Abstract
Background/Objectives: Maxillary defects, whether congenital or acquired, can compromise chewing, speech, and aesthetics. This systematic review aimed to evaluate the application and characteristics of definitive palatal obturators in the rehabilitation of such defects, analyzing techniques of fabrication, materials, outcomes of the fabrication, and limitations reported in the literature. Methods: The review was conducted in accordance with PRISMA 2020 guidelines and was registered in PROSPERO (ID: 1011648). A comprehensive search was performed in PubMed, Scopus, Lilacs, and Google Scholar for studies published from 1 January 2014 to 1 January 2025. Inclusion criteria comprised adult patients treated with definitive palatal obturators and with reported follow-up. Exclusion criteria included studies on children, animals, or lacking patient data. Two reviewers independently screened studies and assessed eligibility. Bias was evaluated qualitatively across five domains. No meta-analysis was conducted; data were synthesized descriptively using charts and tables. The study was funded by the Italian Ministry of Health—Current Research IRCCS. Results: A total of 59 studies involving 83 patients (46 males, 37 females; mean age 54.6 ± 13.8 years) were included. Mucormycosis and squamous cell carcinoma were the primary causes of defects. Conventional impressions using alginate and silicone were most common, while digital techniques were reported in only 6.6% of cases. All definitive obturators were fabricated using acrylic resin, with some featuring hollow bulbs, velopharyngeal extensions, or magnetic retention. Multiple sources of bias were observed. Conclusions: Definitive palatal obturators provide effective functional and aesthetic rehabilitation for maxillary defects. However, evidence is limited by methodological weaknesses, lack of standardization, and underutilization of digital technologies. Future studies should focus on improving reporting quality, adopting innovative fabrication protocols, and generating higher-level clinical evidence to support best practices.
1. Introduction
The maxilla plays a crucial role in chewing, swallowing, and phonation, as it is involved in supporting the dentition, stabilizing the tongue, and ensuring the proper alignment of oro-facial structures [1]. When defects occur in the maxilla, these functions can be severely impaired, leading to difficulties in chewing and swallowing food, alterations in the phonation process with a possible onset of dysarthria or hypernasality, and negative effects on facial aesthetics and symmetry. Such functional impairments can significantly impact the patient’s quality of life, reducing their ability to eat properly and communicate effectively [2,3,4,5].
Maxillary defects can be classified into two main categories: congenital and acquired. Congenital defects, such as cleft lip and palate, are abnormalities present from birth, resulting from an alteration in the embryonic development of facial structures. These defects cause an interruption in the fusion of the nasal and palatal processes. Acquired defects, instead, occur after birth and may result from the following:
- Surgical resections performed to treat benign or malignant neoplasms, such as epithelial or salivary gland tumors involving the maxilla;
- Infectious diseases such as osteomyelitis or bone osteonecrosis caused by factors like radiation;
- Chronic inflammatory conditions, such as cocaine-induced midline destructive lesions (CIMDL) or granulomatosis with polyangiitis, leading to structural and functional alterations of the maxilla;
- Trauma [6,7,8].
One of the main causes of acquired maxillary defects is maxillectomy, a surgical procedure necessary for treating certain head and neck tumors. According to Global Cancer Statistics 2020, oral cancer ranks 15th worldwide in terms of mortality, with 188,438 deaths per year, and 16th in incidence, with 389,846 cases per year [9]. It is more frequently distributed in Melanesia, Central and South Asia, Eastern Europe, Australia/New Zealand, and Western Europe for both sexes [10]. In Italy, approximately 13,000 new cases of these diseases are diagnosed each year. According to the 2021 report by the Italian Association of Medical Oncology, head and neck tumors account for about 3% of all malignant neoplasms in the country [11]. Of these, 90% are oral squamous cell carcinomas, which affect the hard and soft palate in less than 13% of cases. Additionally, salivary gland neoplasms, which make up about 3% of head and neck tumors, can involve the palate if they develop in the minor salivary glands [6,11]. The incidence of these diseases is 18 cases per 100,000 inhabitants, a figure that reflects the European Union average. Incidence is three times higher in Northern Italy and tends to increase with age, regardless of anatomical location, except for nasopharyngeal tumors. The presence of oral comorbidities, such as precancerous lesions or other chronic inflammatory conditions, can further increase the risk of developing malignant tumors in this area, worsening the epidemiological outlook. Understanding these epidemiological data is crucial for planning prevention and early diagnosis strategies: periodic check-ups with the dentist are important, along with professional oral hygiene sessions [12].
In fact, oral squamous cell carcinoma, in particular, has a prognosis that can significantly improve if detected at an early stage [11].
Partial or total maxillectomy often results in oro-nasal, oro-sinus, or oro-naso-sinus communications, leading to clinical complications such as nasal regurgitation of food and significant difficulties in chewing and phonation. These functional and anatomical alterations have a considerable impact on the patient’s quality of life, making targeted rehabilitation essential, whether surgical or prosthetic, to restore the structures compromised by ablative surgery [13].
Although surgical intervention is a viable option for reconstructing resected tissues, this approach is not always feasible.
Another key factor in the development of acquired maxillary defects is cocaine-induced midline destructive lesions (CIMDL). Over the past three years, global cocaine use has remained relatively stable, with estimates suggesting an annual number of users ranging between 14 and 21 million, according to the United Nations Office on Drugs and Crime. Cocaine consumption is particularly high in certain regions of the world, such as North America (approximately 5 million users), South America (4.5 million), Africa (2.8 million), and Western and Central Europe (4 million). These figures indicate a geographical distribution of cocaine use that continues to show significant prevalence in specific areas despite maintaining a stable trend on a global scale. The 2023 European Drug Report reveals that approximately 2.3 million young adults aged 15 to 34 (equivalent to 2.3% of this age group) used cocaine in the past year. Additionally, it is estimated that around 17 million adults between the ages of 15 and 64 have used cocaine at least once in their lifetime. In some European countries, such as Spain and the United Kingdom, the prevalence rates of cocaine use among young adults (15–34 years old) are comparable to or even higher than those recorded in the United States, highlighting a worrying spread of this substance among younger generations in Europe [7,14]. The most commonly used route of cocaine administration is intranasal inhalation, also known as “snorting”. This method of consumption is associated with a range of local adverse effects, particularly in the nasal tract. Habitual nasal insufflation of cocaine can cause significant damage to the nasal mucosa, which, if use becomes chronic and compulsive, leads to the progressive deterioration of nasal structures. Specifically, damage to the mucosa and perichondrium can result in ischemic necrosis of the nasal septal cartilage, ultimately causing septal perforation. In some cases, cocaine-induced lesions can lead to extensive destruction of the osteocartilaginous structures of the nose, paranasal sinuses, and palate, mimicking other pathological conditions such as neoplasms, infections, or immunological disorders. A significant clinical challenge is distinguishing between CIMDL and granulomatosis with polyangiitis, an autoimmune disease that affects blood vessels and can cause similar nasal damage. Currently, no specific diagnostic test can definitively attribute a destructive lesion of the nasal or palatal mucosa to cocaine use. Furthermore, individuals who abuse cocaine often downplay or deny their addiction, further complicating both diagnosis and treatment. CIMDL can be managed with palatal obturators or, in selected cases, through surgical intervention. However, it is important to emphasize that surgical approaches have an unfavorable prognosis if cocaine use continues, as the substance-induced tissue damage and necrosis can impair healing and compromise long-term surgical success. Therefore, the management of these lesions requires an integrated approach that includes cessation of cocaine use along with appropriate medical and prosthetic treatment [7,15].
Maxillary defects can be treated either through surgical intervention or with the use of a palatal obturator [16]. A palatal obturator is a therapeutic prosthesis designed to close an opening or defect in the oral tissues, typically positioned at the level of the hard palate, alveolar structures, or surrounding soft tissues [17]. Its primary function is to restore the anatomical separation between the nasal and oral cavities, provide adequate mandibular support, and help stabilize occlusion [18]. In many cases, a palatal obturator is the most common and preferred therapeutic option over surgical reconstruction due to various clinical and functional reasons:
- Easy visualization of the defect site, allowing for early detection of recurrences;
- Reduced hospitalization time and costs;
- The possibility of avoiding a second surgical procedure;
- Immediate morphological and functional restoration of the oral cavity [19].
