Finger Orthoses for Rehabilitation―Part I: Biomedical Insights and Additive Manufacturing Innovations
Abstract
1. Introduction
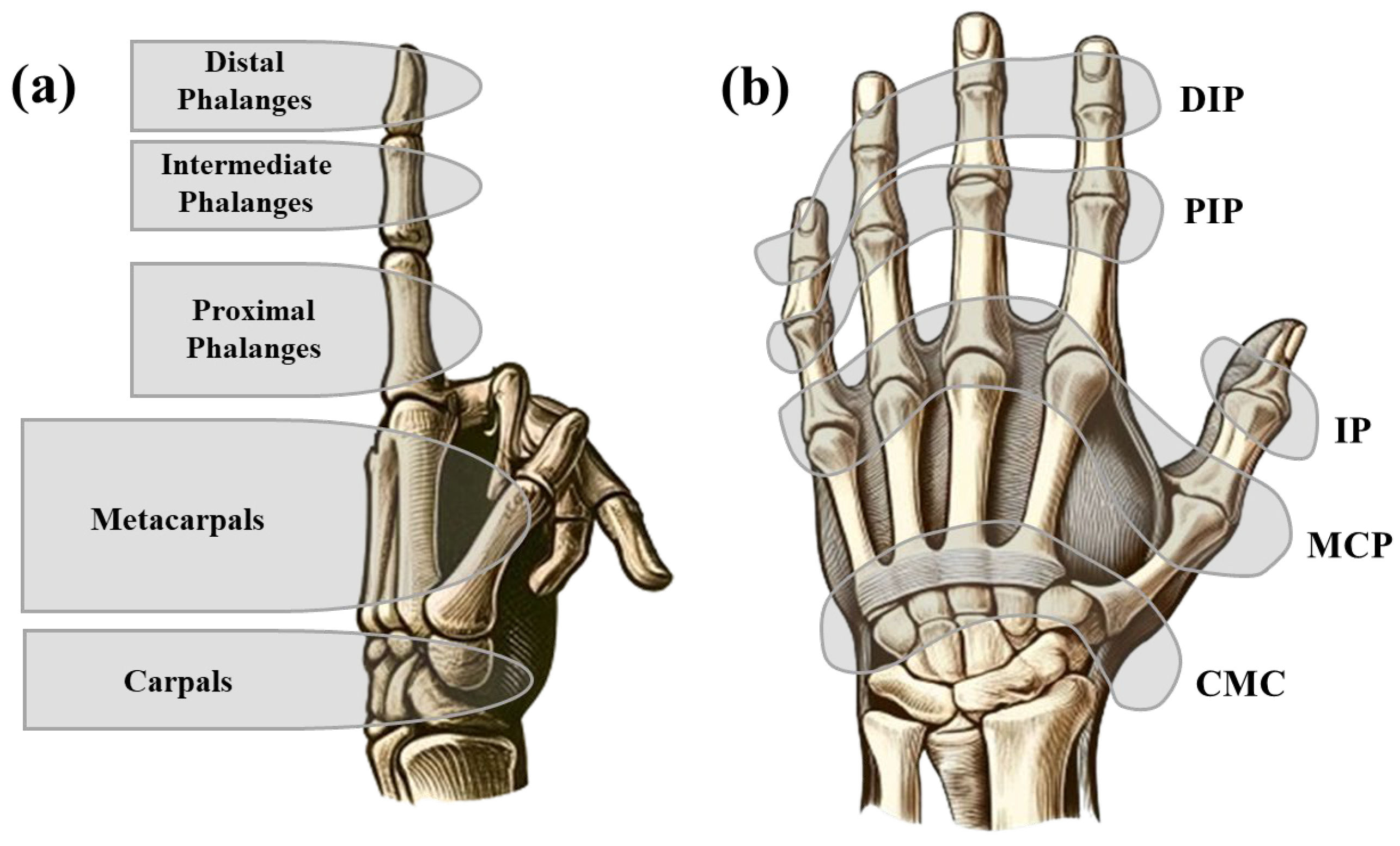
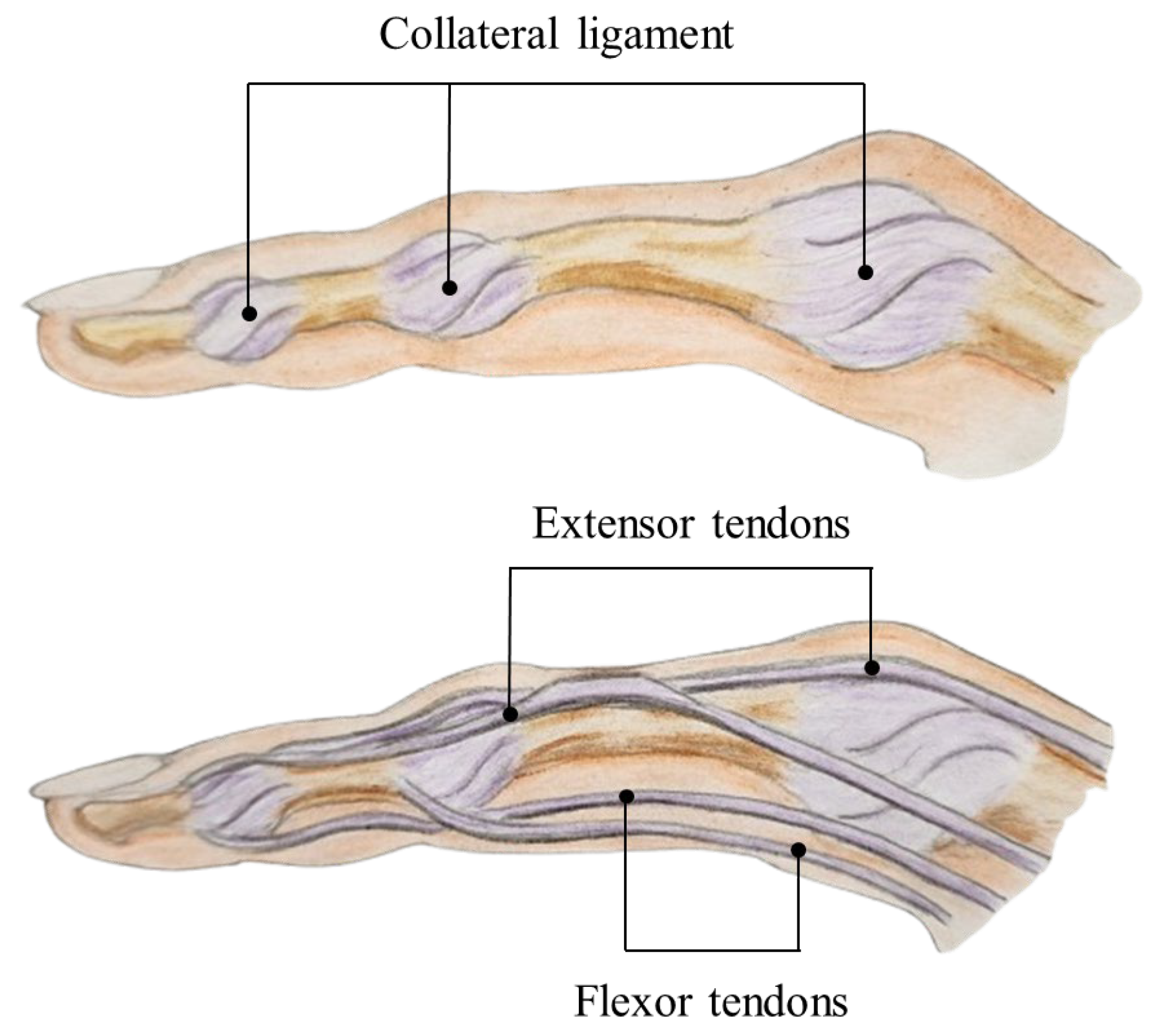
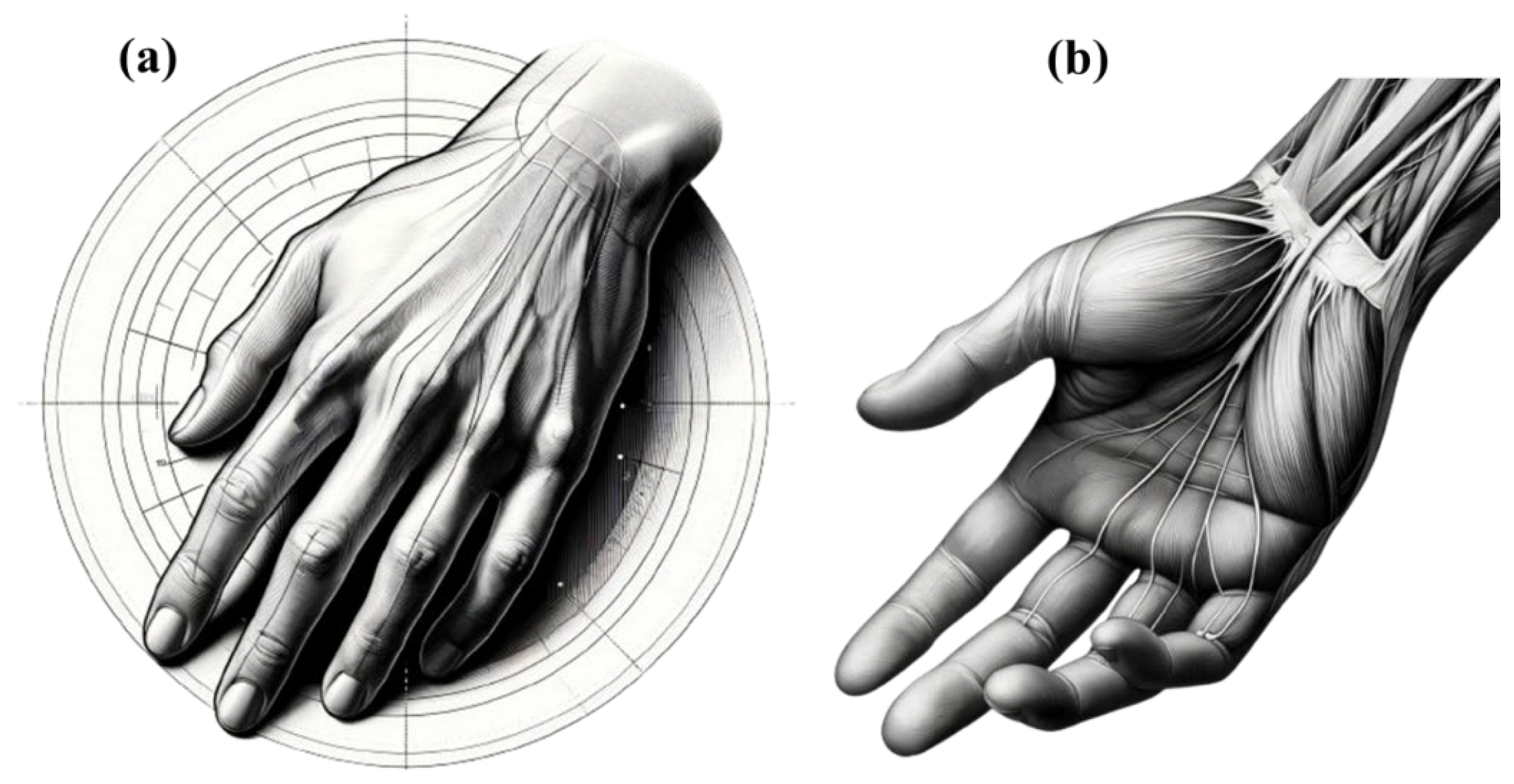
2. Biomechanical and Anatomical Considerations of Fingers and Thumb
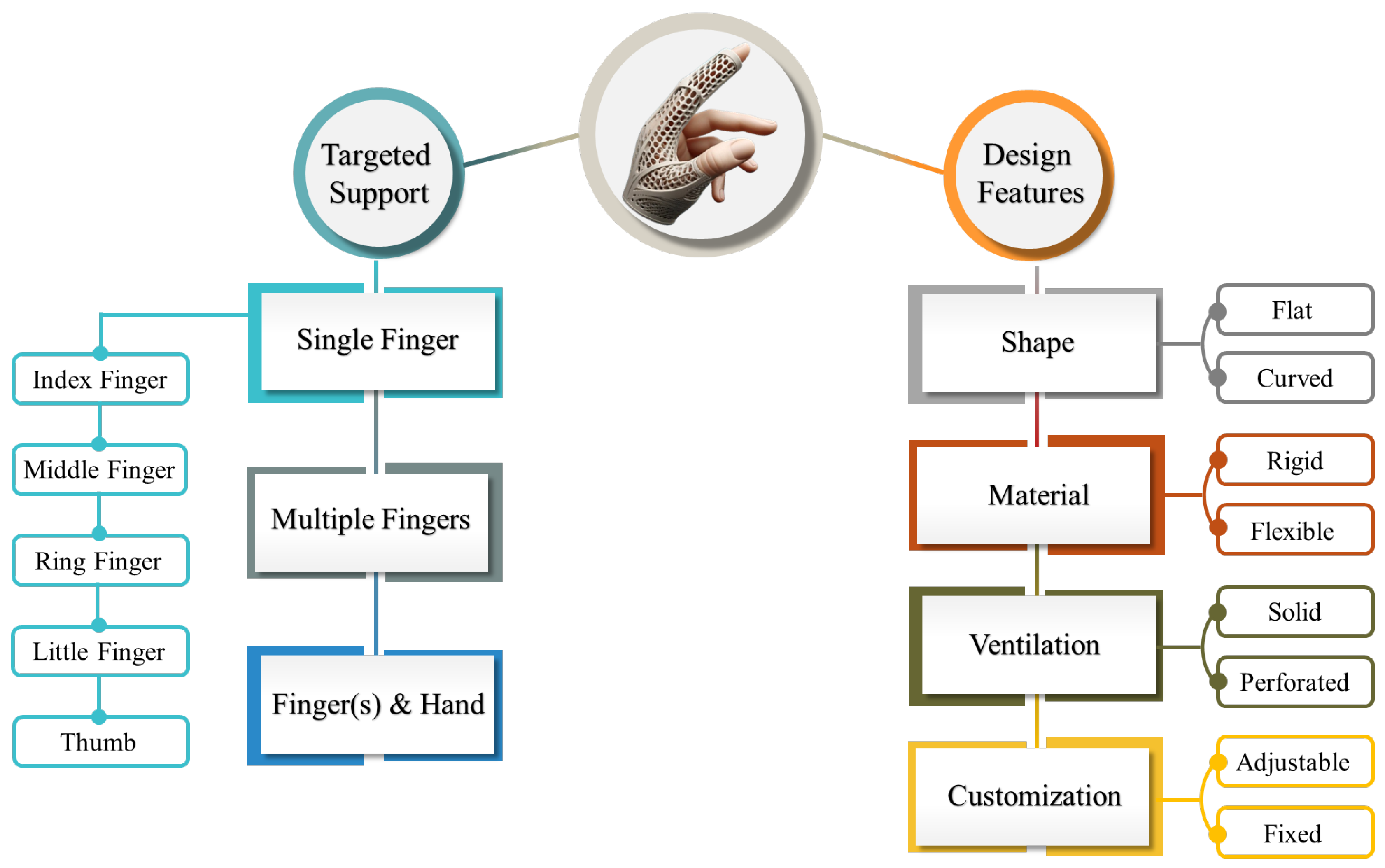
3. Finger Orthosis Classifications and Types
4. Ergonomic and Functional Design Factors
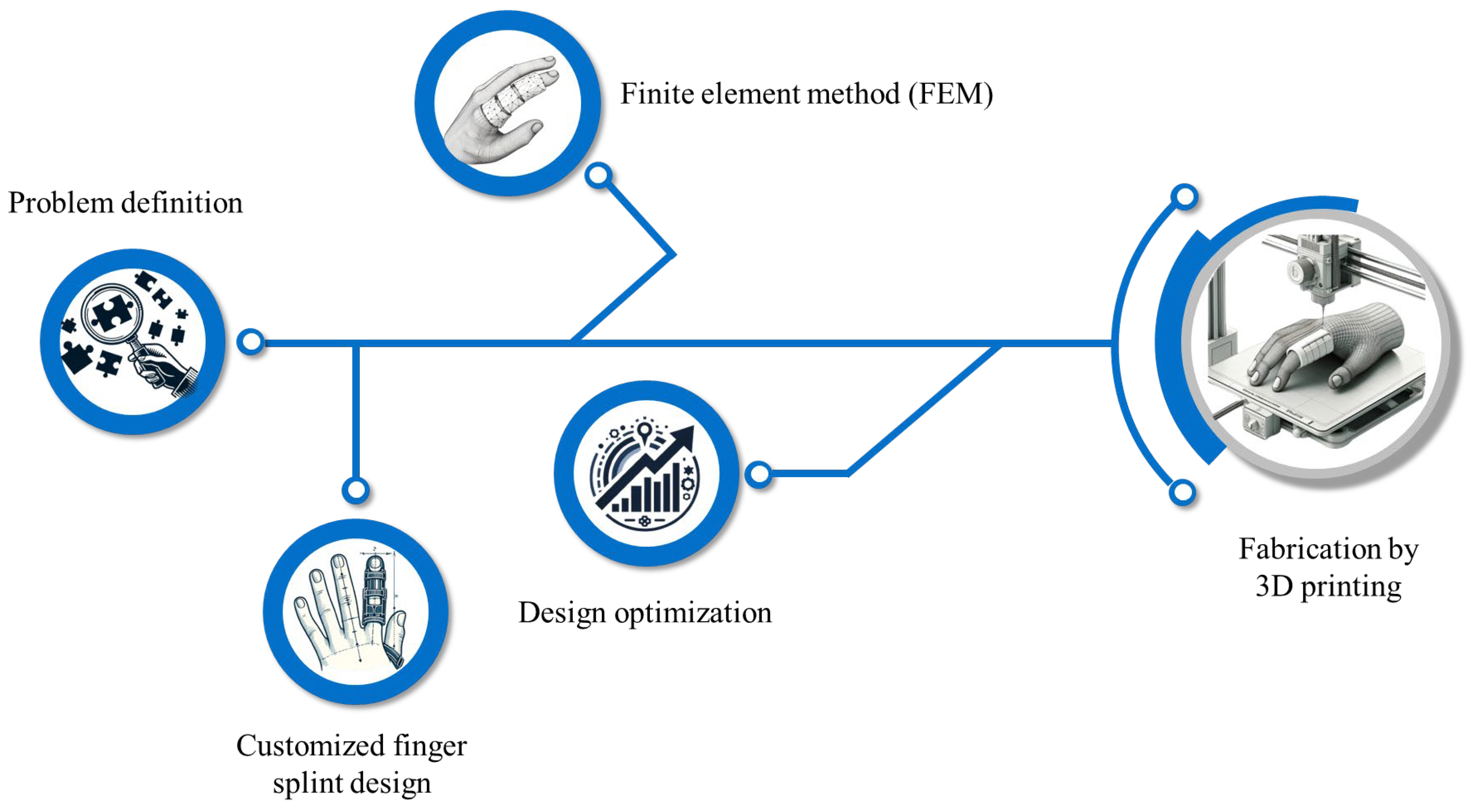
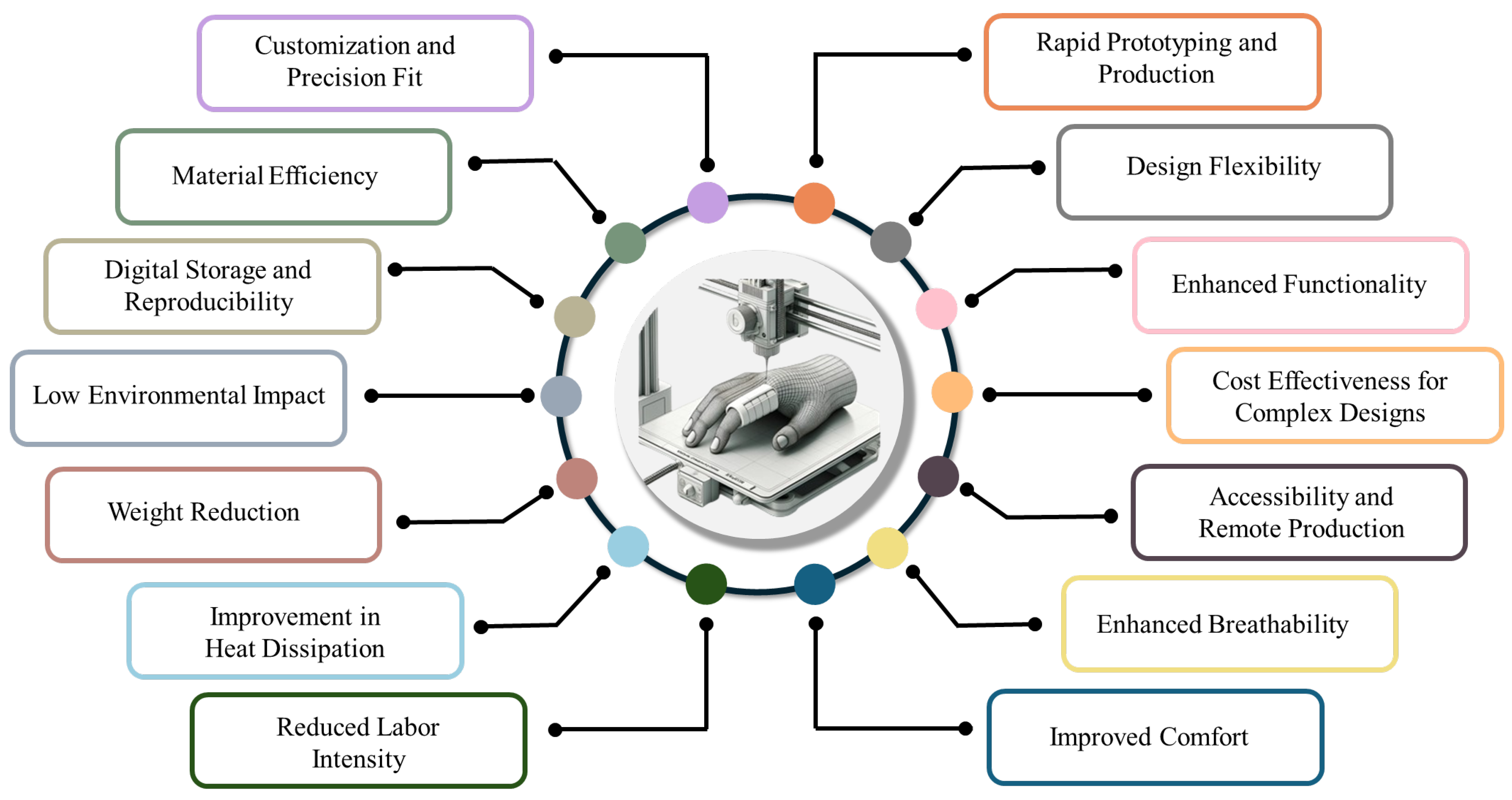
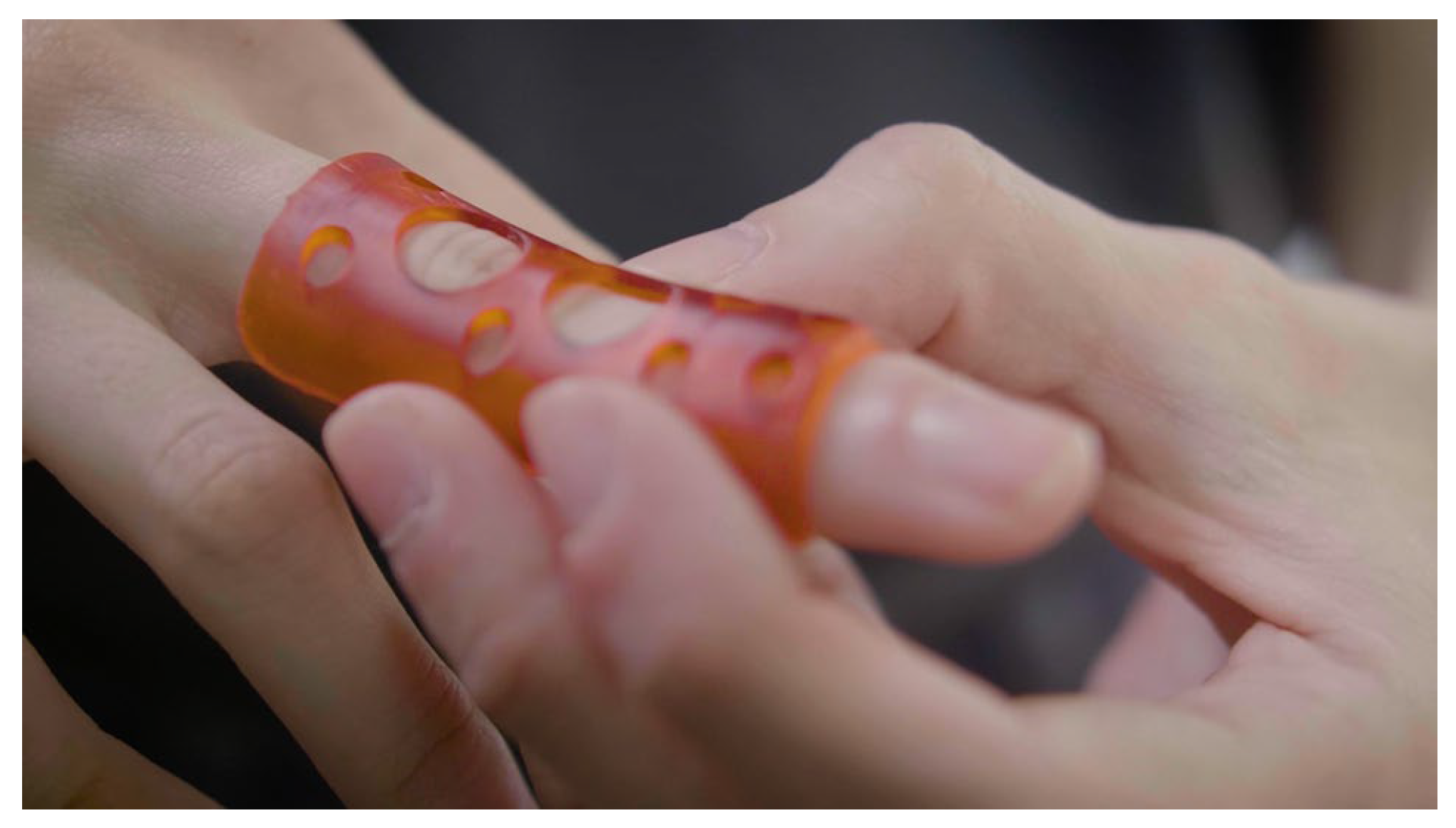
5. Additive Manufacturing of Finger and Thumb Orthoses
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kelly, B.M.; Patel, A.T.; Dodge, C. Upper limb orthotic devices. In Braddom’s Physical Medicine and Rehabilitation, 6th ed.; Cifu, D.X., Ed.; Elsevier: Amsterdam, The Netherlands, 2021; pp. 209–228. [Google Scholar]
- Graziosi, F.; Bonfiglioli, R.; Decataldo, F.; Violante, F.S. Criteria for Assessing Exposure to Biomechanical Risk Factors: A Research-to-Practice Guide—Part 2: Upper Limbs. Life 2025, 15, 109. [Google Scholar] [CrossRef] [PubMed]
- Nambiema, A.; Bertrais, S.; Bodin, J.; Fouquet, N.; Aublet-Cuvelier, A.; Evanoff, B.; Descatha, A.; Roquelaure, Y. Proportion of upper extremity musculoskeletal disorders attributable to personal and occupational factors: Results from the French Pays de la Loire study. BMC Public Health 2020, 20, 456. [Google Scholar] [CrossRef] [PubMed]
- Mattila, R.; Malmivaara, A.; Kastarinen, M.; Kivelä, S.-L.; Nissinen, A. Effects of lifestyle intervention on neck, shoulder, elbow and wrist symptoms. Scand. J. Work Environ. Health 2004, 30, 191–198. [Google Scholar] [CrossRef]
- Driscoll, B.; Leshuk, B. Orthoses for the Upper Extremity. In Prosthetics and Orthotics for Physical Therapists; Routledge: London, UK, 2025; pp. 235–252. [Google Scholar]
- Spaulding, S.E.; Yamane, A.; McDonald, C.L.; Spaulding, S.A. A conceptual framework for orthotic and prosthetic education. Prosthet. Orthot. Int. 2019, 43, 369–381. [Google Scholar] [CrossRef]
- Kringstad, O.; Dahlin, L.B.; Rosberg, H.E. Hand injuries in an older population—A retrospective cohort study from a single hand surgery centre. BMC Musculoskelet. Disord. 2019, 20, 245. [Google Scholar] [CrossRef]
- Moellhoff, N.; Throner, V.; Frank, K.; Benne, A.; Coenen, M.; Giunta, R.E.; Haas-Lützenberger, E.M. Epidemiology of hand injuries that presented to a tertiary care facility in Germany: A study including 435 patients. Arch. Orthop. Trauma Surg. 2023, 143, 1715–1724. [Google Scholar] [CrossRef] [PubMed]
- Rettig, A.C. Athletic injuries of the wrist and hand. Part I: Traumatic injuries of the wrist. Am. J. Sports Med. 2003, 31, 1038–1048. [Google Scholar] [CrossRef]
- Avery, D.M.; Rodner, C.M.; Edgar, C.M. Sports-related wrist and hand injuries: A review. J. Orthop. Surg. Res. 2016, 11, 99. [Google Scholar] [CrossRef]
- Kamath, J.B.; Naik, D.M.; Bansal, A. Current concepts in managing fractures of metacarpal and phalangess. Indian J. Plast. Surg. 2011, 44, 203–211. [Google Scholar] [CrossRef]
- Solaiman, R.H.; Irfanullah, E.; Navarro, S.M.; Keil, E.J.; Onizuka, N.; Tompkins, M.A.; Harmon, J.V. Rising incidence of stair-related upper extremity fractures among older adults in the United States: A 10-year nationwide analysis. Osteoporos. Int. 2023, 34, 1241–1248. [Google Scholar] [CrossRef]
- Iitsuka, T.; Kurumadani, H.; Inagaki, Y.; Ota, H. Recovery in the symmetry of hand use after distal radius fracture. Hand Ther. 2025, 30, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Restrepo, R.; Cervantes, L.F.; Zahrah, D.; Schoenleber, S.; Lee, E.Y. Pediatric Musculoskeletal Trauma: Upper Limb. Semin. Musculoskelet. Radiol. 2021, 25, 105–122. [Google Scholar] [CrossRef] [PubMed]
