Mechanical and Physical Properties of Durable Prosthetic Restorations Printed Using 3D Technology in Comparison with Hybrid Ceramics and Milled Restorations—A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection Criteria
2.2. Exposure and Outcome
2.3. Search Strategy
2.4. Data Extraction Process
2.5. Quality Assessment of Selected Studies
2.6. Quantitative Assessment
3. Results
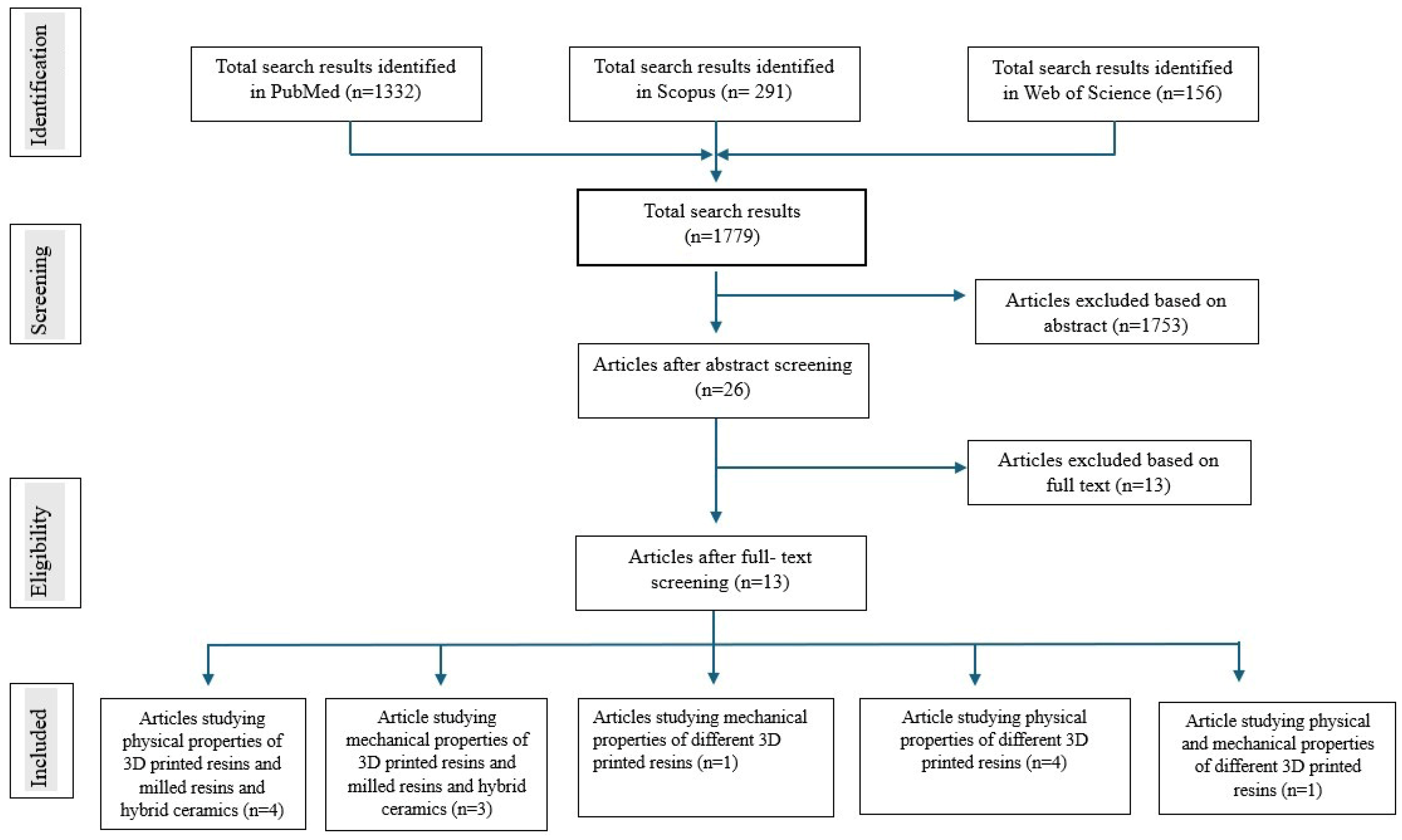
3.1. Findings from the Literature Search
3.2. Features of the Selected Studies
3.3. Assessment of Quality of Selected Studies
3.4. Results from Studies Assessing Physical Properties
3.4.1. Surface Roughness
3.4.2. Color Changes
3.4.3. Water Sorption/Solubility
3.5. Results from Studies Assessing Mechanical Properties
3.5.1. Flexural Strength
3.5.2. Microhardness
3.5.3. Elastic Modulus
4. Discussion
4.1. Physical Properties
4.2. Mechanical Properties
5. Limitations and Future Directions
- All the studies reviewed were in vitro studies, which may not have fully simulated the complex conditions encountered in the oral environment. In vivo studies are crucial for confirming the clinical relevance of these findings.
- It is evident that the composition significantly influences the observed properties and behavior of materials. The materials under study were commercially sourced, and their exact formulations are not publicly disclosed in detail. This necessarily limits the generalizability and reproducibility of the findings.
- The limited number of studies and their relatively short follow-up periods suggest that more long-term research is needed to gain a better understanding of the durability and performance of 3D-printed resins over time.
- Future research should focus on exploring standard surface treatments, material compositions, and printing technologies to enhance the properties of 3D-printed resins further. Additionally, studies that examine the impact of various environmental factors (e.g., exposure to saliva, temperature, and mechanical loading) on the properties of these materials will provide more comprehensive data for their clinical use.
