Gait Assessment in the Transtibial Mercer Universal Prosthesis Designed with a “Neutral Alignment” Socket
Abstract
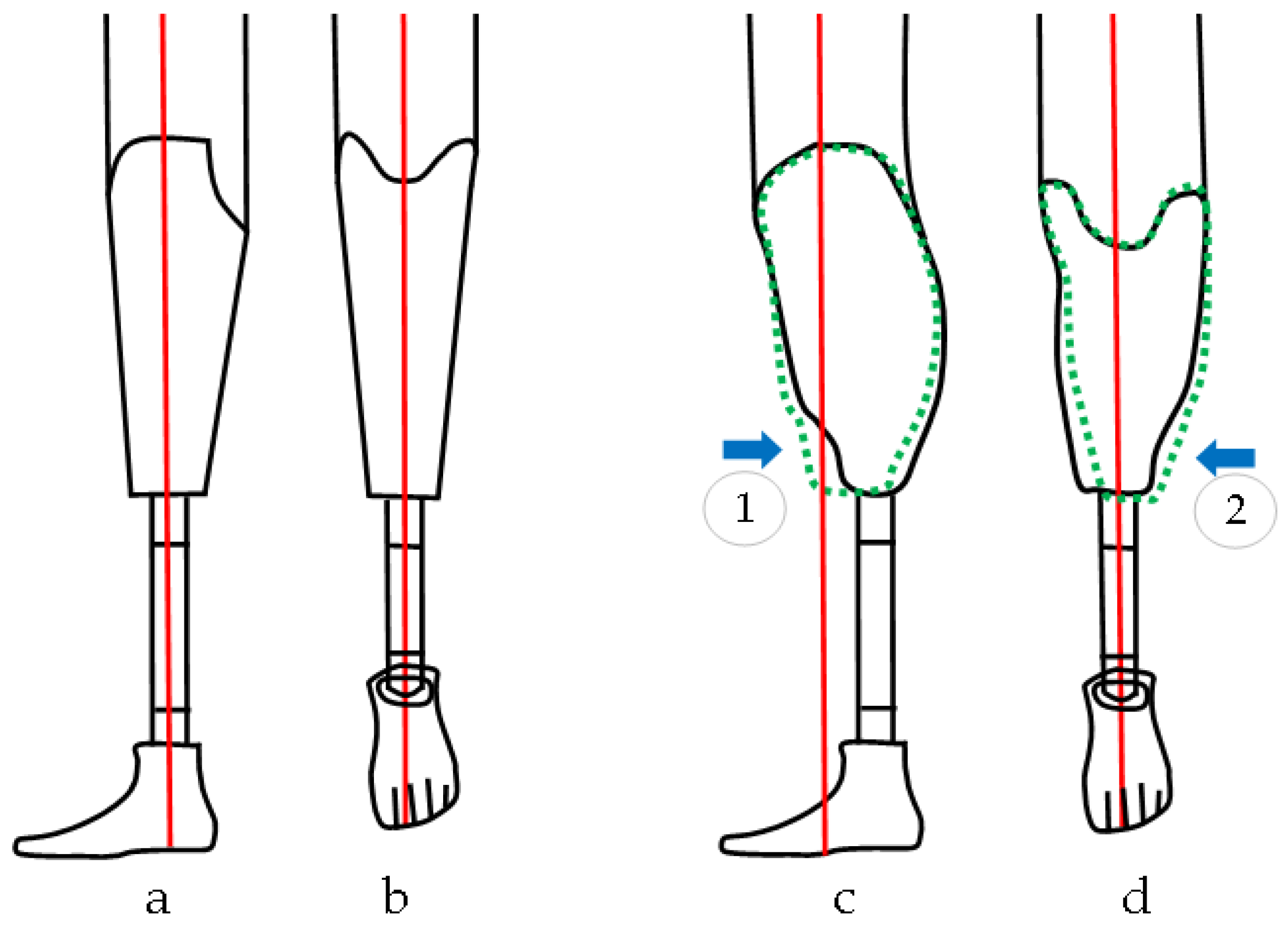
1. Introduction
2. Materials and Methods
2.1. Participants
