 h |
| Lesson 6: Environmental Topics, Heat Illness, Hypothermia, Frostbite, High Altitude Sickness, Poisoning, Bites (Snake, animal bites), Stings, Lightening, Drowning. |
| Lesson 7: Childbirth. |
| Lesson 8: Evacuation Techniques |
| Practical Skill, Post-test, Result, and Certification, Training Evaluation, and Graduation Ceremony |
| Local resources used: RFR were taught how to use local resources, such as clothes, clean water, plastic bags, sticks, and tarpaulin. |
3.2.2. Selection Criteria of RFR
3.2.3. Data Capturing System
3.2.4. Service Delivery System
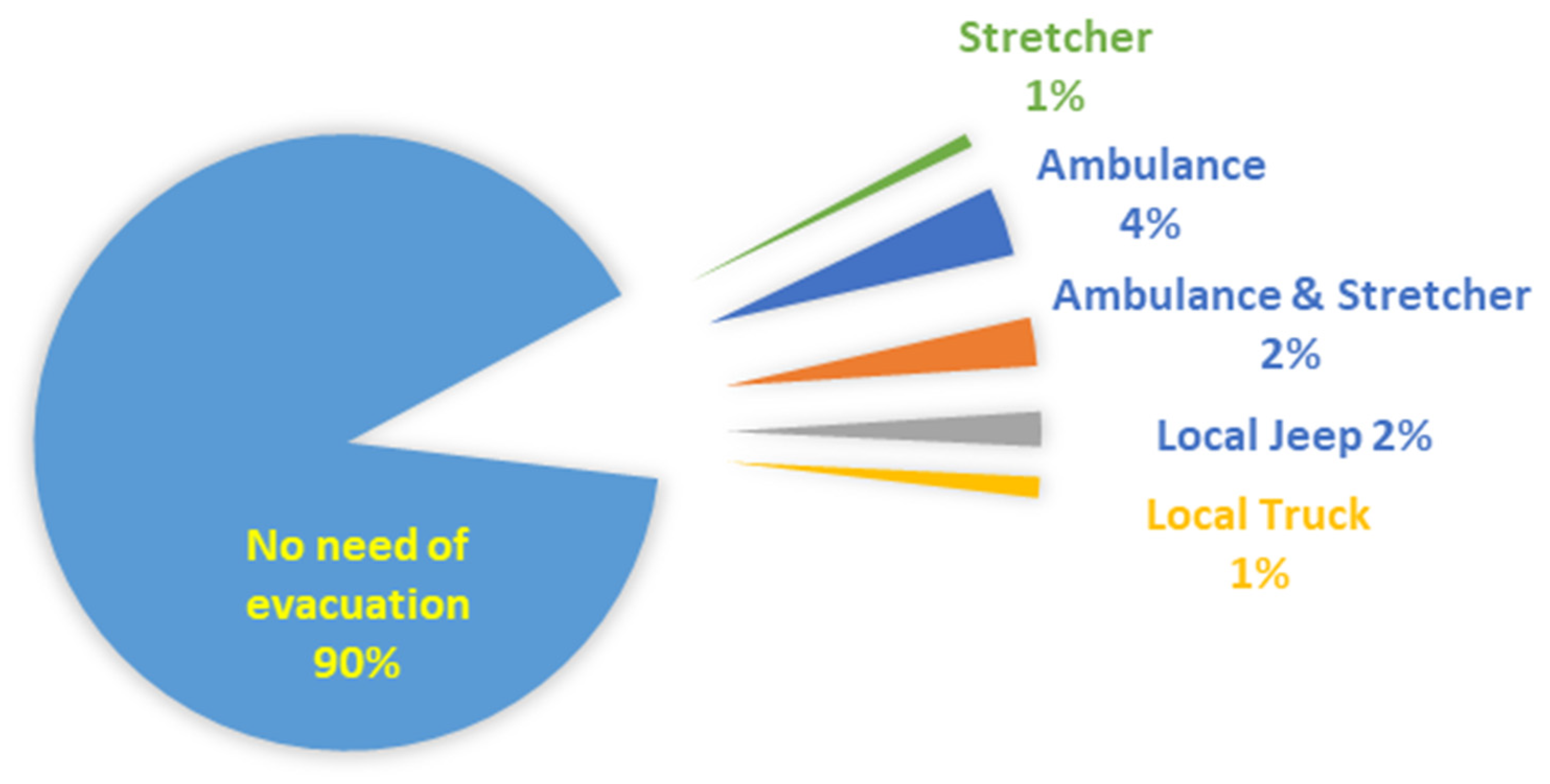
3.2.5. Rural First Responder Evacuation of Burn Victim
3.3. Rural First Responders Model Response for Burn Injuries
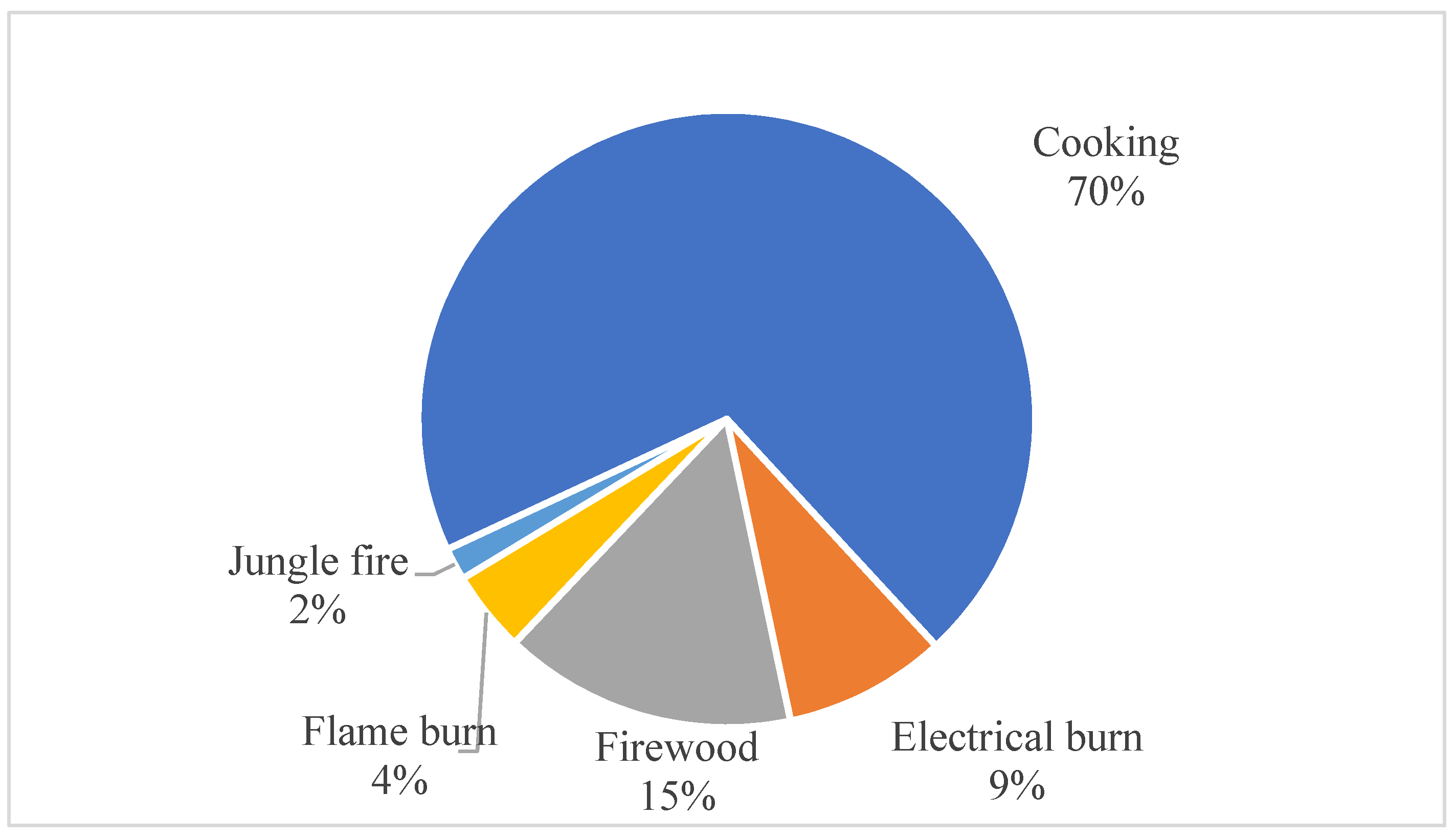
3.4. Burn Case Analysis for Project District Dhading
3.5. Case Studies
| On 8 April 2017, at around 9:00 a.m., a 70-year-old woman was cooking food for lunch. Suddenly, the utensils with which she was cooking the vegetable curry became imbalanced and hot curry spilled over her body. The burn was severe, and her family members first poured drinking water and applied fresh Aloe Vera gel in the wound. |
| While this incident occurred, a trained Rural First Responder, Maiya (name changed), was on her regular teaching job in a school. When she came to know about the incident from a villager, she immediately called to Emergency Communication Center in District