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CAD/CAM | Computer-aided design/computer-aided manufacturing |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta Analyses |
| CONSORT | Consolidated Standards of Reporting Trials |
| SLA | Stereolithography |
| DLP | Digital light processing |
| ISO | International standard organization |
| Ra | Roughness average |
| VHN | Vickers’ hardness number |
| MPa | Mega Pascal |
| MP | Mechanical property |
| PP | Physical property |
| 3D | Three-dimensional |
References
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in Prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [Google Scholar] [CrossRef]
- Temizci, T.; Bozoğulları, H.N. Effect of thermocycling on the mechanical properties of permanent composite-based CAD-CAM restorative materials produced by additive and subtractive manufacturing techniques. BMC Oral Health 2024, 24, 334. [Google Scholar] [CrossRef]
- Nulty, A.B. 3D Printing Part 1—A History and Literature Review Of 3D Printing in Dentistry. Preprints 2021, 2021050221. [Google Scholar] [CrossRef]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Eftekhar Ashtiani, R.; Beyabanaki, E.; Razmgah, M.; Salazar, A.; Revilla-León, M.; Zandinejad, A. Color stability of resin hybrid ceramic materials in comparison to zirconia-reinforced lithium silicate ceramic. Front. Dent. 2023, 20, 37. [Google Scholar] [CrossRef]
- Bozogulları, H.N.; Temizci, T. Evaluation of the Color Stability, Stainability, and Surface Roughness of Permanent Composite-Based Milled and 3D Printed CAD/CAM Restorative Materials after Thermocycling. Appl. Sci. 2023, 13, 11895. [Google Scholar] [CrossRef]
- Park, Y.; Kim, J.; Kang, Y.J.; Shim, E.Y.; Kim, J.H. Comparison of Fracture Strength of Milled and 3D-Printed Crown Materials According to Occlusal Thickness. Materials 2024, 17, 4645. [Google Scholar] [CrossRef]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Mechanical properties and internal fit of 4 CAD-CAM block materials. J. Prosthet. Dent. 2018, 119, 384–389. [Google Scholar] [CrossRef]
- Balestra, D.; Lowther, M.; Goracci, C.; Mandurino, M.; Cortili, S.; Paolone, G.; Louca, C.; Vichi, A. 3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of Literature. Materials 2024, 17, 1380. [Google Scholar] [CrossRef]
- Prause, E.; Malgaj, T.; Kocjan, A.; Beuer, F.; Hey, J.; Jevnikar, P.; Schmidt, F. Mechanical properties of 3D-printed and milled composite resins for definitive restorations: An in vitro comparison of initial strength and fatigue behavior. J. Esthet. Restor. Dent. 2024, 36, 391–401. [Google Scholar] [CrossRef]
- Di Fiore, A.; Stellini, E.; Alageel, O.; Alhotan, A. Comparison of mechanical and surface properties of two 3D printed composite resins for definitive restoration. J. Prosthet. Dent. 2024, 132, 839.e1–839.e7. [Google Scholar] [CrossRef]
- Korkmaz, Y.N.; Buyuk, S.K.; Simsek, H.; Abay, F. Comparison of the Flexural Strength of Three Different Aged and Nonaged 3D-Printed Permanent Crown Resins. Int. J. Prosthodont. 2024, 37, 203–207. [Google Scholar] [CrossRef]
- Nam, N.E.; Hwangbo, N.K.; Kim, J.E. Effects of surface glazing on the mechanical and biological properties of 3D printed permanent dental resin materials. J. Prosthodont. Res. 2024, 68, 273–282. [Google Scholar] [CrossRef]
- Kang, Y.J.; Kim, H.; Lee, J.; Park, Y.; Kim, J.H. Effect of airborne particle abrasion treatment of two types of 3D-printing resin materials for permanent restoration materials on flexural strength. Dent. Mater. 2023, 39, 648–658. [Google Scholar] [CrossRef]
- Vichi, A.; Balestra, D.; Louca, C. Effect of Different Finishing Systems on Surface Roughness and Gloss of a 3D-Printed Material for Permanent Dental Use. Appl. Sci. 2024, 14, 7289. [Google Scholar] [CrossRef]
- Ezmek, B.; Aydin, N. Do Polishing Methods and Colorant Beverages Affect the Color Stainability of 3D-printed Permanent Restorations? J. Adv. Oral Res. 2023, 14, 161–168. [Google Scholar] [CrossRef]
- Krajangta, N.; Klaisiri, A.; Leelaponglit, S.; Intralawan, N.; Tiansuwan, P.; Pisethsalasai, N. Color alteration of CAD/CAM 3D-printed, milled resin-ceramic hybrid material compared to enamel. Dent. Mater. J. 2024, 43, 386–393. [Google Scholar] [CrossRef]
- Çakmak, G.; Oosterveen-Rüegsegger, A.L.; Akay, C.; Schimmel, M.; Yilmaz, B.; Donmez, M.B. Influence of polishing technique and coffee thermal cycling on the surface roughness and color stability of additively and subtractively manufactured resins used for definitive restorations. J. Prosthodont. 2024, 33, 467–474. [Google Scholar] [CrossRef]
- Çakmak, G.; Donmez, M.B.; de Paula, M.S.; Akay, C.; Fonseca, M.; Kahveci, Ç.; Abou-Ayash, S.; Yilmaz, B. Surface roughness, optical properties, and microhardness of additively and subtractively manufactured CAD-CAM materials after brushing and coffee thermal cycling. J. Prosthodont. 2025, 34, 68–77. [Google Scholar] [CrossRef]
- Karaoğlanoğlu, S.; Aydın, N.; Oktay, E.A.; Ersöz, B. Comparison of the Surface Properties of 3D-printed Permanent Restorative Resins and Resin-based CAD/CAM Blocks. Oper. Dent. 2023, 48, 588–598. [Google Scholar] [CrossRef]
- Taşın, S.; Ismatullaev, A. Effect of coffee thermocycling on the color and translucency of milled and 3D printed definitive restoration materials. J. Prosthet. Dent. 2024, 131, 969.e1–969.e7. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar]
- Faggion, C.M. Guidelines for reporting pre-clinical in vitro studies on dental materials. J. Evid. Based Dent. Pract. 2012, 12, 182–189. [Google Scholar] [CrossRef]
- Krithikadatta, J.; Datta, M.; Gopikrishna, V. CRIS guidelines (checklist for reporting in-vitro studies): A concept note on the need for standardized guidelines for improving quality and transparency in reporting in-vitro studies in experimental dental research. J. Conserv. Dent. 2014, 17, 301–304. [Google Scholar] [CrossRef]
- ISO 4049:2019; Polymer-Based Filling, Restorative and Luting Materials. Technical Committee 106-Dentistry. International Standards Organization: Geneva, Switzerland, 2000.