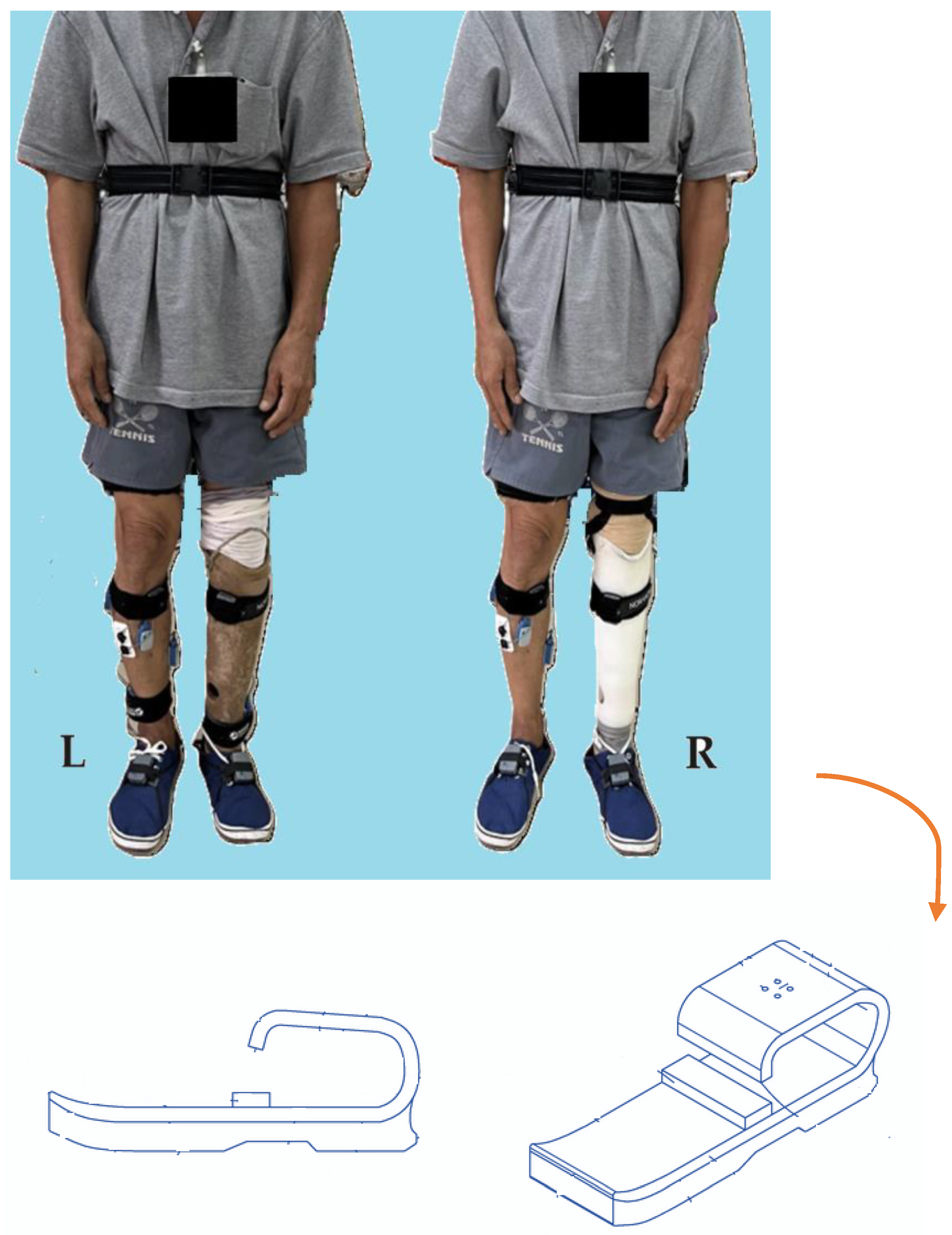
2.2. Gait Assessment Protocol
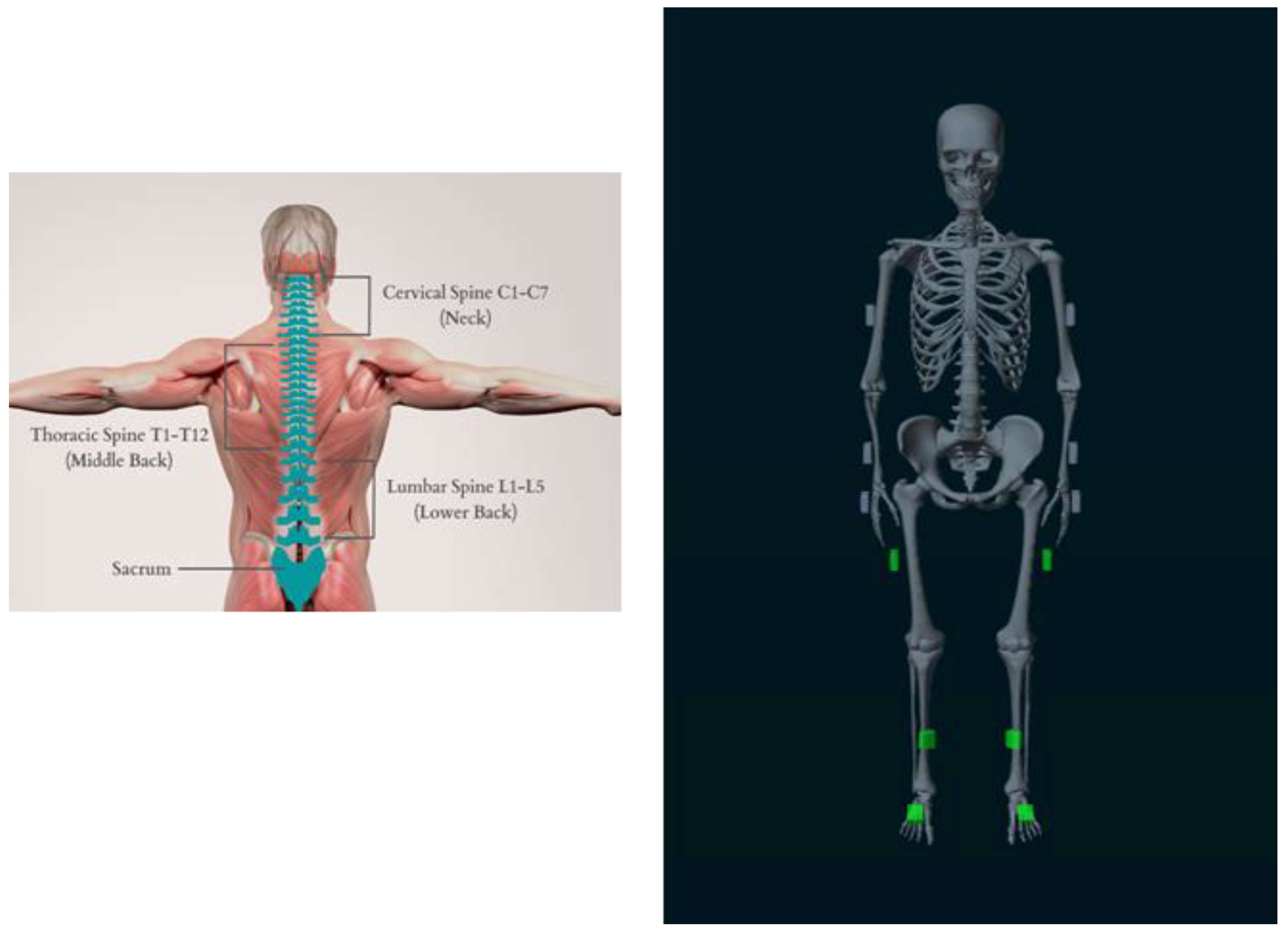
2.3. Instrumentation and Gait Analysis
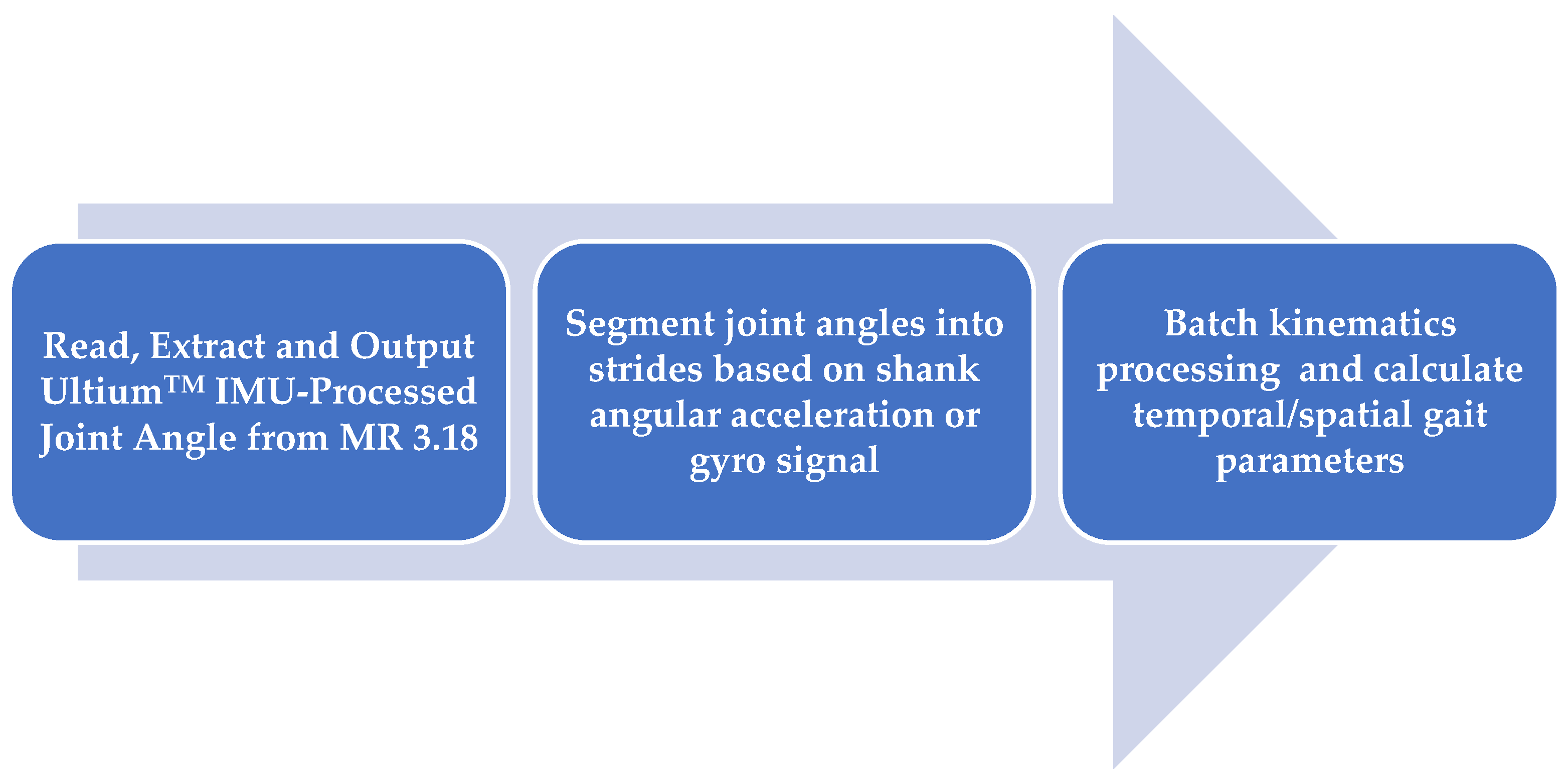
2.4. Data Processing
2.5. Statistical Analysis
- The GSI score is used to quantify similarity of movements between limbs, where
- ❖
- A GSI of 0% indicates perfect symmetry (i.e., no difference between prosthetic and intact limbs).
