Clinical Outcomes in Burns Patients with Early Venous Thromboembolism Prophylaxis Compared with Late-Anticoagulated Patients: A Retrospective Study
Abstract
1. Introduction
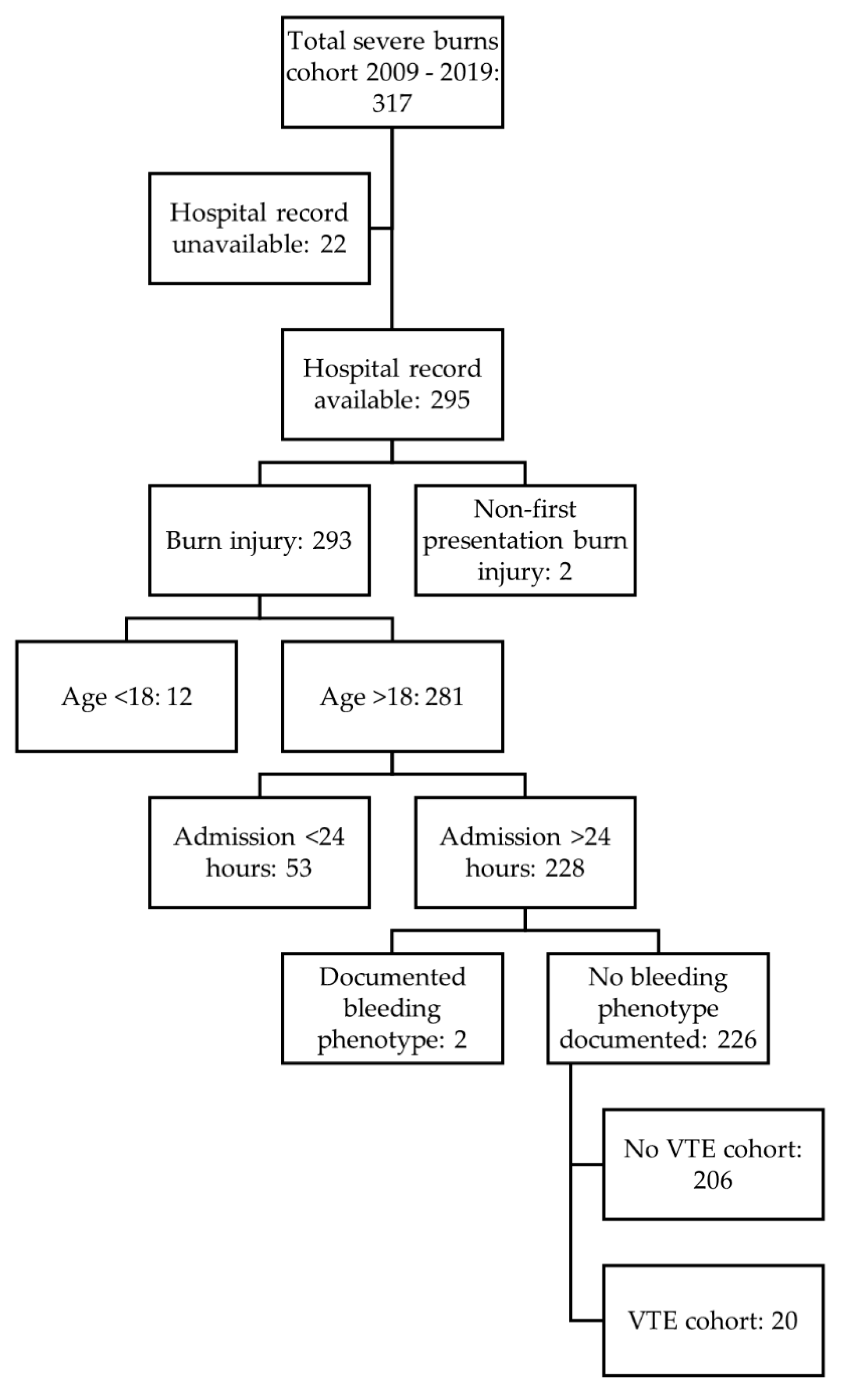
2. Materials and Methods
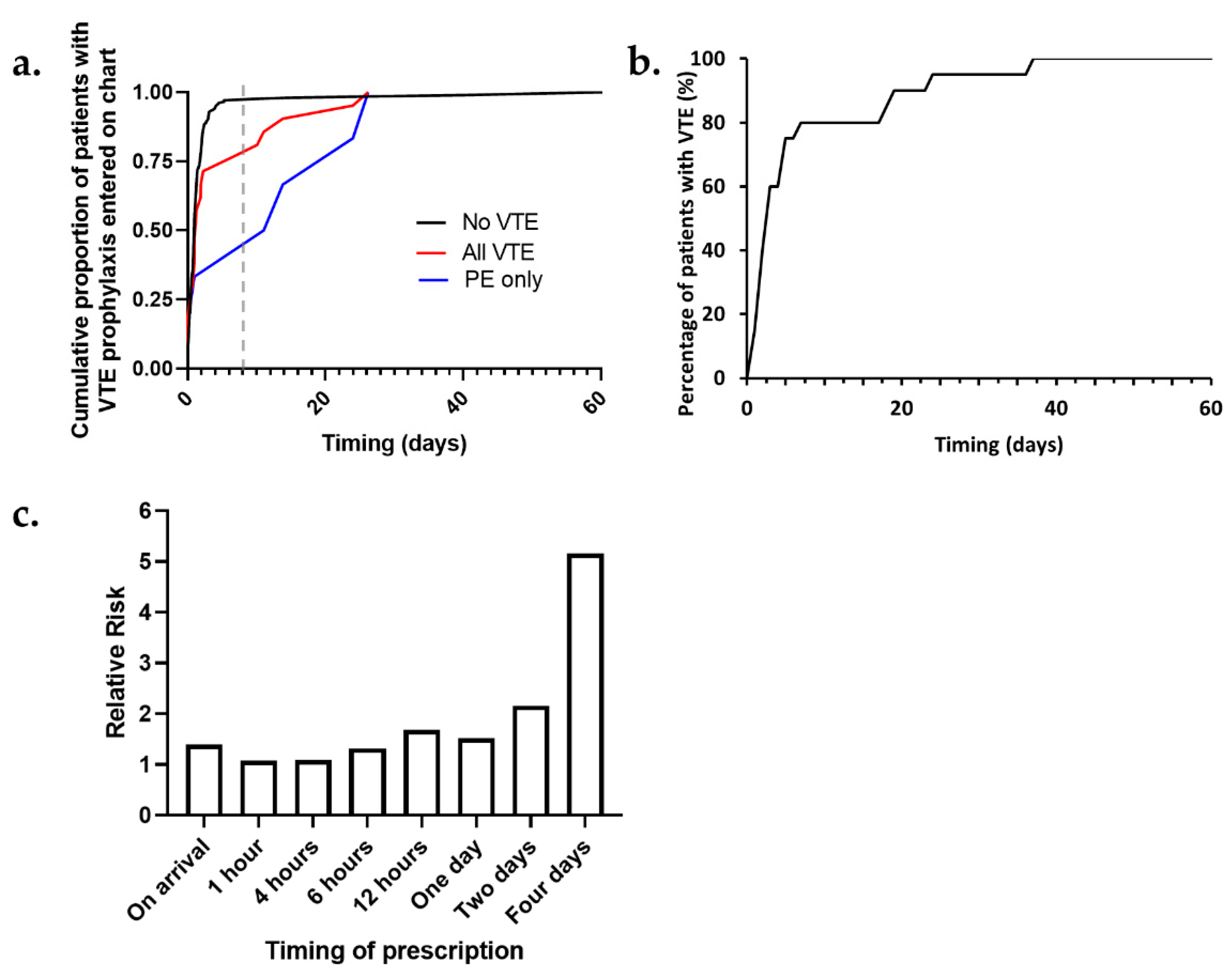
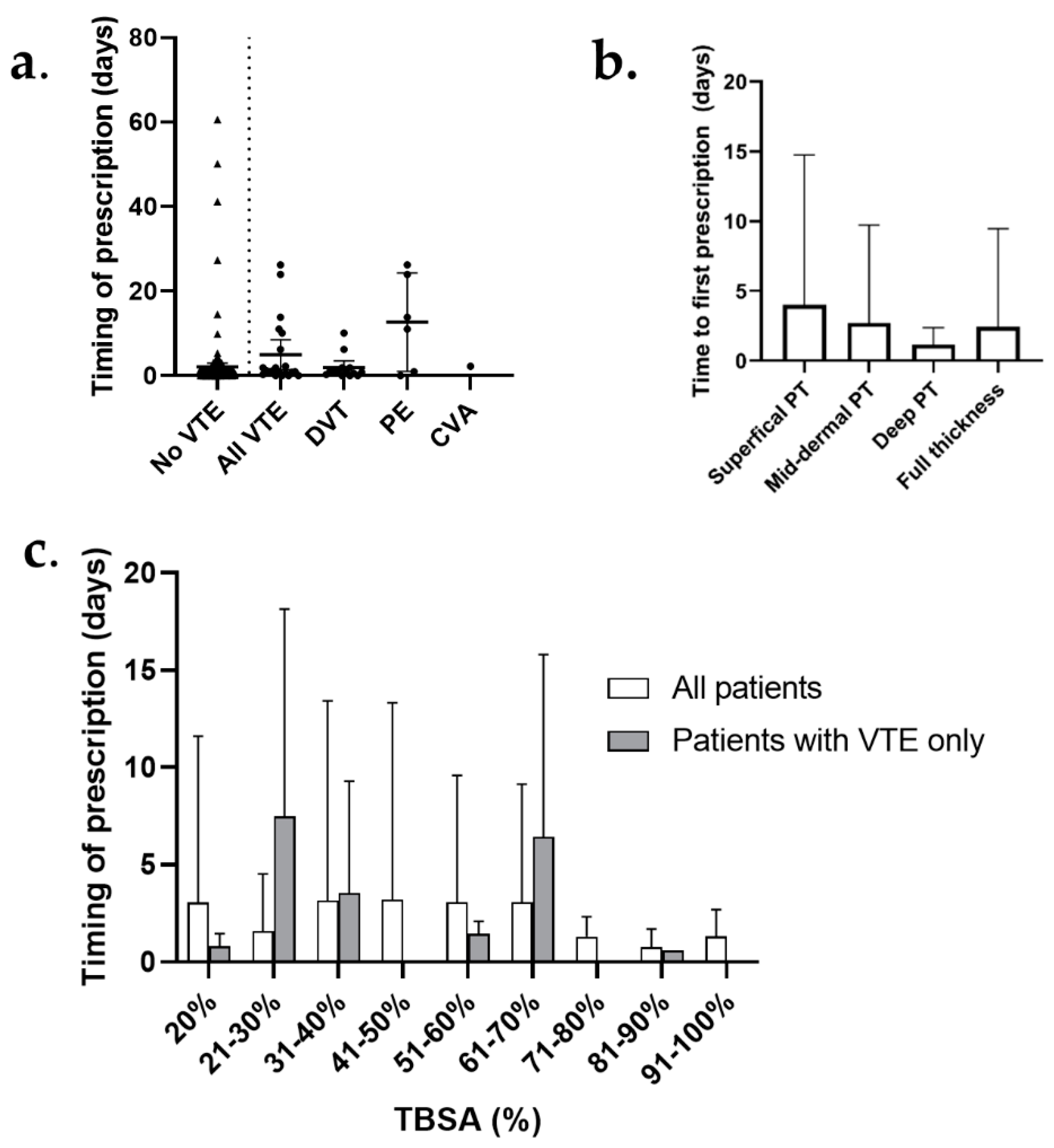
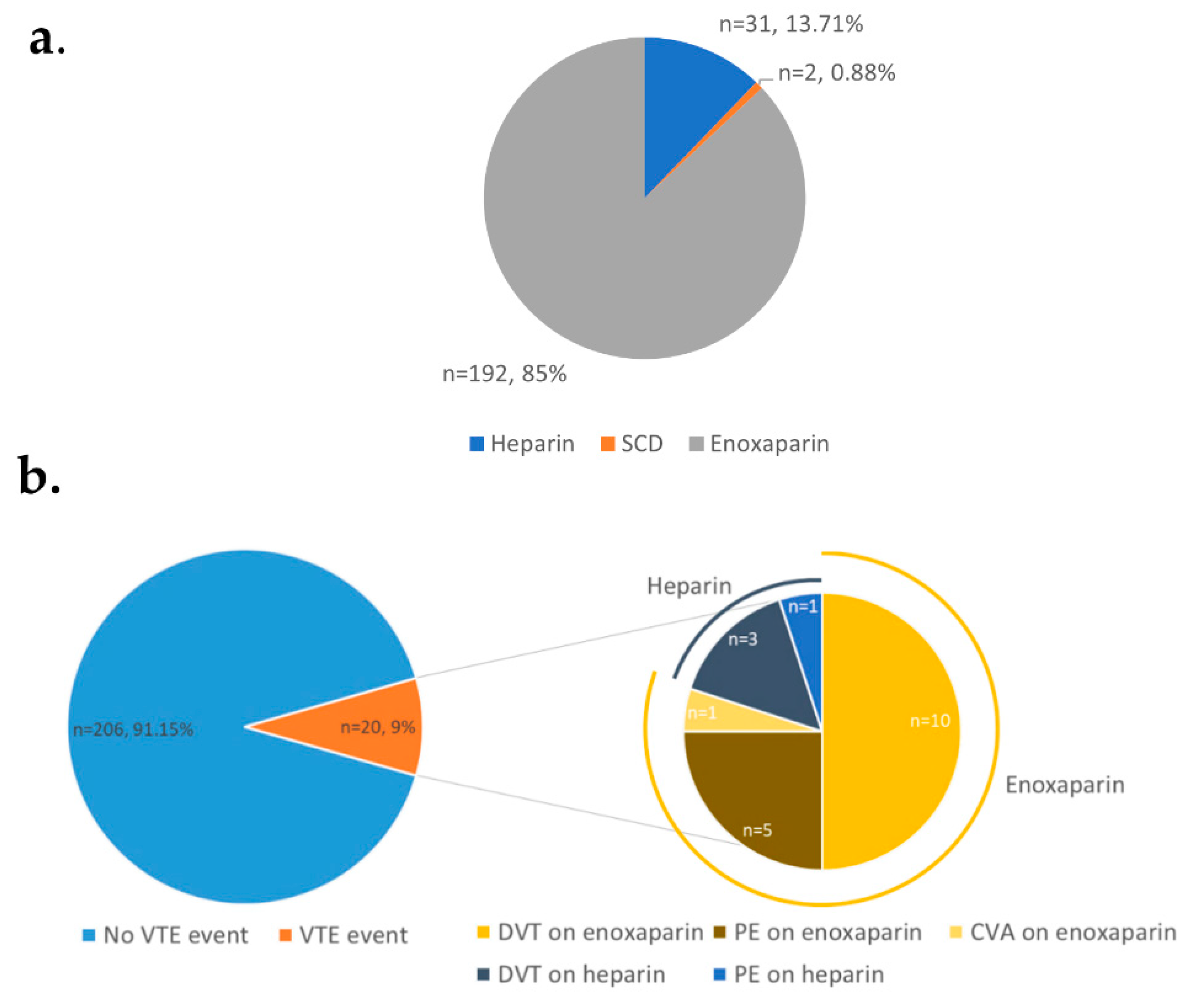
3. Results
4. Discussion
4.1. Institutional Protocol for VTE Prophylaxis
4.2. Timing of VTE Prophylaxis Initiation
4.3. Examination of Patient Subset Who Developed a Pulmonary Embolus
4.3.1. Risk Factor Analysis—Total Body Surface Area Affected by Burn
4.3.2. Risk Factor Analysis—Smoking
4.3.3. Risk Factor Analysis—Anatomical Burn Location
4.4. Mode of Thromboprophylaxis
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Sikora, S.; Papp, A. Venous thromboembolism in burn patients is not prevented by chemoprophylaxis. Burns 2017, 43, 1330–1334. [Google Scholar] [CrossRef]
- Pannucci, C.; Osborne, N.; Wahl, W. Venous Thromboembolism in Thermally Injured Patients: Analysis of the National Burn Repository. J. Burn Care Res. 2011, 32, 6–12. [Google Scholar] [CrossRef]
- Moheimani, F.; Jackson, D.E. Venous thromboembolism: Classification, risk factors, diagnosis, and management. ISRN Hematol. 2011, 2011, 124610. [Google Scholar] [PubMed]
- Ensor, J.; Riley, R.D.; Moore, D.; Snell, K.I.; Bayliss, S.; Fitzmaurice, D. Systematic review of prognostic models for recurrent venous thromboembolism (VTE) post-treatment of first unprovoked VTE. BMJ Open 2016, 6, e011190. [Google Scholar] [CrossRef] [PubMed]