Reconstructive surgery, on the other hand, often carries a high risk of complications, such as flap necrosis and tumor recurrence, particularly in patients who have undergone radiotherapy and chemotherapy [20]. Maxillary defects can be classified using different classification systems reported in the literature. These classifications are not only useful for descriptive purposes but also provide guidance to the surgeon in the reconstruction and rehabilitation phase [21]. Among these classifications, Armany’s Classification for Maxillectomy Defects is an excellent classification and guides prosthodontists in obturator design, even if it is deficient in description of surgical defect [22].
The fabrication of obturator prostheses for maxillary defects can be a significant challenge, especially when using conventional prosthetic methods. These traditional approaches often present difficulties that require advanced technical skills and extensive experience to be effectively managed. Some of the main obstacles include the risk of aspiration during impression-taking, difficulties arising from poor tissue quality due to resections or bone demineralization, and complications in obtaining an impression due to limited mouth opening—commonly seen in patients with surgical scars or those who have undergone radiotherapy. These challenges demand meticulous planning and expertise in handling conventional tools, such as managing impression materials and manually fabricating prostheses. However, with advancements in digital technology and the introduction of computer-aided design (CAD) and computer-aided manufacturing (CAM) techniques, the fabrication of palatal obturators has seen significant improvements. Digital techniques allow for greater precision in the design and production of prostheses, significantly reducing the margin of error compared to traditional methods. Data acquisition through digital scanning enables the creation of highly detailed three-dimensional models of the oral cavity, resulting in more accurately fitted obturators that better adapt to the patient’s anatomical and functional variations [23].
There are three types of palatal obturators that are used in three sequential phases following maxillectomy to ensure optimal recovery of the patient’s oral functions and aesthetics. In the first phase, a surgical obturator is used, which is fabricated before the surgery and placed in the mouth for 7–10 days after the surgical procedure. After its removal, a temporary obturator is constructed, ensuring aesthetic functionality during the 3–4 month healing period. Finally, a definitive obturator prosthesis is created post healing [24].
The aim of this literature review is to explore the therapeutic and prosthetic rehabilitation approach for patients with maxillary defects, focusing on the use of a definitive palatal obturator and analyzing the materials and techniques used in prosthesis fabrication.
2. Materials and Methods
2.1. Protocol Development and Eligibility Criteria
This review was performed according to the Preferred Re-porting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (see Supplementary Materials), and the study protocol has been registered in PROSPERO (ID:1011648).
2.2. Search Strategy
For this study, a computerized search was conducted using the databases of Google Scholar, PubMed (MEDLINE), Lilacs, and Scopus. The research was performed using advanced search options provided by the databases, selecting literature publications available from 1 January 2014 to 1 January 2025, with the use of specific keywords. Finally, the publications were manually reviewed, and articles meeting the exclusion criteria were discarded (Figure 1).
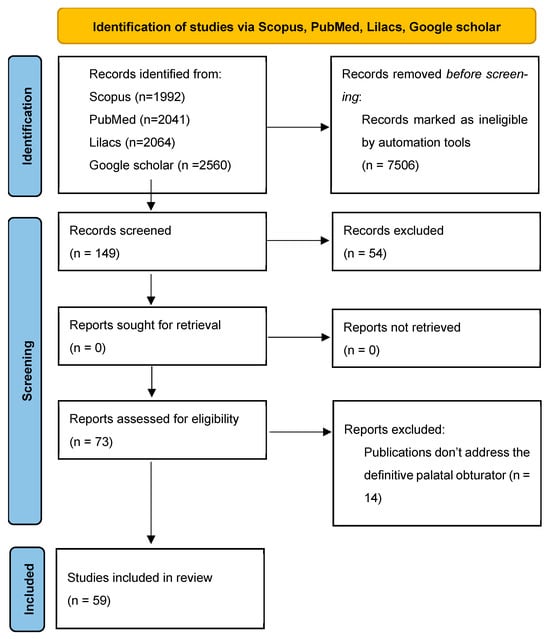
Figure 1.
PRISMA flow diagram.
2.3. Selection Criteria
Inclusion Criteria:
- Time period: last 10 years;
- Main keywords: palatal obturator, years old, follow-up, NOT child;
- Type of prosthesis: definitive obturator prosthesis.
Exclusion Criteria:
- Animal studies;
- Studies lacking information on subjects, such as age and sex;
- Subjects not undergoing periodic follow-ups;
- Subjects under 18 years of age;
- Subjects whose pathology was not specified.
2.4. Search Terms
The main keywords of the selection criteria were organized into a MeSH (Medical Object Headings) applied in the computer databases.
In the Scopus search, the final MeSH was (Palatal obturator) AND (Years old) AND (Follow-up).
In the PubMed search, the final MeSH was (Palatal obturator) AND (Year old) AND (Follow-up) NOT (Child).
In the Lilac search, the final MeSH was (Palatal obturator) AND (Year old) AND (Follow-up) AND NOT (Child).
In the Google Scholar search, the final MeSH was (Palatal obturator) AND (Year old) AND (Follow up) NOT (Child) AND [(Impression) OR (cast) OR (fabrication)].
2.5. Screening and Selection Process
In the Scopus search, there were 105 publications containing the keyword “palatal obturator” in the title and/or abstract. Of these, 67 met the time criterion. By adding the keywords “years old” (to identify publications that specify the age of subjects), “follow-up” (to include studies with follow-up data), and “not child” (to exclude studies involving minors), four publications were found. Among these, one was excluded due to unavailability and one for being unrelated to the topic.
In the PubMed search, 2041 publications contained the keyword “palatal obturator” in the title and/or abstract. Of these, 297 met the time criterion. After applying the keywords “years old”, “follow-up”, and “not child”, 11 publications were identified. Among these, one was excluded for being unrelated to the topic, and wo were excluded since they did not involve definitive palatal obturators.
In the Lilacs search, 2064 publications contained the keyword “palatal obturator” in the title and/or abstract. Of these, 310 met the time criterion. After applying the keywords “years old”, “follow-up”, and “not child”, 11 publications were found. However, nine were excluded: one for being unrelated to the topic and eight for being duplicates already found in PubMed.
In the Google Scholar search, 304 publications were found containing the keywords “palatal obturator”, “years old”, “follow-up”, and “not child”, meeting the time criterion. By adding the keywords “impression OR cast OR fabrication” to identify publications describing the fabrication phases of the palatal obturator, 123 publications were retrieved. Among these, 3 were excluded due to unavailability, 31 for being unrelated to the topic, 1 for overly generic statistical data, 5 for lack of subjects, 5 for missing subject information, 8 for unspecified pathology, 2 for including minors, 1 for lack of periodic follow-ups, 5 for being duplicates within Google Scholar, 2 for being duplicates in PubMed, and 1 for being a duplicate in Lilacs. After these exclusions, 59 publications were included, of which only 47 specifically featured a definitive palatal obturator as the type of prosthesis.
2.6. Data Extraction Process
Titles and abstracts were analyzed independently by two authors (H.Z. and S.P.). If they considered a study inappropriate based on the title and abstract, the study was excluded. A third author (B.A.) resolved any disagreements.
Graphs and tables were created using a spreadsheet application named Google Sheets.
No effect measures of the outcome were determined. None of the articles included were excluded.
2.7. Quality Assestment
Two authors (H.Z. and S.P.) independently evaluated the methodological quality of all included studies. These authors did not use a pre-packaged standard tool but instead personally evaluated each included articles and applied a systematic and transparent approach consistent with the principles of criteria appraisal, integrating elements from the methods provided by JBI (for case series) and the Cochrane handbooks for non-randomized studies. This ensures a methodologically informed assessment tailored to the unique characteristics of the literature on palatal obturators.
In the valuation of the included articles, the authors independently read all the text and deliberately selected what types of bias influenced each single article. The types of bias identified from each single article were gathered and used to reevaluate every single article to assess all the articles with all the types of bias found.
All the types of bias identified were selection bias, publication bias, reporting bias, linguistic/geographical bias, and technological bias.
The evaluation of the type of bias used three risk levels: “high”, “moderate”, and “low”. The “high” risk corresponds to bias that was immediately identified in the analyzed article. The “moderate” risk corresponds to bias that was identified as valid after the reevaluation of all articles with all the types of bias. The “low” risk corresponds to bias that was identified as less valid after the reevaluation of all articles with all the types of bias.
