Abstract
Background: Dental implants have become integral in restoring partially or completely edentulous patients due to their reported long-term success. While titanium remains the primary material for implants and abutments due to its mechanical properties and biocompatibility, zirconia has emerged as a promising alternative, especially for aesthetic regions. This systematic review aimed to assess whether zirconia abutments present a rational alternative to titanium in modern implantology, focusing on their mechanical and clinical performances. Method: The workflow used for this review included the PRISMA checklist. The eligibility criteria included various study types, with a preference given to clinical trials. The search strategy employed the PICO model, including a large number of relevant studies, and online research was carried on the online databases PubMed and Scopus, with “implant” AND “abutment” AND “zirconia” and “zirconia abutment” AND “mechanical properties” used as search strings. Results: Six clinical studies were included with an adequate follow-up and patient cohort; they suggest that while zirconia abutments offer improved aesthetics and biological integration, concerns persist regarding their mechanical properties, particularly regarding their fatigue resistance and connection stability. In vitro studies have revealed differences between titanium and zirconia abutments, with the latter showing greater susceptibility to fatigue-induced deformation and fretting wear. The clinical outcomes, however, demonstrate favourable long-term performance, with zirconia abutments promoting healthy soft tissue conditions. CAD/CAM technologies enable the precise customization of zirconia abutments, enhancing their compatibility and aesthetic outcomes. Conclusions: Although this review faces limitations due to the scarcity of comparative studies and varied methodologies, it underscores the potential of zirconia abutments in implantology. In conclusion, while zirconia abutments offer promising advantages, the careful consideration of patient-specific factors and the long-term outcomes is warranted for their optimal utilisation in implant-supported prostheses.
1. Introduction
Dental implants are considered the therapy of choice for restoring partially or fully edentulous patients because of their reported long-term survival and success [1]. A number of long-term retrospective cohort studies have investigated the relationships between focal factors that may influence implant survival. Attention must be paid to the definition of survival, which means that the implants are still present in the patient’s mouth without biological and/or technical complications and does not necessarily reflect successful treatment [2].
An implant-borne prosthesis consists of a dental implant and an abutment, with retention achieved using a screw, cement or conometric connection [3,4]. Most implants and abutments are now fabricated from commercially pure titanium or titanium alloys due to their superior mechanical properties, biocompatibility and corrosion resistance [5]. More recently, high-strength ceramics such as zirconia have emerged as successful alternatives for aesthetically demanding regions [6].
After an initial focus on clinical success, significant efforts have been made to improve specific aspects of implantology, including aesthetics. In the early 2000s, zirconia abutments were introduced into clinical practice (Figure 1 and Figure 2). Aesthetics was the primum movens, but mechanics remained a challenging issue. Both titanium and zirconia have been shown to cause a lower inflammatory response than other materials, such as gold–platinum alloys [7,8]. In addition, in vitro mechanical studies have shown that aesthetic improvements in the materials do not compromise their structural strength [9,10]. Today, titanium abutments are the most widely used solution for implant rehabilitation due to the high success rate reported in several clinical studies [11,12,13,14].

Figure 1.
Nobel Biocare ProceraTM Abutment Zirconia TM.

Figure 2.
Standard titanium abutment after custom fabrication.
Key clinical goals include the integration of the soft tissue margin with prosthetic crowns and the stability of the transmucosal tunnel with a long epithelial attachment. One of the most critical factors influencing the long-term success of an implant-supported prosthesis is the interface between the restoration and the fixture. The transmucosal passage plays a fundamental role in determining the clinical outcome by directly influencing key aspects such as inflammation control, bone resorption and the overall aesthetic appearance. In cases where high aesthetic standards are required, one of the most common yet undesirable effect is the appearance of grey shadows caused by transparent soft tissue over titanium abutments. These shadows can compromise the natural appearance of the restoration and negatively affect patient satisfaction. To overcome this problem, the careful planning of the implant positioning is essential, including its depth, inclination and orientation within the vestibular–palatal space. In addition, optimising the emergence profile of the abutment is critical to ensure a seamless transition between the implant and the surrounding tissues. An effective strategy to further improve the aesthetic results is the use of zirconia abutments instead of titanium. The white colour of zirconia offers a significant advantage by reducing the visibility of grey shadows and contributing to the more natural appearance of the peri-implant soft tissue [15,16].
While achieving optimal aesthetics is essential in implant-borne restorations, it should never be at the expense of biological integration and long-term tissue health. Successful rehabilitation must balance both functional and aesthetic considerations while ensuring adequate biocompatibility. Fortunately, zirconia has demonstrated excellent biocompatibility and minimal interactions with the surrounding tissues. Research has shown that cellular responses to zirconia surfaces are comparable to those observed with titanium, reinforcing its viability as an alternative abutment material. Both titanium and zirconia abutments have been shown to support stable and long-lasting epithelial attachment, a critical aspect of maintaining peri-implant tissue health [11]. This biological response plays a fundamental role in the overall success of implant rehabilitation and is commonly referred to as biological sealing. The ability of an abutment material to promote secure epithelial attachment contributes significantly to the prevention of bacterial infiltration, inflammation and subsequent bone loss. As a result, the favourable biological properties of zirconia, combined with its aesthetic advantages, make it an increasingly valuable option for achieving both functional stability and superior aesthetic outcomes in implant dentistry [15,17].