- Papamichail, P.; Sagredaki, M.L.; Bouzineki, C.; Kanellopoulou, S.; Lyros, E.; Christakou, A. The Effectiveness of an Exercise Program on Muscle Strength and Range of Motion on Upper Limbs, Functional Ability and Depression at Early Stage of Dementia. J. Clin. Med. 2024, 13, 4136. [Google Scholar] [CrossRef] [PubMed]
- Hofmeister, C.E.P.; Hanna, L.K.H.; Kroonen, L.L.T. Upper extremity nerve injuries. In Combat Orthopedic Surgery; CRC Press: Boca Raton, FL, USA, 2024; pp. 137–146. [Google Scholar]
- Hannah, S.D.; Hudak, P.L. Splinting and radial nerve palsy: A single-subject experiment. J. Hand Ther. 2001, 14, 195–201. [Google Scholar] [CrossRef]
- Boccolari, P.; Tedeschi, R.; Donati, D. Progression and clinical implications of boutonniere deformity. J. Musculoskelet. Surg. Res. 2024, 8, 1–2. [Google Scholar] [CrossRef]
- Carlson, E.J.; Carlson, M.G. Treatment of swan neck deformity in cerebral palsy. J. Hand Surg. 2014, 39, 768–772. [Google Scholar] [CrossRef]
- Tarbhai, K.; Hannah, S.; von Schroeder, H.P. Trigger finger treatment: A comparison of 2 splint designs. J. Hand Surg. 2012, 37, 243–249.e241. [Google Scholar] [CrossRef]
- Ryzewicz, M.; Wolf, J.M. Trigger digits: Principles, management, and complications. J. Hand Surg. 2006, 31, 135–146. [Google Scholar] [CrossRef]
- Walker-McCarter, F.; Fine, J. Mallet Finger and Jersey Finger. In Musculoskeletal Sports and Spine Disorders: A Comprehensive Guide; Springer: Chan, Switzerland, 2017; pp. 149–152. [Google Scholar]
- Buonomo, L.J.; Klein, J.S.; Keiper, T.L. Orthotic devices: Custom-made, prefabricated, and material selection. Foot Ankle Clin. 2001, 6, 249–252. [Google Scholar] [CrossRef]
- Patel, P.; Gohil, P. Custom orthotics development process based on additive manufacturing. Mater. Today Proc. 2022, 59, A52–A63. [Google Scholar] [CrossRef]
- Voulgaris, S.; Kousiatza, C.; Kazakis, G.; Ypsilantis, K.-I.; Galanis, D.; Mitropoulou, C.C.; Gkara, M.; Georgantzinos, S.K.; Soultanis, K.; Lagaros, N.D. Upper Limb Orthoses: Integrating Topology Optimization and 3D Printing for Custom Fit and Function. Appl. Sci. 2025, 15, 827. [Google Scholar] [CrossRef]
- Gehner, A.; Lunsford, D. Additive manufacturing and upper-limb orthoses: A scoping review. J. Prosthet. Orthot. 2024, 36, e25–e34. [Google Scholar] [CrossRef]
- Nouri, A.; Wang, L.; Li, Y.; Wen, C. Materials and Manufacturing for Ankle–Foot Orthoses: A Review. Adv. Eng. Mater. 2023, 25, 2300238. [Google Scholar] [CrossRef]
- Leggit, J.C.; Meko, C.J. Acute finger injuries: Part I. Tendons and ligaments. Am. Fam. Physician 2006, 73, 810–816. [Google Scholar]
- Zhao, K.D.; Robinson, C.A.; Hilliard, M.J. Biomechanics of the Upper Limb. In Atlas of Orthoses and Assistive Devices; Elsevier: Amsterdam, The Netherlands, 2019; pp. 127–133.e122. [Google Scholar]
- Wei, F.-C.; Chen, H.-C.; Chuang, C.-C.; Noordhoff, M.S. Simultaneous multiple toe transfers in hand reconstruction. Plast. Reconstr. Surg. 1988, 81, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Ellis, P.R.; Tsai, T.-M. Management of the traumatized joint of the finger. Clin. Plast. Surg. 1989, 16, 457–473. [Google Scholar] [CrossRef]
- Blazar, P.E.; Steinberg, D.R. Fractures of the proximal interphalangeal joint. J. Am. Acad. Orthop. Surg. 2000, 8, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Hogan, C.J.; Nunley, J.A. Posttraumatic proximal interphalangeal joint flexion contractures. J. Am. Acad. Orthop. Surg. 2006, 14, 524–533. [Google Scholar] [CrossRef]
- Young, N.; Terrington, N.; Francis, D.; Robinson, L.S. Orthotic management of fixed flexion deformity of the proximal interphalangeal joint following traumatic injury: A systematic review. Hong Kong J. Occup. Ther. 2018, 31, 3–13. [Google Scholar] [CrossRef]
- Littler, J.; Herndon, J.; Thompson, J. Examination of the hand. Reconstr. Plast. Surg. 1977, 6, 2973. [Google Scholar]