A third author (B.A.) resolved any disagreements.
Graphs and tables were created using a spreadsheet application named Google Sheets.
3. Results
3.1. Study Characteristics
A total of 59 publications were selected, comprising 50 case reports, 8 case series, and 1 prospective cohort study (Table 1).

Table 1.
Table showing the research results.
3.2. Characteristics of the Identified Subject
These 59 publications included 83 subjects, 46 male and 37 female (Figure 2), with ages ranging from 21 to 90 years, an average age of 54.59 years, and a standard deviation of 13.76 years (Figure 3). That is, 68.27% of the subjects were adults with ages ranging from 40.83 to 68.35 years.
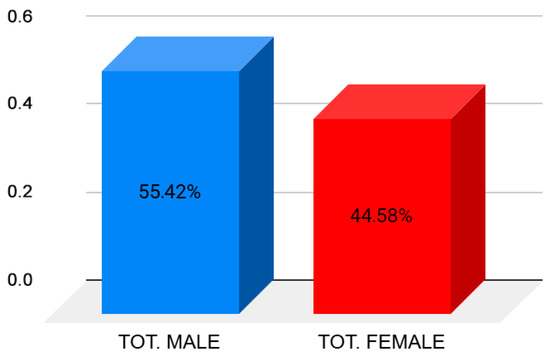
Figure 2.
Histogram representing the percentage of analyzed subject by gender.
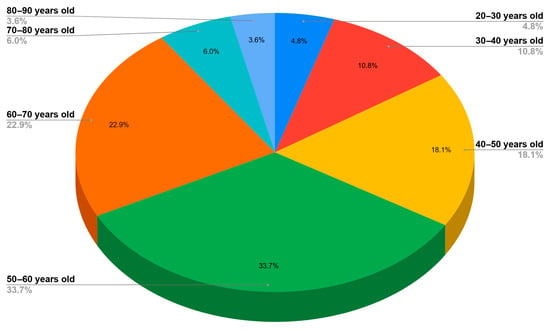
Figure 3.
Pie chart representing the age group distribution of the analyzed subjects.
3.3. Characteristics of the Palatal Defect
3.3.1. Cause of Maxillectomy
The maxillary defect was caused by mucormycosis in 30 patients and squamous cell carcinoma in 17 patients. Additionally, adenoid cystic carcinoma, mucoepidermoid carcinoma, and CIMDL were each observed in four patients, while pleomorphic adenoma and BRONJ affected three patients each, and melanoma was reported in two patients. The following conditions were each identified in one patient: pleomorphic adenocarcinoma, ameloblastoma, cemento-ossifying fibroma, basal cell carcinoma, epithelial-myoepithelial carcinoma, radiotherapy-induced fibrosis, oro-nasal fistula, central giant cell granuloma, dentoalveolar infection, cleft lip and palate, chemical injury, extranodal NK/T-cell lymphoma (nasal type), odontogenic myxoma, osteosarcoma, myofibroblastic sarcoma, and Van der Woude syndrome (Figure 4).
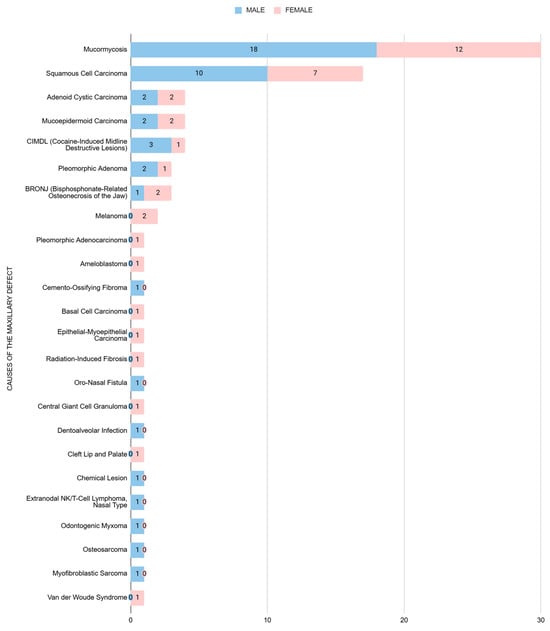
Figure 4.
Bar chart showing the number of individuals affected by each pathology causing the maxillary defect, categorized by gender.
The most frequent pathology leading to palatal defects that were managed prosthetically was mucormycosis, followed by squamous cell carcinoma.
Mucormycosis is a severe fungal infection associated with fulminant fungal sinusitis, usually in people who are immunocompromised. Symptoms depend on where in the body the infection occurs. It most commonly infects the nose, sinuses, eyes, and brain, resulting in a runny nose, one-sided facial swelling and pain, headache, fever, blurred vision, bulging or displacement of the eye (proptosis), and tissue death. It is curable only when diagnosed early, and the fatality rate is about 54%.
Oral squamous cell carcinoma is the most frequent malignant neoplasm of the oral cavity, and it is one of the most common cancers among males worldwide. The survival rates of oral squamous cell carcinoma are low, and they vary among ethnicities and age groups.
3.3.2. Location of the Defect
The defect location for the palatal obturator was on the left side in 24 patients, on the right side in 21 patients, bilateral in 20 patients, and undefined in 18 patients.
The defect site involved only the hard palate in 60 patients, only the soft palate in 4 patients, both locations in 15 patients, was unspecified in 4 patients, and occurred in another location in 2 patients.
The most frequent defect site involved by a palatal obturator was the hard palate (about 90.4% of the subjects). The sides of the maxillary defect were not significant because cases with unknown sides comprised 21.7%, but if we observe the known data, the number of subjects with a known side were similarly distributed on the left side (36.92%), right side (32.31%), and bilateral side (30.77%).
3.4. Characteristics of Palatal Obturator
3.4.1. The Type of Prosthesis
The type of prosthesis was total in 22 devices, partial in 43 devices, palatal in 6 devices, and unspecified in 12 devices.
The most detected type of specified rehabilitation was the partial obturator prosthesis (60.56%). Of these devices, teeth abutment was exploited in 34.88% of cases by wire clasps and in 58.14% of cases by framework clasps.
3.4.2. The Modification of the Prosthesis
The prosthesis was characterized by implant sustainment in 7 cases, magnet retention in 5 cases, velopharyngeal extension in 8 cases, and a hollow bulb in 25 cases.
The most frequent modification of the prosthesis was the creation of a cavity in the prosthesis, called a hollow bulb.
3.5. Characteristic of the Fabrication of the Prosthesis
3.5.1. The Method of Fabrication
The palatal obturator was fabricated using the traditional method in 44 cases, the digital method in 18 cases, and was not specified in 21 cases.
3.5.2. The Impression Material
Impression materials used included alginate in 46 cases, silicone in 24 cases, polyether in 16 cases, wax in 3 cases, tissue conditioner in 3 cases, polysulfide in 2 cases, zinc oxide–eugenol paste in 1 case, and zinc oxide paste without eugenol in 1 case. A digital scanner was used in four cases, and CBCT was used in one case to obtain impressions. In 22 cases, the impression material was not specified; in 2 cases, the definitive impression material was not defined; and in 1 case, the preliminary impression material was not specified.
3.6. Evaluation of Bias
Analysis of the 59 included articles revealed the presence of several methodological biases that affect their quality, external validity, and clinical applicability (Table 2):

Table 2.
Table showing the valuated bias for every article analyzed. The level of risk of bias is evaluated with the grade “high”, “moderate”, and “low”.