In addition to aesthetics and biological interactions, the mechanical properties of the material should be thoroughly investigated [18]. The clinical reliability of zirconia as a restorative material has been extensively documented, particularly in the fabrication of crowns, where it has demonstrated excellent long-term performance. Its success is largely due to its excellent mechanical properties, including its high flexural strength and fracture toughness, which make it a durable and resilient option for dental restorations. One of the most critical aspects to consider when evaluating the functional longevity of any dental material is its resistance to cyclic fatigue, as restorations are subjected to continuous occlusal forces, thermal variations and biomechanical stresses within the oral environment. Zirconia, with its high fatigue resistance, is particularly well suited to these demanding conditions, ensuring long-term stability and reliability in both anterior and posterior restorations. In addition, its ability to withstand high masticatory forces without significant wear or fracturing supports its widespread use in modern dentistry. Understanding the mechanical behaviour of zirconia in response to these forces is essential in predicting its long-term success, particularly when extending its use beyond single-unit crowns to more complex restorations such as multi-unit bridges and implant-borne restorations [19,20]. In vitro tests have demonstrated this characteristic of zirconia abutments, and clinical studies in the literature demonstrate the long-term outcomes of this type of rehabilitation [21,22].
Figure 2 and Figure 3 show the difference between a standard screw abutment with an internal connection and platform switch concept and a new zirconia abutment. In this case they were milled by a technician and cemented to a connector extra-orally. This was a two-piece abutment with a metal adapter, so the abutment–implant interfaces were titanium versus titanium.
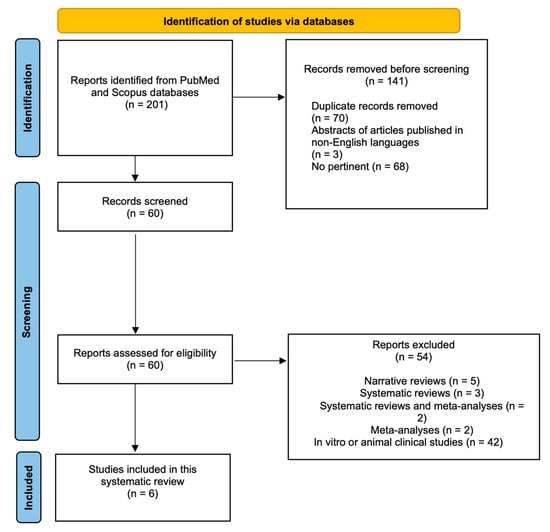
Figure 3.
Inclusion flow chart.
Real clinical indications are not yet available in the literature. Several studies have been designed using different technologies, materials and follow-ups, but only a few articles discuss modern technology applied to this research field with real clinical speculation.
The scope of this systematic review was to investigate whether zirconia abutments are a possible and rational alternative to titanium abutments in modern implantology.
2. Materials and Methods
The PRISMA checklist was followed during the design and writing of this review, and the checklist used is included in the Supplementary Materials (Table S1).
2.1. Focused Questions
- How are the clinical performances and outcomes of zirconia abutments?
- What are the advantages of the application of zirconia abutments?
2.2. Eligibility Criteria
The following inclusion criteria were used in the analysis of the studies:
- Types of studies: Randomised clinical trials, case–control studies, cross-sectional studies, and cohort studies.
- Types of participants: Studies concerning patients with zirconia abutments for implant rehabilitations; only clinical studies were included in this review.
- Types of interventions: The comparison of the clinical performances of zirconia abutments. An assessment of these performances has been made through the performance of case–control, cross-sectional, cohort and clinical RCT studies.
- Outcome types: The identification of the advantages of using zirconia abutments for clinical use.
Only studies that met all the inclusion criteria were included.
However, the following exclusion criteria were considered:
- Articles published in non-English languages;
- Studies where non-zirconia abutments were tested;
- Animal or in vitro studies;
- An absence of ethics committee approval.
2.3. Search Strategy
The PICO (Population, Intervention, Comparison and Outcome) model was used to write this review: “How do zirconia Performs in terms of mechanical properties, esthetic outcomes, and overall clinical success in patients receiving dental implants”?
A literature search was conducted using the electronic databases PubMed (MEDLINE) and Scopus. The abstracts of studies that compared the clinical reliability of zirconia abutments with that of titanium abutments were included in this review.