- Kourelis, T.V.; Wysokinska, E.M.; Wang, Y.; Yang, P.; Mansfield, A.S.; Tafur, A.J. Early venous thromboembolic events are associated with worse prognosis in patients with lung cancer. Lung Cancer 2014, 86, 358–362. [Google Scholar] [CrossRef]
- Tagalakis, V.; Patenaude, V.; Kahn, S.R.; Suissa, S. Incidence of and mortality from venous thromboembolism in a real-world population: The Q-VTE Study Cohort. Am. J. Med. 2013, 126, 832-e13. [Google Scholar] [CrossRef] [PubMed]
- Kesieme, E.; Kesieme, C.; Jebbin, N.; Irekpita, E.; Dongo, A. Deep vein thrombosis: A clinical review. J. Blood Med. 2011, 2, 59. [Google Scholar] [CrossRef] [PubMed]
- Horner, K.; Isitt, C.; Shida, A. The Critically Ill Burn Patient: How Do We Get It Right? In Key Topics in Management of the Critically Ill; Springer: Cham, Switzerland, 2016; pp. 155–166. [Google Scholar]
- Pannucci, C.J.; Osborne, N.H.; Park, H.S.; Wahl, W.L. Acquired inpatient risk factors for venous thromboembolism after thermal injury. J. Burn Care Res. 2012, 33, 84–88. [Google Scholar] [CrossRef]
- Stashenko, G.; Lopes, R.D.; Garcia, D.; Alexander, J.H.; Tapson, V.F. Prophylaxis for venous thromboembolism: Guidelines translated for the clinician. J. Thromb. Thrombolysis 2011, 31, 122–132. [Google Scholar] [CrossRef]
