Applying 3D Scanning and Printing Techniques to Produce Upper Limb Prostheses: Bibliometric Analysis and Scoping Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Search Results
3.2. Summary of the Literature
3.3. Bibliometric Analysis
4. Discussion
4.1. Key Areas of Research
4.1.1. Cluster 1: Prosthesis Design and Evaluation for People
4.1.2. Cluster 2: Prosthesis Control and Sensing Technologies
4.1.3. Cluster 3: Robotics and Mechanical Design
4.1.4. Cluster 4: Accessibility for Prosthesis
4.2. Trends
4.2.1. Trend 1: Focus on Fingers
4.2.2. Trend 2: Advancement of Control Systems
4.2.3. Trend 3: The Rise of 3D Scanning
4.3. Limitations and Implications of Work
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Ventola, C.L. Medical Applications for 3D Printing: Current and Projected Uses. Pharm. Ther. 2014, 39, 704–711. [Google Scholar]
- Manero, A.; Smith, P.; Sparkman, J.; Dombrowski, M.; Courbin, D.; Kester, A.; Womack, I.; Chi, A. Implementation of 3D Printing Technology in the Field of Prosthetics: Past, Present, and Future. Int. J. Environ. Res. Public Health 2019, 16, 1641. [Google Scholar] [CrossRef] [PubMed]
- Paxton, N.C.; Nightingale, R.C.; A Woodruff, M. Capturing patient anatomy for designing and manufacturing personalized prostheses. Curr. Opin. Biotechnol. 2022, 73, 282–289. [Google Scholar] [CrossRef]
- Webster, J.B.; Hakimi, K.N.; Williams, R.M.; Turner, A.P.; Norvell, D.C.; Czerniecki, J.M. Prosthetic fitting, use, and satisfaction following lower-limb amputation: A prospective study. J. Rehabil. Res. Dev. 2012, 49, 1493–1504. [Google Scholar] [CrossRef] [PubMed]
- Eklund, A.; Sexton, S. Standards for Prosthetics and Orthotics Service Provision. In WHO Standards for Prosthetics and Orthotics; WHO: Geneva, Switzerland, 2015; Volume 22, pp. 1–22. [Google Scholar]
- Mduzana, L.; Tiwari, R.; Lieketseng, N.; Chikte, U. Exploring national human resource profile and trends of Prosthetists/Orthotists in South Africa from 2002 to 2018. Glob. Health Action 2020, 13, 1792192. [Google Scholar] [CrossRef]
- de Godoy, J.M.P.; Braile, D.M.; Buzatto, S.H.G.; Longo, O.; Fontes, O.A. Quality of life after amputation. Psychol. Health Med. 2002, 7, 397–400. [Google Scholar] [CrossRef]
- Akkaya, N.; Atalay, N.S.; Selcuk, S.T.; Akkaya, S.; Ardic, F. Impact of body image on quality of life and mood in mastectomized patients and amputees in Turkey. Asian Pac. J. Cancer Prev. 2011, 12, 2669–2673. [Google Scholar]
- Barrios-Muriel, J.; Romero-Sánchez, F.; Alonso-Sánchez, F.J.; Salgado, D.R. Advances in Orthotic and Prosthetic Manufacturing: A Technology Review. Materials 2020, 13, 295. [Google Scholar] [CrossRef]
- Attaran, M. The rise of 3-D printing: The advantages of additive manufacturing over traditional manufacturing. Bus. Horiz. 2017, 60, 677–688. [Google Scholar] [CrossRef]
- Wendo, K.; Barbier, O.; Bollen, X.; Schubert, T.; Lejeune, T.; Raucent, B.; Olszewski, R. Open-Source 3D Printing in the Prosthetic Field—The Case of Upper Limb Prostheses: A Review. Machines 2022, 10, 413. [Google Scholar] [CrossRef]
- Sargent, J.F.; Schwartz, R.X. 3D Printing: Overview, Impacts, and the Federal Role; Congressional Research Service: Washington, DC, USA, 2019.
- Flaubert, J.L.; Spicer, C.M.; Jette, A.M. The Promise of Assistive Technology to Enhance Activity and Work Participation; The National Academic Press: Washington, DC, USA, 2017. [Google Scholar]
- Cordella, F.; Ciancio, A.L.; Sacchetti, R.; Davalli, A.; Cutti, A.G.; Guglielmelli, E.; Zollo, L. Literature Review on Needs of Upper Limb Prosthesis Users. Front. Neurosci. 2016, 10, 209. [Google Scholar] [CrossRef] [PubMed]
- Pahlevan-Sharif, S.; Mura, P.; Wijesinghe, S.N.R. A systematic review of systematic reviews in tourism. J. Hosp. Tour. Manag. 2019, 39, 158–165. [Google Scholar] [CrossRef]
- Sharif, S.P.; Mura, P.; Wijesinghe, S.N.R. Systematic Reviews in Asia: Introducing the ‘PRISMA’ Protocol to Tourism and Hospitality Scholars. In Quantitative Tourism Research in Asia; Springer: Singapore, 2019; pp. 13–33. [Google Scholar] [CrossRef]
- Žujović, M.; Obradović, R.; Rakonjac, I.; Milošević, J. 3D printing technologies in architectural design and construction: A systematic literature review. Buildings 2022, 12, 1319. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L. VOSviewer Manual, Version 1.6.20; Univeristeit Leiden: Leiden, The Netherlands, 2023. [Google Scholar]
- Ellegaard, O.; Wallin, J.A. The bibliometric analysis of scholarly production: How great is the impact? Scientometrics 2015, 105, 1809–1831. [Google Scholar] [CrossRef]
- Dudkiewicz, I.; Gabrielov, R.; Seiv-Ner, I.; Zelig, G.; Heim, M. Evaluation of prosthetic usage in upper limb amputees. Disabil. Rehabil. 2004, 26, 60–63. [Google Scholar] [CrossRef]
- Del Cura, V.O.; Cunha, F.L.; Aguiar, M.L.; Cliquet, A., Jr. Study of the Different Types of Actuators and Mechanisms for Upper Limb Prostheses. Artif. Organs 2003, 27, 507–516. [Google Scholar] [CrossRef]
- Hussaini, A.; Kyberd, P.; Mulindwa, B.; Ssekitoleko, R.; Keeble, W.; Kenney, L.; Howard, D. 3D Printing in LMICs: Functional Design for Upper Limb Prosthetics in Uganda. Prosthesis 2023, 5, 130–147. [Google Scholar] [CrossRef]
- Cabibihan, J.-J.; Abubasha, M.K.; Thakor, N. A Method for 3-D Printing Patient-Specific Prosthetic Arms with High Accuracy Shape and Size. IEEE Access 2018, 6, 25029–25039. [Google Scholar] [CrossRef]
- Sokolowski, S.L.; Meyer, Z. A product design approach to prosthetic design: A case study. In Proceedings of the 2019 Design of Medical Devices Conference, Minneapolis, MN, USA, 15–18 April 2019; Available online: https://asmedigitalcollection.asme.org/BIOMED/proceedings-abstract/DMD2019/V001T10A018/954621 (accessed on 24 October 2023).
- Putra, K.B.; Montgomery, N.; Kalamdani, S.; Chen, L.; Kelly, B.; Wensman, J.; Shih, A. Fabrication and assessment of partial finger prostheses made using 3D-printed molds: A case study. Prosthet. Orthot. Int. 2023, 47, 327–335. [Google Scholar] [CrossRef]
- Alvial, P.; Bravo, G.; Bustos, M.P.; Moreno, G.; Alfaro, R.; Cancino, R.; Zagal, J.C. Quantitative functional evaluation of a 3D-printed silicone-embedded prosthesis for partial hand amputation: A case report. J. Hand Ther. 2017, 31, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.; Shimizu, Y.; Kikuchi, A.; Hada, Y.; Suzuki, K. Rapid and Flexible 3D Printed Finger Prostheses With Soft Fingertips: Technique and Clinical Application. IEEE Access 2022, 10, 60412–60420. [Google Scholar] [CrossRef]
- Alturkistani, R.; Kavin, A.; Devasahayam, S.; Thomas, R.; Colombini, E.L.; Cifuentes, C.A.; Homer-Vanniasinkam, S.; Wurdemann, H.A.; Moazen, M. Affordable passive 3D-printed prosthesis for persons with partial hand amputation. Prosthet. Orthot. Int. 2020, 44, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Azeeb, M.M.; Wan, F.W.F.A.; Rashid, H.; Halim, A.A. Design and Analysis of 3D Printed Prosthetic Hand for Symbrachydactyly Patients. In Proceedings of the International Exchange and Innovation Conference on Engineering & Sciences (IEICES), Fukuoka, Japan, 24–25 October 2019; Volume 5, pp. 87–88. [Google Scholar] [CrossRef]
- GགྷRski, F.; Zawadzki, P.; Wichniarek, R.; Kuczko, W.; Slupińska, S.; Żukowska, M. Automated Design and Rapid Manufacturing of Low-Cost Customized Upper Limb Prostheses. J. Phys. Conf. Ser. 2022, 2198, 012040. [Google Scholar] [CrossRef]
- Zulkifli, M.F.; Hashim, N.M.; Ramlee, M.H.; Whulanza, Y.; Abdullah, A.H. Development of Customized Passive Arm Prosthetics by Integrating 3D Printing and Scanning Technology. Int. J. Online Biomed. Eng. 2023, 19, 65–75. [Google Scholar] [CrossRef]
- Tan, W.S.; Harito, C.; Andhini, G.K.; Martawidjaja, M.; Chainando, N.; Syafi’i, M.; Putra, K.B.; Syafrudin, M. Color Modification of Silicone-Based Prosthetic Finger by 3D-Printed Mold. Prosthesis 2024, 6, 1017–1028. [Google Scholar] [CrossRef]
- Stefanovic, B.; Michalíková, M.; Bednarcíková, L.; Trebunová, M.; Zivcák, J. Innovative approaches to designing and manufacturing a prosthetic thumb. Prosthet. Orthot. Int. 2021, 45, 81–84. [Google Scholar] [CrossRef]
- van der Stelt, M.; Verhulst, A.C.; Vas Nunes, J.H.; Koroma, T.A.R.; Nolet, W.W.E.; Slump, C.H.; Grobusch, M.P.; Maal, T.J.J.; Brouwers, L. Improving Lives in Three Dimensions: The Feasibility of 3D Printing for Creating Personalized Medical Aids in a Rural Area of Sierra Leone. Am. J. Trop. Med. Hyg. 2020, 102, 905–909. [Google Scholar] [CrossRef]
- Hazubski, S.; Bamerni, D.; Otte, A. Conceptualization of a Sensory Feedback System in an Anthropomorphic Replacement Hand. Prosthesis 2021, 3, 415–427. [Google Scholar] [CrossRef]
- Chen, L.; Plott, J.; Hildner, M.; Mei, L.; Shih, A.; Wensman, J.; Kelly, B. Computer-Aided Design and Additive Manufacturing of Custom Silicone Prosthetic Finger. In Proceedings of the ASME 2020 15th International Manufacturing Science and Engineering Conference (MSEC2020), Virtual Conference, 3 September 2020; Volume 1B. [Google Scholar]
- Binedell, T.; Meng, E.; Subburaj, K. Design and development of a novel 3D-printed non-metallic self-locking prosthetic arm for a forequarter amputation. Prosthet. Orthot. Int. 2021, 45, 94–99. [Google Scholar] [CrossRef]
- Pinto, V.V.P.; Alvarez-Jacobo, J.E.; Da Gama, A.E.F. Design and Manufacturing of Flexible Finger Prosthesis Using 3D Printing. In Proceedings of the XXVII Brazilian Congress on Biomedical Engineering, CBEB 2020, Vitória, Brazil, 26–30 October 2020; Bastos-Filho, T.F., Caldeira, E.M.D., Frizera-Neto, A., Eds.; Springer: Cham, Switzerland, 2022; pp. 419–424. [Google Scholar] [CrossRef]
- O’Brien, L.; Montesano, E.; Chadwell, A.; Kenney, L.; Smit, G. Real-World Testing of the Self Grasping Hand, a Novel Adjustable Passive Prosthesis: A Single Group Pilot Study. Prosthesis 2022, 4, 48–59. [Google Scholar] [CrossRef]
- Leite, M.; Soares, B.; Lopes, V.; Santos, S.; Silva, M.T. Design for personalized medicine in orthotics and prosthetics. In Proceedings of the 29th CIRP Design Conference 2019, Póvoa de Varzim, Portugal, 8–10 May 2019; Putnik, G.D., Ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 457–461. [Google Scholar] [CrossRef]
- Zhou, J.; Fu, C.; Fang, J.; Shang, K.; Pu, X.; Zhang, Y.; Jiang, Z.; Lu, X.; He, C.; Jia, L.; et al. Prosthetic finger for fingertip tactile sensing via flexible chromatic optical waveguides. Mater. Horiz. 2023, 10, 4940–4951. [Google Scholar] [CrossRef] [PubMed]
- Brancewicz-Steinmetz, E.; Slabecka, N.; Sniarowski, P.; Wybrzak, K.; Sawicki, J. Surface Structure Modification in Fused Filament Fabrication (FFF) Multi-Material Printing for Medical Applications: Printing of a Hand Prosthesis. 3D Print. Addit. Manuf. 2023, 11, 1972–1980. [Google Scholar] [CrossRef] [PubMed]
- Timm, L.; Etuket, M.; Sivarasu, S. Design and Development of an Open-Source ADL-Compliant Prosthetic Arm for Trans-Radial Amputees. In Proceedings of the 2022 Design of Medical Devices Conference, DMD 2022, Minneapolis, MN, USA, 11–14 April 2022; American Society of Mechanical Engineers: New York City, NY, USA, 2022. [Google Scholar] [CrossRef]
- Zuniga, J.M. 3D printed antibacterial prostheses. Appl. Sci. 2018, 8, 1651. [Google Scholar] [CrossRef]
- Young, K.J.; Pierce, J.E.; Zuniga, J.M. Assessment of body-powered 3D printed partial finger prostheses: A case study. 3D Print. Med. 2019, 5, 7. [Google Scholar] [CrossRef]
- Dumitrescu, G.-C.N.; Braileanu, P.I. Custom Prosthetic Finger Device Using 3D Printable PA11 CF Powder. Ann. “Dunarea de Jos” Univ. Galati. Fascicle IX Met. Mater. Sci. 2023, 46, 33–36. [Google Scholar] [CrossRef]
- Lim, D.; Georgiou, T.; Bhardwaj, A.; O’Connell, G.D.; Agogino, A.M. Customization of a 3D printed prosthetic finger using parametric modeling. In Proceedings of the ASME Design Engineering Technical Conference, Quebec City, QC, Canada, 26–29 August 2018; American Society of Mechanical Engineers (ASME): New York City, NY, USA, 2018. [Google Scholar] [CrossRef]
- Belvončíková, D.; Bednarčíková, L.; Michalíková, M.; Štefanovič, B.; Trebuňová, M.; Mezencevová, V.; Živčák, Z. Development of Mechanism for Finger Prosthesis. Acta Mech. Slovaca 2020, 24, 6–11. [Google Scholar] [CrossRef]
- Nishikawa, K.; Hirata, K.; Takaiwa, M. Development of Self-Powered 5-Finger Pneumatically Driven Hand Prosthesis Using Supination of Forearm. J. Robot. Mechatron. 2022, 34, 454–465. [Google Scholar] [CrossRef]
- Sigdestad, A.; Sharma, S.; Foreman, C. Prosthetic Thumb; California Polytechnic State University: San Luis Obispo, CA, USA, 2020; Available online: https://digitalcommons.calpoly.edu/bmedsp/113/ (accessed on 24 October 2023).