- Dahlin, L.B.; Wiberg, M. Nerve injuries of the upper extremity and hand. EFORT Open Rev. 2017, 2, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.M.; Zatsiorsky, V.M.; Latash, M.L. Contribution of the extrinsic and intrinsic hand muscles to the moments in finger joints. Clin. Biomech. 2000, 15, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Raut, S.; Johnson, R. Acute nerve injuries in the hand: Common patterns and treatment strategies. Orthop. Trauma 2023, 37, 111–117. [Google Scholar] [CrossRef]
- Hosny, H. Peripheral Nerve and Hand Examination. In Clinical Surgical Skills Made Easy; Farag, A., Mansour, E.A., Winter, D.C., Eds.; Springer Nature: Cham, Switzerland, 2024; pp. 271–279. [Google Scholar]
- Duncan, C.C.; Edgley, S.R. Upper Limb Orthoses for the Stroke-and Brain-Injured Patient. In Atlas of Orthoses and Assistive Devices; Elsevier: Amsterdam, The Netherlands, 2019; pp. 146–156.e142. [Google Scholar]
- Sarı, M.I.; Şahin, I.; Gökçe, H.; Öksüz, C. Ring orthosis design and production by rapid prototyping approach. J. Hand Ther. 2020, 33, 170–173. [Google Scholar] [CrossRef]
- Howell, J. Principles and components of upper limb orthoses. In Atlas of Orthoses and Assistive Devices; Elsevier: Amsterdam, The Netherlands, 2019; pp. 134–145.e131. [Google Scholar]
- Macionis, V. A local adhesive finger splint. J. Hand Surg. 2001, 26, 962–964. [Google Scholar] [CrossRef]
- Cooper, C. Fundamentals of Hand Therapy: Clinical Reasoning and Treatment Guidelines for Common Diagnoses, 3rd ed.; Elsevier Mosby: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Habib, A.E.S.E.; Atiyya, A.N.; Aly, A.M. Conservative versus surgical treatment in management of closed mallet finger: A systematic review and metaanalysis. QJM Int. J. Med. 2021, 114, hcab104. [Google Scholar] [CrossRef]
- Cronin, U.M.; O’Sullivan, A.; Sheerin, M.; O’Sullivan, K.J.; Cummins, N.M.; Ryan, D.; O’Sullivan, L.W. Evaluating the clinical benefit and acceptance of a bespoke 3D-printed splint for the treatment of mallet finger injury: A pilot study in a cohort of patients. Int. J. Bioprinting 2024, 10, 518–530. [Google Scholar] [CrossRef]
- Borchers, J.R.; Best, T.M. Common finger fractures and dislocations. Am. Fam. Physician 2012, 85, 805–810. [Google Scholar]
- West-Frasier, J.M.; Vennix, C.L. Basic Splinting. In Ryan’s Occupational Therapy Assistant; Routledge: London, UK, 2024; pp. 484–495. [Google Scholar]
- Güven, E.; Suner-Keklik, S. Custom-made finger splint versus prefabricated finger splint: Finger flexion stabilization. Rev. Assoc. Med. Bras. 2022, 68, 935–938. [Google Scholar] [CrossRef]
- Paternostro-Sluga, T.; Stieger, M. Hand splints in rehabilitation. Crit. Rev. Phys. Rehabil. Med. 2004, 16, 10. [Google Scholar] [CrossRef]
- Wong, S.K. Classification of hand splinting. Hand Surg. 2002, 7, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Larson, D.; Jerosch-Herold, C. Clinical effectiveness of post-operative splinting after surgical release of Dupuytren’s contracture: A systematic review. BMC Musculoskelet. Disord. 2008, 9, 104. [Google Scholar] [CrossRef] [PubMed]
- Shank, T.M.; Cericola, C. Upper Extremity Orthotics for Children and Youth with Cerebral Palsy. In Cerebral Palsy; Miller, F., Bachrach, S., Lennon, N., O’Neil, M.E., Eds.; Springer: Cham, Switzerland, 2020; pp. 3023–3039. [Google Scholar]
- Chhikara, K.; Gupta, S.; Saharawat, S.; Sarkar, S.; Chanda, A. Design, manufacturing, and trial of a 3D printed customized finger splint for patients with rheumatoid arthritis. Rheumato 2023, 3, 51–62. [Google Scholar] [CrossRef]
- Papavasiliou, T.; Shah, R.K.; Chatzimichail, S.; Uppal, L.; Chan, J.C. Three-dimensional printed customized adjustable mallet finger splint: A cheap, effective, and comfortable alternative. Plast. Reconstr. Surg.–Glob. Open 2021, 9, e3500. [Google Scholar] [CrossRef]
- Chanda, A.; Mukherjee, B.; Chatterjee, S. Advances in Orthotic Prosthetic Design: Challenges and Applications. In Materials for Biomedical Simulation: Design, Development and Characterization; Chanda, A., Sidhu, S.S., Singh, G., Eds.; Springer: Singapore, 2023; pp. 37–58. [Google Scholar]