- Bollen, C.M.; Lambrechts, P.; Quirynen, M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. 1997, 13, 258–269. [Google Scholar] [CrossRef]
- Jafarpour, D.; Ferooz, R.; Ferooz, M.; Bagheri, R. Physical and mechanical properties of bulk-fill, conventional, and flowable resin composites stored dry and wet. Int. J. Dent. 2022, 2022, 7946239. [Google Scholar] [CrossRef]
- Mortier, E.; Gerdolle, D.A.; Jacquot, B.; Panighi, M.M. Importance of water sorption and solubility studies for couple bonding agent–resin-based filling material. Oper. Dent. 2004, 29, 669–676. [Google Scholar]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and Machinable Dental Restorative Composites for CAD/CAM Application—Comparison of Mechanical Properties, Fractographic, Texture and Fractal Dimension Analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef]
- Rutkunas, V.; Sabaliauskas, V.; Mizutani, H. Effects of different food colorants and polishing techniques on color stability of provisional prosthetic materials. Dent. Mater. J. 2010, 29, 167–176. [Google Scholar] [CrossRef]
- Alageel, O.; Alhijji, S.; Alsadon, O.; Alsarani, M.; Gomawi, A.A.; Alhotan, A. Trueness, Flexural Strength, and Surface Properties of Various Three-Dimensional (3D) Printed Interim Restorative Materials after Accelerated Aging. Polymers 2023, 15, 3040. [Google Scholar] [CrossRef]
- Rubayo, D.D.; Phasuk, K.; Vickery, J.M.; Morton, D.; Lin, W.S. Influences of build angle on the accuracy, printing time, and material consumption of additively manufactured surgical templates. J. Prosthet. Dent. 2021, 126, 658–663. [Google Scholar] [CrossRef]
- Di Fiore, A.; Meneghello, R.; Brun, P.; Rosso, S.; Gattazzo, A.; Stellini, E.; Yilmaz, B. Comparison of the flexural and surface properties of milled, 3D-printed, and heat polymerized PMMA resins for denture bases: An in vitro study. J. Prosthodont. Res. 2022, 66, 502–508. [Google Scholar] [CrossRef]
- Al-Dulaijan, Y.A.; Alsulaimi, L.; Alotaibi, R.; Alboainain, A.; Alalawi, H.; Alshehri, S.; Khan, S.Q.; Alsaloum, M.; AlRumaih, H.S.; Alhumaidan, A.A.; et al. Comparative Evaluation of Surface Roughness and Hardness of 3D Printed Resins. Materials 2022, 15, 6822. [Google Scholar] [CrossRef]
- Doray, P.G.; Eldiwany, M.S.; Powers, J.M. Effect of resin surface sealers on improvement of stain resistance for a composite provisional material. J. Esthet. Restor. Dent. 2003, 15, 244–249. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| In vitro studies. | Studies in any language other than English. |
| Studies published in English. | Review papers, dissertations, case/technical reports, letters to editors, unpublished abstracts, and commentaries. |
| Studies assessing the physical properties of 3D-printed permanent resins with those of any other materials used to fabricate indirect prosthetic restorations. | Studies comparing the adaptation, marginal fit, and accuracy of 3D-printed permanent resin crowns with those of other materials, with only material properties evaluated. |
| Studies evaluating the mechanical properties of 3D-printed permanent resins with those of any other materials used for fabricating indirect prosthetic restorations. | Studies assessing the effects of different printing parameters on the accuracy and other properties of 3D-printed permanent resins. |
| Studies that compare the physical properties and mechanical or any other properties of different 3D-printed permanent resins. |
| Participant | Permanent resins |
| Intervention | 3D-printing |
| Comparison | Milled resin and hybrid ceramics |
| Outcome | Physical/mechanical properties |
| Database | Search Terms |
|---|---|
| PubMed | (“crowns”[MeSH Terms] OR “crowns”[All Fields] OR (“dental”[All Fields] AND “crown”[All Fields]) OR “dental crown”[All Fields] OR (“denture, partial, fixed”[MeSH Terms] OR (“denture”[All Fields] AND “partial”[All Fields] AND “fixed”[All Fields]) OR “fixed partial denture”[All Fields] OR (“fixed”[All Fields] AND “partial”[All Fields] AND “denture”[All Fields])) OR (“3D”[All Fields] AND (“printed”[All Fields] OR “printing”[MeSH Terms] OR “printing”[All Fields] OR “print”[All Fields] OR “printings”[All Fields] OR “prints”[All Fields]) AND (“permanent”[All Fields] OR “permanently”[All Fields] OR “permanents”[All Fields]) AND (“resin s”[All Fields] OR “resinous”[All Fields] OR “resins, plant”[MeSH Terms] OR (“resins”[All Fields] AND “plant”[All Fields]) OR “plant resins”[All Fields] OR “resin”[All Fields] OR “resins”[All Fields]) AND (“material”[All Fields] OR “material s”[All Fields] OR “materials”[All Fields])) OR (“3D”[All Fields] AND (“printed”[All Fields] OR “printing”[MeSH Terms] OR “printing”[All Fields] OR “print”[All Fields] OR “printings”[All Fields] OR “prints”[All Fields]) AND (“permanent”[All Fields] OR “permanently”[All Fields] OR “permanents”[All Fields]) AND (“material”[All Fields] OR “material s”[All Fields] OR “materials”[All Fields]) AND ((“mechanical”[All Fields] OR “mechanically”[All Fields] OR “mechanicals”[All Fields] OR “mechanics”[MeSH Terms] OR “mechanics”[All Fields] OR “mechanic”[All Fields]) AND (“properties”[All Fields] OR “property”[All Fields])) AND (“physical phenomena”[MeSH Terms] OR (“physical”[All Fields] AND “phenomena”[All Fields]) OR “physical phenomena”[All Fields] OR (“physical”[All Fields] AND “properties”[All Fields]) OR “physical properties”[All Fields]))) AND ((“biological products”[MeSH Terms] OR (“biological”[All Fields] AND “products”[All Fields]) OR “biological products”[All Fields] OR “biologic”[All Fields] OR “biologicals”[All Fields] OR “biological factors”[MeSH Terms] OR (“biological”[All Fields] AND “factors”[All Fields]) OR “biological factors”[All Fields] OR “biologics”[All Fields] OR “biologically”[All Fields] OR “biology”[MeSH Terms] OR “biology”[All Fields] OR “biological”[All Fields]) AND (“properties”[All Fields] OR “property”[All Fields]))) AND ((y_10[Filter]) AND (classical article[Filter] OR clinical study[Filter] OR clinical trial[Filter] OR clinical trial protocol[Filter] OR comparative study[Filter] OR randomized controlled trial[Filter]) AND (English[Filter])) |