- Bustamante, M.; Vega-Centeno, R.; Sánchez, M.; Mio, R. A parametric 3D-printed body-powered hand prosthesis based on the four-bar linkage mechanism. In Proceedings of the 2018 IEEE 18th International Conference on Bioinformatics and Bioengineering, BIBE 2018, Taichung, Taiwan, 29–31 October 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 79–85. [Google Scholar] [CrossRef]
- Secco, E.L.; Moutschen, C.; Agidew, T.F.; Nagar, A.K. A sustainable & biologically inspired prosthetic hand for healthcare. EAI Endorsed Trans. Pervasive Health Technol. 2018, 4, e3. [Google Scholar] [CrossRef]
- Carroll, R.; Carrozza, B.; Lopez, J.; Ordonez, Y.; Sanchez, E.; Kim, D.; Lee, A.; Teh, K.S. Accessible Children’s Prosthetics Created Using 3D Printing Technologies. In Proceedings of the 2018 American Society for Engineering Education Zone IV Conference, Boulder, CO, USA, 25–27 March2018. [Google Scholar]
- Cuellar, J.S.; Plettenburg, D.; Zadpoor, A.A.; Breedveld, P.; Smit, G. Design of a 3D-printed hand prosthesis featuring articulated bio-inspired fingers. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2020, 235, 336–345. [Google Scholar] [CrossRef]
- Mazlan, M.A.; Fadzil, W.F.A.W.; Rashid, H.; Abdullah, A.H. Development of 3D printed symbrachydactyly prosthetic hand. Prosthetic Hand. Int. J. Eng. Adv. Technol. 2019, 9, 5943–5947. [Google Scholar] [CrossRef]
- da Silveira Romero, R.C.; Machado, A.A.; Costa, K.A.; Reis, P.H.R.G.; Brito, P.P.; Vimieiro, C.B.S. Development of a passive prosthetic hand that restores finger movements made by additive manufacturing. Appl. Sci. 2020, 10, 4148. [Google Scholar] [CrossRef]
- Ferreira, D.; Duarte, T.; Alves, J.L.; Ferreira, I. Development of low-cost customised hand prostheses by additive manufacturing. Plast. Rubber Compos. 2018, 47, 25–34. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Young, K.J.; Peck, J.L.; Srivastava, R.; Pierce, J.E.; Dudley, D.R.; Salazar, D.A.; Bergmann, J. Remote fitting procedures for upper limb 3d printed prostheses. Expert Rev. Med. Devices 2019, 16, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.; Schanandore, J.V. Using a 3D-Printed Prosthetic to Improve Participation in a Young Gymnast. Pediatr. Phys. Ther. 2021, 33, E1–E6. [Google Scholar] [CrossRef]
- Figliolia, A.; Medola, F.; Sandnes, F.; Rodrigues, A.C.T.; Paschoarelli, L.C. Avoiding Product Abandonment Through User Centered Design: A Case Study Involving the Development of a 3D Printed Customized Upper Limb Prosthesis. In Advances in Additive Manufacturing, Modeling Systems and 3D Prototyping; DiNicolantonio, M., Rossi, E., Alexander, T., Eds.; Springer: Cham, Switzerland, 2020; pp. 289–297. [Google Scholar] [CrossRef]
- Górski, F.; Gapsa, J.; Kupaj, A.; Kuczko, W.; Zukowska, M.; Zawadzki, P. Virtual Design Process of Customized 3D Printed Modular Upper Limb Prostheses. In Advances in Manufacturing IV; Gorski, F., Pacurar, R., Gonzalez, J.F.R., Rychlik, M., Eds.; Manufacturing 2024; Springer: Cham, Switzerland, 2024; Volume 5, pp. 206–218. [Google Scholar] [CrossRef]
- Cuellar, J.S.; Smit, G.; Breedveld, P.; Zadpoor, A.A.; Plettenburg, D. Functional evaluation of a non-assembly 3D-printed hand prosthesis. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2019, 233, 1122–1131. [Google Scholar] [CrossRef]
- Martinez, C.J.C.; Lagos, F.D.C. Design of a Customized Thumb Prosthesis: Focus on Functionality and Comfort. J. Biomim. Biomater. Biomed. Eng. 2024, 66, 17–26. [Google Scholar] [CrossRef]
- Oporto-Tejerina, F.R.; Tapia-Siles, S.C. Design and prototyping of low cost, 3D printed body powered hand prosthesis for transradial amputees in Bolivia. In Proceedings of the 2023 11th International Conference on Control, Mechatronics and Automation, ICCMA, Agder, Norway, 1–3 November 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 386–391. [Google Scholar] [CrossRef]
- Lee, M.Y.; Lee, S.H.; Leigh, J.H.; Nam, H.S.; Hwang, E.Y.; Lee, J.Y.; Han, S.; Lee, G. Functional improvement by body-powered 3D-printed prosthesis in patients with finger amputation Two case reports. Medicine 2022, 101, e29182. [Google Scholar] [CrossRef]
- Loutan, K.J.; Persad, U. The Design of a Low-Cost Voluntary Closing Finger Prosthetic for Developing Countries. In Proceedings of the ASME 2023 International Design Engineering Technical Conferences and Computers and Information in Engineering Conference, IDETC-CIE2023, Boston, MA, USA, 20–23 August 2023; Volume 2. [Google Scholar]
- da Silva, L.A.; Medola, F.O.; Rodrigues, O.V.; Rodrigues, A.C.T.; Sandnes, F.E. Interdisciplinary-Based Development of User-Friendly Customized 3D Printed Upper Limb Prosthesis. In Advances in Usability, User Experience and ASSISTIVE Technology; Ahram, T.Z., Falcao, C., Eds.; Springer: Cham, Switzerland, 2019; pp. 899–908. [Google Scholar] [CrossRef]
- Panchik, D.; Feeney, G.C.; Springer, A.A.; VanBrocklin, C.G.; Winters, H.E. Designing a 3D Printed Prosthetic to Meet Task-Specific Needs: A Case Study. Internet J. Allied Health Sci. Pract. 2021, 19, 1. [Google Scholar]
- Gorman, N.; Feng, J.; Pareja, S.Y.M. Enhancing Prosthetic Hand Functionality with Elastic 3D-Printed Thermoplastic Polyurethane. In Advances in Human Factors and Ergonomics in Healthcare and Medical Devices (AHFE 2021); Kalra, J., Lightner, N.J., Taiar, R., Eds.; Springer: Cham, Switzerland, 2021; pp. 183–190. [Google Scholar] [CrossRef]
- Barreno-Avila, E.M.; Espin-Lagos, S.M.; Guamanquispe-Vaca, D.V.; Lascano-Moreta, A.M.; Guevara-Morales, C.I.; Freire-Romero, D.R. Design and Construction of a Prosthetic Finger with Distal Phalanx Amputation. In Innovation and Research-Smart Technologies & Systems; Vizuete, M.Z., Botto-Tobar, M., Casillas, S., Gonzalez, C., Sanchez, C., Gomes, G., Durakovic, B., Eds.; CI3 2023; Springer: Cham, Switzerland, 2024; Volume 1, pp. 211–224. [Google Scholar] [CrossRef]
- Chander, S.A.; Datta, B.; Singh, A.; Shivling, V.D. Feasibility of Ratchet-Pawl mechanism for trans-phalangeal finger prosthetic: A minimalistic design approach. J. Braz. Soc. Mech. Sci. Eng. 2024, 46, 160. [Google Scholar] [CrossRef]
- Lee, H.C.; Cipra, R. Design of a Novel Locking Ratcheting Mechanism for a Body-Powered Underactuated Hand. J. Med Devices 2020, 14, 011101. [Google Scholar] [CrossRef]
- Yan, Y.D.; Wang, Y.; Chen, X.Q.; Shi, C.; Yu, J.Z.; Cheng, C. A tendon-driven prosthetic hand using continuum structure. In Proceedings of the 42nd Annual International Conferences of the IEEE Engineering in Medicine and Biology Society: Enabling Innovative Technologies for Global Healthcare EMBC’20, Montreal, QC, Canada, 20–24 July 2020; pp. 4951–4954. [Google Scholar]
- Simone, F.; Rizzello, G.; Seelecke, S.; Motzki, P. A Soft Five-Fingered Hand Actuated by Shape Memory Alloy Wires: Design, Manufacturing, and Evaluation. Front. Robot. AI 2020, 7, 608841. [Google Scholar] [CrossRef] [PubMed]
- Babu, D.; Nasir, A.; Farag, M.; Jabbar, W.A. 3D Printed Prosthetic Robot Arm with Grasping Detection System for Children. Int. J. Adv. Sci. Eng. Inf. Technol. 2023, 13, 226–234. [Google Scholar] [CrossRef]
- Wahit, M.A.A.; Ahmad, S.A.; Marhaban, M.H.; Wada, C.; Izhar, L.I. 3D Printed Robot Hand Structure Using Four-Bar Linkage Mechanism for Prosthetic Application. Sensors 2020, 20, 4174. [Google Scholar] [CrossRef]
- Fonseca, G.; Nunes-Pereira, J.; Silva, A.P. 3D Printed Robotic Hand with Piezoresistive Touch Capability. Appl. Sci. 2023, 13, 8002. [Google Scholar] [CrossRef]
- Akhtar, A. 3D-Printing Hands that Feel. GetMobile Mob. Comput. Commun. 2021, 24, 10–16. [Google Scholar] [CrossRef]
- Zhou, H.; Tawk, C.; Alici, G. A 3D Printed Soft Robotic Hand With Embedded Soft Sensors for Direct Transition Between Hand Gestures and Improved Grasping Quality and Diversity. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 550–558. [Google Scholar] [CrossRef]
- Prakash, A.; Sharma, S. A low-cost transradial prosthesis controlled by the intention of muscular contraction. Phys. Eng. Sci. Med. 2021, 44, 229–241. [Google Scholar] [CrossRef]
- Hussian, J.; Gelani, H.E.; Ahmad, B.; Ali, A.; Rehman, S.; Arshad, W. Design and Development of EMG Controlled Prosthetics Limb with the Self-Charging Capability. In Proceedings of the 2018 International Conference on Power Generation Systems and Renewable Energy Technologies (PGSRET), Islamabad, Pakistan, 10–12 September 2018; pp. 1–4. [Google Scholar] [CrossRef]
- Sheikh, M.A.T.; Pereira, K.P.S.; Gopalakrishna, B.K.; Raju, K. Design and fabrication of automated prosthetic arm. In AIP Conference Proceedings; AIP Publishing: Melville, NY, USA, 2020. [Google Scholar] [CrossRef]
- Sakib, N.; Islam, M.K. Design and Implementation of an EMG Controlled 3D Printed Prosthetic Arm. In Proceedings of the BECITHCON 2019—2019 IEEE International Conference on Biomedical Engineering, Computer and Information Technology for Health, Dhaka, Bangladesh, 28–30 November 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 85–88. [Google Scholar] [CrossRef]
- Bishay, P.; Aguilar, C.; Amirbekyan, A.; Vartanian, K.; Arjon-Ramirez, M.; Pucio, D. Design of a lightweight shape memory alloy stroke-amplification and locking system in a transradial prosthetic arm. In Proceedings of the ASME 2021 Conference on Smart Materials, Adaptive Structures and Intelligent Systems, SMASIS 2021, Virtual Online, 14–15 September 2021; American Society of Mechanical Engineers (ASME): New York City, NY, USA, 2021. [Google Scholar] [CrossRef]
- Imran, A.; Escobar, W.; Barez, F. Design of an Affordable Prosthetic Arm Equipped with Deep Learning Vision-Based Manipulation. In ASME International Mechanical Engineering Congress and Exposition, Proceedings (IMECE); American Society of Mechanical Engineers (ASME): New York City, NY, USA, 2021. [Google Scholar] [CrossRef]
- Dania, A.; Rahman, A.; Hussin, H. Detection of attention and meditation state-based brainwave system to control prosthetic arm. Indones. J. Electr. Eng. Comput. Sci. 2019, 13, 794–800. [Google Scholar] [CrossRef]
- Ali, H.A.; Popescu, D.; Hadar, A.; Vasilateanu, A.; Popa, R.C.; Goga, N.; Qhatan, H.A.D. EEG-based Brain Computer Interface Prosthetic Hand using Raspberry Pi 4. Int. J. Adv. Comput. Sci. Appl. 2021, 12, 44–49. [Google Scholar] [CrossRef]