- (1)
- Selection Bias: Most of the analyzed studies consist of case reports or case series (91.5%), with a near-total absence of controlled or randomized studies. This constitutes a significant selection bias, as the reported cases do not represent a random or representative sample but rather clinical scenarios selected for their rarity, success, or academic interest. Consequently, the generalizability of the findings is markedly limited, reducing their applicability to routine clinical practice;
- (2)
- Publication Bias: Many studies report highly favorable outcomes, such as complete functional rehabilitation, absence of recurrence even in the long term (e.g., 10-year follow-up), or excellent aesthetic results. This trend suggests a significant publication bias, reflecting the higher likelihood of publishing cases with positive outcomes compared to those involving complications, therapeutic failures, or functional limitations. Such bias may lead to an overestimation of the clinical efficacy of the prosthetic approaches described;
- (3)
- Reporting Bias: A critical limitation is the lack of uniformity and completeness in clinical reporting. A substantial proportion of the articles lack essential information, including the classification of the maxillary defect (e.g., Aramany), the type of material used in the prosthesis, the impression technique (analog or digital), and the duration of follow-up. This reporting bias hampers comparative analysis across studies and compromises reproducibility, thereby limiting the ability to draw reliable conclusions regarding the relative effectiveness of the techniques described;
- (4)
- Language and Geographic Bias: Several articles originate from local, non-English-language journals or journals with limited indexing (e.g., Brazilian, Turkish, or Egyptian journals). This introduces both language and geographic bias, as the study selection may not accurately reflect the global literature but rather be influenced by language and database availability. This may result in underrepresentation of clinical experiences from regions with high scientific output (e.g., the United States, Western Europe, etc.) and conversely overrepresentation of less standardized reports;
- (5)
- Technological Bias: Lastly, a notable technological bias was observed due to the limited presence of studies utilizing digital workflows (CAD/CAM, 3D printing, and intraoral scanners). Only a minority of the articles mention the use of such technologies, and even fewer provide comprehensive digital protocols. This limitation reflects both a slow rate of technological adoption in certain clinical settings and a potential disparity in access to digital resources factors that should be considered when evaluating prosthetic solutions.
4. Discussion
This review has examined the available literature on the use of the palatal obturator in the rehabilitation of maxillary defects, aiming to analyze the most common conditions to which it applies, its possible clinical indications, the most commonly used materials, the most frequent fabrication techniques, and its functional characteristics.
4.1. Cause of Maxillectomy
According to the collected data, the most frequent pathology leading to palatal defects that are managed prosthetically is mucormycosis (36.14%), followed by squamous cell carcinoma (20.48%). However, the data on mucormycosis, when analyzed using a temporal criterion, appear to be significantly influenced by the COVID-19 pandemic, with the first cases reported on 31 December 2019. Indeed, COVID-19 has been associated with an increased incidence of mucormycosis [82]. Specifically, mucormycosis was found to be associated with COVID-19 in 73.33% of the analyzed cases, while no associations was observed in 4 cases, one of which, as reported by Salahuddin et al. [43], occurred in the absence of any identifiable risk factors (Table 3).

Table 3.
Table showing the various condition correlated to mucormycosis.
Disregarding the misleading data, the results of the research on the frequency of pathologies leading to maxillary defects are consistent with the data reported in the literature, like those reported by Spiro et al. [83].
Besides the compromission of chewing, speech, and aesthetics caused by these types of defects, these patients also had diseases that lead to systemic complications to the general health of the person. Knowing the most used materials, the most frequent fabrication techniques, and their functional characteristics can help the clinician to speed up the process of prosthetic rehabilitation and to guarantee, with confidence, the comfortability and security of the patient.
4.2. Ideal Indications and Requirements
The thorough analysis of the researched literature has made it possible to identify and comprehensively define the ideal requirements for designing and manufacturing a maxillary obturator:
- Assisting the patient in performing natural functions such as speech, swallowing, and chewing by restoring oral functionality compromised due to the anatomical defect. The prosthesis should closely resemble natural tissues, enhancing not only function but also the patient’s aesthetics. Maintaining periodontal health is not only essential for oral rehabilitation but may also play a role in reducing the risk of neurodegenerative diseases such as Alzheimer’s [84];
- The prosthetic design should allow for easy and quick application, ensuring that the device remains securely and comfortably in place without causing discomfort or instability;
- The prosthesis should be made of durable materials capable of maintaining their physical, aesthetic, and functional properties over time, preserving their original polish and finish for a reasonable period. Chitosan has been shown to promote tissue regeneration and reduce microbial colonization in oral surgery applications [85];
- The prosthesis should be easy to clean, allowing for proper maintenance and oral hygiene, preventing plaque and bacterial buildup, and reducing the risk of infections or other complications.
4.3. Palatal Obturator
4.3.1. Characteristics of Palatal Obturator
In the partial obturator prosthesis, most of the teeth abutment was exploited by framework claps. This means that partial obturator prosthesis is preferred with a metal framework that guarantees more comfort and stability by better retention, a lower thickness, and a lower weight.
The most commonly used material in definitive obturator prostheses is acrylic resin (100% of the specified cases). The main advantages of this material include its resistance to flexion and fatigue, high chemical stability, and ease of modeling. However, its disadvantages include rigidity and porosity [86].
4.3.2. Impression Taking Technique
In the researched literature, various impression-taking techniques are described for patients with palatal defects. In the traditional protocol, through the exclusion of the unspecified cases (26.51% of them), 70.49% of the examined studies involve the fabrication of two impressions: a preliminary impression and a definitive impression. The preliminary impression is predominantly taken with alginate (86.05% of cases), a material that is easy to handle, sets quickly, and is more cost-effective compared to elastomeric materials [87].
This initial impression allows for the creation of a diagnostic model, which is essential for treatment planning and the fabrication of a custom impression tray. The definitive impression, on the other hand, is often made using more detailed materials such as silicone (41.86% of cases) or polyether (37.41% of cases), which provide greater precision in recording the anatomical structures surrounding the defect. In some cases, as reported by Domingues et al. [2] and Aeran et al. [38], a site protection technique is used, involving the insertion of a gauze soaked in Vaseline or a betadine solution inside the cavity. This precaution helps prevent the extravasation of impression material into the nose or maxillary sinuses. In the traditional protocols, 18.03% of the studies mentioned only one impression material, with the prevalence of alginate (7 cases of 11), and 4.92% of the studies did not carry out the impression.
In recent years, advancements in digital technologies have introduced the use of intraoral scanners for impression taking, reducing the need for traditional impression materials. Optical imaging obtained with scanners such as the TRIOS 3Shape allows for highly precise acquisition of the morphology of the palate and surrounding tissues, enabling the digital design of the palatal obturator. This technology, used in CAD/CAM workflows, facilitates the fabrication of custom obturators through 3D printing, improving prosthetic fit quality and reducing laboratory processing times [88]. Only 6.56% of studies with specified impression procedures used the digital method.
4.3.3. Enhancement of the Palatal Obturator
The conventional obturator prosthesis can undergo various modifications to enhance its functional characteristics. These improvements can be categorized into retention, morpho-functional, and lightweight enhancements.
The retention of the prosthesis can be improved through the following methods:
- Implant Retention: This type of obturator is mainly used in the anterior segment of the maxilla, as bone loss in this area is approximately three times greater than in the posterior segment [89,90];
- Magnetic Retention: The two components are connected via magnets, which are positioned laterally and posteriorly to maximize leverage and prosthetic retention [91,92];
- Attachment Systems: In this type of prosthesis, the maxillary prosthesis and the obturator are connected by an attachment system, allowing the patient to separate them for insertion, removal, and cleaning and then reconnect them in the mouth. This system is particularly beneficial for patients with limited mouth opening [93].
The obturator prosthesis can include a velopharyngeal extension that restores soft palate defects and corrects speech. This type of prosthesis extends beyond the residual soft palate to create a separation between the oropharynx and nasopharynx, providing a fixed structure against which the pharyngeal muscles can function to facilitate palatopharyngeal closure [94]. Of all the analyzed cases with soft palate defect, only 42.11% of these created the velopharyngeal extension; in three of them, the defect was only on the soft palate, and in five of them, the defect involved the hard palate, too.
Lightness is an important characteristic of the palatal obturator, as it provides greater retention by counteracting the force of gravity [95].
This can be achieved through bulb cavitation, which also improves speech articulation and reduces nasality [96].
The generation of the cavity in the bulb can be achieved through various techniques documented in the scientific literature, which can be classified into digital methods [97] and analog methods, like wax shim, sugar, acrylic resin shim, polyurethane foam, plaster matrix, cellophane-wrapped asbestos, silicone putty, light-body coated gauze, thermocol, dental stone, play dough, salt, gelatin soap, alum, etc. [98].
4.4. Comparison with Other Similar Studies
Many studies have evaluated the clinical outcomes, the functional outcomes, and the quality of life of patients with maxillary defects rehabilitated with an obturator prosthesis [99,100], also comparing them with other therapeutic indications such as free tissue transfers [19]. However, none of these focused on the materials and techniques used in prosthesis fabrication.