- ❖
- A GSI > 0% indicates asymmetry, where .
- ❖
- A GSI < 0% indicates asymmetry, where .
3. Results
3.1. Demographics and Temporal–Spatial Parameters
3.2. Kinematics
3.3. Gait Symmetry Index (GSI)
4. Discussion
5. Conclusions and Suggestions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McDonald, C.L.; Westcott-McCoy, S.; Weaver, M.R.; Haagsma, J.; Kartin, D. Global prevalence of traumatic non-fatal limb amputation. Prosthet. Orthot. Int. 2021, 45, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Andrysek, J. Lower-limb prosthetic technologies in the developing world: A review of literature from 1994–2010. Prosthet. Orthot. Int. 2010, 34, 378–398. [Google Scholar] [CrossRef] [PubMed]
- Marino, M.; Pattni, S.; Greenberg, M.; Miller, A.; Hocker, E.; Ritter, S.; Mehta, K. Access to prosthetic devices in developing countries: Pathways and challenges. In Proceedings of the 2015 IEEE Global Humanitarian Technology Conference (GHTC), IEEE, Seattle, WA, USA, 8–11 October 2015; pp. 45–51. [Google Scholar] [CrossRef]
- Wyss, D.; Lindsay, S.; Cleghorn, W.L.; Andrysek, J. Priorities in lower limb prosthetic service delivery based on an international survey of prosthetists in low- and high-income countries. Prosthet. Orthot. Int. 2015, 39, 102–111. [Google Scholar] [CrossRef]
- Jensen, J.S.; Raab, W.; Fisk, J.; Hartz, C.; Saldana, A.; Harte, C. Quality of polypropylene sockets for trans-tibial prostheses in low-income countries. Prosthet. Orthot. Int. 2006, 30, 45–59. [Google Scholar] [CrossRef]
- Jensen, J.S.; Nilsen, R.; Zeffer, J. Quality benchmark for trans-tibial prostheses in low-income countries. Prosthet. Orthot. Int. 2005, 29, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Vo, H.V.; Nguyen, B.N.; Le, T.T.; McMahan, C.T.; O’Brien, E.M.; Kunz, R.K. The novel design of the mercer universal prosthesis. In IFMBE Proceedings; Springer: Berlin/Heidelberg, Germany, 2018; pp. 197–204. [Google Scholar] [CrossRef]
- Arora, A.A.; Nguyen, B.E.; Le, T.E.; Lian, B.; Webb, L.X.; Vo, H.V. HMSR RESEARCH Clinical Using 2D Gait Motion Analysis to Evaluate the Mercer Universal Prosthetic Device in a Vietnamese Population. Harv. Med. Stud. Rev. 2018. [Google Scholar]
- Courtney, A.; Orendurff, M.S.; Buis, A. Effect of alignment perturbations in a trans-tibial prosthesis user: A pilot study. J. Rehabil. Med. 2016, 48, 396–401. [Google Scholar] [CrossRef]
- Cherni, Y.; Laurendeau, S.; Robert, M.; Turcot, K. The Influence of Transtibial Prosthesis Type on Lower-Body Gait Adaptation: A Case Study. Int. J. Environ. Res. Public. Health 2023, 20, 439. [Google Scholar] [CrossRef]
- Kobayashi, T.; Orendurff, M.S.; Boone, D.A. Dynamic alignment of transtibial prostheses through visualization of socket reaction moments. Prosthet. Orthot. Int. 2015, 39, 512–516. [Google Scholar] [CrossRef]
- Chen, C.W.J.; Heim, W.; Fairley, K.; Clement, R.J.; Biddiss, E.; Torres-Moreno, R.; Andrysek, J. Evaluation of an instrument-assisted dynamic prosthetic alignment technique for individuals with transtibial amputation. Prosthet. Orthot. Int. 2016, 40, 475–483. [Google Scholar] [CrossRef]
- Kobayashi, T.; Orendurff, M.S.; Zhang, M.; Boone, D.A. Effect of transtibial prosthesis alignment changes on out-of-plane socket reaction moments during walking in amputees. J. Biomech. 2012, 45, 2603–2609. [Google Scholar] [CrossRef]
- Hashimoto, H.; Kobayashi, T.; Gao, F.; Kataoka, M.; Orendurff, M.S.; Okuda, K. The effect of transverse prosthetic alignment changes on socket reaction moments during gait in individuals with transtibial amputation. Gait Posture 2018, 65, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Zahedi, M.S.; Spence, W.D.; Solomonidis, S.E.; Paul, J.P. Alignment of lower-limb prostheses. J. Rehabil. Res. Dev. 1986, 23, 2–19. Available online: http://www.ncbi.nlm.nih.gov/pubmed/3723422 (accessed on 16 July 2024).