Hospital, and RFR was suggested to evacuate her by ambulance; and, in two hours, she was transported to Teaching Hospital at Kathmandu (70 km far from the place incident) via ambulance, for which she was charged $60. |
| After being admitted for three months and spending around $1000 (direct costs including medicines, as reported by the patient’s family members), Malati was discharged from the hospital. |
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. A WHO Plan for Burn Prevention and Care; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- World Health Organization. Injuries and Violence: The Facts; World Health Organization: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/149798/9789241508018_eng.pdf (accessed on 5 April 2021).
- Vidal-Trecan, G.; Tcherny-Lessenot, S.; Grossin, C.; Devaux, S.; Pages, M.; Laguerre, J.; Wassermann, D. Differences between burns in rural and in urban areas: Implications for prevention. Burns 2000, 26, 351–358. [Google Scholar] [CrossRef]
- World Health Organization. Burns. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/burns (accessed on 2 April 2021).
- Central Bureau of Statistics. Annual Household Survey 2015/16; Central Bureau of Statistics: Kathmandu, Nepal; United Nations Development Programme: New York, NY, USA, 2016. Available online: https://neksap.org.np/allpublications/annual-household-survey-2015-16 (accessed on 27 March 2021).
- Pathak, R.S.; Lamichhane, K. Population size growth and distribution. In Population Monograph of Nepal; Central Bureau of Statistics: Kathmandu, Nepal, 2014; Volume I, pp. 15–37. Available online: https://nepal.unfpa.org/sites/default/files/pub-pdf/PopulationMonograph2014Volume1.pdf (accessed on 27 March 2021).
- Liu, E.H.; Khatri, B.; Shakya, Y.M.; Richard, B.M. A 3 year prospective audit of burns patients treated at the Western Regional Hospital of Nepal. Burns 1998, 24, 129–133. [Google Scholar] [CrossRef]
- Sakya, J.; Sah, S.K.; Bhandari, K.B.; Pathak, L.R.; Bhandari, S.B.; Ghimire, S.; Devkota, B.; Hussmann, J. Perception of Community and Hospital Personnel on Burn Treatment and Outcome in Nepal. J. Nepal Med. Assoc. 2018, 56, 924–930. [Google Scholar] [CrossRef] [Green Version]
- Tripathee, S.; Basnet, S.J. Epidemiology of burn injuries in Nepal: A systemic review. Burns Trauma 2017. [Google Scholar] [CrossRef] [Green Version]
- Pant, P.R.; Banstola, A.; Bhatta, S.; Mytton, J.A.; Acharya, D.; Bhattarai, S.; Bisignano, C.; Castle, C.D.; Prasad Dhungana, G.; Dingels, Z.V. Burden of injuries in Nepal, 1990–2017: Findings from the Global Burden of Disease Study 2017. Injury Prev. 2020, 26 (Suppl. S1), i57–i66. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Global Health Estimates Summary Tables 2019. The Global Health Observatory. 2020. Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death (accessed on 4 April 2021).