- Yoshikawa, M.; Ogawa, K.; Yamanaka, S.; Kawashima, N. Finch: Prosthetic Arm With Three Opposing Fingers Controlled by a Muscle Bulge. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Fajardo, J.; Ferman, V.; Cardona, D.; Maldonado, G.; Lemus, A.; Rohmer, E. Galileo hand: An anthropomorphic and affordable upper-limb prosthesis. IEEE Access 2020, 8, 81365–81377. [Google Scholar] [CrossRef]
- Saqib, M.F.; Islam, A.; Bari, M.L.A.; Ahmed, M.S.; Samy, M.A.A. Gesture Controlled Prosthetic Arm with Sensation Sensors. In Proceedings of the 2018 3rd International Conference for Convergence in Technology, I2CT 2018, Pune, India, 6–8 April 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Kenza, A.Z.; Baby, M.; George, M. Implementation of an Efficient Prosthetic Limb Controlled by Electro Myo Graphic(EMG) Signal. In Proceedings of the 2018 International Conference on Emerging Trends and Innovations in Engineering and Technological Research (ICETIETR), Ernalkulam, India, 11–13 July 2018; pp. 1–6. [Google Scholar] [CrossRef]
- Said, S.; Boulkaibet, I.; Sheikh, M.; Karar, A.S.; Alkork, S.; Nait-Ali, A. Machine-Learning-Based Muscle Control of a 3D-Printed Bionic Arm. Sensors 2020, 20, 3144. [Google Scholar] [CrossRef] [PubMed]
- Hussain, I.; Iqbal, Z.; Malvezzi, M.; Seneviratne, L.; Gan, D.; Prattichizzo, D. Modeling and Prototyping of a Soft Prosthetic Hand Exploiting Joint Compliance and Modularity. In Proceedings of the 2018 IEEE International Conference on Robotics and Biomimetics, ROBIO 2018, Kuala Lumpur, Malaysia, 12–15 December 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 65–70. [Google Scholar] [CrossRef]
- De Barrie, D.; Margetts, R.; Goher, K. SIMPA: Soft-Grasp Infant Myoelectric Prosthetic Arm. IEEE Robot. Autom. Lett. 2020, 5, 699–704. [Google Scholar] [CrossRef]
- Hasan, S.; Al-Kandari, K.; Al-Awadhi, E.; Jaafar, A.; Al-Farhan, B.; Hassan, M.; Said, S.; AlKork, S. Wearable mind thoughts controlled open source 3D printed arm with embedded sensor feedback system. In Proceedings of the CHIRA 2018—2nd International Conference on Computer-Human Interaction Research and Applications, Seville, Spain, 19–21 September 2018; SciTePress: Setúbal, Portugal, 2018; pp. 141–149. [Google Scholar] [CrossRef]
- Olsen, N.R.; George, J.A.; Brinton, M.R.; Paskett, M.D.; Kluger, D.T.; Tully, T.N.; Duncan, C.C.; Clark, G.A. An Adaptable Prosthetic Wrist Reduces Subjective Workload. bioRxiv 2019. bioRxiv:1101.808634. [Google Scholar] [CrossRef]
- Ayvali, M.; Wickenkamp, I.; Ehrmann, A. Design, Construction and Tests of a Low-Cost Myoelectric Thumb. Technologies 2021, 9, 63. [Google Scholar] [CrossRef]
- Jabin, J.; Adnan, M.E.; Mahmud, S.S.; Chowdhury, A.M.; Islam, M.R. Low cost 3D printed prosthetic for congenital amputation using flex sensor. In Proceedings of the 2019 5th International Conference on Advances in Electrical Engineering, ICAEE 2019, Dhaka, Bangladesh, 26–28 September 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 821–825. [Google Scholar] [CrossRef]
- Baron, J.; Hazubski, S.; Otte, A. 3D Multi-Material Printing of an Anthropomorphic, Personalized Replacement Hand for Use in Neuroprosthetics Using 3D Scanning and Computer-Aided Design: First Proof-of-Technical-Concept Study. Prosthesis 2020, 2, 362–370. [Google Scholar] [CrossRef]
- Avilés-Mendoza, K.; Gaibor-León, N.G.; Asanza, V.; Lorente-Leyva, L.L.; Peluffo-Ordóñez, D.H. A 3D Printed, Bionic Hand Powered by EMG Signals and Controlled by an Online Neural Network. Biomimetics 2023, 8, 255. [Google Scholar] [CrossRef]
- Chalong, W.; Tanjaipet, S.; Eurcherdkul, P.; Chuckpaiwong, I. A Force-controlled Three-fnger Prosthetic Hand via Three-Dimensional Printing. In IOP Conference Series: Materials Science and Engineering; Institute of Physics Publishing: Bristol, UK, 2020. [Google Scholar] [CrossRef]
- Castro, M.C.F.; Pinheiro, W.C.; Rigolin, G. A Hybrid 3D Printed Hand Prosthesis Prototype Based on sEMG and a Fully Embedded Computer Vision System. Front. Neurorobotics 2022, 15, 751282. [Google Scholar] [CrossRef]
- Cutipa-Puma, D.R.; Coaguila-Quispe, C.G.; Yanyachi, P.R. A low-cost robotic hand prosthesis with apparent haptic sense controlled by electroencephalographic signals. HardwareX 2023, 14, e00439. [Google Scholar] [CrossRef]
- Prakash, A.; Sharma, S. A low-cost system to control prehension force of a custom-made myoelectric hand prosthesis. Res. Biomed. Eng. 2020, 36, 237–247. [Google Scholar] [CrossRef]
- Prakash, A.; Kumari, B.; Sharma, S. A low-cost, wearable sEMG sensor for upper limb prosthetic application. J. Med. Eng. Technol. 2019, 43, 235–247. [Google Scholar] [CrossRef] [PubMed]
- Furui, A.; Eto, S.; Nakagaki, K.; Shimada, K.; Nakamura, G.; Masuda, A.; Chin, T.; Tsuji, T. A myoelectric prosthetic hand with muscle synergy-based motion determination and impedance model-based biomimetic control. Sci. Robot. 2019, 4, aaw6339. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, A.; Lavranos, J.; Tan, Y.; Choong, P.; Oetomo, D. A Paediatric 3D-Printed Soft Robotic Hand Prosthesis for Children with Upper Limb Loss. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, Montreal, QC, Canada, 20–24 July 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020; pp. 3310–3313. [Google Scholar] [CrossRef]
- Ccorimanya, L.; Hassan, M.; Watanabe, R.; Ueno, T.; Hada, Y.; Suzuki, K. A Personalized 3D-Printed Hand Prosthesis for Early Intervention in Children With Congenital Below-Elbow Deficiency: User-Centered Design Case Study. IEEE Access 2023, 11, 50235–50251. [Google Scholar] [CrossRef]
- Mohammadi, A.; Lavranos, J.; Zhou, H.; Mutlu, R.; Alici, G.; Tan, Y.; Choong, P.; Oetomo, D. A practical 3D-printed soft robotic prosthetic hand with multi-articulating capabilities. PLoS ONE 2020, 15, e0232766. [Google Scholar] [CrossRef]
- Toro-Ossaba, A.; Tejada, J.C.; Rúa, S.; López-González, A. A Proposal of Bioinspired Soft Active Hand Prosthesis. Biomimetics 2023, 8, 29. [Google Scholar] [CrossRef]
- Deng, E.; Tadesse, Y. A soft 3d-printed robotic hand actuated by coiled sma. Actuators 2021, 10, 6. [Google Scholar] [CrossRef]
- Leung, E.; Wilkerson, S.A. An Interdisciplinary Myoelectric Prosthetic Hand Capstone Project. In Proceedings of the ASEE Annual Conference and Exposition, Conference Proceedings, Baltimore, MD, USA, 25–28 June 2023; American Society for Engineering Education: Washington, DC, USA, 2023. Available online: https://peer.asee.org/42633 (accessed on 24 October 2023).
- Ke, A.; Huang, J.; He, J. An underactuated prosthetic hand with coupled metacarpophalangeal joints. J. Adv. Comput. Intell. Intell. Inform. 2018, 22, 674–682. [Google Scholar] [CrossRef]
- Ariyanto, M.; Ismail, R.; Setiawan, J.D.; Yuandi, E.P. Anthropomorphic transradial myoelectric hand using tendon-spring mechanism. Telkomnika 2019, 17, 537–548. [Google Scholar] [CrossRef]
- Lunguţ, E.F.; Matei, L.; Roşu, M.M.; Iliescu, M.; Radu, C. Biomechanical Hand Prosthesis Design. Machines 2023, 11, 964. [Google Scholar] [CrossRef]
- Radu, C.; Roșu, M.M.; Matei, L.; Ungureanu, L.M.; Iliescu, M. Concept, Design, Initial Tests and Prototype of Customized Upper Limb Prosthesis. Appl. Sci. 2021, 11, 3077. [Google Scholar] [CrossRef]
- Mühlbauer, P.; Löhnert, L.; Siegle, C.; Stewart, K.W.; Pott, P.P. Demonstrator of a Low-Cost Hand Prosthesis. In IFAC-PapersOnLine; Elsevier: Amsterdam, The Netherlands, 2020; pp. 15998–16003. [Google Scholar] [CrossRef]
- Nihal, R.A.; Broti, N.M.; Deowan, S.A.; Rahman, S. Design and Development of an Anthropomorphic Robotic Hand Using TPU Material. In Proceedings of the ICIET 2019—2nd International Conference on Innovation in Engineering and Technology, Dhaka, Bangladesh, 23–24 December 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Venkatesh, B.; Kumar, M.A. Design and development of wireless operated low cost prosthetic hand by fused deposition modeling. Int. J. Mech. Prod. Eng. Res. Dev. 2018, 8, 393–398. [Google Scholar] [CrossRef]
- Rahmatillah, A.; Salamat, L.; Soelistiono, S. Design and Implementation of Prosthetic Hand Control Using Myoelectric Signal. Int. J. Adv. Sci. Eng. Inf. Technol. 2019, 9, 1231–1237. [Google Scholar] [CrossRef]
- Setty, K.; Van Niekerk, T.; Stopforth, R. Design Considerations of the Touch Hand 4. In Procedia CIRP; Elsevier: Amsterdam, The Netherlands, 2020; pp. 494–502. [Google Scholar] [CrossRef]
- Pontim, C.E.; Alves, M.G.; Júnior, J.J.A.M.; Campos, D.P.; Setti, J.A.P. Development of Bionic Hand Using Myoelectric Control for Transradial Amputees. In IFMBE Proceedings; Springer Science and Business Media: Berlin/Heidelberg, Germany, 2022; pp. 1445–1449. [Google Scholar] [CrossRef]
- Puruhita, S.T.; Satria, N.F.; Hanafi, N.; Kusumawati, E. Development of Teleoperation Humanoid Robot Hand Mimicking Through Human Hand Movement. In Proceedings of the 2020 International Electronics Symposium (IES), Surabaya, Indonesia, 29–30 September 2020; pp. 277–283. [Google Scholar] [CrossRef]
- Zhang, X.; Zhu, T.; Yamayoshi, I.; Hong, D. Dexterity, Sensitivity and Versatility: An Under Actuated Robotic Hand with Mechanical Intelligence and Proprioceptive Actuation. Int. J. Humanoid Robot. 2020, 17, 2050006. [Google Scholar] [CrossRef]
- Farooq, U.; Ghani, U.; Usama, S.A.; Neelum, Y.S. EMG control of a 3D printed myo electric prosthetic hand. In IOP Conference Series: Materials Science and Engineering; Institute of Physics Publishing: Bristol, UK, 2019. [Google Scholar] [CrossRef]
- Tian, L.; Li, H.; Halil, M.F.K.B.A.; Thalmann, N.M.; Thalmann, D.; Zheng, J. Fast 3D Modeling of Anthropomorphic Robotic Hands Based on A Multi-layer Deformable Design. arXiv 2020, arXiv:2011.03742. [Google Scholar] [CrossRef]
- Dunai, L.; Novak, M.; García, C. Espert Human Hand Anatomy-Based Prosthetic Hand. Sensors 2020, 21, 137. [Google Scholar] [CrossRef]
- Omar, S.; Kasem, A.; Ahmad, A.; Ya’akub, S.R.; Ahman, S.; Yunus, E. Implementation of Low-Cost 3D-Printed Prosthetic Hand and Tasks-Based Control Analysis. In Computational Intelligence in Information Systems; Omar, S., Haji Suhaili, W.S., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 213–223. [Google Scholar] [CrossRef]