- Chien, W.C.; Tsai, T.F. Pressure and Skin: A Review of Disease Entities Driven or Influenced by Mechanical Pressure. Am. J. Clin. Dermatol. 2024, 25, 261–280. [Google Scholar] [CrossRef]
- Kelly, B.M.; Berenz, T.; Williams, T. Orthoses for the burned hand. In Atlas of Orthoses and Assistive Devices; Elsevier: Amsterdam, The Netherlands, 2019; pp. 170–175.e171. [Google Scholar]
- Quinlan, C.S.; Hevican, C.; Kelly, J.L. A useful dressing for isolated digit injuries. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 999–1000. [Google Scholar] [CrossRef]
- Cooper, C.; Deshaies, L. Orthotics for the fingers. In Introduction to Orthotics, 4th ed.; Coppard, B., Lohman, H., Eds.; Elsevier: Amsterdam, The Netherlands, 2015; pp. 247–268. [Google Scholar]
- Arulmozhi, R.S.; Vaidya, M.; Poojalakshmi, M.; Ashok Kumar, D.; Anuraag, K. 3D design and printing of custom-fit finger splint. Biomed. Eng. Appl. Basis Commun. 2018, 30, 1850032. [Google Scholar] [CrossRef]
- Mian, S.H.; Umer, U.; Moiduddin, K.; Alkhalefah, H. Finite element analysis of upper limb splint designs and materials for 3D printing. Polymers 2023, 15, 2993. [Google Scholar] [CrossRef]
- Malloum, A.H.; Fozi, M.A.A.; Zain, M.Z.M.; Jaafar, M.H.M.; Deros, M.A. Polyvinyl Alcohol (PVA) Hydrophilic Behaviour of Porosity Condition for 3DPrinted Medical Splinting Devices. J. Eng. Sci. Res. 2023, 7, 12–19. [Google Scholar] [CrossRef]
- Bhathena, H.M. A simple, innovative method of securing burn dressings. Plast. Reconstr. Surg. 2003, 112, 357. [Google Scholar] [CrossRef]
- Bond, M.C.; Abraham, M.K. Immobilization and splinting. In Orthopedic Emergencies: Expert Management for the Emergency Physician; Bond, M.C., Perron, A.D., Abraham, M.K., Eds.; Cambridge University Press: Cambridge, UK, 2013; pp. 248–269. [Google Scholar]
- O’Brien, L. Adherence to therapeutic splint wear in adults with acute upper limb injuries: A systematic review. Hand Ther. 2010, 15, 3–12. [Google Scholar] [CrossRef]
- Glazer, C.; Oravitan, M.; Pantea, C.; Stanila, A.M.; Jurjiu, N.-A.; Totok, A.; Marghitas, M.P.; Avram, C. 3D-printed orthoses vs. traditional plaster cast: A comparative clinical study. Balneo PRM Res. J. 2025, 16, 785. [Google Scholar] [CrossRef]
- Hachoumi, N.; Laabidi, R.; Eddabbah, M. The Use of 3D Additive Technology in the Conception of Upper Extremity Orthotics: Advances, Applications, and Perspectives. In Advanced Nursing Practices for Clinical Excellence; Amane, M., Boussaa, S., Eds.; IGI Global: Hershey, PA, USA, 2025; pp. 223–236. [Google Scholar]
- Choi, H.; Seo, A.; Lee, J. Mallet finger lattice casts using 3D printing. J. Healthc. Eng. 2019, 2019, 4765043. [Google Scholar] [CrossRef] [PubMed]
- Portnoy, S.; Barmin, N.; Elimelech, M.; Assaly, B.; Oren, S.; Shanan, R.; Levanon, Y. Automated 3D-printed finger orthosis versus manual orthosis preparation by occupational therapy students: Preparation time, product weight, and user satisfaction. J. Hand Ther. 2020, 33, 174–179. [Google Scholar] [CrossRef]
- Cıftcı, F.; Hacıoglu, A.; Yesil, T.B.; Ustundag, C.B. DESIGNED AND 3D PRINTED PLA BASED UPPER EXTREMITY FINGER ORTHOSIS. Mühendislik Bilim. Ve Tasarım Derg. 2018, 6, 460–463. [Google Scholar] [CrossRef][Green Version]
- Gupta, A.; Chaturvedi, S.; Bhat, A.K.; Samheel, M. Design and manufacture of customizable finger immobilizer and mallet finger splints. In Proceedings of the 2019 International Conference on Biomedical Innovations and Applications (BIA), Varna, Bulgaria, 8–9 November 2019; pp. 1–4. [Google Scholar]
- Kadioglu, E.; Aydin, H.E.; Kaya, I.; Aydin, N.; Sahin, M.C. Manufacturing and application of personal hand and finger splint with three dimensional printer technology following hand and finger trauma. Ann. Med. Res. 2019, 26, 1474–1477. [Google Scholar] [CrossRef]
- Chen, Y.-J.; Lin, H.; Zhang, X.; Huang, W.; Shi, L.; Wang, D. Application of 3D–printed and patient-specific cast for the treatment of distal radius fractures: Initial experience. 3D Print. Med. 2017, 3, 11. [Google Scholar] [CrossRef]