2.4. Research
The search was performed using the following MESh terms: “implant”, “abutment”, “zirconium oxide”, “zirconium oxide abutment”, and “mechanical properties”; the search terms are shown in Table 1. Only original publications written in English were included in this review. The research time horizon included papers published from 2008 to the present.

Table 1.
Search strings and MEsH terms used on Pubmed and Scopus Databases.
2.5. Data Collection
The data was collected by a single operator without the use of automated tools.
The data results were compared qualitatively; statistical analysis was not performed due to the nature of the results.
The results of the research, with key findings such as the number of patients involved, the type of intervention, complications and follow-ups, have been summarised and included in Table 2. Missing data were not extrapolated. No subgroup analysis was performed with regard to heterogeneity.

Table 2.
Main outcome summary.
Table 2.
Main outcome summary.
| Number of Patients | Number of Implants | Main Outcome | Follow-Up | Study Type | Study Reference | Setting |
|---|---|---|---|---|---|---|
| 123 | 291 | One abutment fracture. Abutment survival rate of 99.66%. | 4 yy | Retrospective cohort study | Parpaiola et al., 2020 [8] | Multicentric: five in Italy and one in England |
| 20 | 40 | Canine, premolar and molar were replaced, half with zirconia abutments and half with Ti ones. No complications during duration of observation (too short), but zirconia, like all ceramics, aged faster than metal. | 3 yy | Randomised controlled trial | Zembic et al., 2009 [14] | University of Zurich (Switzerland) |
| 141 | 158 | Comparison between standard and switching platform for zirconia abutments. No difference between two systems in terms of fracture patterns; difference was found between internal and external hexagon. Survival and success rate of 93,8% and 81,2% (12 yy fu) for standard and 90% and 84% (5 yy fu) for platform switching. | 12 yy | Retrospective study | Passos et al., 2016 [16] | University of British Columbia (Canada) |
| 24 | 42 | No abutment fractures (4 veneering chips). | 1 y | Retrospective study | Nothdurft et al., 2010 [23] | Saarland University (Germany) |
| 56 | 89 | Internal hexagon, comparison of three different groups: titanium, titanium nitride and zirconia abutments. Total of 5 fractures in zirconia group at connection level (4 in posterior region and 1 during clinical phase), none in titanium group. In all failed restorations, fractures in abutment connection were evident at stem level. | 3 yy | Randomised controlled trial | Ferrari et al., 2016 [24] | Department of Prostho- dontics of the University of Siena (Italy) |
| 32 | 49 | 32 patients at T0, 24 patients and 39 implants at T1. Two-piece implant, cemented abutment. Two fracture lines were observed in two different patients, and 6 abutments (in six patients) fractured at connection level (2 after 4 yy, 1 after 5 yy and 3 after 6 yy). Six crown–abutment complexes lost retention. Cumulative rate of survival of 83% over 6 yy. | 6 yy | Cohort prospective study | Cionca et al., 2021 [25] | University Hospitals of Geneva, Geneva, Switzerland |
3. Results
The use of zirconia abutments has made it easier for clinicians to approach aesthetic rehabilitation with dental implants, but since their introduction their mechanical properties have been a challenging area. Although some doubts remain, their clinical performance over time appears to be favourable compared to that of standard abutments. This type of abutment may allow clinicians to improve aesthetics and biological integration with healthy soft tissue.
3.1. Search Outcome
The search string yielded 201 titles (183 Scopus and 18 Pub-Med/MEDLINE). After screening the titles and abstracts, only 60 studies qualified for the next stage of the review. However, as only clinical trials were eligible, only six papers were finally included. The selection process is shown in Figure 3. The clinical studies could be categorised into different types; the results could be grouped (Table 2) into retrospective studies (16%), prospective studies (32%), case and series reports (16%), cohort studies (10%) and RCT studies (16%)
3.2. Risk of Bias
The risk of bias of the main articles reviewed is shown in Table 3. Considering the results, this review has a moderate risk of bias. The articles included did not have a blind structure, except for Ferrari’s paper; the sequence and allocation were not adequate in more than half of the papers reviewed. Ferrari’s paper respected all the parameters assessed and showed a lower risk of bias. All the articles had complete outcome data [26,27].

Table 3.
Risk of bias. The coloured circles indicate the level of risk: red (high risk) and green (low risk).
4. Discussion
Zirconia was discovered in 1892. The first paper on the use of zirconia in the medical field was written in 1969, while the first introduction of zirconia to the dental market was in 2001 [28,29]. Since 2006, zirconia has been used for dental implant abutments. Zirconia is a ceramic material well known for its strength, biocompatibility and aesthetics.