- Leal-Naranjo, J.-A.; Miguel, C.-R.T.-S.; Ceccarelli, M.; Rostro-Gonzalez, H. Mechanical Design and Assessment of a Low-Cost 7-DOF Prosthetic Arm for Shoulder Disarticulation. Appl. Bionics Biomech. 2018, 2018, 4357602. [Google Scholar] [CrossRef]
- Torres-Sanmiguel, C.R. Modeling and Simulation Process via Incremental Methods of a Production-Aimed Upper Limb Prosthesis. Appl. Sci. 2022, 12, 2788. [Google Scholar] [CrossRef]
- Crosby, K.; Robinette, P.; Rhodes, A. Myoelectric Control of Prosthetics and Robotics. In Proceedings of the National Conference On Undergraduate Research (NCUR) 2019, Kennesaw, GA, USA, 11–13 April 2019. [Google Scholar]
- Bharathan, A.; Premkumar, J.; Sudhakar, T.; Janney, J.B.; Sindu. Prosthetic Arm with Functional Fingers and Wireless Recharge on Walk Function. J. Phys. Conf. Ser. 2022, 2318, 012025. [Google Scholar] [CrossRef]
- Herbst, Y.; Polinsky, S.; Fischer, A.; Medan, Y.; Schneor, R.; Kahn, J.; Wolf, A. Scan-Driven Fully-Automated Pipeline for a Personalized, 3D Printed Low-Cost Prosthetic Hand. In Proceedings of the IEEE International Conference on Automation Science and Engineering, Lyon, France, 23–27 August 2021; IEEE Computer Society: Washington, DC, USA, 2021; pp. 183–188. [Google Scholar] [CrossRef]
- Esposito, D.; Savino, S.; Andreozzi, E.; Cosenza, C.; Niola, V.; Bifulco, P. The ‘Federica’ Hand. Bioengineering 2021, 8, 128. [Google Scholar] [CrossRef]
- Ismail, R.; Ariyanto, M.; Wicaksono, L.R.; Ispramuditya, A.; Putri, F.T. The design and analysis of low-cost myoelectric hand using six-bar linkage mechanism. Asia-Pac. J. Sci. Technol. 2022, 27, 1–15. [Google Scholar] [CrossRef]
- Weiner, P.; Starke, J.; Hundhausen, F.; Beil, J.; Asfour, T. The KIT Prosthetic Hand: Design and Control. In Proceedings of the IEEE International Conference on Intelligent Robots and Systems, Madrid, Spain, 1–5 October 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 3328–3334. [Google Scholar] [CrossRef]
- Moodley, K.; Fourie, J.; Imran, Z.; Hands, C.; Rall, W.; Stopforth, R. Touch Hand 4.5: Low-cost additive manufacturing prosthetic hand participated in Cybathlon 2020 ARM discipline. J. Neuroeng. Rehabil. 2022, 19, 130. [Google Scholar] [CrossRef] [PubMed]
- Sreenivasan, N.; Gutierrez, D.F.U.; Bifulco, P.; Cesarelli, M.; Gunawardana, U.; Gargiulo, G.D. Towards Ultra Low-Cost Myoactivated Prostheses. BioMed Res. Int. 2018, 2018, 9634184. [Google Scholar] [CrossRef] [PubMed]
- Blystad, L.C.; Ohlckers, P.; Marchetti, L.; Franti, E.; Dascalu, M.; Ionescu, O.; Dobrescu, D.; Dobrescu, L.; Niculae, C.; Dragomir, D.C.; et al. Bidirectional neuroprosthesis system integration. In Proceedings of the 2020 IEEE 8th Electronics System-Integration Technology Conference (ESTC), Tønsberg, Norway, 15–18 September 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 1–7. [Google Scholar] [CrossRef]
- Abarca, V.E.; Flores, K.M.; Elías, D. The Octa Hand: An Affordable Multi-Grasping 3D-Printed Robotic Prosthesis for Transradial Amputees. In Proceedings of the 2019 5th International Conference on Control, Automation and Robotics (ICCAR), Beijing, China, 19–22 April 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 92–97. [Google Scholar] [CrossRef]
- Tian, L.; Zheng, J.; Cai, Y.; Abdul-Halil, M.F.K.; Thalmann, N.M.; Thalmann, D.; Li, H. Fast 3D Modeling of Prosthetic Robotic Hands Based on a Multi-Layer Deformable Design. Int. J. Bioprint. 2021, 8, 406. [Google Scholar] [CrossRef]
- Butin, C.; Chablat, D.; Aoustin, Y.; Gouaillier, D. Novel Kinematics of an Anthropomorphic Prosthetic Hand Allowing Lateral and Opposite Grasp With a Single Actuator. J. Comput. Nonlinear Dyn. 2023, 18, 061005. [Google Scholar] [CrossRef]
- Vazquez, O.; Alfaro-Ponce, M.; Chairez, I.; Arteaga-Ballesteros, B. Design and Development of 3D Printed Electromyographic Upper Limb Prosthesis. In VIII Latin American Conference on Biomedical Engineering and XLII National Conference on Biomedical Engineering; Diaz, C.A.G., Gonzalez, C.C., Leber, E.L., Velez, H.A., Puente, N.P., Flores, D.L., Andrade, A.O., Galvan, H.A., Martinez, F., Garcia, R., et al., Eds.; Springer: Cham, Switzerland, 2020; pp. 985–992. [Google Scholar] [CrossRef]
- da Silva, B.B.; Porsani, R.N.; Hellmeister, L.A.V.; Medola, F.O.; Paschoarelli, L.C. Design and Development of a Myoelectric Upper Limb Prosthesis with 3D Printing: A Low-Cost Alternative. In Advances in Additive Manufacturing, Modeling Systems and 3D Prototyping; DiNicolantonio, M., Rossi, E., Alexander, T., Eds.; Springer: Cham, Switzerland, 2020; pp. 318–327. [Google Scholar] [CrossRef]
- Górski, F.; Marciniak, A.; Wichniarek, R.; Kuczko, W.; Zukowska, M.; Rybarczyk, J. Development of 3D Printed Low-Cost Individualized Actuated Upper Limb Prostheses. In Advances In Manufacturing IV; Gorski, F., Pacurar, R., Gonzalez, J.F.R., Rychlik, M., Eds.; Manufacturing 2024; Springer: Cham, Switzerland, 2024; Volume 5, pp. 179–192. [Google Scholar] [CrossRef]
- Carter-Davies, D.; Chen, J.S.; Chen, F.; Li, M.; Yang, C.G. Mechatronic Design and Control of a 3D Printed Low Cost Robotic Upper Limb. In Proceedings of the 2018 11th International Workshop on Human Friendly Robotics (HFR), Shenzhen, China, 13–14 November 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 1–6. [Google Scholar] [CrossRef]
- Unanyan, N.N.; Belov, A.A. A Prototype of a Myoelectric Upper-Limb Prosthesis Constructed Using Additive Technologies. Biomed. Eng. 2022, 55, 303–307. [Google Scholar] [CrossRef]
- Tan, Y.X.; Zheng, Y.; Li, X.X.; Li, G.L. Structural Design and Control of a Multi-degree-of-freedom Modular Bionic Arm Prosthesis. In Intelligent Robotics and Applications (ICIRA 2022); Liu, H., Yin, Z., Liu, L., Jiang, L., Gu, G., Wu, X., Ren, W., Eds.; PT II; Springer: Cham, Switzerland, 2022; pp. 689–698. [Google Scholar] [CrossRef]
- Diego, J.R.R.; Martinez, D.W.C.; Robles, G.S.; Dizon, J.R.C. Development of Smartphone-Controlled Hand and Arm Exoskeleton for Persons with Disability. Open Eng. 2020, 11, 161–170. [Google Scholar] [CrossRef]
- Kansal, S.; Garg, D.; Upadhyay, A.; Mittal, S.; Talwar, G.S. DL-AMPUT-EEG: Design and development of the low-cost prosthesis for rehabilitation of upper limb amputees using deep-learning-based techniques. Eng. Appl. Artif. Intell. 2023, 126, 106990. [Google Scholar] [CrossRef]
- Roy, D.P.; Chowdhury, M.Z.A.; Afrose, F.; Hoque, M.E. IEEE Design and Development of a Cost-effective Prosthetic Hand for Upper Limb Amputees. In Proceedings of the 13th Biomedical Engineering International Conference (BMEICON 2021), Ayutthaya, Thailand, 19–21 November 2018. [Google Scholar] [CrossRef]
- Ccorimanya, L.; Watanabe, R.; Hassan, M.; Hada, Y.; Suzuki, K. Design of a myoelectric 3D-printed prosthesis for a child With upper limb congenital amputation. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 5394–5398. [Google Scholar] [CrossRef]
- Herbst, Y.; Sivakumaran, D.; Medan, Y.; Wolf, A. A Low-Cost 3D Printed Prosthetic Hand with a Sensory Feedback Interface. In Proceedings of the 2022 9th IEEE RAS/EMBS International Conference on Biomedical Robotics and Biomechatronics (BIOROB 2022), Seoul, Republic of Korea, 21–24 August 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022; pp. 1–6. [Google Scholar] [CrossRef]
- Parkhomenko, A.; Gladkova, O.; Zalyubovskiy, Y. Investigation and Realisation of Prototyping Technologies for Robotic-Prostheses Computer Aided Design. In Proceedings of the 2019 IEEE 15th International Conference on the Experience of Designing and Application of CAD Systems (CADSM’2019), Polyana, Ukraine, 26 February–2 March 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Gyllinsky, J.V.; Gannon, J.; Akoiwala, C.; Witcher, C.R.; Parra, L.; Baez, J.; Frink, T.; Driscoll, B.; Orduz, J.; Aguanche, Z.C.; et al. Patient Self-assessment of 3D Printed Upper-extremity Prosthetics. In Proceedings of the 2019 IEEE International Conference on Smart Computing (SMARTCOMP 2019), Washington, DC, USA, 12–15 June 2019; pp. 205–207. [Google Scholar] [CrossRef]
- Mohammadi, A.; Lavranos, J.; Choong, P.; Oetomo, D. X-Limb: A Soft Prosthetic Hand with User-Friendly Interface. In Converging Clinical and Engineering Research on Neurorehabilitation III; Masia, L., Micera, S., Akay, M., Pons, J.L., Eds.; Springer: Cham, Switzerland, 2019; pp. 82–86. [Google Scholar] [CrossRef]
- Manero, A.; Sparkman, J.; Dombrowski, M.; Smith, P.; Senthil, P.; Smith, S.; Rivera, V.; Chi, A. Evolving 3D-Printing Strategies for Structural and Cosmetic Components in Upper Limb Prosthesis. Prosthesis 2023, 5, 167–181. [Google Scholar] [CrossRef]
- Mick, S.; Lapeyre, M.; Rouanet, P.; Halgand, C.; Benois-Pineau, J.; Paclet, F.; Cattaert, D.; Oudeyer, P.Y.; De Rugy, A. Reachy, a 3D-Printed Human-Like Robotic Arm as a Testbed for Human-Robot Control Strategies. Front. Neurorobotics 2019, 13, 65. [Google Scholar] [CrossRef]
- Bishay, P.L.; Fontana, J.; Raquipiso, B.; Rodriguez, J.; Boretta, J.M.; Enos, B.; Gay, T.; Mauricio, K. Development of a biomimetic transradial prosthetic arm with shape memory alloy muscle wires. Eng. Res. Express 2020, 2, e035041. [Google Scholar] [CrossRef]
- Bardien, M.A.; Sivarasu, S. ASME the Self Actuated Tenim Hand: The Conversion of a Body-Driven Prosthesis to an Electromechanically Actuated Device. In Proceedings of the 2021 Design of Medical Devices Conference (DMD2021), Minneapolis, MN, USA, 12–15 April 2021. [Google Scholar]
- O’Brien, L.; Cho, E.; Khara, A.; Lavranos, J.; Lommerse, L.; Chen, C. 3D-printed custom-designed prostheses for partial hand amputation: Mechanical challenges still exist. J. Hand Ther. 2021, 34, 539–542. [Google Scholar] [CrossRef]
- Răduică, F.F.; Simion, I. Development of a Low-Cost 3D-Printed Upper Limb Prosthetic Device with Hybrid Actuation for Partial Hand Amputees. Appl. Sci. 2024, 14, 8929. [Google Scholar] [CrossRef]
- Liu, S.; Van, M.; Chen, Z.; Angeles, J.; Chen, C. A novel prosthetic finger design with high load-carrying capacity. Mech. Mach. Theory 2021, 156, 104121. [Google Scholar] [CrossRef]
- Ryu, W.; Choi, Y.; Choi, Y.J.; Lee, S. Development of a Lightweight Prosthetic Hand for Patients with Amputated Fingers. Appl. Sci. 2020, 10, 3536. [Google Scholar] [CrossRef]
