Clinical Efficacy of Anterior Ceramic Materials in Resin-Bonded Fixed Dental Prostheses with Different Bridge Designs—A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Information Sources
2.2. Search Strategy
2.3. Inclusion Criteria
- (1)
- Studies presenting clinical characteristics with quantitative outcomes, including survival rates, failure rates, debonding incidents, fractures, and other biological complications.
- (2)
- Articles of any study design, such as randomized controlled trials (RCTs) and observational studies.
- (3)
- Studies evaluating cantilever or fixed–fixed RBFDPs with sufficient clinical outcome data.
2.4. Exclusion Criteria
- (1)
- Animal studies, in vitro studies, case reports, case series, systematic reviews, and meta-analyses.
- (2)
- Studies lacking intervention with cantilever or fixed–fixed RBFDPs or providing insufficient details on clinical outcomes.
- (3)
- Articles reporting multiple publications on the same patient cohort or with a follow-up duration of less than two years.
2.5. Selection Process
2.6. Study Risk of Bias Assessment
2.7. Statistical Analysis
2.8. Sensitivity and Subgroup Analysis
3. Results
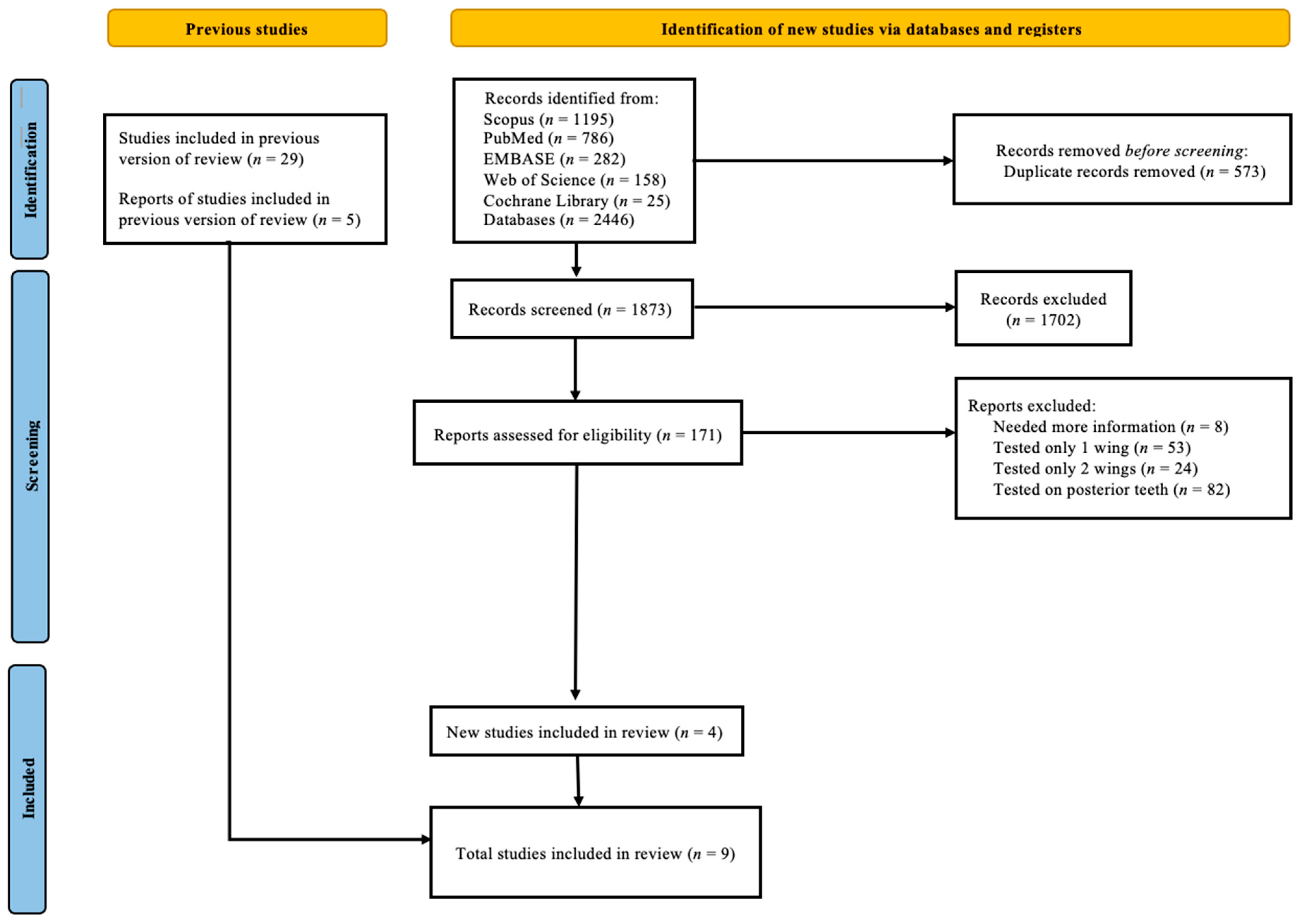
3.1. Search Results and Characteristics of Studies Included
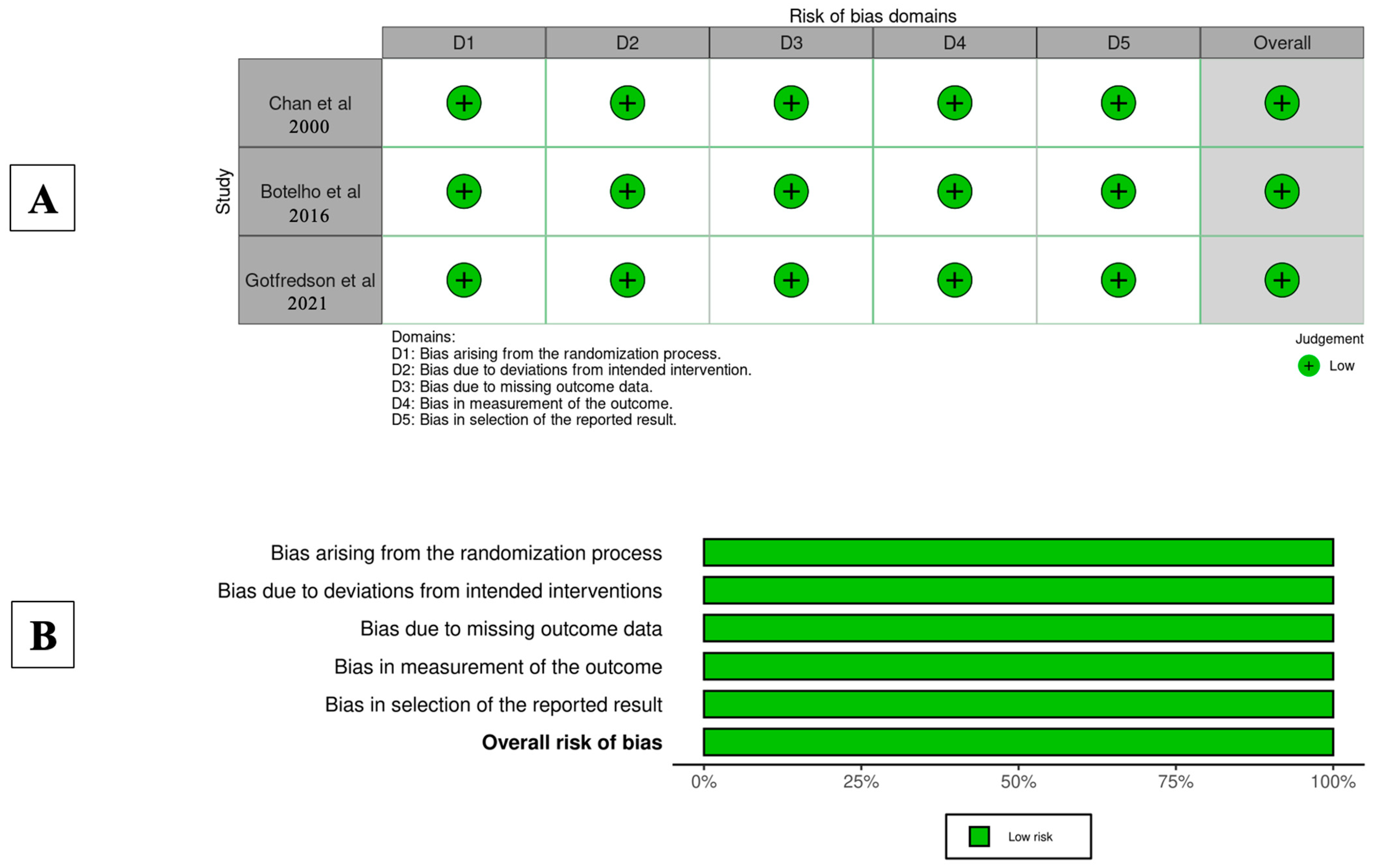
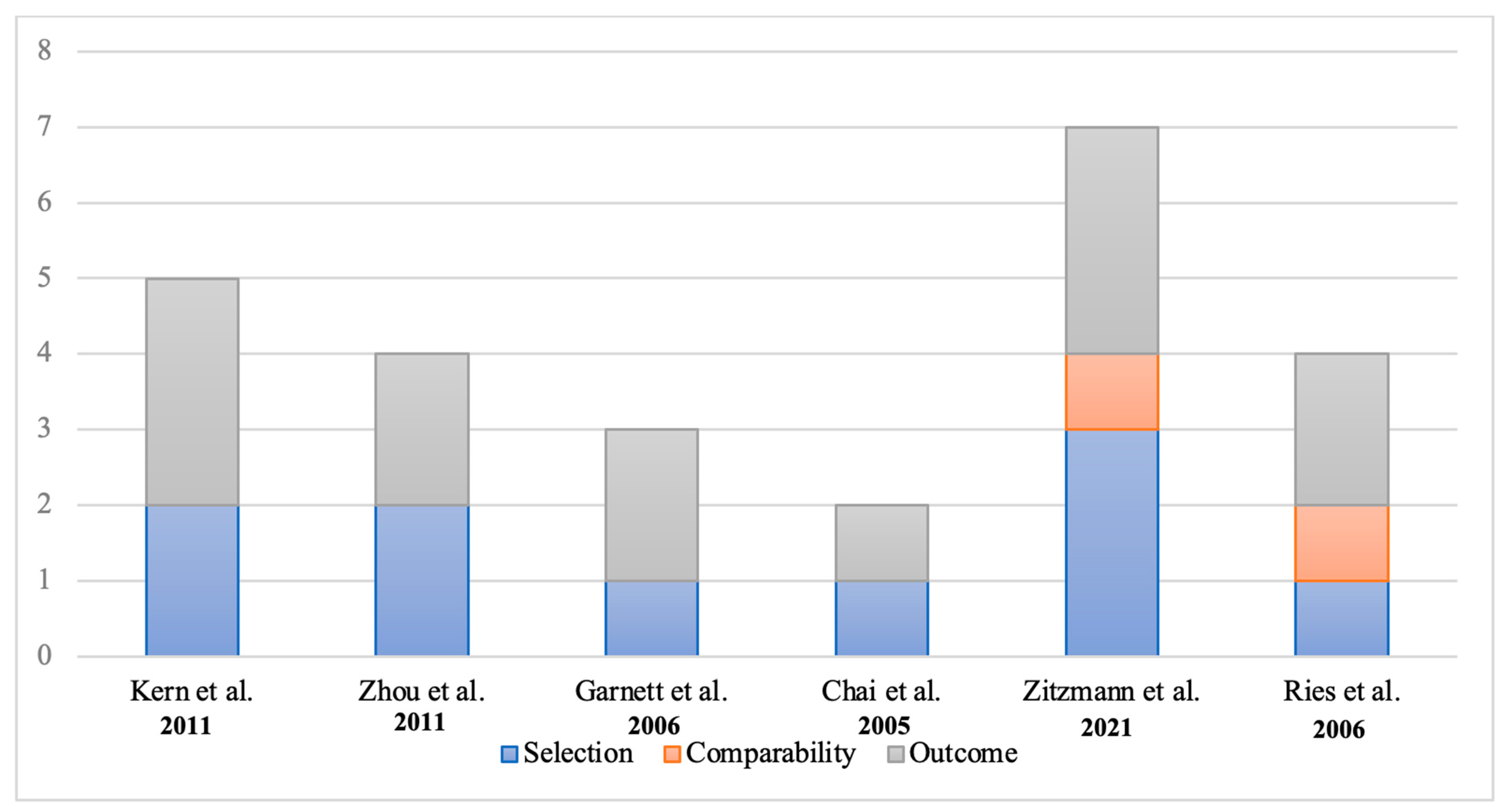
3.2. Quality Assessment
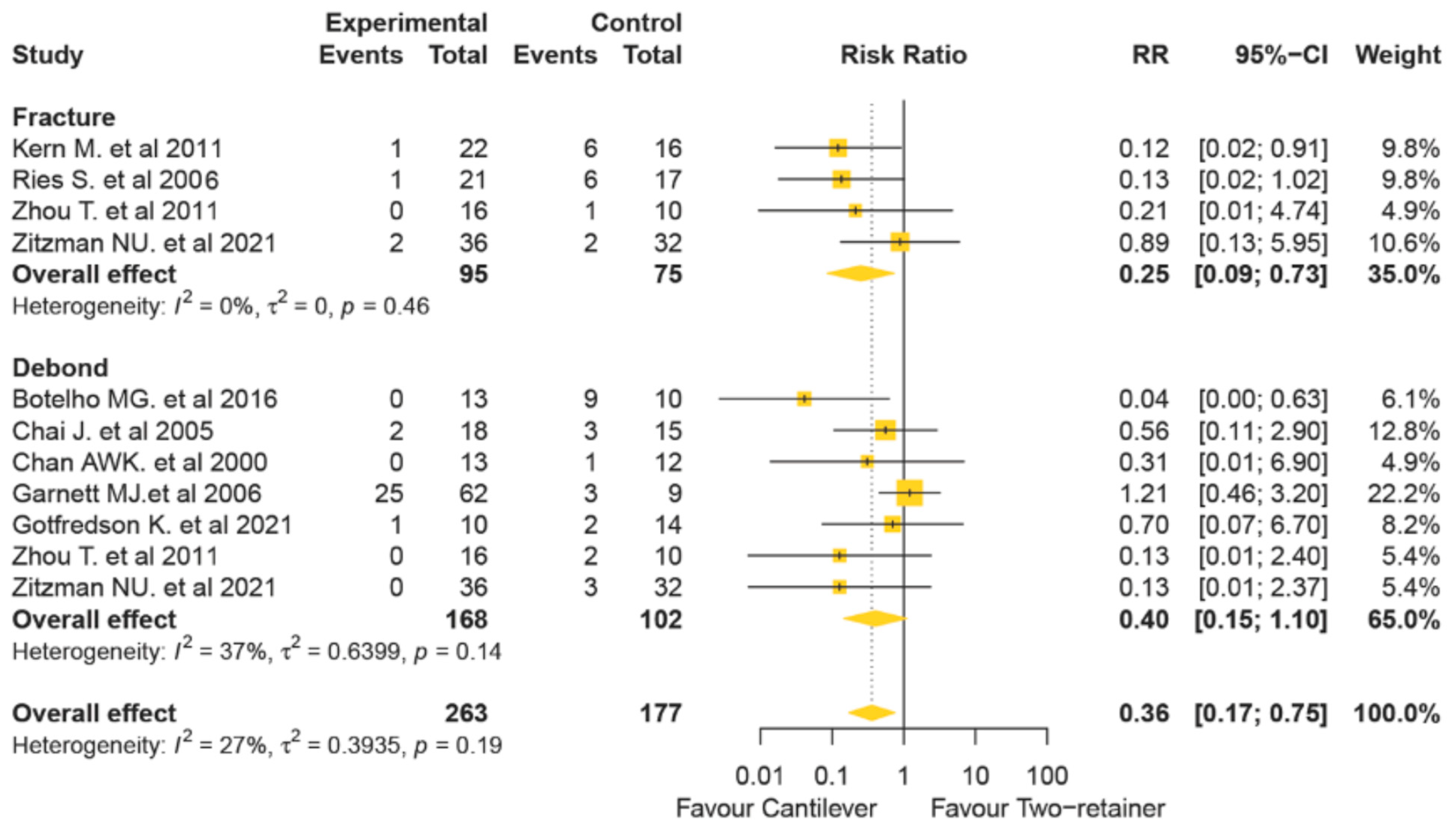
3.3. Synthesis of Results
3.4. Sensitivity and Subgroup Analyses
3.5. Publication Bias of Included Studies
4. Discussion
5. Conclusions
- Success of RBFDPs: Resin-bonded fixed dental prostheses (RBFDPs) show high long-term cumulative survival rates, confirming their effectiveness as minimally invasive restorations.
- Design Preference: RBFDPs with a single retainer in the anterior region are preferred, outperforming two-retainer designs.
- Material Comparison: All-ceramic materials deliver superior esthetic results and higher survival rates compared to metal–ceramic options.
- Recommended Protocols:
- ○
- Utilize conservative preparation techniques like proximal grooves and rests to enhance retention.
- ○
- Follow specific clearance measurements for materials.
- ○
- Strictly adhere to manufacturer guidelines for resin cement usage.
- Material-Specific Recommendations
- ○
- For zirconia: use air abrasion followed by an MDP primer to provide the most durable bond to zirconia ceramics.
- ○
- For lithium disilicate: use 5% HF etching followed by silane application.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| CI | Confidence interval |
| HF | Hydrofluoric acid |