4.5. Limitations of This Systematic Review
The review contains several limitations, each of which may affect the reliability and applicability of the conclusions.
There is a predominance of low-level evidence caused by the inclusion of 50 case reports, 8 case series, and only 1 prospective cohort study. Case reports and case series provide anecdotal evidence and lack control groups, making them prone to bias and limiting generalizability. The scarcity of higher-level evidence (e.g., randomized controlled trials) reduces the strength of the conclusions about the efficacy and reliability of palatal obturators.
There is a limited use of digital technologies; in fact, only 6.56% of studies with specified impression procedures used digital methods like intraoral scanning. This underrepresents modern fabrication techniques that are increasingly becoming standard in clinical settings. Consequently, the review may not fully reflect the current and future potential of CAD/CAM and digital workflows in obturator prosthesis design.
There are unspecified or incomplete data in these studies. Many included studies did not specify critical parameters such as materials used, exact impression methods, or prosthesis design details (e.g., 28 unspecified materials and 22 unspecified impression materials). These incomplete data limit comparative analysis and hinder reproducibility or development of evidence-based protocols for obturator fabrication and clinical application.
There is a lack of quantitative meta-analysis and without statistical synthesis, and it is difficult to assess the overall effect size or draw strong, evidence-based conclusions about clinical outcomes.
The review relies heavily on published case reports and series, which are more likely to highlight successful outcomes. Negative or failed outcomes are often underreported, potentially overestimating the success and functionality of obturator prostheses.
4.6. Recommendations for Future Research
In light of the above, it is hoped that future studies will explore the bio-mechanical characteristics of innovative materials and the impact of new technologies on comfort and therapeutic adherence, thus contributing to the continuous improvement of rehabilitative strategies for patients with maxillary defects.
The combined presence of these biases raises significant methodological concerns and suggests that the current body of evidence, while valuable for describing individual clinical solutions, is insufficient to support strong or generalizable clinical recommendations. Moving forward, it will be essential to promote more rigorous inclusion criteria, broader database and language coverage, and, ideally, meta-analytic statistical analysis to enhance the strength of the evidence.
Only through these improvements can we build a robust evidence base to support prosthetic rehabilitation in patients with maxillary defects.
5. Conclusions
The rehabilitation of maxillary defects represents a complex clinical challenge that requires an integrated, multidisciplinary, and personalized approach.
The obturator allows for the satisfactory restoration of the main orofacial functions, significantly improving the patient’s quality of life not only from a functional perspective but also aesthetically and psychologically. The adoption of digital technologies, such as CAD/CAM design, has significantly improved the precision in the fabrication of these prostheses, facilitating anatomical adaptation and reducing postoperative complications. However, the literature emphasizes the need to standardize protocols for impression taking, material selection, and processing phases in order to ensure more effective and reproducible prosthetic rehabilitation. Furthermore, the evidence gathered indicates that optimal management of a patient with a maxillary defect must be based on an accurate etiopathogenic diagnosis, careful functional evaluation, and constant follow-up.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/prosthesis7050112/s1. PRISMA 2020 Main Checklist.
Author Contributions
Conceptualization and methodology, C.S.; writing—original draft preparation, B.A., H.Z.H. and P.S.; writing—review and editing, C.G. and L.D.; supervision, C.S.; validation, F.C. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Italian Ministry of Health—Current Research IRCCS.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| DX | Right position |
| SX | Left position |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| CAD | Computer-aided design |
| CAM | Computer-aided manufacturing |
| CIMDL | Cocaine-induced midline destructive lesions |
| CBCT | Cone beam computed tomography |
| COVID-19 | Coronavirus disease of 2019 |
| BRONJ | Bisphosphonate-related osteo-necrosis of the jaws |
References
- Ali, M.M.; Khalifa, N.; Alhajj, M.N. Quality of life and problems associated with obturators of patients with maxillectomies. Head Face Med. 2018, 14, 2. [Google Scholar] [CrossRef] [PubMed]
- Domingues, J.M.; Corrêa, G.; Fernandes Filho, R.B.; Hosni, E.S. Palatal obturator prosthesis: Case series. RGO Rev. Gaúcha Odontol. 2016, 64, 477–483. [Google Scholar] [CrossRef]
- Ohno, T.; Hojo, K.; Fujishima, I. Soft obturator prosthesis for postoperative soft palate carcinoma: A clinical report. J. Prosthet. Dent. 2018, 119, 845–847. [Google Scholar] [CrossRef]
- Chen, C.; Ren, W.; Gao, L.; Cheng, Z.; Zhang, L.; Li, S.; Zhi, P.K. Function of obturator prosthesis after maxillectomy and prosthetic obturator rehabilitation. Braz. J. Otorhinolaryngol. 2016, 82, 177–183. [Google Scholar] [CrossRef]
- Tripathi, A.; Gupta, A.; Arora, V. Effect of prosthodontic rehabilitation of maxillary defects on hypernasality of speech. J. Prosthodont. 2016, 25, 202–206. [Google Scholar] [CrossRef]
- Corsalini, M.; Barile, G.; Catapano, S.; Ciocia, A.; Casorelli, A.; Siciliani, R.; Di Venere, D.; Capodiferro, S. Obturator prosthesis rehabilitation after maxillectomy: Functional and aesthetical analysis in 25 patients. Int. J. Environ. Res. Public Health 2021, 18, 12524. [Google Scholar] [CrossRef] [PubMed]
- Trimarchi, M.; Bondi, S.; Della Torre, E.; Terreni, M.R.; Bussi, M. Palate perforation differentiates cocaine-induced midline destructive lesions from granulomatosis with polyangiitis. Acta Otorhinolaryngol. Ital. 2017, 37, 281–285. [Google Scholar] [CrossRef]
- Krishna, C.H.; Babu, J.K.; Fathima, T.; Reddy, G.V. Fabrication of a hollow bulb prosthesis for the rehabilitation of an acquired total maxillectomy defect. BMJ Case Rep. 2014, 2014, bcr2013201400. [Google Scholar] [CrossRef]
- Choudhury, M.; Shanmuganathan, N.; Padmanabhan, T.V.; Swarup, S.; Grover, M.; Arumugam, M. Rehabilitation of post surgical maxillectomy defects using interim obturators—A case series. Indian J. Surg. Oncol. 2014, 5, 315–320. [Google Scholar] [CrossRef]
- Artopoulou, I.I.; Karademas, E.C.; Papadogeorgakis, N.; Papathanasiou, I.; Polyzois, G. Effects of sociodemographic, treatment variables, and medical characteristics on quality of life of patients with maxillectomy restored with obturator prostheses. J. Prosthet. Dent. 2017, 118, 783–789.e4. [Google Scholar] [CrossRef] [PubMed]
- Ceraulo, S.; Carini, F.; Viscardi, D. Nuovo approccio clinico sulla fonetica in pazienti oncologici con protesi otturatoria. Caso clinico. Dental Cadmos 2023, 91, 881–886. [Google Scholar] [CrossRef]
- Barbarisi, A.; Cremonini, F.; Lauritano, D.; Visconti, V.; Caccianiga, G.; Ceraulo, S. Association between periodontal disease and oral benign, potentially malignant, malignant, and chronic immune mediated disorders: A clinical study. Healthcare 2024, 12, 1999. [Google Scholar] [CrossRef]
- Nelke, K.; Matys, J.; Janeczek, M.; Małyszek, A.; Łuczak, K.; Łukaszewski, M.; Frydrych, M.; Kulus, M.; Dąbrowski, P.; Nienartowicz, J.; et al. The Occurrence and Outcomes of Cemento-Osseous Dysplasias (COD) in the Jaw Bones of the Population of Lower Silesia, Poland. J. Clin. Med. 2024, 13, 6931. [Google Scholar] [CrossRef] [PubMed]
- European Union Drugs Agency (EUDA). Cocaine—The Current Situation in Europe. European Drug Report. 2023. Available online: https://www.emcdda.europa.eu (accessed on 12 August 2025).