| Scopus | (TITLE-ABS-KEY (dental crown) OR TITLE-ABS-KEY (fixed partial denture) OR TITLE-ABS-KEY (3D printed resin materials) AND TITLE-ABS-KEY (mechanical properties) AND TITLE-ABS-KEY (physical properties)) |
| Web of science | ALL = (dental crown) OR ALL = (fixed partial denture) AND ALL = (3D printed permanent resin materials) AND ALL = (Physical properties) AND ALL = (mechanical properties) AND ALL = (biological properties) |
| Sl No | Author/Year | Study Type | Brand Name/Manufacturer of Materials Studied | Composition | Properties Examined | Sample Size (n) | Technique Used for Specimen Fabrication/Printing Parameters | Dimensions and Shape of Specimens |
|---|---|---|---|---|---|---|---|---|
| 1. | Di Fiore et al., 2024 [11] | In vitro | Saremco print Crowntec (Saremco Dental AG) Varseo Smile Crown Plus (Bego GmbH) | Composite resins Resin ceramic hybrid material | MPs—flexural strength (FS), elastic modulus, microhardness PP—surface roughness | n = 40 for FS and elastic modulus (20 in each group) n = 10 for microhardness (5 in each group) n = 20 for water sorption and solubility, surface roughness | 3D-printed with DLP Layer thickness—50 μm Orientation—0° | (25 × 2 × 2 mm) rectangular bars (Ø15 × 3 mm) and (Ø15 × 1 mm) circular disks |
| 2. | Korkmaz et al., 2024 [12] | In vitro | Saremco crowntec Senertec P-Crown V2 Senertec P-Crown V3 | Flowable polymer based on methacrylic acid ester Resin with ceramic fillers | MP—flexural strength | n = 60 aged and non-aged (10 in each group) | SLA Layer thickness—50 μm Orientation—90° | (25 × 2 × 2 mm) rectangular bars |
| 3. | Krajangta et al., 2024 [17] | In vitro | Varseosmile crown plus, VS Cerasmart, CS | Resin–ceramic hybrid material Milled resin ceramic hybrid material | PPs—color and translucency changes | n = 60 (n = 15, immersed in distilled water, coffee) | 3D-printed with DLP Layer thickness—50 μm Orientation—N/M Milled | (12 × 14 × 1.5) rectangular bars |
| 4. | Nam EN et al., 2024 [13] | In vitro | Formlabs, Graphy Tera Harz permanent | Methacrylic acid ester-based 3D-printed permanent resin 3D-printed resins | MPs—flexural strength, Vickers hardness PPs—color stability, surface roughness | n = 45 (n = 5, no treatment, glazed, sand glazed) | 3D-printed with DLP Layer thickness—50 μm Orientation—N/M | (10 × 18 × 4) rectangular bars (9 × 2) circular disks |
| 5. | Çakmak G et al., 2023 [19] | In vitro | Crowntec, CT VarseoSmile Crown Plus, VS Brilliant Crios, BC Enamic, VE Mark II, VM | 3D-printed composite resin 3D-printed hybrid composite resins Milled reinforced composite resin Milled polymer-infiltrated ceramic network Milled felspathic ceramic | MP—microhardness PP—surface roughness | n = (10) | 3D-printed with DLP Layer thickness—50 μm Orientation—N/M Wet-sliced with precision cutter | (Ø10 × 1 mm) circular disks |
| 6. | Karaoğlanoğlu et al., 2023 [20] | In vitro | Cerasmart 270 (GC, Zahnfabrik, Germany) Grandio Blocs (VOCO GmbH, Germany) Crowntec (Saremco Dental AG, Switzerland) Permanent Crown (Formlabs, USA) | Nanoceramic CAD/CAM block Nanohybrid CAD/ CAM block 3D-printed permanent resin Methacrylic acid ester-based printed permanent resin | MP—microhardness PPs—surface roughness, color changes | n = 96 (n = 8, immersed in tea, coffee, and distilled water) | Precision cutting machine 3D-printed with DLP 3D-printed with SLA Layer thickness—50 μm Orientation—N/M | (12 × 8 × 2) rectangular bars |
| 7. | Vichi A et al., 2024 [15] | In vitro | Permanent Crown (Formlabs, USA) | Methacrylic acid ester-based printed permanent resin | PPs—surface roughness, color changes | n = 80 (n = 10) 8 different finishing and polishing methods Sof-Lex™ Spiral Wheels (SW), Identoflex Lucent no paste (Ln), Sof-Lex™ XT Pop-on Disc (SD), Identoflex Lucent + paste (Lp), resin nitrogen polymerized (NG), Optiglaze (OG), Opti1Step (OS), and HiLusterPLUS (HL) | 3D-printed with SLA Layer thickness—50 μm Orientation—N/M | (14 × 14 × 5 mm) square shape |
| 8. | Ezmek et al., 2023 [16] | In vitro | Permanent Crown (Formlabs, USA) | Methacrylic acid ester-based 3D-printed permanent resin | PP—color changes | n = 120 (n = 10) a. mechanical polishing; b. Optiglaze (GC Dental Products Corp, Aichi, Japan); c. Vita Akzent LC (VITA Zahnfabrik, Bad Säckingen, Germany). subgroups immersed in distilled water, coffee, tea, and red wine | 3D-printed with SLA Layer thickness—50 μm Orientation—0° | (10 mm × 1.5 mm) circular disks |
| 9. | Bozogullari et al., 2023 [6] | In vitro | Crowntec Permanent Crown Resin | 3D-printed permanent resin Methacrylic acid ester-based 3D-printed permanent resin | PPs—color stability, stainability, surface roughness | N = 150 (n = 10 for material surface roughness) (n = 20 for material for color stability and stainability) | 3D-printed with DLP 3D-printed with stereolithography Layer thickness—50 μm Orientation—90° | rectangular-shaped specimens (14 × 12 × 2 mm) |
| 10. | Tasin et al., 2024 [21] | In vitro | VarseoSmile Crownplus (VSP), Permanent Crown (PC) IPS e.max CAD (LDS) Vita Enamic (PICN), Cerasmart (RNC) | 3D-printed permanent resin Methacrylic acid ester-based printed permanent resin Lithium disilicate-based glass-matrix ceramic Polymer-infiltrated feldspathic ceramic Polymer-infiltrated feldspathic ceramic Composite resin material | PPs—color changes, translucency | n = 60 (n = 12 per group) | 3D-printed with DLP 3D-printed with SLA Layer thickness—50 μm Orientation—0° | plate-shaped specimens (12 × 12 × 1 mm) |