| MDP | Methacryloyloxydecyl dihydrogen phosphate |
| OR | Odds ratio |
| OVD | Occlusal vertical dimension |
| RBFDPs | Resin-bonded fixed dental prostheses |
| RCT | Randomized controlled trial |
References
- Edelhoff, D.; Liebermann, A.; Beuer, F.; Stimmelmayr, M.; Güth, J.-F. Minimally invasive treatment options in fixed prosthodontics. Quintessence Int. 2016, 47, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Zalkind, M.; Ever-Hadani, P.; Hochman, N. Resin-bonded fixed partial denture retention: A retrospective 13-year follow-up. J. Oral Rehabil. 2003, 30, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Tan, W.C.; Tan, K.; Brägger, U.; Zwahlen, M.; Lang, N.P. A systematic review of the survival and complication rates of resin-bonded bridges after an observation period of at least 5 years. Clin. Oral Implant. Res. 2008, 19, 131–141. [Google Scholar] [CrossRef]
- Kern, M. Clinical long-term survival of two-retainer and single-retainer all-ceramic resin-bonded fixed partial dentures. Quintessence Int. 2005, 36, 141–147. [Google Scholar]
- Kern, M.; Cleser, R. Cantilevered all-ceramic, resin-bonded fixed partial dentures: A new treatment modality. J. Esthet. Restor. Dent. 1997, 9, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Jurado, C.A.; Tsujimoto, A.; Watanabe, H.; Villalobos-Tinoco, J.; Garaicoa, J.L.; Markham, M.D.; Barkmeier, W.W.; Latta, M.A. Chair-side CAD/CAM fabrication of a single-retainer resin bonded fixed dental prosthesis: A case report. Restor. Dent. Endod. 2020, 45, e15. [Google Scholar] [CrossRef]
- Olin, P.S.; Hill, E.M.E.; Donahue, J.L. Clinical evaluation of resin-bonded bridges: A retrospective study. Quintessence Int. 1991, 22, 873–877. [Google Scholar]
- Hansson, O.; Bergström, B. A longitudinal study of resin-bonded prostheses. J. Prosthet. Dent. 1996, 76, 132–139. [Google Scholar] [CrossRef]
- Behr, M.; Rammelsberg, P.; Handel, G.; Leibrock, A.; Stich, W.; Rosentritt, M. Adhesive-fixed partial dentures in anterior and posterior areas. Results of an on-going prospective study begun in 1985. Clin. Oral Investig. 1998, 2, 31–35. [Google Scholar] [CrossRef]
- Sailer, I.; Bonani, T.; Brodbeck, U.; Hammerle, C. Retrospective Clinical Study of Single-Retainer Cantilever Anterior and Posterior Glass-Ceramic Resin-Bonded Fixed Dental Prostheses at a Mean Follow-up of 6 Years. Int. J. Prosthodont. 2013, 26, 443–450. [Google Scholar] [CrossRef]