- da Silva, A.B.S.; Mendes, G.E.P.; Bragato, E.S.; Novelli, G.L.; Monjardim, M.; Andrade, R.M. Finger Prosthesis Driven by DEA Pairs as Agonist-Antagonist Artificial Muscles. Biomimetics 2024, 9, 110. [Google Scholar] [CrossRef]
- Navaraj, W.T.; Nassar, H.; Dahiya, R. Prosthetic Hand with Biomimetic Tactile Sensing and Force Feedback. In Proceedings of the 2019 IEEE International Symposium on Circuits and Systems (ISCAS), Sapporo, Japan, 26–29 May 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 1–4. [Google Scholar] [CrossRef]
- Ige, E.O.; Adetunla, A.; Awesu, A.; Ajayi, O.K. Sensitivity Analysis of a Smart 3D-Printed Hand Prosthetic. J. Robot. 2022, 2022, 9145352. [Google Scholar] [CrossRef]
- Urriolagoitia-Sosa, G.; Romero-Ángeles, B.; Díaz-León, C.; Gallegos-Funes, F.J.; Martínez-Reyes, J.; Vargas-Bustos, J.A.; Urriolagoitia-Calderón, G. Hand prosthesis prototype construction with the implementation of phalanges through 3D printing technology. Prog. Addit. Manuf. 2023, 8, 681–692. [Google Scholar] [CrossRef]
- Salazar, M.; Rosero, R.; Zambrano, O.; Portero, P. Impact of 3D printing technology for the construction of a prototype of low-cost robotic arm prostheses. Adv. Mech. Eng. 2024, 16, 1–17. [Google Scholar] [CrossRef]
- Shibanoki, T.; Jin, K. A 3D-printable Prosthetic Hand Based on a Dual-arm Operation Assistance Model. In Proceedings of the 2021 IEEE 3rd Global Conference on Life Sciences and Technologies (IEEE Lifetech 2021), Nara, Japan, 9–11 March 2021; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2021; pp. 133–134. [Google Scholar] [CrossRef]
- Bangera, U.M.; Pinto, R.; Pais, C.A.; Tauro, S.H.; Binu, K.G. Design and Development of Controlled Arm Using Electromyographic Signals. In Emerging Trends in Mechanical Engineering 2018; Gopalakrishna, B.K., Mudradi, S., Eds.; AIP Publishing: Melville, NY, USA, 2019. [Google Scholar] [CrossRef]
- Medina-Coello, P.; Salvador-Domínguez, B.; Badesa, F.J.; Corral, J.M.R.; Plastrotmann, H.; Morgado-Estévez, A. Anthropomorphic Robotic Hand Prosthesis Developed for Children. Biomimetics 2024, 9, 401. [Google Scholar] [CrossRef]
- Arthaya, B.; Ivan, V. Preliminary Design of 3D Printing Prosthetic Hand. J. Adv. Manuf. Syst. 2023, 22, 67–84. [Google Scholar] [CrossRef]
- Xu, C.C.; Dong, S.; Ma, Y.F.; Zhan, J.W.; Wang, Y.C.; Wang, X.J. A Self-sensing TSA-actuated Anthropomorphic Robot Hand. J Bionic Eng. 2024, 21, 1174–1190. [Google Scholar] [CrossRef]
- Votta, A.M.; Günay, S.V.; Zylich, B.; Skorina, E.; Rameshwar, R.; Erdoğmuş, D.; Onal, C.D. Kinematic Optimization of an Underactuated Anthropomorphic Prosthetic Hand. In Proceedings of the 2020 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Las Vegas, NV, USA, 24 October–24 January 2021; pp. 3397–3403. [Google Scholar] [CrossRef]
- Zhou, H.; Tawk, C.; Alici, G. A 3D Printed Soft Prosthetic Hand with Embedded Actuation and Soft Sensing Capabilities for Directly and Seamlessly Switching Between Various Hand Gestures. In Proceedings of the 2021 IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM), Delft, The Netherlands, 12–16 July 2021; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2021; pp. 75–80. [Google Scholar] [CrossRef]
- Mio, R.; Bustamante, M.; Salazar, G.; Elias, D.A. A 3D-Printed Prosthetic Hand with Modular Reconfigurable Fingers. In Interdisciplinary Applications of Kinematics; Kecskemethy, A., Flores, F.G., Carrera, E., Elias, D.A., Eds.; Springer: Cham, Switzerland, 2019; pp. 93–102. [Google Scholar] [CrossRef]
- Patel, K.; Magee, K.; Hoover, B.; Yu, J.; Ashuri, T.; Moghadam, A.A.A. Development of Robotic Hand with Novel Soft 3D Printed Actuators. In Proceedings of the ASME 2023 International Mechanical Engineering Congress and Exposition, IMECE2023, New Orleans, LA, USA, 29 October–2 November 2023; Volume 5. [Google Scholar] [CrossRef]
- Kocejko, T.; Weglerski, R.; Zubowicz, T.; Ruminski, R.; Wtorek, J.; Arminski, K. Design aspects of a low-cost prosthetic arm for people with severe movement disabilities. In Proceedings of the 2020 13th International Conference on Human System Interaction (HSI), Tokyo, Japan, 6–8 June 2020; pp. 295–299. [Google Scholar] [CrossRef]
- Ahsan, M.S.; Hasan, K.M. Design and Development of an Electromyography Sensor Actuated Prosthetic Arm. Lat. Am. Appl. Res. Int. J. 2022, 52, 191–200. [Google Scholar] [CrossRef]
- Liu, S.Q.; Zhang, H.B.; Yin, R.X.; Chen, A.; Zhang, W.J. Flexure Hinge Based Fully Compliant Prosthetic Finger. In Proceedings of theSAI Intelligent Systems Conference (INTELLISYS) 2016, London, UK, 21–22 September 2016; Bi, Y., Kapoor, S., Bhatia, R., Eds.; Springer: Cham, Switzerland, 2018; Volume 2, pp. 839–849. [Google Scholar] [CrossRef]
- D’Almeida, H.; Almeida, P.; Charters, T.; Mendes, M. Electro-pneumatic Control of Soft Robotic Hand Prosthesis Actuators. In Proceedings of the 2019 6th IEEE Portuguese Meeting in Bioengineering (ENBENG), Lisbon, Portugal, 22–23 February 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 1–4. [Google Scholar] [CrossRef]
- Bachtiar, Y.; Pristovani, R.D.; Dewanto, S.; Pramadihanto, D. Mechanical and Forward Kinematic Analysis of Prosthetic Robot Hand for T-FLoW 3.0. In Proceedings of the 2018 International Electronics Symposium on Engineering Technology and Applications (IES-ETA), Bali, Indonesia, 29–30 October 2018; pp. 275–280. [Google Scholar] [CrossRef]
- Dellagostin, J.; Cukla, A.; Bisogno, F.; Sales, R.; Strapazzon, L.; Salvador, G. Predicting the Movement Intention and Controlling the Grip of a Myoelectrical Active Prosthetic Arm. In Intelligent Systems Design and Applications; ISDA 2021; Abraham, A., Gandhi, N., Hanne, T., Hong, T.P., Rios, T.N., Ding, W., Eds.; Springer: Cham, Switzerland, 2022; pp. 1098–1109. [Google Scholar] [CrossRef]
- Mayyas, M.; Mamidala, I. Prosthetic finger based on fully compliant mechanism for multi-scale grasping. Microsyst. Technol. 2021, 27, 2131–2145. [Google Scholar] [CrossRef]
- Chandak, K.; Sanadhya, A.; Gohil, J.; Trivedi, R.; Parikh, P.; Chauhan, M.; Patel, K.; Prajapati, H. Electromyography operated soft finger-like actuator for prosthesis. In International Journal of Interactive Design and Manufacturing—IJIDEM; Springer Nature: Berlin/Heidelberg, Germany, 2024. [Google Scholar] [CrossRef]
- Votta, A.M.; Günay, S.Y.; Erdogmus, D.; Önal, C. Force-Sensitive Prosthetic Hand with 3-axis Magnetic Force Sensors. In Proceedings of the 2019 IEEE International Conference on Cyborg and Bionic Systems (CBS), Munich, Germany, 18–20 September 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 104–109. [Google Scholar] [CrossRef]
- Nguyen, P.D.; Pham, C.T. Towards a modular and dexterous transhumeral prosthesis based on bio-signals and active vision. In Proceedings of the 2019 IEEE International Symposium on Measurement and Control in Robotics (ISMCR): Robotics for the Benefit of Humanity, Houston, TX, USA, 19–21 September 2019; Harman, T.L., Taqvi, Z., Eds.; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Sureshbabu, A.V.; Rass, D.; Zimmermann, M. A Lightweight Transradial Hand Prosthesis with a Variable Position Thumb and Thermoregulation. In Proceedings of the 2019 19th International Conference on Advanced Robotics (ICAR), Belo Horizonte, Brazil, 2–6 December 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 61–68. [Google Scholar] [CrossRef]
- Setty, K.; Van Niekerk, T.; Stopforth, R.; Sewsunker, K.; Plessis, A.D. Design and Kinematic Analysis of a Multi-Grip Hand—Touch Hand 4. Int. J. Mech. Eng. Robot. Res. 2022, 11, 466–478. [Google Scholar] [CrossRef]
- Tasar, B.; Gülten, A.; Yakut, O. Design and manufacturing of 15 DOF myoelectric controlled prosthetic hand. Pamukkale Univ. J. Eng. Sci. 2020, 26, 884–892. [Google Scholar] [CrossRef]
- Liu, L.J.; Sun, N.; Li, K. System Design and Kinematic Analysis of a Dexterous Hand with Humanoid Characteristics. In Proceedings of the 2024 WRC Symposium on Advanced Robotics and Automation, WRC SARA, Beijing, China, 23 August 2024; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2024; pp. 163–169. [Google Scholar] [CrossRef]
- Teng, Z.C.; Xu, G.H.; Liang, R.H.; Li, M.; Zhang, S.C.; Chen, J.Z.; Han, C.C. Design of an Underactuated Prosthetic Hand with Flexible Multi-Joint Fingers and EEG-Based Control. In Proceedings of the 2018 IEEE International Conference on Cyborg and Bionic Systems (CBS), Shenzhen, China, 25–27 October 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 647–651. [Google Scholar] [CrossRef]
- Rochez, J.; Woodruff, I.; Rogers, M.; Alba-Flores, R. Classifying Hand Gestures using Artificial Neural Networks for a Robotic Application. In Proceedings of the 2019 IEEE SOUTHEASTCON, Huntsville, AL, USA, 11–14 April 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 1–5. [Google Scholar] [CrossRef]
- Ryu, W.; Kim, D.; Choi, Y.; Lee, S. Development of Prosthetic Finger with Actuator. In Proceedings of the 2019 16th International Conference on Ubiquitous Robots (UR), Jeju, Republic of Korea, 24–27 June 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 313–318. [Google Scholar] [CrossRef]
- Chan, Y.; Tse, Z.T.H.; Ren, H.L. Printable Kirigami-inspired Flexible and Soft Anthropomorphic Robotic Hand. J. Bionic Eng. 2022, 19, 668–677. [Google Scholar] [CrossRef]
- Rocha, R.P.; Lopes, P.A.; de Almeida, A.T.; Tavakoli, M.; Majidi, C. Fabrication and characterization of bending and pressure sensors for a soft prosthetic hand. J. Micromechanics Microengineering 2018, 28, 034001. [Google Scholar] [CrossRef]
- Nikafrooz, N.; Leonessa, A. A Single-Actuated, Cable-Driven, and Self-Contained Robotic Hand Designed for Adaptive Grasps. Robotics 2021, 10, 109. [Google Scholar] [CrossRef]
- Teng, Z.C.; Xu, G.H.; Liang, R.H.; Li, M.; Zhang, S.C.; Tao, T.F. A Novel Underactuated Robotic Finger with Variable Stiffness Joints. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 5305–5309. [Google Scholar] [CrossRef]
- Baqer, I.A.; Soud, W.A.; Ahmed, M.R. Design optimisation for a novel underactuated robotic finger by genetic algorithms. Aust. J. Mech. Eng. 2020, 20, 397–405. [Google Scholar] [CrossRef]