- Rampi, A.; Vinciguerra, A.; Bondi, S.; Policaro, N.S.; Gastaldi, G. Cocaine-induced midline destructive lesions: A real challenge in oral rehabilitation. Int. J. Environ. Res. Public Health 2021, 18, 3219. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Cardelli, P.; Bigelli, E.; Vertucci, V.; Balestra, F.; Montani, M.; De Carli, S.; Arcuri, C. Palatal obturators in patients after maxillectomy. Oral Implantol. 2015, 7, 86–92. [Google Scholar]
- Smith, J.; Doe, A.; Kumar, R. Bridging the gap between immediate surgical and definitive oral rehabilitation with interim obturators: A case report. Cureus 2024, 16, e332234. [Google Scholar]
- Brandão, T.B.; Vechiato Filho, A.J.; Batista, V.E.; de Oliveira, M.C.; Santos-Silva, A.R. Obturator prostheses versus free tissue transfers: A systematic review of the optimal approach to improving the quality of life for patients with maxillary defects. J. Prosthet. Dent. 2016, 115, 247–253.e4. [Google Scholar] [CrossRef]
- Rimaoui, S.; El Assraoui, K.; Bellemkhannate, S. Immediate surgical obturator prosthesis: Case report. Eur. J. Dent. Oral Health 2023, 4, 17–21. [Google Scholar] [CrossRef]
- Durrani, Z.; Hassan, S.G.; Alam, S.A. A study of classification systems for maxillectomy defects. JPPA 2013, 1, 117–124. Available online: https://jppa.pk/jppa/article/view/23 (accessed on 12 August 2025).
- Alqarni, H.; Alfaifi, M.; Ahmed, W.M.; Almutairi, R.; Kattadiyil, M.T. Classification of maxillectomy in edentulous arch defects, algorithm, concept, and proposal classifications: A review. Clin. Exp. Dent. Res. 2023, 9, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Brucoli, M.; Boffano, P.; Pezzana, A.; Corio, C.; Benech, A. The use of optical scanner for the fabrication of maxillary obturator prostheses. Oral Maxillofac. Surg. 2020, 24, 157–161. [Google Scholar] [CrossRef]
- Taqi Fadhil, S.M.; Mumcu, E. Rehabilitation of a patient with palatal defect—A case report. J. Surg. Surgical Res. 2019, 5, 93–96. [Google Scholar] [CrossRef]
- Correia-Neto, I.J.; Correa, M.B.; Araújo, A.L.D.; Penafort, P.V.M.; Colafemina, A.C.E.; Elias, R.D.A.; Lopes, M.A. A primary oral mucosal melanoma of the hard palate with no recurrence: Report of a 10 years follow-up. Spec. Care Dentist. 2024, 44, 751–755. [Google Scholar] [CrossRef]
- Bañaga Cabrera, C.B.; Romero Muñoz, J.M.; Carrillo Collado, M.Á.; Muñoz Salcido, G.; López-Mendoza, J.A.; Mandujano Law, H.K.; Parreiras, S.O.; Cartagena, A.F. Prosthetic rehabilitation after hemimaxillectomy: A case report. Gen. Dent. 2023, 71, 36–41. [Google Scholar]
- Mughal, M.S.; Kaur, I.P.; Akbar, H.; Abbas, S.H.; Angi, P. Hard palate perforation in an elderly man with dementia. Cureus 2021, 13, e15872. [Google Scholar] [CrossRef]
- Vosselman, N.; Merema, B.J.; Schepman, K.P.; Raghoebar, G.M. Patient-specific sub-periosteal zygoma implant for prosthetic rehabilitation of large maxillary defects after oncological resection. Int. J. Oral Maxillofac. Surg. 2019, 48, 115–117. [Google Scholar] [CrossRef]
- Pinheiro, T.N.; Fayad, F.; Júnior, L.R.M.; Nichthauser, B.; Braga, F.; Passos, S.M. Palatal perforation and chemical ulcers of the tongue in a blind patient. Spec. Care Dentist. 2017, 37, 253–257. [Google Scholar] [CrossRef]
- Oki, M.; Kanazaki, A.; Taniguchi, H. Osteoradionecrosis following carbon ion radiotherapy: Case history report of a soft palate defect. Int. J. Prosthodont. 2016, 29, 448–450. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sathyanarayanan, R.; Suresh, V.; Therese Thomas, B.A. Polymorphous low-grade adenocarcinoma of the palate: A rare case report. Iran J. Cancer Prev. 2015, 9, e3447. [Google Scholar] [CrossRef]
- Murakami, M.; Nishi, Y.; Umezono, M.; Kamashita, Y.; Nishimura, M. Fabrication of a movable obturator following maxillary reconstruction with slit-shaped fenestration. J. Prosthodont. 2015, 24, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Troeltzsch, M.; Probst, F.; Troeltzsch, M.; Ehrenfeld, M.; Otto, S. Conservative management of medication-related osteonecrosis of the maxilla with an obturator prosthesis. J. Prosthet. Dent. 2015, 113, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Soares, M.E.C.; Falci, A.L.V.; Freitas, S.F.; Mesquita, A.T.M.; Galo, R. Reabilitação oral com prótese obturadora em comunicação buconasal após ocorrência de carcinoma de células escamosas: Relato de caso. Rev. Bras. Cancerol. 2022, 68, e192182. [Google Scholar] [CrossRef]
- Correia-Neto, I.J.; Correa, M.B.; Colafemina, A.C.E.; Roza, A.L.O.C.; Elias, R.A.; Vargas, P.A.; Lopes, M.A. Oral malignant melanoma on the palate: Case report with 10 years of follow-up. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2024, 137, e168. [Google Scholar] [CrossRef]
- Rattanakuntee, S.; Thosaporn, W.; Ketchaikosol, N.; Imerb, N. Granular cell ameloblastoma in maxilla: A report of rare case. Oral Maxillofac. Surg. Cases 2023, 9, 100299. [Google Scholar] [CrossRef]
- El Hussieny Fayad, N.; Nassar Mohammed, H. Retention and quality of life of different manufacturing techniques of palatal obturator for acquired palatal defect in treatment of post COVID-19 associated mucormycosis (CAM). Egypt. Dent. J. 2023, 69, 1221–1232. [Google Scholar] [CrossRef]
- Goyal, S. Palatal obturator—A case report. Univ. J. Dent. Sci. 2024, 10, 1. [Google Scholar] [CrossRef]
- Roslan, H.; Shahabudın, S. Palatal obturator prosthesis: A clinical case report. Cumhuriyet Dent. J. 2018, 21, 55–60. [Google Scholar] [CrossRef]
- Aeran, H.; Kumar, V.; Aeran, M. Enhancing quality of life: A hollow bulb obturator in palatal defect rehabilitation—A case report. Int. J. Oral Health Dent. 2023, 9, 234–238. [Google Scholar] [CrossRef]
- Trivedi, M.; Guddu, G.; Daftary, M.; Devikaa, T.C.; Chaudhary, R. Management of maxillary defect via obturator: A case report with review of literature. Turk. J. Physiother. Rehabil. 2022, 32, 35572–35581. [Google Scholar]
- Khan, A.; Akhtar, A.; Saleem, T. Oral rehabilitation of a geriatric patient with velopharyngeal insufficiency: A case report. J. Postgrad. Med. Inst. 2024, 38, 81–84. Available online: https://www.jpmi.org.pk/index.php/jpmi/article/view/3244 (accessed on 17 February 2024).
- Aradya, A.; Ranganatha, N.; HS, S.; Sandeep, G. Fabrication of single piece definitive obturator for post surgical maxillectomy defect during COVID-19 pandemic—A literature review with clinical case report. Bangladesh J. Med. Sci. 2022, 21, 676–684. [Google Scholar] [CrossRef]
- Saadellaoui, I.; Bekri, S.; Labidi, A.; Yaala, M.B.; Mabrouk, Y.; Mansour, L. Combination of CAD/CAM technologies and conventional processing in the fabrication of a maxillary obturator prosthesis: A clinical report. J. Med. Life 2024, 17, 375–380. [Google Scholar] [CrossRef]
- Salahuddin, A.; Abbasi, M.S. Prosthodontic management of maxillectomy patient with an obturator: A case report. Altamash J. Dent. Med. 2024, 3, 37–41. Available online: https://ajdm.altamash.edu.pk/index.php/ojs3/article/view/59 (accessed on 26 November 2024).