- Thoma, D.S.; Sailer, I.; Ioannidis, A.; Zwahlen, M.; Makarov, N.; Pjetursson, B.E. A systematic review of the survival and complication rates of resin-bonded fixed dental prostheses after a mean observation period of at least 5 years. Clin. Oral Implant. Res. 2017, 28, 1421–1432. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.C.; Azevedo, L.; Fonseca, P.; Viana, P.C.; Araújo, F.; Villarinho, E.; Fernandes, G.V.O.; Correia, A. The Success Rate of the Adhesive Partial Fixed Prosthesis after Five Years: A Systematic Review. Prosthesis 2023, 5, 282–294. [Google Scholar] [CrossRef]
- Gratton, D.R.; Jordan, R.E.; Teteruck, W.R. Resin-bonded bridges: The state of the art. Ont. Dent. 1983, 60, 9–11, 13–16, 18–19. [Google Scholar] [PubMed]
- Sasse, M.; Eschbach, S.; Kern, M. Randomized clinical trial on single retainer all-ceramic resin-bonded fixed partial dentures: Influence of the bonding system after up to 55 months. J. Dent. 2012, 40, 783–786. [Google Scholar] [CrossRef]
- Dundar, M.; Ozcan, M.; Comlekoglu, E.; Gungor, M.A. A preliminary report on short-term clinical outcomes of three-unit resin-bonded fixed prostheses using two adhesive cements and surface conditioning combinations. Int. J. Prosthodont. 2010, 23, 353–360. [Google Scholar]
- Wei, Y.-R.; Wang, X.-D.; Zhang, Q.; Li, X.-X.; Blatz, M.B.; Jian, Y.-T.; Zhao, K. Clinical performance of anterior resin-bonded fixed dental prostheses with different framework designs: A systematic review and meta-analysis. J. Dent. 2016, 47, 1–7. [Google Scholar] [CrossRef]
- Tezulas, E.; Yildiz, C.; Evren, B.; Ozkan, Y. Clinical procedures, designs, and survival rates of all-ceramic resin-bonded fixed dental prostheses in the anterior region: A systematic review. J. Esthet. Restor. Dent. 2018, 30, 307–318. [Google Scholar] [CrossRef]
- Garnett, M.J.; Wassell, R.W.; Jepson, N.J.; Nohl, F.S. Survival of resin-bonded bridgework provided for post-orthodontic hypodontia patients with missing maxillary lateral incisors. Br. Dent. J. 2006, 201, 527–534. [Google Scholar] [CrossRef]
- Botelho, M. Design principles for cantilevered resin-bonded fixed partial dentures. Quintessence Int. 2000, 31, 613–619. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar] [CrossRef]
- Grant, J.; Hunter, A. Measuring inconsistency in knowledgebases. J. Intell. Inf. Syst. 2006, 27, 159–184. [Google Scholar] [CrossRef]
- van Dalen, A.; Feilzer, A.J.; Kleverlaan, C.J. The influence of surface treatment and luting cement on in vitro behavior of two-unit cantilever resin-bonded bridges. Dent. Mater. 2005, 21, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Gotfredsen, K.; Alyass, N.; Hagen, M. A 5-Year Randomized Clinical Trial on 3-Unit Fiber-Reinforced vs 3- or 2-Unit Metal-Ceramic Resin-Bonded Fixed Dental Prostheses. Int. J. Prosthodont. 2021, 34, 703–711. [Google Scholar] [CrossRef]