- Pinzur, M.S.; Cox, W.; Kaiser, J.; Morris, T.; Patwardhan, A.; Vrbos, L. The effect of prosthetic alignment on relative limb loading in persons with trans-tibial amputation: A preliminary report. J. Rehabil. Res. Dev. 1995, 32, 373–377. Available online: http://www.ncbi.nlm.nih.gov/pubmed/8770802 (accessed on 30 January 2023). [PubMed]
- Muvvala, C.S.; Kethar, J.; Ganapathy, S. Implementation of Prosthetics in Underdeveloped Countries. J. Stud. Res. 2021, 10, 1–7. [Google Scholar] [CrossRef]
- Park, S.; Yoon, S. Validity evaluation of an inertial measurement unit (IMU) in gait analysis using statistical parametric mapping (SPM). Sensors 2021, 21, 3667. [Google Scholar] [CrossRef]
- Berner, K.; Cockcroft, J.; Morris, L.D.; Louw, Q. Concurrent validity and within-session reliability of gait kinematics measured using an inertial motion capture system with repeated calibration. J. Bodyw. Mov. Ther. 2020, 24, 251–260. [Google Scholar] [CrossRef]
- Al-Amri, M.; Nicholas, K.; Button, K.; Sparkes, V.; Sheeran, L.; Davies, J.L. Inertial measurement units for clinical movement analysis: Reliability and concurrent validity. Sensors 2018, 18, 719. [Google Scholar] [CrossRef]
- Aftab, Z.; Shad, R. Estimation of gait parameters using leg velocity for amputee population. PLoS ONE 2022, 17, e0266726. [Google Scholar] [CrossRef]
- Aftab, Z. Assessing the validity of dual-minima algorithm for heel-strike and toe-off prediction for the amputee population. medRxiv 2021. [Google Scholar] [CrossRef]
- Love, J.; Selker, R.; Marsman, M.; Jamil, T.; Dropmann, D.; Verhagen, J.; Ly, A.; Gronau, Q.F.; Smíra, M.; Epskamp, S.; et al. JASP: Graphical statistical software for common statistical designs. J. Stat. Softw. 2019, 88, 1. [Google Scholar] [CrossRef]
- Holm, S. A Simple Sequentially Rejective Multiple Test Procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Chang, Y.; Ko, C.-Y.; Jeong, B.; Kang, J.; Choi, H.-J.; Kim, G.; Shin, H.; Park, S. Changes in Spatiotemporal Parameters and Lower Limb Coordination During Prosthetic Gait Training in Unilateral Transfemoral Amputees. Int. J. Precis. Eng. Manuf. 2022, 23, 361–373. [Google Scholar] [CrossRef]
- Kova, I.; Medved, V.; Ostoji, L. Spatial, Temporal and Kinematic Characteristics of Traumatic Transtibial Amputees’ Gait. Coll. Antropol. 2010, 34 (Suppl. 1), 205–213. [Google Scholar]
- Herzog, W.; Nigg, B.M.; Read, L.J.; Olsson, E. Asymmetries in ground reaction force patterns in normal human gait. Med. Sci. Sports Exerc. 1989, 21, 110–114. [Google Scholar] [CrossRef]