- Irani, N.; Ozelie, R. Satisfaction with Customizable 3D-Printed Finger Orthoses Compared to Commercial SilverRing™ Splints. Open J. Occup. Ther. 2023, 11, 1–9. [Google Scholar] [CrossRef]
- O’Brien, V.H.; Thurn, J. A simple distal radioulnar joint orthosis. J. Hand Ther. 2013, 26, 287–290. [Google Scholar] [CrossRef]
- Kunkel, M.E.; Araújo, A.C.C.P.S. Narrative Review on the Application of Additive Manufacturing in the Production of Upper Limb Orthoses. In Current Trends in Biomedical Engineering; Lombello, C.B., da Ana, P.A., Eds.; Springer: Cham, Switzerland, 2023; pp. 61–77. [Google Scholar]
- Chen, Y.; Lin, H.; Yu, Q.; Zhang, X.; Wang, D.; Shi, L.; Huang, W.; Zhong, S. Application of 3D-Printed Orthopedic Cast for the Treatment of Forearm Fractures: Finite Element Analysis and Comparative Clinical Assessment. BioMed Res. Int. 2020, 2020, 9569530. [Google Scholar] [CrossRef]
- Karaki, A.; Hammoud, A.; Masad, E.; Khraisheh, M.; Abdala, A.A.; Ouederni, M. A review on material extrusion (MEX) of polyethylene-challenges, opportunities, and future prospects. Polymer 2024, 307, 127333. [Google Scholar] [CrossRef]
- Karaki, A.; Masad, E.; Khraisheh, M.; Ouederni, M. Fused deposition modeling of polyethylene (PE): Printability assessment for low-density polyethylene and polystyrene blends. Compos. Part C Open Access 2024, 15, 100499. [Google Scholar] [CrossRef]
- Bachhar, N.; Gudadhe, A.; Kumar, A.; Andrade, P.; Kumaraswamy, G. 3D printing of semicrystalline polypropylene: Towards eliminating warpage of printed objects. Bull. Mater. Sci. 2020, 43, 171. [Google Scholar] [CrossRef]
- Bahar, A.; Belhabib, S.; Guessasma, S.; Benmahiddine, F.; Hamami, A.E.A.; Belarbi, R. Mechanical and thermal properties of 3D printed polycarbonate. Energies 2022, 15, 3686. [Google Scholar] [CrossRef]
- Vidakis, N.; Petousis, M.; Kechagias, J. A comprehensive investigation of the 3D printing parameters’ effects on the mechanical response of polycarbonate in fused filament fabrication. Prog. Addit. Manuf. 2022, 7, 713–722. [Google Scholar] [CrossRef]
- Zaborovskii, N.; Masevnin, S.; Smekalenkov, O.; Murakhovsky, V.; Ptashnikov, D. Patient-specific 3D-Printed PEEK implants for spinal tumor surgery. J. Orthop. 2025, 62, 99–105. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Alghauli, M.A.; Algabri, R.S.; Hamadallah, H.H.; Aboalrejal, A.N.; Zafar, M.S.; Fareed, M.A. Applications, modifications, and manufacturing of polyetheretherketone (PEEK) in dental implantology: A comprehensive critical review. Int. Mater. Rev. 2025, 70, 103–136. [Google Scholar] [CrossRef]
- Zhu, Y.; Guo, S.; Ravichandran, D.; Ramanathan, A.; Sobczak, M.T.; Sacco, A.F.; Patil, D.; Thummalapalli, S.V.; Pulido, T.V.; Lancaster, J.N. 3D-Printed Polymeric Biomaterials for Health Applications. Adv. Healthc. Mater. 2025, 14, 2402571. [Google Scholar] [CrossRef]
- Aziz, M.M.; Beard, L.; Ali, S.; Eltaggaz, A.; Deiab, I. Optimization Scheme for 3D Printing of PLA–PHBV–PCL Biodegradable Blends for Use in Orthopedic Casting. Polymers 2025, 17, 852. [Google Scholar] [CrossRef]
- Prem Kumar, C.; Sivanagaraju, N.; Loknath, D.; Mallikarjun Rao, G.N.; Vakkalagadda, M. Shape Memory Polymers, Blends, and Composites: Processing, Properties, and Applications. Polymer 2025, 64, 1253–1281. [Google Scholar] [CrossRef]
- Luo, L.; Zhang, F.; Wang, L.; Liu, Y.; Leng, J. Recent advances in shape memory polymers: Multifunctional materials, multiscale structures, and applications. Adv. Funct. Mater. 2024, 34, 2312036. [Google Scholar] [CrossRef]
- Barmouz, M.; Uribe, L.V.; Ai, Q.; Azarhoushang, B. Design and fabrication of a novel 4D-printed customized hand orthosis to treat cerebral palsy. Med. Eng. Phys. 2024, 123, 104087. [Google Scholar] [CrossRef]
- Reese, J.; Seo, J.H.; Srinavasa, A. Orthorigami: Implementing Shape-Memory Polymers for Customizing Orthotic Applications. In Proceedings of the Fourteenth International Conference on Tangible, Embedded, and Embodied Interaction, Sydney, NSW, Australia, 9–12 February 2020; pp. 123–130. [Google Scholar]