- Botelho, M.G.; Chan, A.W.; Leung, N.C.; Lam, W. Long-term evaluation of cantilevered versus fixed–fixed resin-bonded fixed partial dentures for missing maxillary incisors. J. Dent. 2016, 45, 59–66. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chan, A.W.K.; Barnes, I.E. A prospective study of cantilever resin-bonded bridges: An initial report. Aust. Dent. J. 2000, 45, 31–36. [Google Scholar] [CrossRef]
- Zhou, T.; Wang, X.; Zhang, G. All-ceramic resin bonded fixed partial denture made of IPS hot-pressed casting porcelain restore anterior missing teeth: A three years clinical observation. Beijing Da Xue Xue Bao Yi Xue Ban = J. Peking Univ. Health Sci. 2011, 43, 77–80. [Google Scholar]
- Kern, M.; Sasse, M. Ten-year survival of anterior all-ceramic resin-bonded fixed dental prostheses. J. Adhes. Dent. 2011, 13, 407–410. [Google Scholar] [CrossRef]
- Zitzmann, N.U.; von Büren, A.; Glenz, F.; Rohr, N.; Joda, T.; Zaugg, L.K. Clinical outcome of metal- and all-ceramic resin-bonded fixed dental prostheses. J. Prosthodont. Res. 2021, 65, 243–248. [Google Scholar] [CrossRef]
- Chai, J.; Chu, F.C.S.; Newsome, P.R.H.; Chow, T.W. Retrospective survival analysis of 3-unit fixed-fixed and 2-unit cantilevered fixed partial dentures. J. Oral Rehabil. 2005, 32, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Ries, S.; Wolz, J.; Richter, E.-J. Effect of design of all-ceramic resin-bonded fixed partial dentures on clinical survival rate. Int. J. Periodontics Restor. Dent. 2006, 26, 143–149. [Google Scholar]
- Galiatsatos, A.A.; Bergou, D. Clinical evaluation of anterior all-ceramic resin-bonded fixed dental prostheses. Quintessence Int. 2014, 45, 9–14. [Google Scholar] [CrossRef]
- Kern, M. Fifteen-year survival of anterior all-ceramic cantilever resin-bonded fixed dental prostheses. J. Dent. 2017, 56, 133–135. [Google Scholar] [CrossRef] [PubMed]
- Koutayas, S.O.; Kern, M.; Ferraresso, F.; Strub, J.R. Influence of framework design on fracture strength of mandibular anterior all-ceramic resin-bonded fixed partial dentures. Int. J. Prosthodont. 2001, 15, 223–229. [Google Scholar]
- Walker, M.P.; Spencer, P.; Eick, J.D. Effect of simulated resin-bonded fixed partial denture clinical conditions on resin cement mechanical properties. J. Oral Rehabil. 2003, 30, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Piva, A.M.D.; Tribst, J.P.; Saavedra, G.S.; Souza, R.O.; de Melo, R.M.; Borges, A.L.; Özcan, M. Short communication: Influence of retainer configuration and loading direction on the stress distribution of lithium disilicate resin-bonded fixed dental prostheses: 3D finite element analysis. J. Mech. Behav. Biomed. Mater. 2019, 100, 103389. [Google Scholar] [CrossRef]