- De Pauw, K.; Serrien, B.; Baeyens, J.-P.; Cherelle, P.; De Bock, S.; Ghillebert, J.; Bailey, S.; Lefeber, D.; Roelands, B.; Vanderborght, B.; et al. Prosthetic gait of unilateral lower-limb amputees with current and novel prostheses: A pilot study: Kinetics and kinematics of prosthetic gait. Clin. Biomech. 2020, 71, 59–67. [Google Scholar] [CrossRef]
- Laing, S.; Lythgo, N.; Lavranos, J.; Lee, P.V.S. Transtibial Prosthetic Socket Shape in a Developing Country: A study to compare initial outcomes in Pressure Cast hydrostatic and Patella Tendon Bearing designs. Gait Posture 2017, 58, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Laing, S.; Lee, P.V.S.; Lavranos, J.; Lythgo, N. The functional, spatio-temporal and satisfaction outcomes of transtibial amputees with a hydrocast socket following an extended usage period in an under-resourced environment. Gait Posture 2018, 66, 88–93. [Google Scholar] [CrossRef]
- Lee, P.V.S.; Lythgo, N.; Laing, S.; Lavranos, J.; Thanh, N.H. 10Pressure casting technique for transtibial prosthetic socket fit in developing countries. J. Rehabil. Res. Dev. 2014, 51, 101–110. [Google Scholar] [CrossRef]
- Bateni, H.; Olney, S.J. Effect of the Weight of Prosthetic Components on the Gait of Transtibial Amputees. JPO J. Prosthetics Orthot. 2004, 16, 113–120. [Google Scholar] [CrossRef]
- Jensen, J.S.; Nilsen, R.; Zeffer, J.; Fisk, J.; Hartz, C. Clinical field testing of vulcanized rubber feet for trans-tibial amputees in tropical low-income countries. Prosthet. Orthot. Int. 2006, 30, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Fiedler, G.; Liu, Z. Evaluation of gait variable change over time as transtibial amputees adapt to a new prosthesis foot. Biomed. Res. Int. 2019, 2019, 9252368. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, T.; Bellmann, M.; Proebsting, E.; Blumentritt, S. Effects of Adaptation to a Functionally New Prosthetic Lower-Limb Component: Results of Biomechanical Tests Immediately after Fitting and after 3 Months of Use. JPO J. Prosthet. Orthot. 2014, 26, 134–143. Available online: http://journals.lww.com/jpojournal (accessed on 14 July 2024). [CrossRef]
- Ray, S.F.; Wurdeman, S.R.; Takahashi, K.Z. Prosthetic energy return during walking increases after 3 weeks of adaptation to a new device. J. Neuroeng. Rehabil. 2018, 15, 6. [Google Scholar] [CrossRef]