- Kumar, A.; Chhabra, D. Multidisciplinary topology and material optimization approach for developing patient-specific limb orthosis using 3D printing. Rapid Prototyp. J. 2023, 29, 1757–1771. [Google Scholar] [CrossRef]
- Pal, A.K.; Mohanty, A.K.; Misra, M. Additive manufacturing technology of polymeric materials for customized products: Recent developments and future prospective. RSC Adv. 2021, 11, 36398–36438. [Google Scholar] [CrossRef] [PubMed]
- Patterson, R.M.; Salatin, B.; Janson, R.; Salinas, S.P.; Mullins, M.J.S. A current snapshot of the state of 3D printing in hand rehabilitation. J. Hand Ther. 2020, 33, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Emzain, Z.F.; Amrullah, U.S.; Mufarrih, A.; Qosim, N.; Herlambang, Y.D. Design optimization of sleeve finger splint model using Finite Element Analysis. J. Polimesin 2021, 19, 147–152. [Google Scholar]
- Zolfagharian, A.; Gregory, T.M.; Bodaghi, M.; Gharaie, S.; Fay, P. Patient-specific 3D-printed splint for mallet finger injury. Int. J. Bioprinting 2020, 6, 16–28. [Google Scholar] [CrossRef]
- Nouri, A.; Rohani Shirvan, A.; Li, Y.; Wen, C. Additive manufacturing of metallic and polymeric load-bearing biomaterials using laser powder bed fusion: A review. J. Mater. Sci. Technol. 2021, 94, 196–215. [Google Scholar] [CrossRef]
- Bansal, S.; Tripathi, A.; Kumar, N.; Singh, T.; Ranganath, M. Modeling and Analysis of Finger Splint for Mild to High-Grade Mallet Finger Fracture. Evergreen 2023, 10, 1074–1079. [Google Scholar] [CrossRef]
- Mohammed, M.I.; Fay, P. Design and additive manufacturing of a patient specific polymer thumb splint concept. In Proceedings of the Solid Freeform Fabrication 2018, the 29th Annual International Solid Freeform Fabrication Symposium, Austin, TX, USA, 13–15 August 2018; pp. 873–886. [Google Scholar]
- Nam, H.S.; Seo, C.H.; Joo, S.Y.; Kim, D.H.; Park, D.S. The application of three-dimensional printed finger splints for post hand burn patients: A case series investigation. Ann. Rehabil. Med. 2018, 42, 634–638. [Google Scholar] [CrossRef]
- Nasseri, S.; Castellano, V.K.; Ong, T.; DeDiego, A.; Naseri, N. Design, simulation and fabrication of a new finger support. Int. J. Curr. Eng. Technol. 2018, 8, 954–962. [Google Scholar] [CrossRef]
- Poier, P.H.; Weigert, M.C.; Rosenmann, G.C.; de Carvalho, M.G.R.; Ulbricht, L.; Foggiatto, J.A. The development of low-cost wrist, hand, and finger orthosis for children with cerebral palsy using additive manufacturing. Res. Biomed. Eng. 2021, 37, 445–453. [Google Scholar] [CrossRef]
- Shine, K.M.; Schlegel, L.; Ho, M.; Boyd, K.; Pugliese, R. From the ground up: Understanding the developing infrastructure and resources of 3D printing facilities in hospital-based settings. 3D Print. Med. 2022, 8, 21. [Google Scholar] [CrossRef]
- Blaya, F.; Pedro, P.S.; Silva, J.L.; D’Amato, R.; Heras, E.S.; Juanes, J.A. Design of an orthopedic product by using additive manufacturing technology: The arm splint. J. Med. Syst. 2018, 42, 54. [Google Scholar] [CrossRef]
- Kothavade, P.; Kafi, A.; Dekiwadia, C.; Kumar, V.; Sukumaran, S.B.; Shanmuganathan, K.; Bateman, S. Extrusion 3D Printing of Intrinsically Fluorescent Thermoplastic Polyimide: Revealing an Undisclosed Potential. Polymers 2024, 16, 2798. [Google Scholar] [CrossRef] [PubMed]
- Guamán-Rivera, R.; Martínez-Rocamora, A.; García-Alvarado, R.; Muñoz-Sanguinetti, C.; González-Böhme, L.F.; Auat-Cheein, F. Recent Developments and Challenges of 3D-Printed Construction: A Review of Research Fronts. Buildings 2022, 12, 229. [Google Scholar] [CrossRef]
- Yang, T.H.; Lu, S.C.; Lin, W.J.; Zhao, K.; Zhao, C.; An, K.N.; Jou, I.M.; Lee, P.Y.; Kuo, L.C.; Su, F.C. Assessing finger joint biomechanics by applying equal force to flexor tendons in vitro using a novel simultaneous approach. PLoS ONE 2016, 11, e0160301. [Google Scholar] [CrossRef]