- Yoshida, T.; Kurosaki, Y.; Mine, A.; Kimura-Ono, A.; Mino, T.; Osaka, S.; Nakagawa, S.; Maekawa, K.; Kuboki, T.; Yatani, H.; et al. Fifteen-year survival of resin-bonded vs. full-coverage fixed dental prostheses. J. Prosthodont. Res. 2019, 63, 374–382. [Google Scholar] [CrossRef]
- Chen, J.; Cai, H.; Ren, X.; Suo, L.; Pei, X.; Wan, Q. A Systematic Review of the Survival and Complication Rates of All-Ceramic Resin-Bonded Fixed Dental Prostheses. J. Prosthodont. 2018, 27, 535–543. [Google Scholar] [CrossRef]
- Aggstaller, H.; Beuer, F.; Edelhoff, D.; Rammelsberg, P.; Gernet, W. Long-term clinical performance of resin-bonded fixed partial dentures with retentive preparation geometry in anterior and posterior areas. J. Adhes. Dent. 2008, 10, 301–306. [Google Scholar]
- Rammelsberg, P.; Pospiech, P.; Gernet, W. Clinical factors affecting adhesive fixed partial dentures: A 6-year study. J. Prosthet. Dent. 1993, 70, 300–307. [Google Scholar] [CrossRef]
- Miettinen, M.; Millar, B.J. A review of the success and failure characteristics of resin-bonded bridges. Br. Dent. J. 2013, 215, E3. [Google Scholar] [CrossRef]
- Hussey, D.; Linden, G. The clinical performance of cantilevered resin-bonded bridgework. J. Dent. 1996, 24, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, I.d.O.; Pereira, C.N.d.B.; Abreu, L.G.; Diniz, I.M.; de Magalhães, C.S.; da Silveira, R.R. Do different protocols affect the success rate or bond strength of glass-ceramics repaired with composite resin? A systematic review and meta-analysis. J. Prosthet. Dent. 2023. [Google Scholar] [CrossRef] [PubMed]
- Creugers, N.; Snoek, P.; Hof, M.V.; Käuyser, A. Clinical performance of resin-bonded bridges: A 5-year prospective study. Part III: Failure characteristics and survival after rebonding. J. Oral Rehabil. 1990, 17, 179–186. [Google Scholar] [CrossRef]
- Özcan, M.; Vallittu, P.K. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent. Mater. 2003, 19, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Strasser, T.; Preis, V.; Behr, M.; Rosentritt, M. Roughness, surface energy, and superficial damages of CAD/CAM materials after surface treatment. Clin. Oral Investig. 2018, 22, 2787–2797. [Google Scholar] [CrossRef]
- Lehmann, F.; Kern, M. Durability of Resin Bonding to Zirconia Ceramic Using Different Primers. J. Adhes. Dent. 2009, 11, 479–483. [Google Scholar]