- Colvenkar, S.; Prakash, R.; Fatima, S.; Ahmed, M.S.; Reddy, G.K. Prosthodontic rehabilitation of a completely edentulous patient with a cleft palate: A case report. Cureus 2023, 15, e33522. [Google Scholar] [CrossRef] [PubMed]
- Saadellaoui, I.; Nasri, B.; Bekri, S.; Labidi, A.; Rezigui, S.; Mansour, L. Velo-palatal obturator prosthesis after maxillectomy following squamous cell carcinoma: A case report. Prosthodontics 2024, 74, 238–248. [Google Scholar] [CrossRef]
- Khan, M.W.U.; Naeem, S.; Iqbal, Q. Prosthetic rehabilitation of an acquired maxillary defect with definitive obturator prosthesis—A clinical technique. J. Pak. Dent. Assoc. 2020, 29, 100–102. [Google Scholar] [CrossRef]
- Singhal, M.K.; Ahmad, F.; Nair, C.; Bankoti, P. A cast partial obturator with hollow occlusal shim and semi-precision attachment. Indian J. Dent. Res. 2018, 29, 123–127. [Google Scholar] [CrossRef]
- Rathee, M.; Divakar, S.; Jain, P.; Alam, M.; Singh, S. Post maxillectomy rehabilitation and amelioration of quality of life of post-COVID rhinocerebral mucormycosis patients using obturator: A case series. J. Fam. Med. Prim. Care 2022, 11, 7476–7482. [Google Scholar] [CrossRef]
- Bisoc, A.; Ciavoi, G.; Țig, I.A.; Dina, M.N.; Popovici, R.A.; Todor, L.; Andrei, O.C. Fabricating an obturator prosthesis after maxillectomy in a rare case of adenoid cystic carcinoma—Case report and review of the literature. Res. Clin. Med. J. 2020, 4, 25–30. [Google Scholar]
- Ximenes, I.S.; Malta, C.E.N.; Martins, J.O.L.; Lemos, J.V.M.; Barros, L.O.; Gomes, C.E.A.; Verde, R.M.B.L. Oral rehabilitation after partial maxillectomy for removal of pleomorphic adenoma: Case report. RGO Rev. Gaúcha Odontol. 2023, 71, e20230001. [Google Scholar] [CrossRef]
- Abrol, K.; Pandey, S.; Agarwal, S.; Tripathi, S. Prosthodontic management of sub-total maxillectomy: A case report. Chron. Dent. Res. 2019, 8, 1. [Google Scholar]
- Javed, B.; Agarwal, S.; Nayak, D.; Singh, K. Prosthodontic management of oromaxillary defect: A case report. J. Orofac. Rehabil. 2021, 1, 102–105. [Google Scholar] [CrossRef]
- Faheemuddin, M.; Yazdanie, N.; Nawaz, M.S. Impact of prosthodontic treatment on the oral health related quality of life in a maxillectomy patient with multiple impairments. J. Ayub Med. Coll. Abbottabad 2014, 26, 246–251. [Google Scholar]
- Chebbi, K.; Bouaziz, K.; Tayari, O.; Berkaoui, A.; Bouzidi, M.A.; Jaouadi, J. Palatal obturator after maxillectomy following squamous cell carcinoma. Case Rep. Dent. 2022, 2022, 5545333. [Google Scholar] [CrossRef]
- Rawas, M.A.; Rashid, F.; Barman, A.; Farook, T.H.; Oulabi, A.A.; Nafi, B.J.; Mohammad, K.A. Sustaining an obturator prosthesis with zygomatic suspension wires in a case of subtotal maxillectomy and insufficient ridge supported retention: A case report. Bangladesh J. Med. Sci. 2020, 19, 582–585. [Google Scholar] [CrossRef]
- Arantes, D.C.; Rodrigues, R.A.A.; de Arruda, J.A.A.; de Magalhães, C.S.; Mesquita, R.A.; Goyatá, F.R.; Moreira, A.N.; Moreno, A. Maxillofacial prosthetic rehabilitation of patients with resection of squamous cell carcinoma: A report of two cases. Contemp. Clin. Dent. 2020, 11, 294–297. [Google Scholar] [CrossRef]
- Özcivelek, T.; Kılıçarslan, M.A. Full digital workflow of a 2-piece obturator with polyetherketoneketone in a patient with maxillectomy and trismus: A clinical and laboratory report. J. Prosthet. Dent. 2024, 131, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Riegel, C.; Grando, C.; Brum, R.S.; Brucker, M.R.; Maito, F.L. Multidisciplinary diagnosis and treatment of oral squamous cell carcinoma after oro-antral communication: 2 years of follow-up. J. Oral Diagn. 2020, 5, 1–5. [Google Scholar] [CrossRef]
- Siraj, H.; Al-Gorashi, A.; Moussa, K.; El-Sheikh, A. Prosthetic rehabilitation of acquired maxillectomy defect: A case report with 10 years follow-up. Int. J. Med. Dent. Case Rep. 2014, 1, 271114. [Google Scholar] [CrossRef]
- Chahal, S.; Dahiya, D.; Nagar, P.; Mittal, S. Digitally fabricated precision attachment with cast partial framework retained obturator in a partial maxillectomy patient following mucormycosis: A case report. Natl. J. Maxillofac. Surg. 2024, 15, 332–336. [Google Scholar] [CrossRef]
- Joseph, A.; Hazari, P.; Somkuwar, K.; Yadav, N.S.; Mahajan, H.; Narwani, S. Prosthetic rehabilitation of a rhinocerebral mucormycosis patient. J. Appl. Dent. Med. Sci. 2021, 7, 35–39. [Google Scholar] [CrossRef]
- De Riu, G.; Soma, D.; Biglio, A.; Raho, M.T.; Mura, D.; Michelon, F.; Salzano, G.; Piombino, P.; Lechien, J.R.; Vaira, L.A. Primary reconstruction of total maxillectomy with custom-made subperiosteal implant and temporal muscle flap: A case report. Appl. Sci. 2023, 13, 6269. [Google Scholar] [CrossRef]
- Gueutier, A.; Kün-Darbois, J.-D.; Laccourreye, L.; Breheret, R. Anatomical and functional rehabilitation after total bilateral maxillectomy using a custom-made bone-anchored titanium prosthesis. Int. J. Oral Maxillofac. Surg. 2019, 49, 392–396. [Google Scholar] [CrossRef]
- Suenaga, H.; Iikubo, M.; Tamahara, T.; Dodo, M.; Peck, C.; Koseki, T.; Sasaki, K. Dental care using an oral appliance to support hematopoietic stem cell transplantation for NK/T cell lymphoma, nasal type, with palatal perforation. J. Prosthodont. Res. 2022, 66, 353–356. [Google Scholar] [CrossRef]
- El Charkawi, H.; Nasar, H. Prosthetic management of palatal perforation in heroin abuse patient. Dent. Oral Craniofac. Res. 2015, 1, 126–130. [Google Scholar] [CrossRef]
- Bhargava, A.; Soni, S.; Raj, K.; Gupta, M.; Deshpande, R.; Khan, M.F. Analog and digital protocols for functional prosthetic rehabilitation of post-COVID-19 rhino-orbito cerebral mucormycosis maxillofacial defects: A case series. J. Pharm. Bioallied Sci. 2023, 15 (Suppl. S2), S1347–S1350. [Google Scholar] [CrossRef] [PubMed]
- Sundar, M.K.; Kumar, G.P.S.; Lakhanpal, S. A Comprehensive Prosthodontic Management of Subtotal Maxillectomy. Int. J. Prosthodont. Restor. Dent. 2014, 4, 120–126. [Google Scholar] [CrossRef]
- Kudva, A.; Srikanth, G.; Singh, A.; Chitra, A.; Suryanarayan, R.K.; Francis, M. Reconstruction of maxillary defects using virtual surgical planning and additive manufacturing technology: A tertiary care centre experience. J. Maxillofac. Oral Surg. 2024, 23, 644–652. [Google Scholar] [CrossRef]
- Ouaalla, M.; El Assraoui, K.; Zeroual, R.; Bellemkhannate, S. Rehabilitation of a patient with partial maxillectomy: A case report. Integr. J. Med. Sci. 2021, 9, 481. [Google Scholar] [CrossRef]
- Negreiros, W.A.; Teixeira, R.R.; Peixoto, R.F.; Regis, R.R. The challenge of managing oral maxillofacial rehabilitation with quality and cost-benefit. J. Prosthet. Dent. 2022, 127, 508–514. [Google Scholar] [CrossRef]