The introduction of zirconia abutments into clinical implant management offers several advantages: Aesthetically, they improve the rehabilitation of the anterior region, where traditional abutments can cause undesirable mucosal discolouration [20,30,31]. The biological interactions are also crucial when discussing zirconia abutments [32], along with their mechanical properties. In terms of the biological implications, zirconia is considered to be a highly biocompatible substrate, allowing for long epithelial attachment with this type of material; the connective structure also has a good interaction with zirconia [33]. Zirconia abutments can provide excellent aesthetic results, particularly where the natural appearance of the gingival tissue is important. Digital workflows allow for the creation of zirconia abutments that closely mimic the appearance of natural teeth, improving the overall aesthetic outcome of the restoration. Healthy soft tissue conditions can improve the emergence profile of the crowns, enhancing the aesthetics.
However, clinicians must carefully evaluate the thickness of zirconia abutments in relation to the emergence profile and the potential risk of mucosal dehiscence and soft tissue recession. While zirconia offers aesthetic advantages due to its white colour, a thicker abutment wall may be required to ensure adequate strength, which may present mechanical challenges, especially in cases with limited space. In contrast, titanium abutments can maintain structural integrity with thinner residual walls, making them a more mechanically favourable option in high-stress areas. On the other hand, the favourable colour of zirconia compared to that of titanium allows for a more pronounced and naturally integrated emergence profile without the risk of grey shadows showing through the soft tissue. This enhanced emergence profile plays a critical role in the transition between the internal connective tissue and the epithelial layer, contributing to improved tissue adaptation and aesthetic results. A well-designed zirconia abutment with an optimal thickness can help achieve both mechanical reliability and soft tissue stability, ultimately improving the long-term success of the implant restoration. Therefore, the choice between zirconia and titanium abutments should be guided by a balance between mechanical durability, biological integration and aesthetic requirements, tailored to the specific needs of each patient. The absence of undesirable colour translucency could provide room for a stronger support structure [13]. The relationship between zirconia abutments and their effect on the long epithelial attachment (also known as the biologic width) is an important consideration in implantology and periodontology; the biologic width is a term used to describe the space occupied by the junctional epithelium and connective tissue fibres around a tooth or dental implant abutment [34]. Zirconia is generally considered to be a biocompatible material, meaning that it is well tolerated by the surrounding oral tissues and allows for the formation of a long epithelial attachment [35]. Zirconia abutments can promote healthy soft tissue conditions due to their biocompatibility, smooth surface and minimal plaque retention [36,37]. Healthy soft tissue is essential for long-term implant success and is a prerequisite for good mucosal sealing [38]. The correct design and contours of standard zirconia abutments are also essential to support healthy soft tissue attachment [15].
In terms of mechanical properties, regarding the occlusal load, zirconia differs from metals such as titanium [39,40]: in fact, due to its inherently brittle nature, this ceramic can be susceptible to large tensile forces with low residual elasticity [41]. These implications lead us to a specific evaluation of the thickness of the abutment during milling and personalisation [33]. From a biomechanical point of view, the characteristics of zirconia are influenced by the stabilising element; using yttrium (Y), ytterbium (Yb), niobium (Nb) and tantalum (Ta) oxide as stabilisers could increase the fracture toughness [42].
In vitro tests have shown that titanium and zirconia behave differently at the junction level, with zirconia abutments showing more deformation and fretting wear after fatigue cycles than Ti abutments [43]. The connection is one of the most important parts of the system; considering the interface, perfect sealing is guaranteed by the lifelong stability of the connection between the osteointegrated part and the restoration.
The analysis of different abutment-to-implant connection materials is important to achieve a stable abutment connection (IAC), which is a key factor for long-term clinical success from both biological and mechanical points of view [9,33]. The fracture rate seems to be influenced by the design of the internal or external connection [16]. Two other studies reported fractures at the junction level and showed how the junction interfaces in zirconia abutments could be improved [24,25]. Fractures at the junction level appear to be a weakness of this abutment type, so a change in the design of the junction platform could improve its performance and fatigue strength [25].
In terms of clinical mechanical performance, zirconia abutments have shown limitations in their fatigue strength. Ferrari et al. (2016) [24] and Cionca et al. (2021) [25] reported fractures at the connection level, particularly in the posterior region, highlighting concerns regarding the long-term mechanical stability. Ferrari’s work demonstrated that fracture lines were visible at the STEM level in the connection portion at a 3-year follow-up. Cionca et al. calculated a survival rate of 83% during their 6-year study, finding two fracture lines and six fractures at the connection level in 49 implants. In contrast, titanium abutments showed superior resistance to mechanical stress, as demonstrated by Parpaiola et al. (2020) [8], where only one fracture occurred during four years of follow-ups. Passos et al. (2016) [16], with a study based on 12 years of follow-ups and involving 158 implants, observed no significant difference in the fracture patterns between standard and switching platforms, but internal and external hexagonal connections influenced the survival rates. On the other hand, the concept of platform switching was confirmed to promote peri-implant tissue health.