- Gould, M.K.; Garcia, D.A.; Wren, S.M.; Karanicolas, P.J.; Arcelus, J.I.; Heit, J.A.; Samama, C.M. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012, 141, e227S–e277S. [Google Scholar] [CrossRef]
- Johnson, R.M.; Richard, R. Partial-thickness burns: Identification and management. Adv. Ski. Wound Care. 2003, 16, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Lu, P.; Harms, K.A.; Paul, E.; Bortz, H.; Lo, C.; Cleland, H. Venous thromboembolism in burns patients: Are we underestimating the risk and underdosing our prophylaxis? J. Plast. Reconstr. Aesthetic Surg. 2020. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Janus, E.; Bassi, A.; Jackson, D.; Nandurkar, H.; Yates, M. Thromboprophylaxis use in medical and surgical inpatients and the impact of an electronic risk assessment tool as part of a multi-factorial intervention. A report on behalf of the elVis study investigators. J. Thromb. Thrombolysis 2011, 32, 279–287. [Google Scholar] [CrossRef][Green Version]
- Kelly, J.; Rudd, A.; Lewis, R.R.; Hunt, B.J. Screening for subclinical deep-vein thrombosis. QJM An. Int. J. Med. 2001, 94, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; de Staercke, C.; Hooper, W.C. The effects of obesity on venous thromboembolism: A review. Open J. Prev. Med. 2012, 2, 499. [Google Scholar] [CrossRef] [PubMed]
- Allman-Farinelli, M.A. Obesity and venous thrombosis: A review. Semin. Thromb. Hemost. 2011, 37, 903–907. [Google Scholar] [CrossRef] [PubMed]