- Blatz, M.B.; Sadan, A.; Kern, M. Resin-ceramic bonding: A review of the literature. J. Prosthet. Dent. 2003, 89, 268–274. [Google Scholar] [CrossRef]
- Wegner, S.M.; Kern, M. Long-term resin bond strength to zirconia ceramic. J. Adhes. Dent. 2000, 2, 139–147. [Google Scholar]
- Tanaka, R.; Fujishima, A.; Shibata, Y.; Manabe, A.; Miyazaki, T. Cooperation of Phosphate Monomer and Silica Modification on Zirconia. J. Dent. Res. 2008, 87, 666–670. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Chiche, G.; Holst, S.; Sadan, A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 2007, 38, 745–753. [Google Scholar] [PubMed]
- Shokry, M.; Al-Zordk, W.; Ghazy, M. Retention strength of monolithic zirconia crowns cemented with different primer-cement systems. BMC Oral Health 2022, 22, 187. [Google Scholar] [CrossRef]
- Kukiattrakoon, B.; Jampa, T.; Sanohkan, S.; Larpboonphol, N.; Sae-Yib, T.; Manoppan, S. The effect of various primers on shear bond strength of zirconia ceramic and resin composite. J. Conserv. Dent. 2013, 16, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Steiner, R.; Heiss-Kisielewsky, I.; Schwarz, V.; Schnabl, D.; Dumfahrt, H.; Laimer, J.; Steinmassl, O.; Steinmassl, P. Zirconia Primers Improve the Shear Bond Strength of Dental Zirconia. J. Prosthodont. 2020, 29, 62–68. [Google Scholar] [CrossRef]
| Experimental Study 3 Papers | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study (Study Design) | Mean Follow Up Time (Month) | Prosthesis Design | Manufacturing Procedure | Clinical Considerations | Failures | |||||
| Materials | Surface Treatment | Tooth Preparation | Isolation Method | Bonding System | Debond | Fracture | Others | |||
| Gotfredson 2021 (RCTs) [26] | 36 | Cantilever = 10 Fixed-Fixed = 14 | Metal- ceramic | Electrolyte etching of cast metal (18% HCl for 10 min) | Vertical, approximal groove A half circular prep at cingulum limited removal of enamel | Not reported | Panavia EX | Cantilever = 1 Fixed-fixed = 1 | Cantilever = 0 Fixed-Fixed = 0 | 0 1 (esthetics) |
| Botelho et al 2016 (RCTs) [27] | 216.5 | Cantilever = 13 Fixed-Fixed = 10 | Metal ceramic | Sandblasted with 50 um alumina particles at pressure of 520 kPa | Broad coverage of enamel Marginal ridge and cingulum rests on each abutment Rest seat and proximal groove | Rubber dam | Panavia | Cantilever = 0 Fixed-fixed = 8 | Cantilever = 0 Fixed-Fixed = 0 | 0 1 (perio) |