- Joo, S.Y.; Cho, Y.S.; Seo, J.; Seo, Y.; Yi, S.; Seo, C.H. Motion-Mimicking Robotic Finger Prosthesis for Burn-induced Partial Hand Amputee: A Case Report. J. Burn. Care Res. 2024, 46, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Guo, K.; Lu, J.X.; Yang, H.B. Simulation and experimental study on rope driven artificial hand and driven motor. Technol. Health Care 2024, 32, S287–S297. [Google Scholar] [CrossRef] [PubMed]
- Bishay, P.L.; Wilgus, J.; Chen, R.R.; Valenzuela, D.; Medina, V.; Tan, C.; Ittner, T.; Caldera, M.; Rubalcava, C.; Safarian, S.; et al. Controlling a Below-the-Elbow Prosthetic Arm Using the Infinity Foot Controller. Prosthesis 2023, 5, 1206–1231. [Google Scholar] [CrossRef]
- Joochim, C.; Siriwatcharakul, N. Artificial Human Arm Controlled by Muscle Electromyography (EMG). In Proceedings of the 2018 Third International Conference on Engineering Science and Innovative Technology (ESIT), North Bangkok, Thailand, 19–22 April 2018. [Google Scholar] [CrossRef]
- Artal-Sevil, J.S.; Acón, A.; Montañés, J.L.; Domínguez, J.A. Design of a Low-Cost Robotic Arm controlled by Surface EMG Sensors. In Proceedings of the 2018 XIII Technologies Applied to Electronics Teaching Conference (TAEE), La Laguna, Spain, 20–22 June 2018; pp. 1–8. [Google Scholar] [CrossRef]
- Shibanoki, T.; Jin, K.; Maeda, M. An EMG- Based Teleoperation System with Small Hand Based on a Dual-Arm Task Model. In Proceedings of the 2023 8th International Conference on Control and Robotics Engineering, ICCRE, Niigata, Japan, 21–23 April 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 40–43. [Google Scholar] [CrossRef]
- Yurova, V.A.; Velikoborets, G.; Vladyko, A. Design and Implementation of an Anthropomorphic Robotic Arm Prosthesis. Technologies 2022, 10, 103. [Google Scholar] [CrossRef]
- Ahsan, M.S.; Hasan, K.M. Development of Noninvasive Electroencephalogram Brain Sensor Actuated Motorized Prosthetic Arm to Support Disabled People. In Proceedings of the International Conference on Electronics, Communications and Information Technology 2021 (ICECIT 2021), Khulna, Bangladesh, 14–16 September 2021; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2021; pp. 1–4. [Google Scholar] [CrossRef]
- Esposito, D.; Savino, S.; Cosenza, C.; Andreozzi, E.; Gargiulo, G.D.; Polley, C.; Cesarelli, G.; D’Addio, G.; Bifulco, P. Evaluation of Grip Force and Energy Efficiency of the ‘Federica’ Hand. Machines 2021, 9, 25. [Google Scholar] [CrossRef]
- Jing, X.B.; Yong, X.; Tian, L.; Togo, S.; Jiang, Y.; Yokoi, H.; Li, G. Development of Tendon Driven Under-Actuated Mechanism Applied in an EMG Prosthetic Hand with Three Major Grasps for Daily Life. In Proceedings of the 2018 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Madrid, Spain, 1–5 October 2018; Maciejewski, A.A., Okamura, A., Bicchi, A., Stachniss, C., Song, D.Z., Lee, D.H., Chaumette, F., Ding, H., Li, J.S., Wen, J., et al., Eds.; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 2774–2779. [Google Scholar] [CrossRef]
- Prakash, A.; Sharma, N.; Sharma, S. An affordable transradial prosthesis based on force myography sensor. Sens. Actuators A Phys. 2021, 325, 112699. [Google Scholar] [CrossRef]
- Attaoui, A.; Naifar, S.; Bradai, S.; Atitallah, B.B.; Kanoun, O. Design and fabrication of an affordable, high-performance life-size humanoid robotic hand with integrated nanocomposite strain sensors. Int. J. Adv. Manuf. Technol. 2024, 136, 1363–1378. [Google Scholar] [CrossRef]
- Belford, A.; Moshizi, S.A.; Razmjou, A.; Asadnia, M. Using Miniaturized Strain Sensors to Provide a Sense of Touch in a Humanoid Robotic Arm. Front. Mech. Eng. 2020, 6, 550328. [Google Scholar] [CrossRef]
- Guevara-Roselló, J.; Murillo-Aldecoba, J.E. Development of electric hand prothesis controlled by voice commands and muscle sensors. Tecnol. En Marcha 2024, 37, 103–109. [Google Scholar] [CrossRef]
- Sahbel, A.; Nasif, A.; Magdy, A.; Elaydi, M.; Sobhy, N.; Abbas, A. A Low-Cost Lightweight Prosthetic Arm with Soft Gripping Fingers Controlled Using CNN. In Proceedings of the 2024 14th International Conference on Electrical Engineering, ICEENG 2024, Cairo, Egypt, 21–23 May 2024; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2024; pp. 145–147. [Google Scholar] [CrossRef]
- Zhao, R.; Chen, O. NeuroLimbAI: Enhancing Sensory Feedback in an Origami Inspired Prosthetic Arm with Electroencephalogram-Controlled Noninvasive Vibrotactile Haptic Feedback. In Proceedings of the 2024 4th International Conference on Applied Artificial Intelligence, ICAPAI, Halden, Norway, 16 April 2024; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2024; pp. 1–7. [Google Scholar] [CrossRef]
- Zhou, H.; Mohamtnadi, A.; Oetomo, D.; Alici, G. A Novel Monolithic Soft Robotic Thumb for an Anthropomorphic Prosthetic Hand. IEEE Robot. Autom. Lett. 2019, 4, 602–609. [Google Scholar] [CrossRef]
- Esposito, D.; Cosenza, C.; Gargiulo, G.D.; Andreozzi, E.; Niola, V.; Fratini, A.; D’Addio, G.; Bifulco, P. Experimental Study to Improve ‘Federica’ Prosthetic Hand and Its Control System. In XV Mediterranean Conference on Medical and Biological Engineering and Computing—MEDICON 2019; Henriques, J., Neves, N., DeCarvalho, P., Eds.; Springer: Cham, Switzerland, 2020; pp. 586–593. [Google Scholar] [CrossRef]
- Khatik, R.; Yadav, V. Myoelectric Signal Based Multiple Grip Pattern Prosthetic Arm. In Proceedings of the 2018 6th Edition of International Conference on Wireless Networks & Embedded Systems (WECON), Rajpura, India, 16–17 November 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 92–96. [Google Scholar] [CrossRef]
- Liao, B.; Zang, H.; Zhu, N.; Liu, D.; Tuo, J.; He, T.; Hu, L.; Yang, Z. System Design and Experiment of Bionics Robotic Arm with Humanoid Characteristics. In Proceedings of the 2018 WRC Symposium on Advanced Robotics and Automation (WRC SARA), Beijing, China, 16 August 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 90–95. [Google Scholar] [CrossRef]
- Triwiyanto, T.; Hamzah, S.; Luthfiyah, I.P.; Pawana, A.; Utomo, B. A low cost and open-source anthropomorphic prosthetics hand for transradial amputee. In Proceedings of the International Conference on Science and Applied Science (ICSAS) 2019, Surakarta, Indonesia, 20 July 2019; Suparmi, A., Nugraha, D.A., Eds.; AIP Publishing: Melville, NY, USA, 2019. [Google Scholar] [CrossRef]
- Sujana, I.N.; Sukor, J.A.; Jalani, J.; Sali, F.N.; Rejab, S.M. Cost-Effective Prosthetic Hand for Amputees: Challenges and Practical Implementation. Int. J. Integr. Eng. 2023, 15, 282–299. [Google Scholar] [CrossRef]
- Park, J.W.; Greenspan, B.; Tabb, T.; Gallo, E.; Danielescu, A. 3D Printed Energy Return Elements for Upper Limb Sports Prosthetics. Prosthesis 2023, 5, 13–34. [Google Scholar] [CrossRef]
- Dyer, B.; Glithro, R.; Batley, A. The design of an upper arm prosthesis utilising 3D printing conceived for the 2020 Tokyo paralympic games: A technical note. J. Rehabil. Assist. Technol. Eng. 2022, 9, 20556683221113308. [Google Scholar] [CrossRef]
- Day, S.J.; Riley, S.P. Utilising three-dimensional printing techniques when providing unique assistive devices: A case report. Prosthet. Orthot. Int. 2017, 42, 45–49. [Google Scholar] [CrossRef]
- Gróski, F.; Rybarczyk, D.; Wichiniarek, R.; Wierzbicka, N.; Kuczko, W.; Żukowska, M.; Regulski, R.; Pacurar, R.; Comsa, D.S.; Baila, D.I.; et al. Development and Testing of an Individualized Sensorised 3D Printed Upper Limb Bicycle Prosthesis for Adult Patients. Appl. Sci. 2023, 13, 12918. [Google Scholar] [CrossRef]
- Górski, F.; Łabudzki, R.; Żukowska, M.; Sanfilippo, F.; Ottestad, M.; Zelenay, M.; Băilă, D.I.; Pacurar, R. Experimental Evaluation of Extended Reality Technologies in the Development of Individualized Three-Dimensionally Printed Upper Limb Prostheses. Appl. Sci. 2023, 13, 8035. [Google Scholar] [CrossRef]
- Kopová, B.; Bakeš, M.; Čížek, M.; Horký, A.; Dvořák, J.; Ráž, K.; Chval, Z. Development and Production of a Children’s Upper-Limb Cycling Adapter Using 3D Printing. Materials 2024, 17, 4731. [Google Scholar] [CrossRef]
- Rhyne, B.J.; Post, B.K.; Chesser, P.; Roschli, A.; Love, L.J. Reverse engineering a transhumeral prosthetic design for additive manufacturing. In Proceedings of the 28th Annual International Solid Freeform Fabrication Symposium, Austin, TX, USA, 7–9 August 2017; pp. 2419–2429. [Google Scholar] [CrossRef]
- Lázaro-Guevara, J.; Gondokaryono, R.; González, L.; Garrido, K.; Sujumnong, N.; Wee, A.; Miscione, J. A Graphic User Interface (GUI) to build a cost-effective customizable 3D printed Prosthetic Hand. bioRxiv 2020. bioRxiv:2020.03.18.997486. [Google Scholar] [CrossRef]
- Su, H.; Kim, T.-H.; Moeinnia, H.; Kim, W.S. A 3D Printed Wearable Electromyography Wristband. In Proceedings of the FLEPS 2023—IEEE International Conference on Flexible and Printable Sensors and Systems, Proceedings, Boston, MA, USA, 9–12 July 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 1–4. [Google Scholar] [CrossRef]
- Mohammadi, A.; Hajizadeh, E.; Tan, Y.; Choong, P.; Oetomo, D. A bioinspired 3D-printable flexure joint with cellular mechanical metamaterial architecture for soft robotic hands. Int. J. Bioprint. 2023, 9, 696. [Google Scholar] [CrossRef]
- Munakata, G.; Zanini, P.; Titotto, S. 3D fingerprint design proposal using spider movement mechanism and soft robotic technology. Res. Biomed. Eng. 2020, 36, 361–368. [Google Scholar] [CrossRef]
- Garcia, L.; Naves, M.; Brouwer, D.M. 3D-printed flexure-based finger joints for anthropomorphic hands. In Proceedings of the IEEE International Conference on Intelligent Robots and Systems, Madrid, Spain, 1–5 October 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 1437–1442. [Google Scholar] [CrossRef]
- Secco, E.L.; Moutschen, C. A Soft Anthropomorphic & Tactile Fingertip for Low-Cost Prosthetic & Robotic Applications. EAI Endorsed Trans. Pervasive Health Technol. 2018, 4, e1. [Google Scholar] [CrossRef]
- Secco, E.L.; Agidew, T.F.; Nagar, A.K. An optical-based fingertip force sensor. Adv. Sci. Technol. Eng. Syst. J. 2018, 3, 23–27. [Google Scholar] [CrossRef]
- Wolterink, G.; Dias, P.; Sanders, R.G.P.; Muijzer, F.; Beijnum, B.J.V.; Veltink, P.; Krijnen, G. Development of Soft sEMG Sensing Structures Using 3D-Printing Technologies. Sensors 2020, 20, 4292. [Google Scholar] [CrossRef] [PubMed]