- Lindström, S.; Germain, M.; Crous-Bou, M.; Smith, E.N.; Morange, P.E.; van Hylckama Vlieg, A.; de Haan, H.G.; Chasman, D.; Ridker, P.; Brody, J.; et al. Assessing the causal relationship between obesity and venous thromboembolism through a Mendelian Randomization study. Hum. Genet. 2017, 136, 897–902. [Google Scholar] [CrossRef]
- Cheng, Y.J.; Liu, Z.H.; Yao, F.J.; Zeng, W.T.; Zheng, D.D.; Dong, Y.G.; Wu, S.H. Current and former smoking and risk for venous thromboembolism: A systematic review and meta-analysis. PLoS Med. 2013, 10, e1001515. [Google Scholar] [CrossRef]
- Enga, K.F.; Braekkan, S.K.; Hansen-Krone, I.J.; Le Cessie, S.; Rosendaal, F.R.; Hansen, J.B. Cigarette smoking and the risk of venous thromboembolism: The Tromsø Study. J. Thromb. Haemost. 2012, 10, 2068–2074. [Google Scholar] [CrossRef]
- Barker, R.C.; Marval, P. Venous thromboembolism: Risks and prevention. Contin. Educ. Anaesth. Crit. Care Pain 2011, 11, 18–23. [Google Scholar] [CrossRef]
- Lin, H.; Faraklas, I.; Cochran, A.; Saffle, J. Enoxaparin and antifactor Xa levels in acute burn patients. J. Burn. Care Res. 2011, 32, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Bittner, E.A.; Shank, E.; Woodson, L.; Martyn, J.J. Acute and perioperative care of the burn-injured patient. Anesthesiology 2015, 122, 448–464. [Google Scholar] [CrossRef] [PubMed]
- Barrett, Y.C.; Wang, J.; Song, Y.; Pursley, J.; Wastall, P.; Wright, R.; LaCreta, F.; Frost, C. A randomised assessment of the pharmacokinetic, pharmacodynamic and safety interaction between apixaban and enoxaparin in healthy subjects. Thromb. Haemost. 2012, 107, 916–924. [Google Scholar] [PubMed]