- Darter, B.J.; Syrett, E.D.; Foreman, K.B.; Kubiak, E.; Sinclair, S. Changes in frontal plane kinematics over 12-months in individuals with the Percutaneous Osseointegrated Prosthesis (POP). PLoS ONE 2023, 18, e0281339. [Google Scholar] [CrossRef]
- Barnett, C.; Vanicek, N.; Polman, R.; Hancock, A.; Brown, B.; Smith, L.; Chetter, I. Kinematic gait adaptations in unilateral transtibial amputees during rehabilitation. Prosthet. Orthot. Int. 2009, 33, 135–147. [Google Scholar] [CrossRef]
| Sex | 19 Male/1 Female | |
| Age | 60 ± 8 year | |
| Height | 1.60 ± 0.07 m | |
| Prosthetic Mass | Conventional Prosthesis (CVP) | 1.55 ± 0.35 kg |
| Mercer Universal Prosthesis (MUP) | 1.31 ± 0.16 kg | |
| Descriptive Statistics: Mean (Std) | Two-Factor Repeated ANOVA | ||||||
|---|---|---|---|---|---|---|---|
| MUP | CVP | p-Value | |||||
| Prosthetic | Intact | Prosthetic | Intact | Device * Limb | Device | Limb | |
| Stride Time (s) | 1.26 (0.15) | 1.26 (0.15) | 1.24 (0.13) | 1.24 (0.13) | 0.171 | 0.086 | 0.641 |
| Stance Time (s) | 0.65 (0.12) | 0.61 (0.05) | 0.61 (0.09) | 0.63 (0.06) | 0.287 | <0.001 ** | <0.001 ** |
| Swing Time (s) | 0.71 (0.14) | 0.55 (0.03) | 0.67 (0.12) | 0.57 (0.03) | 0.785 | 0.003 ** | <0.001 ** |
| Speed (m/s) | 0.68 (0.19) | 0.69 (0.20) | 0.72 (0.13) | 0.72 (0.13) | 0.590 | 0.378 | 0.276 |
| Stride Length (m) | 0.86 (0.21) | 0.86 (0.20) | 0.87 (0.10) | 0.89 (0.10) | 0.419 | 0.696 | 0.348 |
| Step Length (m) | 0.44 (0.12) | 0.45 (0.14) | 0.42 (0.10) | 0.48 (0.09) | 0.120 | 0.752 | 0.265 |
| Descriptive Statistics: Mean (Std) | Two-Factor Repeated ANOVA | ||||||
|---|---|---|---|---|---|---|---|
| MUP | CVP | p-Value | |||||
| Prosthetic | Intact | Prosthetic | Intact | Device * Limb | Device | Limb | |
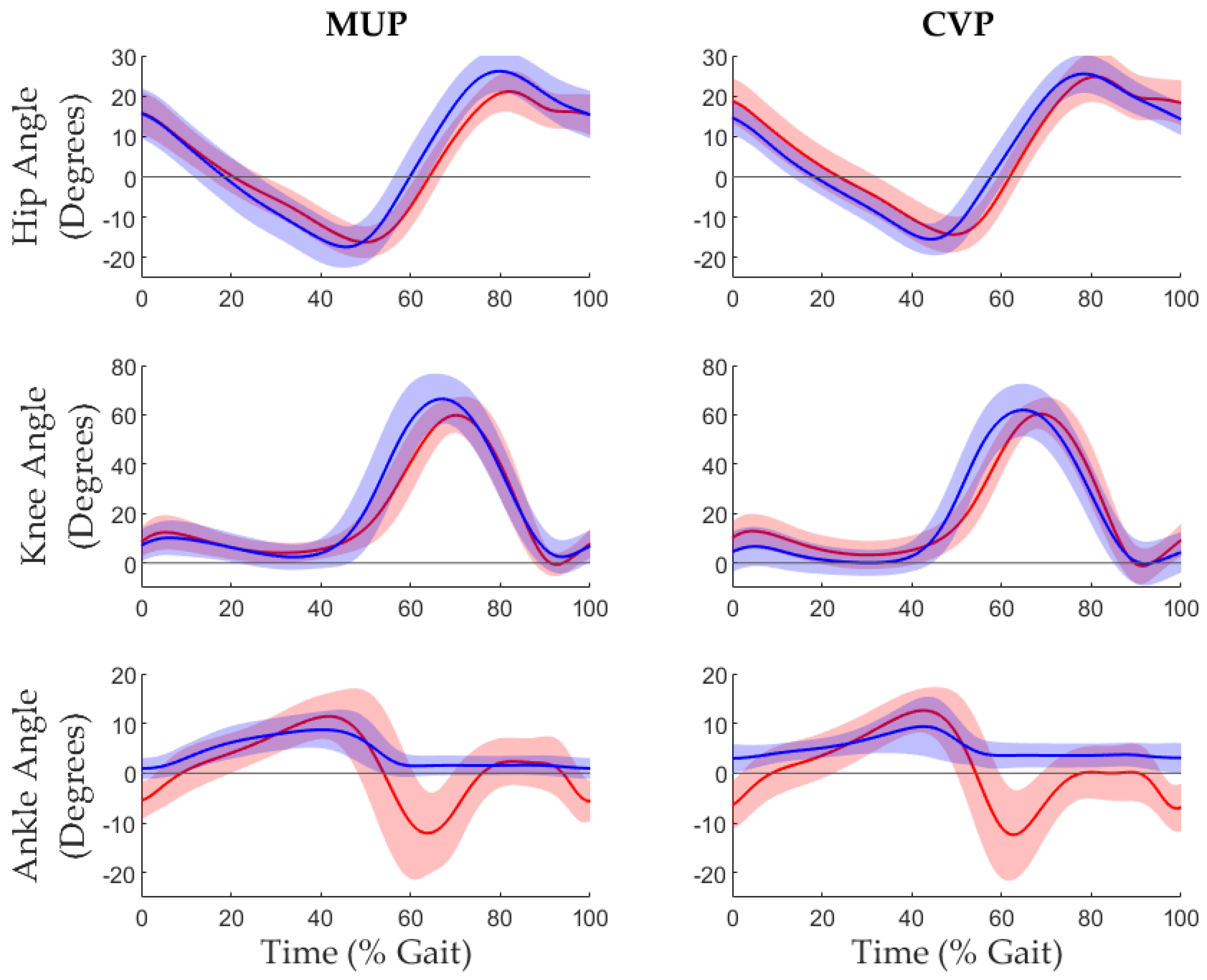
| Hip Extension (°) | −18.6 (4.1) | −17.1(3.) | −16.1 (3.5) | −14.8 (4.7) | 0.786 | 0.013 * | 0.092 |
| Knee Extension (°) | −0.4 (6.2) | −1.4(4.5) | −3.2 (5.8) | −1.5 (7.2) | 0.459 | 0.301 | 0.230 |
| Ankle Plantarflex (°) | 0.3 (2.2) | −17.6 (7.7) | 1.9 (2.9) | −15.1 (7.0) | 0.435 | 0.011 * | <0.001 ** |
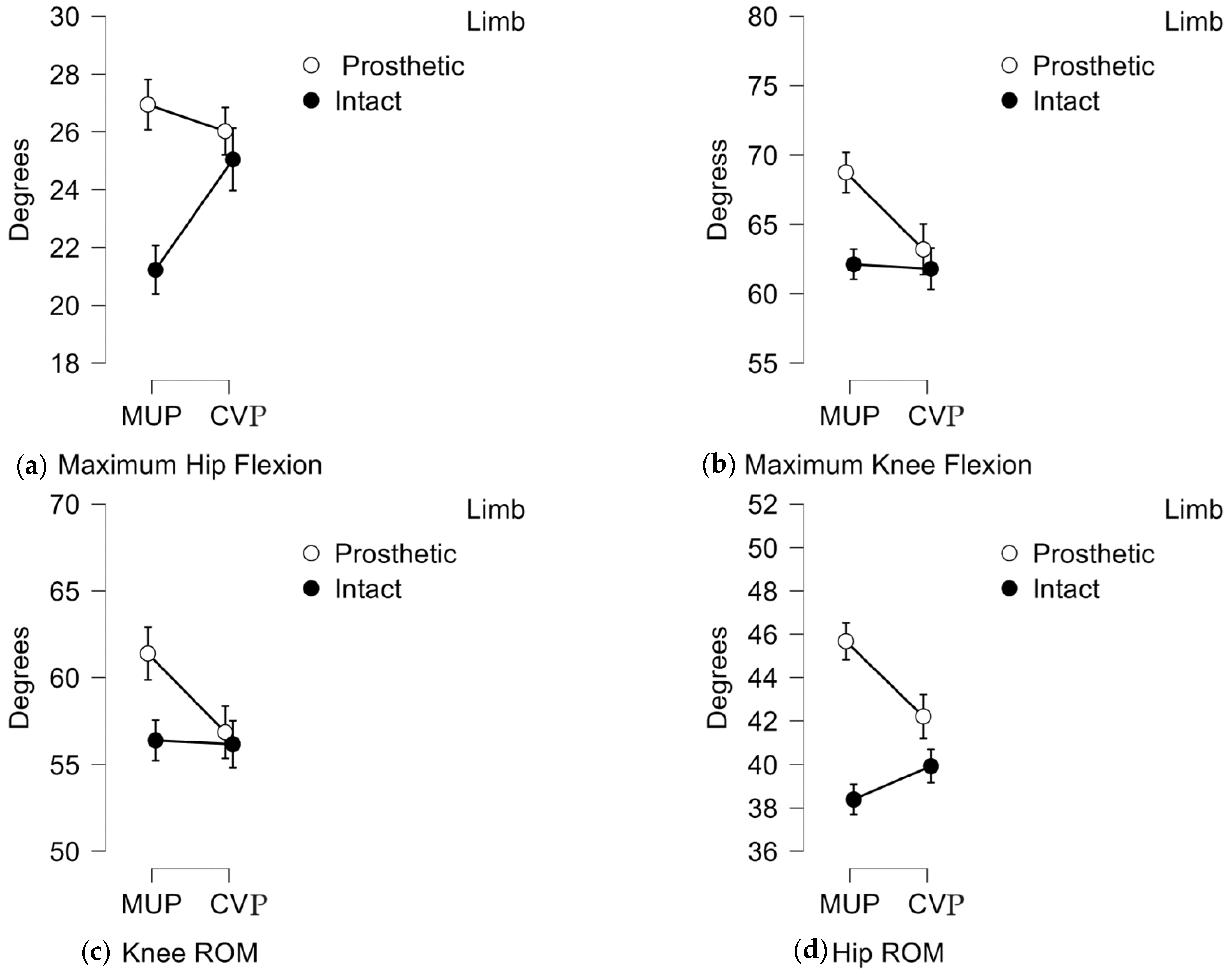
| Hip Flexion (°) | 26.9 (4.8) | 21.2 (4.9) | 26.03 (4.5) | 25.1 (6.1) | 0.013 | 0.039 * | 0.008 |
| Knee Flexion (°) | 68.4 (9.3) | 62.0(5.8) | 63.2 (9.3) | 61.6 (6.3) | 0.025 | 0.016 * | 0.067 |
| Ankle Dorsiflex (°) | 9.3 (4.1) | 12.8 (4.4) | 10.1 (6.2) | 13.7 (4.4) | 0.929 | 0.281 | 0.004 * |
| Hip ROM (°) | 45.5 (5.3) | 38.2 (4.1) | 42.1 (6.1) | 39.8 (4.3) | 0.014 * | 0.124 | <0.001 ** |
| Knee ROM (°) | 68.8 (10.6) | 63.1 (5.6) | 66.3 (8.6) | 63.0 (6.5) | 0.033 * | 0.024 * | 0.168 |