| 11. | Kang et al., 2023 [14] | In vitro | Tera Harz TC-80DP Graphy, Seoul, Korea. Permanent Crown Formlabs, Somerville, MA, USA. | UDMA resin Bis-EMA (BEMA) resin | MP—flexural strength | n = 196 | 3D-printed with DLP 3D-printed with SLA | bar-shaped specimens (25 mm × 2 × 2 mm) |
| 12. | Çakmak et al., 2023 [18] | In vitro | Crowntech (CT) VarseoSmile Crownplus (VS) Cera Smart (CS) | 3D-printed resin 3D-printed resin Nanoceramic resin | PP—surface roughness, color stability | n = 90 (n = 30 per group) | 3D-printed with DLP Layer thickness—50 μm Orientation—0° | rectangular-shaped (14 × 12 × 1 mm) |
| 13. | Temizci et al., 2024 [2] | In vitro | Saremco Print Crowntec [SC] Formlabs Permanent Crown Resin [FP]) Vita Mark II [VM] Cerasmart 270 [CS] Vita Enamic [VE] | Composite-based resin Composite-based resin Feldspatic glass ceramic Polymer infiltrated ceramic Hybrid nanoceramic | MPs—flexural strength, microhardness | n = 200 (n = 40 per group) | 3D-printed with DLP 3D-printed with SLA Layer thickness—50 μm Orientation—90° | disk-shaped specimens (13 × 1.2 mm) for flexural strength 100 square specimens (14 × 14 × 2 mm) for VHN test |
| Item | 1 | 2a | 2b | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Di Fiore A et al., 2024 [11] | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No | Yes | Yes | No | No | Yes |
| Kormaz et al., 2024 [12] | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No | Yes | Yes | No | No | Yes |
| Krajangta et al., 2024 [17] | No | Yes | Yes | Yes | Yes | Yes | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Nam et al., 2024 [13] | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Çakmak G et al., 2023 [19] | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Karaoğlanoğlu S et al., 2023 [20] | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Vichi et al., 2024 [15] | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Ezmek B et al., 2023 [16] | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Bozogulları HN et al. 2024 [6] | No | Yes | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Tasin S et al., 2024 [21] | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Kang, YJ et al., 2023 [14] | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Çakmak G et al., 2023 [18] | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Temizci T et al., 2024 [2] | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Sl No | Author/Year | SR Before | SR After Surface Treatment | Medium of Exposure Causing Changes in Surface Roughness | Measuring Device Used | Conclusion |
|---|---|---|---|---|---|---|
| 1. | Di Fiore et al., 2024 [11] | Saramco—0.52 ± 0.05 μm Varseo smile—0.54 ± 0.04 μm | 0.97 ± 0.06 μm 0.88 ± 0.05 μm | Toothbrushing simulated device with total of 10,000 cycles | Noncontact profilometer | The surface roughness of both 3D-printed resins was affected by brushing simulation. |
| 2. | Nam et al., 2024[13] | Formlabs No treatment—0.47 ± 0.12 μm Glazing—0.03 ± 0.02 μm Sand glazing—0.03 ± 0.01 μm Graphy No treatment—0.47 ± 0.12 μm Glazing—0.03 ± 0.02 μm Sand glazing—0.03 ± 0.01 μm | Formlabs No treatment—0.08 ± 0.00 μm Glazing—0.02 ± 0.00 μm Sand glazing—0.02 ± 0.00 μm Graphy No treatment—0.23 ± 0.14 μm Glazing—0.05 ± 0.04 μm Sand glazing—0.07 ± 0.05 μm | Artificial toothbrushing device specimen brushed for 20,000 cycles | Stylus profilometer | Samples with sand-glazed and glazed surfaces exhibited low surface roughness. |
| 3. | Karaoğlanoğlu et al., 2023 [20] | Grandio Blocs Baseline—0.187 ± 0.01 μm Cerasmart 270 Baseline—0.146 ± 0.01 μm Crowntec Baseline—0.187 ± 0.01 μm Permanent Crown Baseline—0.191 ± 0.01 μm | Grandio Blocs Coffee—0.196 ± 0.01 μm Tea—0.198 ± 0.01 μm Water—0.193 ± 0.01 μm Cerasmart 270 Coffee—0.154 ± 0.01 μm Tea—0.156 ± 0.02 μm Water—0.148 ± 0.01 μm Crowntec Coffee—0.195 ± 0.02 μm Tea—0.198 ± 0.02 μm Water—0.189 ± 0.01 μm Permanent Crown Coffee—0.195 ± 0.02 μm Tea—198 ± 0.01 μm Water—0.193 ± 0.01 μm | Immersion in coffee, tea, and distilled water and stored in incubator for 30 days at 37 °C | Contact Profilometer | Cerasmart 270 showed the lowest surface roughness, Grandio blocs and Crowntec showed the same values, and Permanent Crown showed more surface roughness. |
| 4. | Vichi et al., 2024 [15] | Permanent Crown (Formlabs, USA) | NG—0.25 μm SD—0.44 μm OG—0.46 μm Lp—0.52 μm Ln—0.59 μm OS—0.73 μm SW—0.77 μm HL—0.83 μm | Finishing and polishing methods Sof-Lex™ Spiral Wheels (SW), Sof-Lex™ XT Pop-on Disc (SD), Identoflex Lucent no paste (Ln), Identoflex Lucent + paste (Lp), resin nitrogen polymerized (NG), Optiglaze (OG), Opti1Step (OS), and HiLusterPLUS (HL) | Profilometer | NG > SD = OG = Lp; Lp = Ln; Ln = OS; OS = SW; and SW = HL. |
| 5. | Bozogullari et al., 2023 [6] | Crowntec SC 0.039 ± 0.005 μm Permanent Crown—0.044 ± 0.004 μm Cerasmart 270—0.037 ± 0.008 μm Vita Enamic—0.174 ± 0.043 μm Vitamark II—0.096 ± 0.035 C μm | Crowntec SC 0.038 ± 0.007 μm Permanent Crown 0.045 ± 0.009 μm Cerasmart 270 0.041 ± 0.008 μm Vita Enamic 0.201 ± 0.041 μm Vitamark II 0.115 ± 0.031 μm | Thermocycling, 5000 cycles | Profilometer | Ra values before thermocycling: VE > VM > PC > SC > CS. Ra values after thermocycling: VE > VM > PC > CS > SC. In general, surface roughness increased after thermocycling. |
| 6. | Kang et al., 2023 [14] | Tera Harz TC-80DP Control—0.63 ± 0.05 μm Permanent Crown Control—0.68 ± 0.08 μm | Tera Harz TC-80DP at 0.1/0.2/0.3 MPa with 50 µm alumina 0.32 ± 0.04/0.93 ± 0.05/1.73 ± 0.16 μm Tera Harz TC-80DP at 0.1/0.2/0.3 MPa with 100 µm alumina 0.62 ± 0.45/1.62 ± 0.29/1.44 ± 0.2 μm Permanent Crown at 0.1/0.2/0.3 MPa with 50 µm alumina 0.96 ± 0.68/1.29 ± 0.09/2.34 ± 0.30 μm Permanent Crown at 0.1/0.2/0.3 MPa with 100 µm alumina 1.10 ± 0.15/2.77 ± 0.47/3.23 ± 0.74 μm | Air particle abrasion using alumina particles of 50 and 110 µm, 10,000 thermal cycles | Field emission scanning electron microscope | Both the resins presented porosity on the surface after the surface treatment with alumina particles. Deep cracks and irregular deep areas were observed in the Permanent Crown group treated with coarse particles under high pressure. Increase in surface roughness observed with sandblasting particle size and the pressure of the 3D printing resin. |