| Characteristic | Percentage (Patient Number) 1 |
|---|---|
| Age (mean ± 95% CI) | 41 ± 17 |
| Gender (Male) | 72.12% (163 patients) |
| BMI (kg/m2) (mean ± 95% CI) | 25.9 ± 5.5 |
| Obese patients | 13.27% (30 patients) |
| Average length of stay (days) (mean ± 95% CI) 2 | 33.35 ± 30.5 |
| Burn depth | |
| Superficial Partial Thickness (PT) burn | 11.50% (26 patients) |
| Mid-dermal PT burn | 15.93% (36 patients) |
| Deep PT burn | 3.54% (8 patients) |
| Full thickness burn | 42.92% (97 patients) |
| Not documented | 26.10% (59 patients) |
| Burn size (mean ± 95% CI) | 38.35% ± 20.30 |
| 20% TBSA | 15.50% (35 patients) |
| 21–30% TBSA | 37.61% (85 patients) |
| 31–40% TBSA | 15.50% (35 patients) |
| 41–50% TBSA | 7.08% (16 patients) |
| 51–60% TBSA | 8.85% (20 patients) |
| 61–70% TBSA | 7.07% (16 patients) |
| 71–80% TBSA | 2.65% (6 patients) |
| 81–90% TBSA | 3.09% (7 patients) |
| 91–100% TBSA | 2.65% (6 patients) |
| VTE | 20 (8.85%) |
| DVT | 13 (5.75%) |
| PE | 6 (2.65%) |
| CVA | 1 (0.44%) |
| Relative Risk | 95% CI | p Value | |
|---|---|---|---|
| Obesity (BMI ≥ 30 kg/m2) | 2.80 | 1.17 to 6.72 | 0.0212 (*) |
| Heart failure | 4.48 | 0.20 to 106.95 | NS |
| Hepatic failure | 2.01 | 0.25 to 15.56 | NS |
| Renal failure | 1.92 | 0.62 to 5.88 | NS |
| Smoking history | 2.19 | 1.38 to 3.50 | 0.0007 (***) |
| Superficial PT burn | 0.40 | 0.02 to 6.54 | NS |