- Tong, Y.; Kucukdeger, E.; Halper, J.; Cesewski, E.; Karakozoff, E.; Haring, A.P.; Mcllvain, D.; Singh, M.; Khandelwal, N.; Meholic, A.; et al. Low-cost sensor-integrated 3D-printed personalized prosthetic hands for children with amniotic band syndrome: A case study in sensing pressure distribution on an anatomical human-machine interface (AHMI) using 3D-printed conformal electrode arrays. PLoS ONE 2019, 14, e0214120. [Google Scholar] [CrossRef]
- Ismail, R.; Taqriban, R.B.; Ariyanto, M.; Atmaja, A.T.; Sugiyanto; Caesarendra, W.; Glowacz, A.; Irfan, M.; Glowacz, W. Affordable and faster transradial prosthetic socket production using photogrammetry and 3d printing. Electronics 2020, 9, 1456. [Google Scholar] [CrossRef]
- Olsen, J.; Day, S.; Dupan, S.; Nazarpour, K.; Dyson, M. 3D-Printing and Upper-Limb Prosthetic Sockets: Promises and Pitfalls. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 527–535. [Google Scholar] [CrossRef]
- Hallworth, B.W.; Austin, J.A.; Williams, H.E.; Rehani, M.; Shehata, A.W.; Hebert, J.S. A Modular Adjustable Transhumeral Prosthetic Socket for Evaluating Myoelectric Control. IEEE J. Transl. Eng. Health Med. 2020, 8, e0700210. [Google Scholar] [CrossRef]
- Roda-Sales, A.; Llop-Harillo, I. Identifying Users’ Needs to Design and Manufacture 3D-Printed Upper Limb Sockets: A Survey-Based Study. Appl. Sci. 2024, 14, 3708. [Google Scholar] [CrossRef]
- Górski, F.; Wichniarek, R.; Kuczko, W.; Zukowska, M. Study on Properties of Automatically Designed 3D-Printed Customized Prosthetic Sockets. Materials 2021, 14, 5240. [Google Scholar] [CrossRef]
- Lee, F.A.; El Leow, M.; Yen, C.C.; Wang, W. 3D-printed nails for aesthetic silicone prostheses. Prosthet. Orthot. Int. 2022, 46, 641–645. [Google Scholar] [CrossRef]
- Pittaccio, S.; Lavorgna, M.; Romanò, J.; Sorrentino, A.; Cerruti, P.; Rollo, G.; Ascione, C.; Raucci, M.G.; Soriente, A.; Casaleggi, V.; et al. Hybrid Manufacturing of Upper-Limb Prosthesis Sockets with Improved Material Properties. In Computers Helping People with Special Needs; Miesenberger, K., Kouroupetroglou, G., Mavrou, K., Manduchi, R., Rodriguez, M.C., Penaz, P., Eds.; ICCHP-AAATE 2022, PT II; Springer: Cham, Switzerland, 2022; pp. 395–402. [Google Scholar] [CrossRef]
- Cortes, F.R.; Segatto, M.E.V.; Díaz, C.A.R. Development of a force myography sensor for PrHand prosthesis activation using fiber bragg grating sensor and 3D printing. In Proceedings of the 2024 Latin American Workshop on Optical Fiber Sensors, LAWOFS 2024, Campinas, Brazil, 20–22 May 2024; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2024; pp. 1–2. [Google Scholar] [CrossRef]
- Lee, H.; Park, J.; Kang, B.B.; Cho, K.J. Single-Step 3D Printing of Bio-Inspired Printable Joints Applied to a Prosthetic Hand. 3D Print. Addit. Manuf. 2023, 10, 917–929. [Google Scholar] [CrossRef] [PubMed]
- de Backer-Bes, F.; Lange, M.; Brouwers, M.; van Wijk De Hoogstraat, I. Xperience Prosthesis Transhumeral: An Innovative Test Prosthesis. JPO J. Prosthet. Orthot. 2024, 36, 193–197. [Google Scholar] [CrossRef]
- Senthil, P.; Vishanagra, O.; Sparkman, J.; Smith, P.; Manero, A. Design and Assessment of Bird-Inspired 3D-Printed Models to Evaluate Grasp Mechanics. Biomimetics 2024, 9, 195. [Google Scholar] [CrossRef] [PubMed]
- Abass, Z.; Meng, W.; Xie, S.Q.; Zhang, Z.Q. A Robust, Practical Upper Limb Electromyography Interface Using Dry 3D Printed Electrodes. In Proceedings of the 2019 IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM), Hong Kong, China, 8–12 July 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 453–458. [Google Scholar] [CrossRef]
- Costa, V.T.L.; Pai, C.N. Superficial Characteristics of Acetone Vapor Treated ABS Printed Parts for Use in Upper Limb Prosthesis. In Proceedings of the XXVI Brazilian Congress on Biomedical Engineering, CBEB 2018, Armação de Buzios, RJ, Brazil, 21–25 October 2018; CostaFelix, R., Machado, J.C., Alvarenga, A.V., Eds.; Springer: Singapore, 2019; Volume 1, pp. 365–376. [Google Scholar] [CrossRef]
- Al-Timemy, A.H.; Serrestou, Y.; Khushaba, R.N.; Yacoub, S.; Raoof, K. Hand Gesture Recognition With Acoustic Myography and Wavelet Scattering Transform. IEEE Access 2022, 10, 107526–107535. [Google Scholar] [CrossRef]
- Nam, K.; Crick, C. Self-trainable 3D-printed prosthetic hands. In Proceedings of the 2021 30th IEEE International Conference on Robot And Human Interactive Communication (RO-MAN), Vancouver, BC, Canada, 8–12 August 2021; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2021; pp. 1196–1201. [Google Scholar] [CrossRef]
- Fajardo, J.; Ferman, V.; Muñoz, A.; Andrade, D.; Neto, A.R.; Rohmer, E. User-Prosthesis Interface for Upper Limb Prosthesis Based on Object Classification. In Proceedings of the 15th Latin American Robotics Symposium 6th Brazilian Robotics Symposium 9th Workshop on Robotics in Education (LARS/SBR/WRE 2018), João Pessoa, Brazil, 6–10 November 2018; DoNascimento, T.P., Colombini, E.L., DeBrito, A.V., Garcia, L.T.D., Sa, S.T.D., Goncalves, L.M.G., Eds.; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 390–395. [Google Scholar] [CrossRef]
- Paskett, M.D.; Olsen, N.R.; George, J.A.; Kluger, D.T.; Brinton, M.R.; Davis, T.S. A Modular Transradial Bypass Socket for Surface Myoelectric Prosthetic Control in Non-Amputees. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 2070–2076. [Google Scholar] [CrossRef]
- James, A.; Seth, A.; Mukhopadhyay, S. Realtime Hand Landmark Tracking to Aid Development of a Prosthetic Arm for Reach and Grasp Motions. In Proceedings of the 2021 IEEE International Symposium on Robotic and Sensors Environments (ROSE 2021), Virtual Conference, 28–29 October 2021; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2021; pp. 1–7. [Google Scholar] [CrossRef]
- Fajardo, J.; Cardona, D.; Maldonado, G.; Neto, A.R.; Rohmer, E. A Robust H∞ Full-State Observer for Under-Tendon-Driven Prosthetic Hands. In Proceedings of the 2020 IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM), Boston, MA, USA, 6–9 July 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020; pp. 1555–1560. [Google Scholar] [CrossRef]
- Iyer, V.; Chan, J.; Culhane, I.; Mankoff, J.; Gollakota, S. Machinery Wireless Analytics for 3D Printed Objects. In Proceedings of the UIST 2018: 31ST Annual ACM Symposium on User Interface Software and Technology, Berlin, Germany, 14–17 October 2018; Association for Computing Machinery: New York, NY, USA, 2018; pp. 141–152. [Google Scholar] [CrossRef]
- Zhao, Y.; Chen, C.; Lu, B.Y.; Zhu, X.Y.; Gu, G.Y. All 3D-Printed Soft High-Density Surface Electromyography Electrode Arrays for Accurate Muscle Activation Mapping and Decomposition. Adv. Funct. Mater. 2024, 34, 2312480. [Google Scholar] [CrossRef]
- Alkhatib, F.; Mahdi, E.; Cabibihan, J.J. Design and Analysis of Flexible Joints for a Robust 3D Printed Prosthetic Hand. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 784–789. [Google Scholar] [CrossRef]
- Rahiminejad, E.; Parvizi-Fard, A.; Iskarous, M.M.; Thakor, N.V.; Amiri, M. A Biomimetic Circuit for Electronic Skin With Application in Hand Prosthesis. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 2333–2344. [Google Scholar] [CrossRef]
- Deprez, K.; De Baecke, E.; Tijskens, M.; Schoeters, R.; Velghe, M.; Thielens, A. A Circular, Wireless Surface-Electromyography Array. Sensors 2024, 24, 1119. [Google Scholar] [CrossRef]
- Al-Timemy, A.H.; Serrestou, Y.; Yacoub, S.; Raoof, K.; Khushaba, R.N. Hand Force Estimation from Acoustic Myography Using Deep Wavelet Scattering Transform and Long Short-Term Memory. In Proceedings of the 2023 45th Annual International Conference of the IEEE Engineering in Medicine & Biology Society, EMBC, Sydney, Australia, 24–27 July 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 1–4. [Google Scholar] [CrossRef]
- Tawk, C.; Spinks, G.M.; Panhuis, M.I.H.; Alici, G. 3D Printable Vacuum-Powered Soft Linear Actuators. In Proceedings of the 2019 IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM), Hong Kong, China, 8–12 July 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 50–55. [Google Scholar] [CrossRef]
- Mohapatra, S.; Tadesse, Y. Signal Conditioning Circuit for 3D Printed Flexible Strain Sensor for Hand Orthosis Application. In Proceedings of the 17TH IEEE Dallas Circuits and Systems Conference, DCAS 2024, Richardson, TX, USA, 19–21 April 2024; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2024; pp. 1–6. [Google Scholar] [CrossRef]
- Ntagios, M.; Navaraj, W.T.; Dahiya, R. 3D printed phalanx packaged with embedded pressure sensor. In Proceedings of the 2018 IEEE Sensors, New Delhi, India, 28–31 October 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 1–4. [Google Scholar] [CrossRef]
- Hong, G.W.; Lee, S.; Kim, J.H. Fabrication and characterization of 3D printed flexible capacitive pressure sensor for wearable devices and bio-mechanical applications. In Proceedings of the Nano-, Bio-, Info-Tech Sensors and 3D Systems III, Denver, CO, USA, 3–7 March 2019; Kim, J., Ed.; The Society of Photo-Optical Instrumentation Engineers: Bellingham, WA, USA, 2019. [Google Scholar] [CrossRef]
- Ntagios, M.; Escobedo, P.; Dahiya, R. 3D printed packaging of photovoltaic cells for energy autonomous embedded sensors. In Proceedings of the 2020 IEEE Sensors, Rotterdam, The Netherlands, 25–28 October 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- Navaraj, W.T.; Ozioko, O.; Dahiya, R. Capacitive-Piezoelectric Tandem Architecture for Biomimetic Tactile Sensing in Prosthetic Hand. In Proceedings of the 2018 IEEE Sensors, New Delhi, India, 28–31 October 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 1–4. [Google Scholar] [CrossRef]
- Mutlu, R.; Singh, D.; Tawk, C.; Sariyildiz, E. A 3D-Printed Soft Haptic Device with Built-in Force Sensing Delivering Bio-Mimicked Feedback. Biomimetics 2023, 8, 127. [Google Scholar] [CrossRef]
- Gunawardane, P.; Cheung, P.; Zhou, H.; Alici, G.; de Silva, C.W.; Chiao, M. A Versatile 3D-Printable Soft Pneumatic Actuator Design for Multi-Functional Applications in Soft Robotics. Soft Robot. 2024, 11, 709–723. [Google Scholar] [CrossRef]