- Rafique, M.A.; Khan, S.; Ahmed, H. Restoration of a post-surgical defect by magnetic maxillofacial prosthesis: A case report. J. Univ. Med. Dent. Coll. 2020, 11, 44–48. [Google Scholar] [CrossRef]
- Ali, I.; Srivastava, R.K.; Wadhwani, P.; Dubey, M.; Parveen, G.; Singh, S.; Yadav, A.K. Odontogenic myxoma in maxilla: A case report and review. Univ. J. Dent. Sci. 2015, 1, 1–2. [Google Scholar]
- Gudala, R.; Botu, B.R.; Gadadasu, S.; Vaddeswarapu, R.M.; Lokesh, K.V.; Sarvepalli, M. Van Der Woude Syndrome: A case report. J. Res. Adv. Dent. 2021, 11, 236–241. [Google Scholar]
- Anous, M.; Alotaibi, M.; Alqahtani, R.; Alhendi, F. Sino-nasal mucormycosis in non-compliant insulin-dependent diabetic patient: A case report with an insight on underlying psychological factors. Surg. Case Rep. 2024, 1, 100005. [Google Scholar] [CrossRef]
- Selukar, M.; Godbole, S.; Tawade, S.U.; Nimonkar, S. Troubleshooting in designing and fabricating a hollow bulb cast partial denture in a partial maxillectomy patient: A case report. Cureus 2024, 16, e58220. [Google Scholar] [CrossRef] [PubMed]
- Saxena, D.; Pahwa, A.; Kumar, A. Rehabilitation of acquired maxillary defect with patient-specific implants post-mucormycosis resection: A case report. Cureus 2024, 16, e70784. [Google Scholar] [CrossRef] [PubMed]
- Bak, S.Y.; Oh, W.S.; Erman, A. Treatment of velopharyngeal dysfunction: A clinical report. J. Prosthet. Dent. 2020, 123, 888–891. [Google Scholar] [CrossRef] [PubMed]
- Nanda, A.; Koli, D.; Sharma, S.; Suryavanshi, S.; Verma, M. Alleviating speech and deglutition: Role of a prosthodontist in multidisciplinary management of velopharyngeal insufficiency. J. Indian Prosthodont. Soc. 2015, 15, 281–283. [Google Scholar] [CrossRef]
- Sudhakar, S.; Velugubantla, R.G.; Erva, S.; Chennoju, S.K. Management of mucoepidermoid carcinoma of the palate utilizing (18)F-FDG PET/CT. J. Clin. Imaging Sci. 2014, 4 (Suppl. S2), 5. [Google Scholar] [CrossRef]
- Abdullah, B.; Museedi, O.; Allawi, N.; Ismael, F.J.; Warnakulasuriya, S. Impact of COVID-19 on the prevalence of oral and maxillofacial disorders: A retrospective cohort study. Sci. Prog. 2025, 108, 1. [Google Scholar] [CrossRef]
- Spiro, R.H.; Strong, E.W.; Shah, J.P. Maxillectomy and its classification. Head Neck 1997, 19, 309–314. [Google Scholar] [CrossRef]
- Barbarisi, A.; Visconti, V.; Lauritano, D.; Cremonini, F.; Caccianiga, G.; Ceraulo, S. Correlation between periodontitis and onset of Alzheimer’s disease: A literature review. Dent. J. 2024, 12, 331. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Fiorillo, L.; Cervino, G.; Bramanti, E.; Campagna, P.; Cicciù, A. Chitosan use in dentistry: A systematic review of recent clinical studies. Mar. Drugs 2019, 17, 417. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Laino, L.; Troiano, G.; Amoroso, G.R.; Crimi, S.; Bianchi, A.; Nastro Siniscalchi, E.; Cicciù, M. Alginate materials and dental impression technique: A current state of the art and application to dental practice. Materials 2019, 12, 3452. [Google Scholar] [CrossRef]
- Niakan, S.; Asgari, N.; Rafeie, N.; Barati, S. Severe Maxillectomy Defect Rehabilitation with an Implant-Retained Obturator Prosthesis: A Case Report. Front. Dent. 2024, 9, 2. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Paul, A.; Dhawan, P.; Jain, N. Digital applications in the fabrication of obturators in maxillectomy defects: A systematic review. Cureus 2024, 16, e70479. [Google Scholar] [CrossRef]
- Mortellaro, C.; Garagiola, U.; Lucchina, A.G.; Grivetto, F.; Milone, G.; Pappalardo, S.; Sammartino, G. The use of silicon elastomer in maxillofacial rehabilitation as a substitute for or in conjunction with resins. J. Craniofac. Surg. 2006, 17, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Aboseada, N.I.; Mohamed, F.S.; El-Shabrawy, S.M. Retention of implant retained obturator using two implant placement configurations for maxillectomy cases: In-vitro study. BMC Oral Health 2024, 24, 1059. [Google Scholar] [CrossRef]
- Kapetanakos, M.; Golden, M.; Huryn, J.M. Rehabilitation of a patient after a total maxillectomy with a 2-piece magnetically retained obturator: A clinical report. J. Prosthet. Dent. 2020, 123, 184–187. [Google Scholar] [CrossRef]
- Parameswari, B.D.; Rajakumar, M.; Jagadesaan, N.; Annapoorni, H. Case presentation of two maxillectomy patients restored with two-piece hollow bulb obturator retained using two different types of magnets. J. Pharm. Bioallied Sci. 2017, 9 (Suppl. S1), S252–S256. [Google Scholar] [CrossRef] [PubMed]
- Shetty, P.P.; Chowdhary, R.; Shetty, P.P. A maxillofacial prosthetic obturator using precision attachments. Indian J. Dent. Res. 2020, 31, 799–802. [Google Scholar] [CrossRef]
- Ahmed, B. Rehabilitation of surgically resected soft palate with interim velopharyngeal obturator. Int. J. Oral Craniofac. Sci. 2015, 1, 31–33. [Google Scholar] [CrossRef]
- Kulkarni, P.R.; Kulkarni, R.S.; Shah, R.J.; Maru, K. Prosthetic Rehabilitation of a Partially Edentulous Patient with Maxillary Acquired Defect by a Two-Piece Hollow Bulb Obturator (Using a Dentogenic Concept). J. Coll. Physicians Surg. Pak. 2017, 27, 514–516. [Google Scholar] [PubMed]
- Kumar, P.; Jain, V.; Thakar, A.; Aggarwal, V. Effect of varying bulb height on articulation and nasalance in maxillectomy patients with hollow bulb obturator. J. Prosthodont. Res. 2013, 57, 200–205. [Google Scholar] [CrossRef]
- Ooms, A. Optimized and User-Friendly Workflow for the Fabrication of 3D Printed Maxillary Hollow Closed Surface Model Obturator Using CT, Intraoral Scanning Technology, and Computer Aided/Manufacturing. Master’s Thesis, University of Twente, Enschede, The Netherlands, 2022. Available online: https://purl.utwente.nl/essays/93279 (accessed on 15 July 2025).
- Nimonkar, S.V.; Belkhode, V.M.; Asiri, A.M.; Aldossary, M.F.; Nimonkar, P.V. A method of hollowing the obturator prosthesis and an overview on the pros and cons of the various materials used for hollowing. J. Med. Life 2021, 14, 383–389. [Google Scholar] [CrossRef]
- Molinero-Mourelle, P.; Helm, A.; Cobo-Vázquez, C.; Lam, W.Y.; Azevedo, L.; Pow, E.H.; Gómez-Polo, M. Treatment Outcomes of Implant-Supported Maxillary Obturator Prostheses in Patients with Maxillary Defects: A Systematic Review. Int. J. Prosthodont. 2020, 33, 429–440. [Google Scholar] [CrossRef]
- Dos Santos, D.M.; de Caxias, F.P.; Bitencourt, S.B.; Turcio, K.H.; Pesqueira, A.A.; Goiato, M.C. Oral rehabilitation of patients after maxillectomy. A systematic review. Br. J. Oral Maxillofac. Surg. 2018, 56, 256–266. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).