| Mid-dermal PT burn | 0.90 | 0.30 to 2.74 | NS |
| Deep-dermal PT burn | 0.79 | 0.31 to 2.03 | NS |
| Full thickness burn | 1.20 | 0.80 to 1.78 | NS |
| Mean difference | |||
| Age | 2.50 | −5.64 to 10.67 | NS |
| BMI | 0.14 | −2.41 to 2.693 | NS |
| Total Body Surface Area Burn (TBSA, %) | 8.57 | −0.94 to 18.08 | NS |
| Relative Risk | 95% CI | p Value | |
|---|---|---|---|
| Inhalation injury | 1.32 | 0.79 to 2.22 | NS |
| Scalp burns | 2.22 | 1.06 to 4.64 | 0.035 (*) |
| Facial burns | 1.20 | 0.87 to 1.65 | NS |
| Eye burns | 3.24 | 1.83 to 5.75 | 0.0001 (****) |
| Neck burns | 1.17 | 0.70 to 1.96 | NS |
| Breast burns | 1.37 | 0.92 to 2.03 | NS |
| Trunk burns | 1.43 | 1.17 to 1.74 | 0.0004 (***) |
| Buttock burns | 1.58 | 0.88 to 2.83 | NS |
| Perineum burns | 0.95 | 0.32 to 2.82 | NS |
| Dorsal hand burns | 1.79 | 0.86 to 3.70 | NS |
| Palmar hand burns | 1.71 | 0.76 to 3.87 | NS |
| Upper limb burns | 1.27 | 1.09 to 1.49 | 0.0027 (**) |
| Foot burns | 0.51 | 0.13 to 1.95 | NS |
| Dorsal foot burns | 2.16 | 0.52 to 8.95 | NS |
| Sole foot burns | 1.04 | 0.06 to 17.78 | NS |
| Lower limb burns | 1.44 | 1.27 to 1.64 | <0.0001 (****) |
| Relative Risk | 95% CI | p Value | |
|---|---|---|---|
| Sepsis | 1.28 | 0.51 to 3.21 | NS |
| Requiring Intensive Care Unit (ICU) admission | 1.29 | 1.06 to 1.56 | 0.0096 (**) |
| Operative burns management | 0.95 | 0.766 to 1.17 | NS |
| Required debridement | 0.62 | 0.09 to 4.27 | NS |
| Temporary skin substitute | 1.38 | 1.11 to 1.69 | 0.0026 (*) |