| 7. | Çakmak et al., 2023 [18] | Cerasmart—CP/OG/VA 0.27 ± 0.09/0.23 ± 0.10/0.24 ± 0.03 μm Crown tech—CP/OG/VA 0.49 ± 0.24/0.5 ± 0.19/0.6 ± 0.28 μm VarseoSmile Crown Plus—CP/OG/VA 0.37 ± 0.06/0.29 ± 0.06/0.3 ± 0.04 μm | Cerasmart—CP/OG/VA 0.1 ± 0.01/0.14 ± 0.05/0.28 ± 0.01 μm Crown tech—CP/OG/VA 0.19 ± 0.11/0.31 ± 0.12/0.40 ± 0.17 μm VarseoSmile Crown Plus—CP/OG/VA 0.16 ± 0.11/0.21 ± 0.10/0.26 ± 0.12 μm | Conventional polishing (control-CP)/application of surface sealant (Optiglaze; GC Corp (OG)/ Vita Akzent LC; Vita Zahnfabrik (VA)) Coffee thermal cycling, 10,000 cycles | Profilometer | Before polishing: conventional polishing—CT > VA > CS OG-CT > VA > CS VA-C T > VA > CS. After Coffee thermal cycling and polishing: conventional polishing—CT > VA > CS OG-CT > VA > CS VA-C T > VA > CS. The Ra of CS was similar to or lower than the Ra of other materials, regardless of the polishing technique. CP mostly led to lower Ra values than other polishing techniques, whereas VA resulted in a high Ra regardless of the material-time. |
| 8. | Çakmak et al., 2023 [19] | VarseoSmile Crown Plus (VS)—3.58 ± 1.01 μm Crown tech (CT)2.79 ± 1.10 μm BRILLIANT Crios (BC)—0.27 ± 0.03 μm Enamic (VE)—0.64 ± 0.32 μm Mark II (VM)—0.70 ± 0.11 μm | VarseoSmile Crown Plus (VS) After polishing/after brushing/coffee thermocycling 0.36 ± 0.12/0.85 ± 0.47/0.43 ± 0.16 μm Crown tech (CT)—0.71 ± 0.62/0.61 ± 0.14/0.40 ± 0.11 μm BRILLIANT Crios (BC)—0.15 ± 0.05/0.81 ± 0.14/0.74 ± 0.14 μm Enamic (VE)—0.25 ± 0.04/0.27 ± 0.06/0.20 ± 0.03 μm Mark II (VM)—0.17 ± 0.05/0.14 ± 0.03/0.17 ± 0.03 μm | VarseoSmile and Crown tech—conventional polishing BRILLIANT Crios and Enamic—two-step polishing kit VM: Mark II—finishing with flexible disks, polishing using diamond polishing paste 25,000 cycles of artificial brushing using automatic brushing machine 10,000 thermal cycles | Profilometer | Before polishing—VS > CT > VE > VM > BC After polishing—CT > VS > VE > VM > BC After brushing—VS > BC > CT > VE > VM After coffee thermal cycling—BC > VS > CT > VE > VM Before polishing, all materials had their highest surface roughness except BC, where roughness increased after brushing and coffee thermal cycling. |
| Sl No | Author/year | Medium of Immersion/Surface Treatment | Aging/Duration of Immersion | 3D-Printed Permanent Resin—Mean Color Changes | Milled Resin—Mean Color Change | Instrument Used | Conclusion |
|---|---|---|---|---|---|---|---|
| 1. | Krajangta et al., 2024 [17] | Immersion in
| 30 days of immersion | Varseo smile crown plus ∆TP = −1.37 (0.17 units) immersed in water ∆TP = −0.23 (0.06) units immersed in coffee | Cerasmart ∆TP = −1.03 (0.54) units immersed in water ∆TP = −0.39(0.6) units immersed in coffee | Spectrophotometer Vita Easyshade™ Advance 4.0 | The translucency of both resins reduced after immersion in water and coffee. |
| 2. | Nam et al., 2024 [13] | Resin surface with no treatment/glazed/sand glazed Immersion in
| 30 days of immersion | ∆E Form labs—No treatment/glazed/sand glazed Coffee—7.5 ± 3.6, 7.0 ± 1.3, 6.3 ± 1.1 units Curry—18.5 ± 14.1, 2.6 ± 1.2, 1.9 ± 0.5 units Distilled water—1.7 ± 0.3, 2.4 ± 0.7, 3.0 ± 0.3 units Graphy Coffee—2.6 ± 0.8, 3.4 ± 1.3, 3.2 ± 1.9 units Curry—18.7 ± 4.2, 6.4 ± 2.8, 5.4 ± 1.4 units Distilled water—3.8 ± 0.6, 6.4 ± 0.7, 5.6 ± 0.2 units | NA | Colorimeter | Greater color changes were observed in untreated samples than glazed and sand-glazed samples and they varied with the surface treatment. |
| 3. | Karaoğlanoğlu et al., 2023 [20] | Immersion in tea, coffee, and distilled water; stored at 37 °C | 30 days of immersion | ∆E at 1 day/7 days/30 days Crowntec Coffee—0.4 ± 0.1/1.5 ± 0.2/3.2 ± 0.4 units Tea—0.9 ± 0.2/4.1 ± 0.4/6.3 ± 0.5 units Water—0.3 ± 0.1/0.4 ± 0.1/0.6 ± 0.1 units Permanent Crown Coffee—0.6 ± 0.1/1.4 ± 0.2/2.7 ± 0.2 units Tea—0.8 ± 0.2/3.9 ± 0.3/5.6 ± 0.3 units Water—0.4 ± 0.1/0.6 ± 0.1/0.7 ± 0.1 units | ∆E at 1 day/7 days/30 days Grandio Blocs Coffee—0.5 ± 0.1/1.3 ± 0.2/1.8 ± 0.1 units Tea—0.9 ± 0.1/3.6 ± 0.3/4.2 ± 0.3 units Water—0.3 ± 0.1/0.5 ± 0.1/0.7 ± 0.1 units Cerasmart 270 Coffee—0.6 ± 0.1/1.2 ± 0.2/1.8 ± 0.2 units Tea—0.8 ± 0.1/3.4 ± 0.3/4.4 ± 0.3 units Water—0.4 ± 0.1/0.6 ± 0.1/0.7 ± 0.1 units | Spectrophotometer device | Color changes observed in 3D-printed resins and resin-based CAD/CAM blocks immersed in tea and coffee were similar on the first and seventh days, with greater color changes noted in the 3D-printed resins after 30 days. |
| 4. | Ezmek et al., 2023 [16] | a. mechanical polishing. b. Optiglaze (GC Dental Products Corp, Aichi, Japan); c. Vita Akzent LC (VITA Zahnfabrik, Bad Säckingen, Germany); later immersion in distilled water, coffee, tea, and red wine | 30 days of immersion | Distilled water/coffee/tea/red wine Mechanical polishing 0.77 ± 0.19/3.65 ± 0.95/3.56 ± 1.00/4.90 ± 1.48 units Optiglaze 1.05 ± 0.27/0.87 ± 0.23/0.65 ± 0.12/0.47 ± 0.21 units Vita Akzent LC 1.88 ± 0.30/2.85 ± 0.28/1.66 ± 0.55/0.92 ± 0.30 units | NA | Spectrophotometer | Mechanical polishing groups showed the highest ΔE00 values. The most significant discoloration in the mechanical polishing group was due to red wine. Optiglaze reduced the discoloration caused by all beverages in the 3D-printed resin group. Vita Akzent LC reduced discoloration caused by tea and red wine. |