| Ankle ROM (°) | 8.9 (3.5) | 30.3 (6.4) | 8.2 (7.7) | 28.8 (5.7) | 0.675 | 0.305 | <0.001 ** |
| Mean GSI (SEM) | Paired t-Test p < 0.05 | Effect Size | |||
|---|---|---|---|---|---|
| MUP | CVP | Cohen’s d | SE | ||
| Stride Duration (s) | 0.5 (0.2) | −0.2 (0.4) | 0.120 | 0.364 | 0.309 |
| Stance Duration (s) | −7.8 (1.4) | −10.2 (1.8) | 0.185 | 0.308 | 0.249 |
| Swing Duration (s) | 9.4 (1.6) | 10.2 (1.8) | 0.838 | −0.046 | 0.221 |
| Speed (m/s) | −1.2 (1.3) | −0.7 (0.8) | 0.747 | −0.073 | 0.284 |
| Stride Length (m) | −0.3 (1.4) | −1.6 (0.9) | 0.473 | 0.164 | 0.333 |
| Step Length (m) | −0.8 (8.4) | −14.9 (8.0) | 0.135 | 0.349 | 0.255 |
| Mean GSI (SEM) | Paired t-Test p < 0.05 | Effect Size | |||
|---|---|---|---|---|---|
| MUP | CVP | Cohen’s d | SE | ||
| Hip Extension (°) | 9.1 (4.9) | 11.1 (7.9) | 0.780 | −0.063 | 0.228 |
| Knee Extension (°) | 18.7 (19.4) | 25.1 (23.0) | 0.806 | −0.056 | 0.275 |
| Ankle Plantarflexion (°) | −163.4 (46.0) | −267.9 (61.3) | 0.013 * | 0.610 | 0.161 |
| Hip Flexion (°) | 24.2 (5.5) | 5.2 (5.) | 0.012 * | 0.619 | 0.293 |
| Knee Flexion (°) | 9.7 (2.8) | 1.7 (4.2) | 0.026 * | 0.541 | 0.209 |
| Ankle Dorsiflexion (°) | −32.9 (10.9) | −36.4 (12.2) | 0.738 | 0.076 | 0.198 |
| Hip ROM (°) | 17.1 (2.9) | 5.1 (3.5) | 0.014 * | 0.606 | 0.333 |
| Knee ROM (°) | 7.8 (3.6) | 0.6 (4.0) | 0.044 * | 0.482 | 0.209 |
| Ankle ROM (°) | −109.2 (6.5) | −120.4 (10.3) | 0.323 | 0.227 | 0.284 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le, T.T.; McMahan, C.T.; Vo, H.V.; Brandon, S.C.E. Gait Assessment in the Transtibial Mercer Universal Prosthesis Designed with a “Neutral Alignment” Socket. Prosthesis 2025, 7, 31. https://doi.org/10.3390/prosthesis7020031
Le TT, McMahan CT, Vo HV, Brandon SCE. Gait Assessment in the Transtibial Mercer Universal Prosthesis Designed with a “Neutral Alignment” Socket. Prosthesis. 2025; 7(2):31. https://doi.org/10.3390/prosthesis7020031
Chicago/Turabian StyleLe, Trung T., Craig T. McMahan, Ha V. Vo, and Scott C. E. Brandon. 2025. "Gait Assessment in the Transtibial Mercer Universal Prosthesis Designed with a “Neutral Alignment” Socket" Prosthesis 7, no. 2: 31. https://doi.org/10.3390/prosthesis7020031
APA StyleLe, T. T., McMahan, C. T., Vo, H. V., & Brandon, S. C. E. (2025). Gait Assessment in the Transtibial Mercer Universal Prosthesis Designed with a “Neutral Alignment” Socket. Prosthesis, 7(2), 31. https://doi.org/10.3390/prosthesis7020031