| Skin graft | 0.59 | 0.42 to 0.84 | 0.0034 (*) |
| Parenteral nutrition | 0.98 | 0.44 to 2.15 | NS |
| Death during admission | 0.52 | 0.14 to 1.99 | NS |
| Mean difference | |||
| Time to first dose (Minutes) | 2470 | −2155 to 7094 | NS |
| Total ICU minutes | −379 | −11,739 to 10,980 | NS |
| Length of hospital stay (days) | 9.81 | −3.24 to 22.9 | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brazilek, R.; Cleland, H.J. Clinical Outcomes in Burns Patients with Early Venous Thromboembolism Prophylaxis Compared with Late-Anticoagulated Patients: A Retrospective Study. Eur. Burn J. 2021, 2, 63-74. https://doi.org/10.3390/ebj2030006
Brazilek R, Cleland HJ. Clinical Outcomes in Burns Patients with Early Venous Thromboembolism Prophylaxis Compared with Late-Anticoagulated Patients: A Retrospective Study. European Burn Journal. 2021; 2(3):63-74. https://doi.org/10.3390/ebj2030006
Chicago/Turabian StyleBrazilek, Rose, and Heather J. Cleland. 2021. "Clinical Outcomes in Burns Patients with Early Venous Thromboembolism Prophylaxis Compared with Late-Anticoagulated Patients: A Retrospective Study" European Burn Journal 2, no. 3: 63-74. https://doi.org/10.3390/ebj2030006
APA StyleBrazilek, R., & Cleland, H. J. (2021). Clinical Outcomes in Burns Patients with Early Venous Thromboembolism Prophylaxis Compared with Late-Anticoagulated Patients: A Retrospective Study. European Burn Journal, 2(3), 63-74. https://doi.org/10.3390/ebj2030006