| Chan et al 2000 (RCTs) [28] | 35 (1 wing) 33 (2 wings) | Cantilever = 13 Fixed-fixed = 12 | Metal- ceramic | Grit blasted with 50 um alumina particles at pressure of 520 kPa | Broad coverage of enamel, supragingival margins, marginal ridge and cingulum rests on each abutment Some with retention form (proximal grooves and additional tests) | Rubber dam | Panavia | Cantilever = 0 Fixed-fixed = 1 | Cantilever = 0 Fixed-Fixed = 0 | 0 0 |
| Observational Study 6 Papers | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Mean Follow up Time (Month) | Prosthesis Design | Manufacturing Procedure | Clinical Considerations | Failures | ||||
| Materials | Surface Treatment | Tooth Preparation | Isolation Method | Bonding System | Debond | Fracture | |||
| Zhou et al 2011 (Prospective Cohort) [29] | 41.3 | Cantilever = 16 Fixed-fixed = 10 | Empress II, e.max Press, Ivoclar Vivadent | 2% HF 69 s | No retention form | Cotton roll | Variolink II | Cantilever = 0 Fixed-fixed = 2 | Cantilever = 0 Fixed-fixed = 1 |
| Kern et al 2011 (Prospective Cohort) [30] | 111.1 (1 wing) 120.2 (2 wings) | Cantilever = 22 Fixed-fixed = 16 | 16 In ceram Alumina (fixed-fixed) 14 In ceram Alumina 8 In ceram Zirconia | Tribochemically silica coated and silanated (2 wings) Air abrasion (1 wing) | A lingual veneer, a groove on the cingulum, a small proximal box (2 mm × 1 mm × 0.5 mm) | Rubber dam | Panavia TC | Cantilever = 0 Fixed-fixed = 0 | Cantilever = 1 Fixed-fixed = 7 |
| Zitzmann et al 2021 (Retrospective Cohort) [31] | 56.1 | Cantilever = 36 Fixed-Fixed = 32 | Metal-Ceramic (1 wing = 15, 2 wings = 22) All-ceramic (1 wing = 21, 2 wings = 10) | 18 LiSi etched 5% HF 20 s 14 Zirconia Metal – tribochemical silica coating + ceramic primer/silane | No undercut Shallow Groove at cingulum Slight proximal wrap around Clear margin Thickness zirconia 0.7 mm Thickness LiSi 1 mm In general, oral thickness = 0.5 mm (Metal-ceramic) | Rubber dam | Resin Cement | Cantilever = 0 Fixed-fixed = 3 | Cantilever = 2 Fixed-Fixed = 2 |
| Garnett et al 2006 (Retrospective Cohort) [18] | 59.3 | Cantilever = 62 Fixed-fixed =9 | Metal-ceramic Non-perforated Ni-Cr sandblasted with 50-250 um alumina + chemically adhesive resin | Not reported | 69 cases no report of extent of preparation | Rubber dam | Panavia 21 | Cantilever = 25 Fixed-fixed = 3 | Cantilever = 0 Fixed-fixed = 0 |
| Chai et al 2005 (Retrospective Cohort) [32] | 29 | Cantilever = 18 Fixed-fixed = 15 | Metal-ceramic (metal framework use base-metal alloy – Ni 72%, Cr20%, Mo8%) -> air abraded with 50 um alumina -> prep with carborumdum stone & tungsten carbide bur) -> clean in water bath | Air-abraded with 50 um alumina particles | Abutment prep create a single path of insertion Support from cingulum rests Stability and retention from maximum palatal coverage by metal framework | Not reported | Panavia | Cantilever = 2 Fixed-fixed = 3 | Cantilever = 0 Fixed-fixed = 0 |