| 5. | Bozo gullari et al., 2023 [6] | Immersion in distilled water and coffee after thermocycling | 7 days at 37 °C | ∆E00 Crowntec SC Distilled water—before/after 2.57 ± 0.56/3.62 ± 0.48 units Coffee 2.53 ± 0.61/5.36 ± 0.58 units Permanent Crown Distilled water 0.93 ± 0.25/1.04 ± 0.51 units Coffee 0.90 ± 0.28/1.99 ± 0.26 units | Cerasmart Distilled water 1.17 ± 0.37/1.29 ± 0.43 units Coffee 1.18 ± 0.37/1.44 ± 0.33 units Vita Enamic Distilled water 1.19 ± 0.39/1.20 ± 0.44 units Coffee 1.24 ± 0.34/2.36 ± 1.53 units Vitamark II Distilled water 0.75 ± 0.07/0.76 ± 0.10 units Coffee 0.77 ± 0.04/2.18 ± 0.34 units | Spectrophotometer | The highest mean ∆E00 values were seen in the SC group (2.57_0.56), followed by those in VE (1.20_0.44), CS (1.18_0.37), FP (0.93_0.25), and VM (0.76_0.10). The highest mean DE00 values in coffee solution (5.36_0.58) and distilled water (3.62_0.48) were seen in SC group. The lowest mean DE00 values (0.77_0.04) in distilled water at T2 were seen in the VM group. The CS group also showed the lowest mean DE00 value (1.44_0.33) in coffee Crowntec and Vita Enamic showed unacceptable color changes. |
| 6. | Tasin et al., 2024 [21] | Immersed in coffee and thermocycled for 10,000 cycles | Immersion in coffee | ∆E00 VarseoSmile Crown plus (VSP) 1.38/−0.65 units Permanent Crown (PC) 1.35/−0.43 units | ∆E00/∆RTA00 IPS e.max CAD (LDS) 0.48/−0.17 units Vita Enamic (PICN) 0.96/-0.24 units Cerasmart (RNC) 1.03/−0.37 units | Spectrophotometer | The highest ΔE00 values were found in VSP and PC, and the lowest ΔE00 values were found in LDS. The highest|ΔRTP00 |values were observed for VSP, and the lowest|ΔRTP00|values were found in LDS after coffee thermocycling. |
| 7. | Çakmak et al., 2023 [18] | Immersed in coffee after polishing and thermocycled for 10,000 cycles | Immersion in coffee | ∆E00 Crown Tech—Conventional polishing/optiglaze/Vita Akzent 0.89 ± 0.18/1.04 ± 0.60/1.52 ± 0.84 units VarseoSmile Crown Plus 1.98 ± 0.18/1.38 ± 0.59/1.77 ± 0.68 units | ∆E00 Cerasmart—Conventional polishing/optiglaze/Vita Akzent 0.47 ± 0.34/0.99 ± 0.42/1.04 ± 0.35 units | Spectrophotometer | Polishing techniques affected the ΔE00 values of CS and VS while only CP affected the ΔE00 values among tested materials. CS OG < VA < CP VS OG < CP < VS CS-VA had moderately unacceptable color change. |
| 8. | Çakmak et al., 2023 [19] | Polishing/brushing/coffee thermal cycling | Tooth brushing, 25000 cycles Coffee thermal cycling, 10,000 cycles | ∆E00 Crown Tech After polishing/after brushing/coffee thermal cycling 1.74 ± 0.52/1.47 ± 0.46/2.44 ± 0.52units VarseoSmile Crown Plus (VS) After polishing/after brushing/coffee thermal cycling 1.19 ± 0.68/9.35 ± 0.54/9.13 ± 1.41 units | ∆E00 Enamic,(VM) After polishing/after brushing/coffee thermal cycling 0.87 ± 0.40/1.25 ± 0.29/0.92 ± 0.14 units BRILLIANT Crios (BC) After polishing/after brushing/coffee thermal cycling 1.27 ± 0.55/0.47 ± 0.20/1.14 ± 0.59 units Mark II (VM) After polishing/after brushing/coffee thermal cycling 0.87 ± 0.40/1.25 ± 0.29/0.92 ± 0.14 units | Spectrophotometer | After polishing: CT > BC > VS > VM > VE. After brushing: VS > CT > VM > VE > BC. After coffee thermal cycling: VS > CT > BC > VM > VE. VS had the highest ΔE00 values. |
| Sl No | Author/Year | Water Sorption | Solubility | Conclusion |
|---|---|---|---|---|
| 1. | Di Fiore et al., 2024 [11] | Saramco—11.52 ± 0.6 g/mm3 Varseo smile—12.43 ± 0.4 g/mm3 | 1.36 ± 0.4 g/mm3 0.98 ± 0.3 g/mm3 | After 21 days, both the resins showed significant difference in water sorption values. |
| Sl No | Author and Year | Mean/Median Values of Maximum Force for 3D-Printed Resins | Mean/Median Values of Maximum Force for Milled/Hybrid Ceramics | Exposure Medium/Aging Technique | Machine Used for Testing | Conclusion |
|---|---|---|---|---|---|---|
| 1. | Di Fiore et al., 2024 [11] | Saramco—123.4 ± 8.7 MPa (dry) 97.5 ± 15.2 MPa (30 days after storage) Varseo smile—109.9 ± 15.8 (dry) 94.2 ± 11.7 MPa (30 days after storage) | NA | Stored in distilled water for 30 days at 37 ± 1 °C. | UTM | The flexural strength of both 3D-CRs decreased due to artificial aging. |
| 2. | Korkmaz et al., 2024 [12] | Saremco Crowntec Aged—88.04 MPa Non-aged—92.06 MPa Senertec P—Crown V2 Aged—57.03 MPa Non-aged—63.13 MPa Senertec P—Crown V3 Aged—65.88 MPa Non-aged—71.81 MPa | NA | Thermocycling, 10,000 cycles | UTM | Saremco Crowntec aged and non-aged groups > Senertek P Crown V3 > Senertek P Crown V2. Artificial aging decreased values of flexural strength in all 3D-printed resin groups. |
| 3. | Nam et al., 2024 [13] | Formlabs No treatment—133.1 ± 16.2 MPa Glazing—146.6 ± 19.0 MPa Sand glazing—136.2 ± 13.7 MPa Graphy No treatment—130.6 ± 9.2 MPa Glazing—161.5 ± 6.1 MPa Sand glazing—158.9 ± 11.8 MPa | NA | Glazing—surfaces were coated by a resin-exclusive photocuring glazing solution (OPTIGLAZE, GC Corporation, Tokyo, Japan); Sand glazed surfaces were coated by a resin exclusive photocuring glazing solution after sandblasting with 50 μm aluminum oxide particles | UTM | The flexural strength of Formlabs samples was significantly lower regardless of surface treatment. |
| 4. | Kang et al., 2023 [14] | Tera Harz TC-80DP Before—Control/0.1/0.2/0.3 MPa with 50 µm alumina 141.11/141.35/134.30/130.02 MPa Before—Control/0.1/0.2/0.3 MPa with 110 µm alumina 141.11/134.52/133.82/121.77 MPa After—Control/0.1/0.2/0.3 MPa with 50 µm alumina 134.57/112.15/112.77/110.22 MPa After—Control/0.1/0.2/0.3 MPa with 110 µm alumina 134.57/106.85/106.61/108.29 MPa Permanent Crown Before—Control/0.1/0.2/0.3 MPa with 50 µm alumina 125.68/111.99/112.88/112.42 MPa Before—Control/0.1/0.2/0.3 MPa with 100 µm alumina 125.68/89.330/84.455/83.786 MPa After—Control/0.1/0.2/0.3 MPa with 50 µm alumina 72.455/84.268/71.277/74.170 MPa After—Control/0.1/0.2/0.3 MPa with 100 µm alumina 72.455/71.036/78.991/70.848 MPa | N/A | Air particle abrasion using 50 and 110 µm alumina particles 10,000 thermal cycles between 5 °C and 55 °C in distilled water | UTM | The Tera Harz group exhibited higher flexural strength compared with the Permanent Crown group. Flexural strength decreased significantly after thermocycling in both groups. |