For aesthetic results, zirconia abutments significantly improved the soft tissue colour and reduced the visibility of metal shadows. Zembic et al. (2009) [14] emphasised the importance of zirconia in highly aesthetic areas. However, its long-term aesthetic stability remains a concern due to age-related wear.
It must be considered that a key factor is clinical longevity; studies such as those by Nothdurft et al. (2010) [23] and Parpaiola et al. (2020) [8] reported high survival rates for zirconia abutments, but retention issues were noted in a study by Cionca et al. (2021) [25] where six crown–abutment complexes lost retention. Passos et al. (2016) [16] confirmed comparable survival rates between zirconia and titanium abutments, further supporting their clinical viability.
From a biological point of view, Zembic et al. (2009) [14] demonstrated that periodontal parameters (PPD, BoP, BL) are related to the peri-implant health status and are similar to those of titanium. Similar biological results were reported in the Cionca study, where the probing pocket depth (PPD) remained within the physiologic range at six years without significant variation since loading. The Modified Bleeding Index (mBI) results were consistent with mucosal health, while radiographic measurements taken throughout the study indicated stable bone levels. Nothdurft also analysed the bone levels and found no significant changes over time. In addition, mBI values indicated healthy conditions in approximately 85% of cases, suggesting stable and non-inflammatory peri implant conditions in both hard and soft tissues. Parpaiola et al. confirmed previous findings, reporting a mean PPD of 2.75 mm and no statistically significant differences between groups for both PPD and BoP measurements. Passos’s group evaluated the BoP and gingival recession to assess the mucosal stability and health. Of the 158 cases analysed, 153 showed less than 1 mm of recession and 143 were BoP-negative. In terms of the periodontal parameters, no statistically significant differences in the BoP measurements were observed. However, a trend towards increased inflammation was observed in the standard platform group, with 12.7% BoP-positive cases (9/71) compared to 6.9% (6/87) in the platform switching group.
From a clinical point of view, all the studies included in this review showed encouraging results over a long follow-up period, reinforcing the potential of this type of abutment in implant-borne restorations. The results suggest that these abutments, when used under the appropriate conditions, could be successfully integrated into routine clinical practice, providing both functional stability and aesthetic benefits. However, their long-term success depends on strict adherence to proper indications and careful case selection. Each patient presents unique anatomical, biomechanical and aesthetic considerations, making a thorough preoperative assessment essential. Factors such as the bone quality, soft tissue characteristics, occlusal dynamics and prosthetic design must be carefully analysed to ensure that the chosen abutment material provides optimal support and durability. The clinician must also consider the interactions between the abutment and the surrounding tissues to minimise complications such as peri-implant inflammation or mechanical failure. By carefully evaluating each case and tailoring treatment accordingly, the incorporation of these abutments into clinical practice can contribute to improved patient outcomes and long-term prosthetic success.
Zirconia abutments are well suited to digital workflows and CAD/CAM technologies, which allow for precise design, fabrication and customisation to meet patient-specific anatomy and aesthetic requirements [44,45]. Their use ensures a proper fit with implants and restorations, while supporting an ideal emergence profile that promotes epithelial attachment and soft tissue health. However, the success of zirconia abutments in CAD/CAM workflows depends on proper training and expertise in this technology [46].
The studies included in this review showed considerable variation in the study designs and clinical approaches. In addition, they were published over a long period of time, reflecting the use of different products and methodologies that have evolved over time. This variability adds a degree of complexity to the comparative analysis of the results and is one of the main limitations of this review. Another important consideration is the relatively small number of articles included in this review. Although the studies were selected based on strict inclusion criteria, the limited sample size may affect the generalizability of the findings. Despite the small number of included studies, it is worth noting that they included large patient cohorts, and some had long follow-up periods. This is a major strength, as it allows not only the short-term clinical results to be assessed but also the long-term stability and performance of the analysed abutments. However, another limitation of this review is the high risk of bias present in some of the included studies. The potential for bias arises from several factors, such as the study design, sample size, patient selection criteria and data collection and analysis methods. Given these considerations, future research in this area should aim to adopt a more standardised and rigorous methodology to minimise the risk of bias and increase the reliability of the findings. Ideally, future studies should include a larger cohort of patients and follow more structured protocols with standardised selection and assessment criteria. This would provide more robust and comparable data, ultimately leading to clearer clinical guidelines on the use of zirconia abutments compared with titanium abutments.
5. Conclusions
Zirconia abutments may be considered for use in implant-supported prostheses due to their mechanical fatigue resistance. However, their use should be carefully evaluated and recommended only in cases where the clinical indications are appropriate. The aesthetic outcome could benefit from the colour of the abutment structure, particularly in thin soft tissue phenotypes, thus mitigating the grey translucency of titanium abutments. The use of zirconia abutments appears to create good conditions for host cell and tissue integration with a long epithelial attachment; at the same time, zirconia surfaces have excellent hygienic properties that contribute to the maintenance of peri-implant health. In conclusion, zirconia abutments are a feasible clinical option in implant-supported prostheses. Further high-quality clinical studies are required to fully validate the routine use of these abutments.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/prosthesis7050113/s1, Table S1. PRISMA 2020 checklist.