- Matsunaga, F.; Kokubu, S.; Tortos Vinocour, P.E.; Ke, M.T.; Hsueh, Y.H.; Huang, S.Y.; Gomez-Tames, J.; Yu, W. Finger joint stiffness estimation with joint modular soft actuators for hand telerehabilitation. Robotics 2023, 12, 83. [Google Scholar] [CrossRef]



| Aspect | Mobilization Splints (Dynamic) | Immobilization Splints (Static) |
|---|---|---|
| Purpose | Support and protect with limited movement | Fully immobilize to prevent any movement |
| Use cases |
|
|
| Design characteristics |
|
|
| Patient compliance |
|
|
| Production cost |
|
|
| Manufacturing cycle |
|
|
| Examples |
|
|
| Benefits |
|
|
| Classification | Subcategory | Type of Splint | Examples |
|---|---|---|---|
| By functionality | Immobilization splints | Static finger splints | Stack splint; aluminum foam splint; buddy tape; ulnar gutter splint; ring splint; adhesive splint |
| Mobilization splints | Dynamic finger splints | Dynamic extension splint | |
| Static finger splints | Ring splint | ||
| Resting splints | Static finger splints | Static progressive splint; soft volar splint | |
| Correctional splints | Dynamic finger splints | Dynamic extension splint | |
| Static finger splints | Silver ring splint; ulnar deviation splint | ||
| By joint involvement | DIP joint splints | Stack splint; dip immobilizer | |
| PIP joint splints | Ring splint; gutter splint | ||
| MCP joint splints | MCP blocking splint; ulnar deviation splint | ||
| Thumb splints | Thumb spica splint; CMC splint | ||
| By material | Rigid splints | Aluminum foam splint; stack splint; ulnar gutter splint | |
| Soft splints | Buddy tape; soft volar splint | ||
| Custom-made splints | Custom thermoplastic splint; custom molded splint | ||
| By condition | Traumatic injuries | Gutter splint; mallet finger splint; ulnar gutter splint | |
| Chronic conditions | Silver ring splint; ring splint | ||
| Post-surgical splints | Dynamic extension splint, static progressive splint | ||
| By design | Prefabricated splints | Ring splint; silver ring splint | |
| Custom-made splints | Custom thermoplastic splint; custom molded splint |
| Material | Tensile Strength (MPa) | Elongation at Break (%) | Properties | Clinical Notes |
|---|---|---|---|---|
| PLA | 50–70 | 4–10 | Biodegradable, easy to print | Suitable for rigid splints, prototyping |
| ABS | 30–50 | 10–50 | Tough, slightly flexible | Better impact resistance than PLA |
| TPU | 50–80 | 200–600 | Elastic, shock-absorbing | Ideal for soft splints or inserts |
| PA11/PA12 | 40–60 | 250–400 | Durable, wear-resistant | Excellent for functional, long-term splints |
| PETG | 40–50 | 50–120 | Transparent, good strength | Improved heat dissipation |
| CF-Nylon | 60–110 | 1–15 | Reinforced, high strength | Lightweight and strong splints |
| PP | 30–40 | 100–600 | Lightweight, biocompatible | Limited use due to printing challenges |
| PE | 10–40 | 300–600 | Soft, flexible | Rarely used due to adhesion issues |
| PC | 55–75 | 100–150 | High strength, heat resistant | Requires controlled printing environment |
| PEEK | 90–110 | 40–50 | Implant-grade, high-temp | Rare in splints due to high cost and complexity |
| Objective | Method | Materials | Description | Ref. |
|---|---|---|---|---|
| To support and correct finger deformities due to RA | FDM | ABS; PLA | Custom-fit splints for RA finger deformities. They are lightweight, comfortable, and easy to clean. | [61] |
| To provide a patient-specific splint for mild to high-grade mallet finger fracture | ─ | PLA | Patient-specific splint with improved ergonomics, material efficiency, breathability, and hygiene. | [98] |
| To manage finger deformities caused by RA | FDM | PLA | A cost-effective, customized 3D-printed splint improving finger alignment, dexterity, and comfort, tested on 20 patients. | [54] |