| 5. | Temizci et al., 2024 [2] | Saremco Print Crowntec [SC] Non-aging—232.67 ± 5.94 MPa Aging—215.31 ± 6.39b MPa Formlabs Permanent Crown Resin [FP] Non-aging—234.67 ± 6.14 MPa Aging—230.23 ± 10.35 MPa | Vita Mark II [VM] Non-aging—173.49 ± 3.47 MPa Aging—153.49 ± 5.37 MPa Cerasmart 270 [CS] Non-aging—296.11 ± 11.56 MPa Aging—278.05 ± 6.11 MPa Vita Enamic [VE] Non-aging—173.99 ± 1.99 MPa Aging—173.63 ± 4.77 MPa | Thermocycling, 5000 cycles | UTM | CS > FP > SC > VE > VM after thermal cycling. Thermal cycling had an insignificant effect on flexural strength values for all tested materials. |
| Sl No | Author/Year | Mean Microhardness of 3D-Printed Resin | Mean Microhardness of Milled Resin | Surface Treatment/Exposure Medium | Machine Used for Testing | Conclusion |
|---|---|---|---|---|---|---|
| 1. | Di Fiore et al., 2024 [11] | Saramco—33.2 ± 0.8 Hv (dry); 31.7 ± 0.9 Hv (30 days after storage) Varseo smile—31.5 ± 0.6 (dry); 29.6 ± 1.0 Hv (30 days after storage) | NA | Stored for 30 days in distilled water at 37 ± 1 °C | Microhardness tester | No significant difference between two groups. |
| 2. | Nam et al., 2024 [13] | Formlabs No treatment—25.4 ± 3.1 Hv Glazing—26.5 ± 2.4 Hv Sand glazing—30.5 ± 3.9 Hv Graphy No treatment —9.7 ± 1.7 Hv Glazing—11.5 ± 1.2 Hv Sand glazing—11.2 ± 1.2 Hv | NA | No treatment Glazed Sand glazed | Microhardness indentation device | VHN of Formlabs-samples was higher than that of graphy samples. |
| 3. | Karaoğlanoğlu et al., 2023 [20] | Crowntec Baseline—30.0 ± 1.3 Hv Coffee—29.9 ± 1.2 Hv Tea—29.8 ± 1.3 Hv Water—31.0 ± 1.2 Hv Permanent Crown Baseline—37.4 ± 1.3 Hv Coffee—36.6 ± 1.7 Hv Tea—35.8 ± 1.7 Hv Water—37.4 ± 1.4 Hv | Grandio Blocs Baseline 203.9 ± 3.6 Hv Coffee—192.8 ± 4.7 Hv Tea—180.8 ± 3.9 Hv Water—199.1 ± 4.5 Hv Cerasmart 270 Baseline—109.5 ± 1.9 Hv Coffee—103.8 ± 2.7 Hv Tea—98.3 ± 2.4 Hv Water—102.8 ± 3.8 Hv | Immersion in coffee tea and distilled water and stored in incubator at 37 °C for 30 days. | Vickers microhardness tester | Grandio Blocs CAD/CAM Block > Cerasmart 270 > Permanent Crown > Crowntec. |
| 4. | Çakmak et al., 2023 [19] | Varseo Smile Crown Plus (VS) After polishing/after brushing/coffee thermal cycling 34.57 ± 1.23/33.26 ± 1.62/32.47 ± 1.78 Hv Crown Tech (CT) After polishing/after brushing/coffee thermal cycling 30.59 ± 2.95/29.74 ± 2.66/30.49 ± 3.91 Hv | BRILLIANT Crios (BC) 82.2 ± 7.08/80.26 ± 6.81/73.76 ± 4.69 Hv Enamic VE 286.3 ± 22.87/282 ± 13.14/266.47 ± 19.72 Hv Mark II (VM) 680.55 ± 37.73/679.93 ± 28.32/558.66 ± 39.82 Hv | 25,000 cycles of artificial brushing using an automatic brushing machine Immersion in coffee and 10,000 thermal cycles | Vickers microhardness tester | VM > VE > BC > VS > CT. VS and CT had lowest microhardness values followed by VM, VE, and BC in decreasing order. Microhardness of VM reduced after coffee thermocycling. |
| 5. | Temizci et al., 2024 [2] | Saremco Print Crowntec [SC] Non-aging –232.67 ± 5.94 Hv Aging—215.31 ± 6.39 Hv Formlabs Permanent Crown Resin [FP] Non-aging—234.67 ± 6.14 Hv Aging—230.23 ± 10.35 Hv | Vita Mark II [VM] Non-aging—173.49 ± 3.47 Hv Aging—153.49 ± 5.37 Hv Cerasmart 270 [CS] Non-aging—296.11 ± 11.56 Hv Aging—278.05 ± 6.11 Hv Vita Enamic [VE] Non-aging—173.99 ± 1.99 Hv Aging—173.63 ± 4.77 Hv | Thermocycling, 5000 cycles | Emcotest- Durascan G5 hardness testing device | VM > VE > CS > FP > SC. 3D-printed resin groups exhibited lowest VHN values. Effect of thermocycling significantly affected only VE and VM groups. |
| Sl No | Author/Year | Mean/Median Values of Maximum Force | Exposure Medium/Aging Technique | Machine Used for Testing | Conclusion |
|---|---|---|---|---|---|
| 1. | Di Fiore et al., 2024 [11] | Saramco—4.20 ± 0.3 Gpa (dry); 4.00 ± 0.2 Gpa (30 days after storage) Varseo smile—3.82 ± 0.2 Gpa (dry); 3.70 ± 0.1 Gpa (30 days after storage) | Stored in distilled water for 30 days at 37 ± 1 °C | UTM | Significant difference was found between Crowntec 3D CR, Saremco Print, and Varseo Smile Crown Plus 3D CR after immersion in water for 30 days. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Swapna, B.V.; Shivamurthy, B.; George, V.T.; Sulaya, K.; Nayak, V.M. Mechanical and Physical Properties of Durable Prosthetic Restorations Printed Using 3D Technology in Comparison with Hybrid Ceramics and Milled Restorations—A Systematic Review. Prosthesis 2025, 7, 90. https://doi.org/10.3390/prosthesis7040090
Swapna BV, Shivamurthy B, George VT, Sulaya K, Nayak VM. Mechanical and Physical Properties of Durable Prosthetic Restorations Printed Using 3D Technology in Comparison with Hybrid Ceramics and Milled Restorations—A Systematic Review. Prosthesis. 2025; 7(4):90. https://doi.org/10.3390/prosthesis7040090
Chicago/Turabian StyleSwapna, Bettanapalya. V., B. Shivamurthy, Vinu Thomas George, Kavishma Sulaya, and Vaishnavi M Nayak. 2025. "Mechanical and Physical Properties of Durable Prosthetic Restorations Printed Using 3D Technology in Comparison with Hybrid Ceramics and Milled Restorations—A Systematic Review" Prosthesis 7, no. 4: 90. https://doi.org/10.3390/prosthesis7040090
APA StyleSwapna, B. V., Shivamurthy, B., George, V. T., Sulaya, K., & Nayak, V. M. (2025). Mechanical and Physical Properties of Durable Prosthetic Restorations Printed Using 3D Technology in Comparison with Hybrid Ceramics and Milled Restorations—A Systematic Review. Prosthesis, 7(4), 90. https://doi.org/10.3390/prosthesis7040090