Author Contributions
Conceptualization, A.S. and D.D.M.; methodology, A.S.; software, D.D.M.; validation, M.M., F.V. and A.S.; formal analysis, A.S.; investigation, D.D.M.; resources, A.S.; data curation, D.D.M.; writing—original draft preparation, D.D.M.; writing—review and editing, D.D.M., A.S. and F.V.; visualisation, M.M.; supervision, D.S. and P.Z.; project administration, A.S. and D.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data supporting the results of the research are presented within the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Sanz-Martín, I.; Sanz-Sánchez, I.; Carrillo de Albornoz, A.; Figuero, E.; Sanz, M. Effects of Modified Abutment Characteristics on Peri-implant Soft Tissue Health: A Systematic Review and Meta-analysis. Clin. Oral Implants Res. 2018, 29, 118–129. [Google Scholar] [CrossRef]
- Daneshvar, S.; Matthews, D.; Michuad, P.-L.; Ghiabi, E. Success and Survival Rates of Dental Implants Restored at an Undergraduate Dental Clinic: A 13-Year Retrospective Study with a Mean Follow-up of 5.8 Years. Int. J. Oral Maxillofac. Implants 2016, 31, 870–875. [Google Scholar] [CrossRef]
- Goto, T. Osseointegration and Dental Implants; John Wiley & Sons: Hoboken, NJ, USA, 2014; Volume 24, ISBN 9780813813417. [Google Scholar]
- Lupi, S.M.; Todaro, C.; De Martis, D.; Blasi, P.; Rodriguez y Baena, R.; Storelli, S. The Conometric Connection for the Implant-Supported Fixed Prosthesis: A Narrative Review. Prosthesis 2022, 4, 458–467. [Google Scholar] [CrossRef]
- Simonis, P.; Dufour, T.; Tenenbaum, H. Long-term Implant Survival and Success: A 10–16-year Follow-up of Non-submerged Dental Implants. Clin. Oral Implants Res. 2010, 21, 772–777. [Google Scholar] [CrossRef]
- de Almeida Basílio, M.; Cardoso, K.V.; Antonio, S.G.; Rizkalla, A.S.; Santos Junior, G.C.; Arioli Filho, J.N. Effects of Artificial Aging Conditions on Yttria-Stabilized Zirconia Implant Abutments. J. Prosthet. Dent. 2016, 116, 277–285. [Google Scholar] [CrossRef]
- Tischler, M. The Future of Implant Dentistry. Dent. Today 2016, 35, 84–85. [Google Scholar]
- Parpaiola, A.; Toia, M.; Norton, M.; Cecchinato, D.; Bressan, E.; Lops, D. CAD/CAM Implant Abutments: Peri-Implant Hard and Soft Tissue Response with Up to 4 Years of Follow-up—A Retrospective Cohort Study Evaluation. Int. J. Periodontics Restor. Dent. 2020, 40, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Kerstein, R.B.; Radke, J. A Comparison of Fabrication Precision and Mechanical Reliability of 2 Zirconia Implant Abutments. Int. J. Oral Maxillofac. Implants 2008, 23, 1029–1036. [Google Scholar]
- Vozzo, L.M.; Azevedo, L.; Fernandes, J.C.H.; Fonseca, P.; Araújo, F.; Teixeira, W.; Fernandes, G.V.O.; Correia, A. The Success and Complications of Complete-Arch Implant-Supported Fixed Monolithic Zirconia Restorations: A Systematic Review. Prosthesis 2023, 5, 425–436. [Google Scholar] [CrossRef]
- Sordi, M.B.; Sarwer-Foner, S.N.D.; Schünemann, F.H.; Apaza-Bedoya, K.; Juanito, G.M.P.; Henriques, B.; Henriques, B.; Magini, R.S.; Benfatti, C.A.M. Biological Behavior of Titanium, Zirconia or PEEK Dental Implant-Abutments. In Biodental Engineering V; CRC Press: London, UK; Taylor & Francis Group: Boca Raton, FL, USA, 2019; pp. 31–42. [Google Scholar]
- Foong, J.K.W.; Judge, R.B.; Palamara, J.E.; Swain, M.V. Fracture Resistance of Titanium and Zirconia Abutments: An in Vitro Study. J. Prosthet. Dent. 2013, 109, 304–312. [Google Scholar] [CrossRef]
- Halim, F.C.; Pesce, P.; De Angelis, N.; Benedicenti, S.; Menini, M. Comparison of the Clinical Outcomes of Titanium and Zirconia Implant Abutments: A Systematic Review of Systematic Reviews. J. Clin. Med. 2022, 11, 5052. [Google Scholar] [CrossRef]