| For conservative upper limb finger treatment | FDM | PLA | A custom 3D-printed PLA orthosis that is ergonomic, easy to clean, and supportive for finger deformities. | [71] |
| To rectify discomfort and improper fit caused by conventional splints for mallet finger injuries | SLA | Black resin | Custom 3D-printed splints for mallet finger, improving fit, comfort, and functionality with high patient satisfaction. | [46] |
| To address excess material, poor fit, and discomfort caused by conventional splints | FDM | ABS | An optimized conical sleeve splint, reducing mass by 42.18% while maintaining structural integrity. | [95] |
| To resolve discomfort, poor fit, and hygiene issues associated with conventional splints | FDM | PLA | Customizable 3D-printed PLA splints with better fit, comfort, functionality, and thermoformable adjustments. | [72] |
| To lower costs and improve customization, addressing poor fit in conventional orthoses | FDM | PLA | Comparison of 3D-printed orthoses to SilverRing™ showing similar fit, comfort, and esthetics with better affordability. | [75] |
| Hand and finger splint for trauma | FDM | PLA | Personalized splints for 25 patients showing full recovery, cost-effectiveness, improved comfort, no radiological artifacts, and easy return to daily activities. | [73] |
| Mallet finger splint for tendon injuries | FDM | PLA; PETG; ABS; CF-Nylon | Customized splints showing improved strength, weight reduction, comfort, and heat dissipation, ideal for mallet finger rehabilitation. | [92] |
| Porous finger splint | FDM | PLA; PVA | Breathable, comfortable splints with a 70/30 PLA/PVA ratio for increased porosity. | [63] |
| Thumb splint for musculoskeletal conditions | FDM | ABS | Customized splints offering better ergonomics, esthetics, comfort, and moisture release than traditional splints. | [99] |
| Finger splints for hand-burn patients | FDM | TPU; PLA | Customized, breathable, cost-effective splints that improve patient compliance and were easily adjustable. | [100] |
| Finger support | PolyJet | Rubber and elastomer | Flexible, resizable support for finger deformities, validated by FEA and testing for strength and reliability. | [101] |
| Mallet finger splint | FDM | PLA | Custom-fit, low-cost, radiolucent splints for mallet finger, offering ease of production, better fit, and improved compliance. | [55] |
| To minimize or prevent progress of deformities in children with cerebral palsy | FDM | PLA | Lightweight, esthetically pleasing orthoses developed through an 8-step process, using low-cost materials. | [102] |
| Swan neck deformity treatment | FDM | ABS | Software for patient-specific orthosis models for 3D printing, offering lighter, better-fitting, and more esthetic orthoses with higher satisfaction but longer preparation time. | [70] |
| Finger splint for mallet finger injury | FDM | PLA | Reducing mass and improving mechanical properties and heat dissipation, with the splint retaining 71.13% of its original mass performing best. | [96] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nouri, A.; Wang, L.; Bakhtiari, H.; Li, Y.; Wen, C. Finger Orthoses for Rehabilitation―Part I: Biomedical Insights and Additive Manufacturing Innovations. Prosthesis 2025, 7, 62. https://doi.org/10.3390/prosthesis7030062
Nouri A, Wang L, Bakhtiari H, Li Y, Wen C. Finger Orthoses for Rehabilitation―Part I: Biomedical Insights and Additive Manufacturing Innovations. Prosthesis. 2025; 7(3):62. https://doi.org/10.3390/prosthesis7030062
Chicago/Turabian StyleNouri, Alireza, Lijing Wang, Hamed Bakhtiari, Yuncang Li, and Cuie Wen. 2025. "Finger Orthoses for Rehabilitation―Part I: Biomedical Insights and Additive Manufacturing Innovations" Prosthesis 7, no. 3: 62. https://doi.org/10.3390/prosthesis7030062
APA StyleNouri, A., Wang, L., Bakhtiari, H., Li, Y., & Wen, C. (2025). Finger Orthoses for Rehabilitation―Part I: Biomedical Insights and Additive Manufacturing Innovations. Prosthesis, 7(3), 62. https://doi.org/10.3390/prosthesis7030062