- Jha, A.K.; Dhakal, N.; Gyanwali, P.; Humagain, B.; Jha, N.; BC, R.K.; Sah, P.; Pradhan, A.; Dhimal, M. Quality of Essential Medicines in Public Health Care Facilities of Nepal 2019; Nepal Health Research Council: Kathmandu, Nepal, 2019.
- Sharma, N.P.; Duke, J.M.; Lama, B.; Thapa, B.; Dahal, P.; Bariya, N.D.; Marston, W.; Wallace, H.J. Descriptive epidemiology of unintentional burn injuries admitted to a tertiary-level government hospital in Nepal: Gender-specific patterns. Asia Pac. J. Public Health 2015, 27, 551–560. [Google Scholar] [CrossRef] [PubMed]
- Chalise, P.R.; Shrestha, S.; Sherpa, K.; Nepal, U.; Bhattachan, C.L.; Bhattacharya, S.K. Epidemiological and bacteriological profile of burn patients at Nepal Medical College Teaching Hospital. Nepal Med. Coll. J. 2008, 10, 233–237. [Google Scholar] [PubMed]
- Gurung, G.; Derrett, S.; Hill, P.C.; Gauld, R. Governance challenges in the Nepalese primary health care system: Time to focus on greater community engagement? Int. J. Health Plan. Manag. 2016, 31, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Response and Beyond: The Road to Resilience, Health Sector Interventions Following the Nepal Earthquake 2015 and Lessons Learned; Nepal Health Research Council: Kathmandu, Nepal, 2017.
- Sedain, B. Unnatural Causes of Deaths in Nepal; University Grants Commission: Bhaktapur, Nepal, 2021. [Google Scholar]
- Sinha, R. Project Evaluation Report of Emergency Medical Services Project Implemented by District Health Office of Dhading; Social Welfare Council: Lalitpur, Nepal, 2019. [Google Scholar]
- Reydon, B. Social Embeddedness. Institutions for Rural Land Management and Land Grabbing: The Cases of Afghanistan and Brazil 2016. Paper Presented at the Colloque International “Les Frontières de la Question Foncière. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.491.582&rep=rep1&type=pdf (accessed on 6 April 2021).
- Medical Teams International. Rural First Responder: Handbook; District Health Office Dhading and Medical Teams International: Alexandria, VA, USA, 2016. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bist, B.S.; Sedain, B.; Shrestha, M.; Tripathi, P. Community Response to Burn Injuries: Examples from Dhading District of Nepal. Eur. Burn J. 2021, 2, 55-62. https://doi.org/10.3390/ebj2030005
Bist BS, Sedain B, Shrestha M, Tripathi P. Community Response to Burn Injuries: Examples from Dhading District of Nepal. European Burn Journal. 2021; 2(3):55-62. https://doi.org/10.3390/ebj2030005
Chicago/Turabian StyleBist, Bimal Singh, Bhagabati Sedain, Maheshwar Shrestha, and Prativa Tripathi. 2021. "Community Response to Burn Injuries: Examples from Dhading District of Nepal" European Burn Journal 2, no. 3: 55-62. https://doi.org/10.3390/ebj2030005
APA StyleBist, B. S., Sedain, B., Shrestha, M., & Tripathi, P. (2021). Community Response to Burn Injuries: Examples from Dhading District of Nepal. European Burn Journal, 2(3), 55-62. https://doi.org/10.3390/ebj2030005