| Ries 2006 (Historical Clinical Trials) [33] | 21.2 (1 wing) 15.1 (2 wings) | Cantilever = 21 Fixed-fixed = 17 | All ceramics 26 Empress II 12 e.max Ivoclar Vivadent | 5% HF + silane (monobond S, Ivoclar) | Preparation followed guidelines for proposed of PFM involving minimal veneer prep of lingual aspect, groove on cingulum and shallow approximal preparation No exposure of dentin | Rubber dam | Not reported | Cantilever = 0 Fixed-fixed = 0 | Cantilever = 1 Fixed-fixed = 6 |
| Failures | ||
|---|---|---|
| N | Risk Ratio (95% CI) | |
| Models | ||
| Fixed effects Model | 9 | 0.32 (0.19–0.55) |
| Random effects model | 9 | 0.36 (0.17–0.75) |
| Materials | ||
| All-ceramic | 3 | 0.12 (0.03–0.43) |
| Metal-Ceramic | 5 | 0.56 (0.21–1.53) |
| Both | 1 | 0.89 (0.13–5.95) |
| Rubber dam | ||
| Yes | 5 | 0.20 (0.07–0.56) |
| No | 1 | 0.09 (0.01–1.62) |
| Preparation Deign (Groove) | ||
| Yes | 7 | 0.30 (0.14–0.67) |
| No | 2 | 0.48 (0.04–5.40) |
| Study Design | ||
| Observational | 6 | 0.43 (0.17–1.07) |
| Experimental | 3 | 0.23 (0.04–1.28) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panyasuksri, N.; Angkasith, P.; Yavirach, A.; Chaijareenont, P.; Saokaew, S.; Kanchanasurakit, S. Clinical Efficacy of Anterior Ceramic Materials in Resin-Bonded Fixed Dental Prostheses with Different Bridge Designs—A Systematic Review and Meta-Analysis. Prosthesis 2025, 7, 41. https://doi.org/10.3390/prosthesis7020041
Panyasuksri N, Angkasith P, Yavirach A, Chaijareenont P, Saokaew S, Kanchanasurakit S. Clinical Efficacy of Anterior Ceramic Materials in Resin-Bonded Fixed Dental Prostheses with Different Bridge Designs—A Systematic Review and Meta-Analysis. Prosthesis. 2025; 7(2):41. https://doi.org/10.3390/prosthesis7020041
Chicago/Turabian StylePanyasuksri, Nutsongsak, Pattarika Angkasith, Apichai Yavirach, Pisaisit Chaijareenont, Surasak Saokaew, and Sukrit Kanchanasurakit. 2025. "Clinical Efficacy of Anterior Ceramic Materials in Resin-Bonded Fixed Dental Prostheses with Different Bridge Designs—A Systematic Review and Meta-Analysis" Prosthesis 7, no. 2: 41. https://doi.org/10.3390/prosthesis7020041
APA StylePanyasuksri, N., Angkasith, P., Yavirach, A., Chaijareenont, P., Saokaew, S., & Kanchanasurakit, S. (2025). Clinical Efficacy of Anterior Ceramic Materials in Resin-Bonded Fixed Dental Prostheses with Different Bridge Designs—A Systematic Review and Meta-Analysis. Prosthesis, 7(2), 41. https://doi.org/10.3390/prosthesis7020041