- Zembic, A.; Sailer, I.; Jung, R.E.; Hämmerle, C.H.F. Randomized-Controlled Clinical Trial of Customized Zirconia and Titanium Implant Abutments for Single-Tooth Implants in Canine and Posterior Regions: 3-Year Results. Clin. Oral Implants Res. 2009, 20, 802–808. [Google Scholar] [CrossRef]
- Vazouras, K.; Margvelashvili-malament, M.; Kim, Y.J.; Weber, H.; Finkelman, M. An Esthetic Evaluation of Different Abutment Materials in the Anterior Maxilla: A Randomized Controlled Clinical Trial. J. Prosthodont. 2022, 31, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Passos, S.P.; Linke, B.; Larjava, H.; French, D. Performance of Zirconia Abutments for Implant-Supported Single-Tooth Crowns in Esthetic Areas: A Retrospective Study up to 12-Year Follow-Up. Clin. Oral Implants Res. 2016, 27, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Alkahtany, M.; Beatty, M.W.; Alsalleeh, F.; Petro, T.M.; Simetich, B.; Zhou, Y.; Feely, D.; Polyzois, G. Color Stability, Physical Properties and Antifungal Effects of ZrO2 Additions to Experimental Maxillofacial Silicones: Comparisons with TiO2. Prosthesis 2023, 5, 916–938. [Google Scholar] [CrossRef]
- Mavriqi, L.; Traini, T. Mechanical Properties of Translucent Zirconia: An In Vitro Study. Prosthesis 2023, 5, 48–59. [Google Scholar] [CrossRef]
- Sorrentino, R.; Ruggiero, G.; Toska, E.; Leone, R.; Zarone, F. Clinical Evaluation of Cement-Retained Implant-Supported CAD/CAM Monolithic Zirconia Single Crowns in Posterior Areas: Results of a 6-Year Prospective Clinical Study. Prosthesis 2022, 4, 383–393. [Google Scholar] [CrossRef]
- Barile, G.; Capodiferro, S.; De Rosa, G.; Muci, G.; Vanzanelli, A.; Corsalini, M. Screwed Monolithic Zirconia Crowns for Mono-Implant Posterior Rehabilitation: A Prospective Clinical Study on 41 Patients with a 7-Year Follow-Up. Prosthesis 2023, 5, 1037–1048. [Google Scholar] [CrossRef]
- Di Alberti, L.; Di Alberti, C.; Donini, F.; Lo Muzio, L.; Cadrobbi, F.; D’Agostino, A.; De Santis, D.; Bertossi, D. Clinical and Mechanical Evaluation of Screw-Retained Implant-Supported Zirconia Restorations. A 36 Months Prospective Clinical Study. Minerva Stomatol. 2018, 62, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Schnider, N.; Forrer, F.; Brägger, U.; Hicklin, S. Clinical Performance of One-Piece, Screw-Retained Implant Crowns Based on Hand-Veneered CAD/CAM Zirconia Abutments After a Mean Follow-up Period of 2.3 Years. Int. J. Oral Maxillofac. Implants 2018, 33, 188–196. [Google Scholar] [CrossRef]
- Nothdurft, F.; Pospiech, P. Prefabricated zirconium dioxide implant abutments for single-tooth replacement in the posterior region: Evaluation of peri-implant tissues and superstructures after 12 months of function. Clin. Oral Implant. Res. 2010, 21, 857–865. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Tricarico, M.G.; Cagidiaco, M.C.; Vichi, A.; Gherlone, E.F.; Zarone, F.; Sorrentino, R. 3-Year Randomized Controlled Prospective Clinical Trial on Different CAD-CAM Implant Abutments. Clin. Implant Dent. Relat. Res. 2016, 18, 1134–1141. [Google Scholar] [CrossRef] [PubMed]
- Cionca, N.; Hashim, D.; Mombelli, A. Two-piece Zirconia Implants Supporting All-Ceramic Crowns: Six-year Results of a Prospective Cohort Study. Clin. Oral Implants Res. 2021, 32, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, S.; Kloukos, D.; Petridis, H.; Pandis, N. An Assessment of the Risk of Bias in Randomized Controlled Trial Reports Published in Prosthodontic and Implant Dentistry Journals. Int. J. Prosthodont. 2015, 28, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Sheth, V.H.; Shah, N.P.; Jain, R.; Bhanushali, N.; Bhatnagar, V. Development and Validation of a Risk-of-Bias Tool for Assessing in Vitro Studies Conducted in Dentistry: The QUIN. J. Prosthet. Dent. 2024, 131, 1038–1042. [Google Scholar] [CrossRef]
- Hanawa, T. Zirconia versus Titanium in Dentistry: A Review. Dent. Mater. J. 2020, 39, 24–36. [Google Scholar] [CrossRef]
- Sadowsky, S.J. Has Zirconia Made a Material Difference in Implant Prosthodontics? A Review. Dent. Mater. 2020, 36, 1–8. [Google Scholar] [CrossRef]
- Jung, R.E.; Holderegger, C.; Sailer, I.; Khraisat, A.; Suter, A.; Hämmerle, C.H.F. The Effect of All-Ceramic and Porcelain-Fused-to-Metal Restorations on Marginal Peri-Implant Soft Tissue Color: A Randomized Controlled Clinical Trial. Int. J. Periodontics Restor. Dent. 2008, 28, 357–365. [Google Scholar]
- Jung, R.E.; Sailer, I.; Hämmerle, C.H.F.; Attin, T.; Schmidlin, P. In Vitro Color Changes of Soft Tissues Caused by Restorative Materials. Int. J. Periodontics Restor. Dent. 2007, 27, 251. [Google Scholar]
- Denry, I.; Kelly, J.R. State of the Art of Zirconia for Dental Applications. Dent. Mater. 2008, 24, 299–307. [Google Scholar] [CrossRef]
- Yüzügüllü, B.; Avci, M. The Implant-Abutment Interface of Alumina and Zirconia Abutments. Clin. Implant Dent. Relat. Res. 2008, 10, 113–121. [Google Scholar] [CrossRef]
- Derks, J.; Tomasi, C. Peri-Implant Health and Disease. A Systematic Review of Current Epidemiology. J. Clin. Periodontol. 2015, 42, S158–S171. [Google Scholar] [CrossRef]
- Nakamura, K.; Kanno, T.; Milleding, P.; Ortengren, U. Zirconia as a Dental Implant Abutment Material: A Systematic Review. Int. J. Prosthodont. 2010, 23, 299–309. [Google Scholar]
- Zhang, Y.; Lawn, B.R. Evaluating Dental Zirconia. Dent. Mater. 2019, 35, 15–23. [Google Scholar] [CrossRef]
- Remísio, M.; Borges, T.; Castro, F.; Gehrke, S.; Fernandes, J.; Fernandes, G. Histologic Osseointegration Level Comparing Titanium and Zirconia Dental Implants: Meta-Analysis of Preclinical Studies. Int. J. Oral Maxillofac. Implants 2023, 38, 667–680. [Google Scholar] [CrossRef] [PubMed]
- Lindhe, J.; Meyle, J. Peri-Implant Diseases: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 282–285. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.Q.; Tan, K.B.; Nicholls, J.I. Load Fatigue Performance of Implant-Ceramic Abutment Combinations. Int. J. Oral Maxillofac. Implants 2009, 24, 636–646. [Google Scholar]
- Freifrau von Maltzahn, N.; Bernard, S.; Kohorst, P. Two-part Implant Abutments with Titanium and Ceramic Components: Surface Modification Affects Retention Forces—An In-vitro Study. Clin. Oral Implants Res. 2019, 30, 903–909. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, C.; Bocchieri, S.; Sambataro, S.; Surace, G.; Stumpo, C.; Fiorillo, L. Occlusal Load Considerations in Implant-Supported Fixed Restorations. Prosthesis 2020, 2, 252–265. [Google Scholar] [CrossRef]
- Ban, S.; Yasuoka, Y.; Sugiyama, T.; Matsuura, Y. Translucent and Highly Toughened Zirconia Suitable for Dental Restorations. Prosthesis 2023, 5, 60–72. [Google Scholar] [CrossRef]
- Nam, R.-K.; Lee, S.; Park, E.-J.; Kwon, H.-B.; Yoon, H.-I. Three-Dimensional Deformation and Wear of Internal Implant-Abutment Connection: A Comparative Biomechanical Study Using Titanium and Zirconia. Int. J. Oral Maxillofac. Implants 2018, 33, 1279–1286. [Google Scholar] [CrossRef]
- Yoo, S.-Y.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y.; Park, J.-M.; Chung, S. Comparison of Fit and Stability Between 3D-Printed and Milled Implant Abutments with Titanium-6Al-4V and Co-Cr Metal Alloys. Int. J. Oral Maxillofac. Implants 2023, 38, 1014–1024. [Google Scholar] [CrossRef] [PubMed]
- Gallo, S.; Pascadopoli, M.; Pellegrini, M.; Pulicari, F.; Manfredini, M.; Zampetti, P.; Spadari, F.; Maiorana, C.; Scribante, A. CAD/CAM Abutments versus Stock Abutments: An Update Review. Prosthesis 2022, 4, 468–479. [Google Scholar] [CrossRef]
- Çin, V.; İzgi, A.D.; Kale, E.; Yilmaz, B. Marginal and Internal Fit of Monolithic Zirconia Crowns Fabricated by Using Two Different CAD-CAM Workflows: An In Vitro Study. Prosthesis 2023, 5, 35–47. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).