- Christ, J.F.; Aliheidari, N.; Pötschke, P.; Ameli, A. Bidirectional and Stretchable Piezoresistive Sensors Enabled by Multimaterial 3D Printing of Carbon Nanotube/Thermoplastic Polyurethane Nanocomposites. Polymers 2019, 11, 11. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Huang, J.; Wang, M.; Deng, K.; Guo, C.; Li, B.; Cheng, Y.; Sun, H.; Ye, H.; Pan, T.; et al. Structural Electronic Skin for Conformal Tactile Sensing. Adv. Sci. 2023, 10, 2304106. [Google Scholar] [CrossRef] [PubMed]
- George, J.A.; Radhakrishnan, S.; Brinton, M.; Clark, G.A. IEEE Inexpensive and Portable System for Dexterous High-Density Myoelectric Control of Multiarticulate Prostheses. In Proceedings of the 2020 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Toronto, ON, Canada, 11–14 October 2020; pp. 3441–3446. [Google Scholar] [CrossRef]
- O’Brien, K.W.; Xu, A.; Levine, D.J.; Aubin, C.A.; Yang, H.J.; Xiao, M.F.; Wiesner, L.W.; Shepherd, R.F. Elastomeric passive transmission for autonomous force-velocity adaptation applied to 3D-printed prosthetics. Sci. Robot. 2018, 3, aau5543. [Google Scholar] [CrossRef] [PubMed]
- Bondok, M.A.; Elsheikh, M.E.; Elhadek, M. IEEE New Prosthetic Socket Designs for Transradial Amputee: Experiment without Healthy Subjects and Amputee. In Proceedings of the 2024 14th International Conference on Electrical Engineering, ICEENG 2024, Cairo, Egypt, 21–23 May 2024; pp. 114–119. [Google Scholar] [CrossRef]
- Gao, Z.; Gong, Z.H.; Zhu, G.P.; Zhang, T. IEEE A Solid-liquid Composite Flexible Bionic Tactile Sensor for Dexterous Hands. In Proceedings of the 2024 IEEE International Conference on Advanced Intelligent Mechatronics, AIM 2024, Boston, MA, USA, 15–19 July 2024; 2024; pp. 1560–1566. [Google Scholar] [CrossRef]
- Zhang, Z.P.; Han, T.J.; Huang, C.J.; Shuai, C.J. Hardware and Software Design and Implementation of Surface-EMG-Based Gesture Recognition and Control System. Electronics 2024, 13, 454. [Google Scholar] [CrossRef]
- Navaraj, W.; Dahiya, R. Fingerprint-Enhanced Capacitive-Piezoelectric Flexible Sensing Skin to Discriminate Static and Dynamic Tactile Stimuli. Adv. Intell. Syst. 2019, 1, 1900051. [Google Scholar] [CrossRef]
- Nassar, H.; Khandelwal, G.; Chirila, R.; Karagiorgis, X.; Ginesi, R.E.; Dahiya, A.S.; Dahiya, R. Fully 3D printed piezoelectric pressure sensor for dynamic tactile sensing. Addit. Manuf. 2023, 71, 103601. [Google Scholar] [CrossRef]
- Tawk, C.; Spinks, G.M.; Alici, G.; Panhuis, M.I.H. 3D Printable Linear Soft Vacuum Actuators: Their Modeling, Performance Quantification and Application in Soft Robotic Systems. IEEE/ASME Trans. Mechatron. 2019, 24, 2118–2129. [Google Scholar] [CrossRef]
- Prakash, A.; Sharma, S.; Sharma, N. A compact-sized surface EMG sensor for myoelectric hand prosthesis. Biomed. Eng. Lett. 2019, 9, 467–479. [Google Scholar] [CrossRef]
- Chang, M.H.; Jung, I.; Seo, K.W.; Park, J.; Choi, H.; Cho, K.J. Posture-dependent variable transmission mechanism for prosthetic hand inspired by human grasping characteristics. Intell. Serv. Robot. 2024, 17, 389–399. [Google Scholar] [CrossRef]
- Minshew, Z.; Alba-Flores, R. Hand Prosthesis Control using Electromyographic Signal Trained Neural Network for Live Gesture Classification. In Proceedings of the 2019 IEEE SOUTHEASTCON, Huntsville, AL, USA, 11–14 April 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Artal-Sevil, J.S.; Montañés, J.L.; Acón, A.; Domínguez, J.A. IEEE Control of a Bionic Hand using real-time gesture recognition techniques through Leap Motion Controller. In Proceedings of the 2018 XIII Technologies Applied to Electronics Teaching Conference (TAEE), La Laguna, Spain, 20–22 June 2018. [Google Scholar]
- Zhou, H.; Tawk, C.; Alici, G. A Multipurpose Human–Machine Interface via 3D-Printed Pressure-Based Force Myography. IEEE Trans. Ind. Inform. 2024, 20, 8838–8849. [Google Scholar] [CrossRef]
- Waisarikit, A.; Ross, S.; Ross, G.M.; Udee, N.; Mahasaranon, S. Modified natural rubber glove with spent coffee grounds for prothesis arm cover. Mater. Today Proc. 2021, 47, 3577–3584. [Google Scholar] [CrossRef]
- Proesmans, R.; Deprez, K.; Velghe, M.; Thielens, A. An on-body antenna for control of a wireless prosthesis in the 2.45 GHz industrial scientific and medical frequency band. IET Microw. Antennas Propag. 2022, 16, 919–932. [Google Scholar] [CrossRef]
- Tymkovych, M.; Selivanova, K.; Avrunin, O.; Kostin, D.; Bezverkhyi, O.; Baklaiev, V.; Omiotek, Z.; Smailova, S.; Kumargazhanova, S. 3D scanning technologies by optical RealSense cameras for SIREN-based 3D hand representation. In Proceedings of the Optical Fibers and Their Applications 2023, Lublin, Poland, 11–14 September 2023; Wojcik, W., Omiotek, Z., Smolarz, A., Eds.; Society of Photo-Optical Instrumentation Engineers: Bellingham, WS, USA, 2023. [Google Scholar] [CrossRef]
- Neri, P.; Barone, S.; Paoli, A.; Razionale, A.V.; Tamburrino, F. A Depth-Camera Based System for the Real-Time Scanning of Upper Limb Anatomy. In Design Tools and Methods in Industrial Engineering II; Rizzi, C., Campana, F., Bici, M., Gherardini, F., Ingrassia, T., Cicconi, P., Eds.; ADM 2021; Springer Nature: Lviv, Ukraine, 2022; pp. 245–255. [Google Scholar] [CrossRef]
- Yang, Y.S.; Xu, J.; Elkhuizen, W.S.; Song, Y. The development of a low-cost photogrammetry-based 3D hand scanner. HardwareX 2021, 10, e00212. [Google Scholar] [CrossRef] [PubMed]
- Volonghi, P.; Baronio, G.; Signoroni, A. 3D scanning and geometry processing techniques for customised hand orthotics: An experimental assessment. Virtual Phys. Prototyp. 2018, 13, 105–116. [Google Scholar] [CrossRef]
- Gaballa, A.; Lambert, L.A.; Diab, K.; Cabibihan, J.J. Image Processing of 3D Scans for Upper Limb Prosthesis of the War-Wounded. In Proceedings of the 2020 IEEE 20th International Conference on Bioinformatics and Bioengineering (BIBE 2020), Cincinnati, OH, USA, 26–28 October 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020; pp. 596–601. [Google Scholar] [CrossRef]
- Lee, J.; Chesang, A.; Gichane, M.; Busogi, M.; Byiringiro, J.; Tucker, C. Reducing the Barriers to Designing 3D-Printable Prosthetics in Resource-Constrained Environments. In Proceedings of the ASME 2023 International Design Engineering Technical Conferences and Computers and Information in Engineering Conference, IDETC-CIE2023, Boston, MA, USA, 20–23 August 2023; American Society of Mechanical Engineers: New York City, NY, USA, 2023. [Google Scholar] [CrossRef]
- Neri, P.; Paoli, A.; Aruanno, B.; Barone, S.; Tamburrino, F.; Razionale, A.V. 3D scanning of Upper Limb anatomy by a depth-camera-based system. International Journal of Interactive Design and Manufacturing—IJIDEM. Int. J. Interact. Des. Manuf. 2024, 18, 5599–5610. [Google Scholar] [CrossRef]
- Kirtania, D.K. Network Visualization of ChatGPT Research: A study based on term and keyword co-occurrence network analysis. arXiv 2023, arXiv:2304.01948. [Google Scholar] [CrossRef]
- Narong, D.K.; Hallinger, P. A Keyword Co-Occurrence Analysis of Research on Service Learning: Conceptual Foci and Emerging Research Trends. Educ. Sci. 2023, 13, 339. [Google Scholar] [CrossRef]
- Smail, L.C.; Neal, C.; Wilkins, C.; Packham, T.L. Comfort and function remain key factors in upper limb prosthetic abandonment: Findings of a scoping review. Disabil. Rehabil. Assist. Technol. 2021, 16, 821–830. [Google Scholar] [CrossRef]
- Xiao, Z.G.; Menon, C. A Review of Force Myography Research and Development. Sensors 2019, 19, 4557. [Google Scholar] [CrossRef]

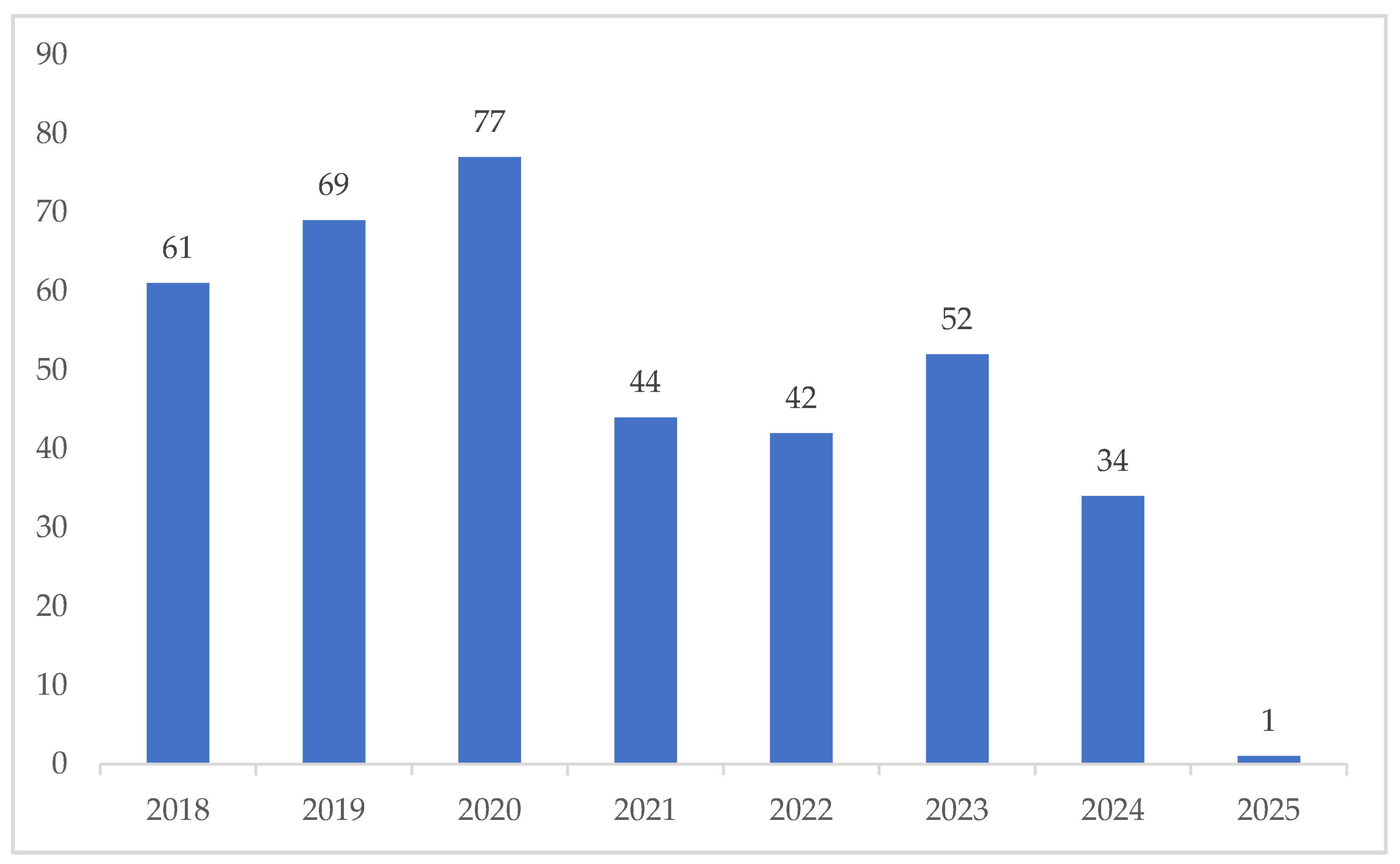

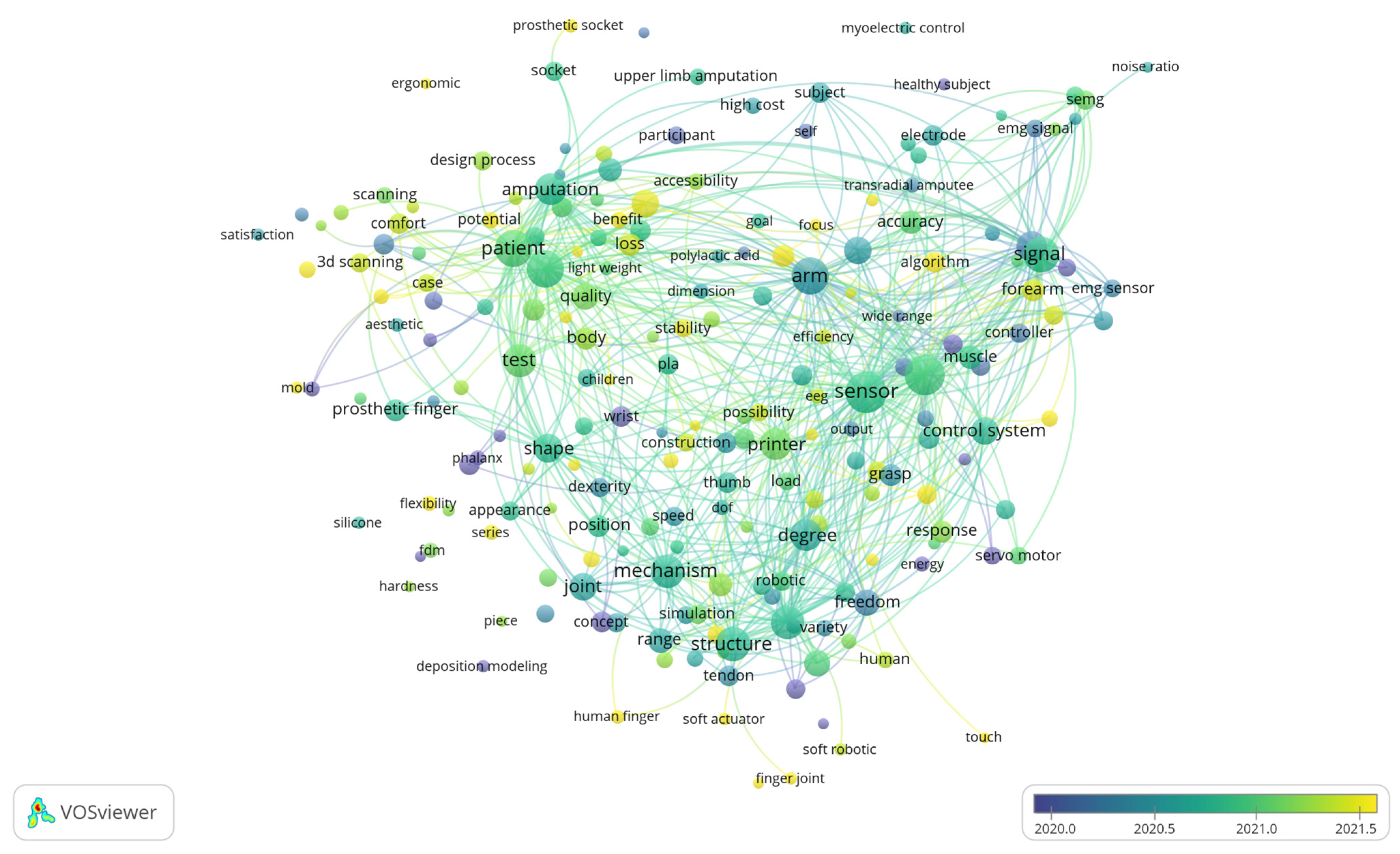
| Techniques/Materials | Use Cases/Comparison | Example Paper |
|---|---|---|
| 3D scanning techniques | ||
| CT Scan | Used in a clinical setting; special equipment is needed which hospitals generally already have | [24] |
| Commercial Scanner | Multiple commercial scanners are available to buy and have higher accuracy | [23,47,100,241] |
| Photogrammetry | Uses 2D photographs to create 3D models; cost-effective, requires minimal specialized equipment, lower accuracy | [45,46,240,292] |
| Printing methods | ||
| Fused Filament Fabrication/Fused Deposition Modeling (FFM/FDM) | Mostly used in prototyping and low-cost manufacturing; affordable, easy to use, and compatible with various materials like PLA and ABS | [30,31,44,48,51,55,77] |
| Selective Laser Sintering (SLS) | Good for printing complex parts and detailed parts; uses powdered materials; durable prototype | [47,116,138,235] |
| Stereolithography (SLA) | High-resolution and smooth finish; commonly used in dentistry and precision engineering | [116,123] |
| Materials | ||
| Polylactide (PLA) | Cheapest material; mostly used for quick, affordable prototyping or creating non-functional models | [27,29,30,31,46] |
| Acrylonitrile Butadiene Styrene (ABS) | Durable and resistant to impact; best for functional prototypes and mechanical parts | [52,53,56,77] |
| Thermoplastic Polyurethane (TPU) | Flexible and compliant; often used for soft robotics parts | [28,80,85,93,94,231] |
| Thermoplastic Elastomer (TPE) | Extremely flexible and stretchable; recommended for wearables | [51] |
| Polyethylene Terephthalate Glycol (PETG) | Durable, transparent, food-safe, and hard to tear | [57,78,241] |
| No | Cluster | Theme | Number of Keywords | Representative Keywords |
|---|---|---|---|---|
| 1 | Red | Prosthesis design and evaluation for people | 20 | child |
| comfort | ||||
| functionality | ||||
| patient | ||||
| user 3d scanning | ||||
| 2 | Blue | Prosthesis control and sensing technologies | 18 | control |
| sensor | ||||
| electromyography | ||||
| surface electromyography | ||||
| 3 | Green | Mechanical design and robotics | 17 | actuator |
| degrees of freedom | ||||
| robotic hand | ||||
| soft robotics | ||||
| 4 | Yellow | Accessibility for prosthesis | 7 | cost |
| low cost | ||||
| daily living | ||||
| open source |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chainando, N.; Martawidjaja, M.; Darius, R.A.; Yahya, L.C.; Yemima, S.; Tan, W.S.; Harito, C.; Chandra, R.C.; Andhini, G.K.; Putra, K.B.; et al. Applying 3D Scanning and Printing Techniques to Produce Upper Limb Prostheses: Bibliometric Analysis and Scoping Review. Prosthesis 2025, 7, 26. https://doi.org/10.3390/prosthesis7020026
Chainando N, Martawidjaja M, Darius RA, Yahya LC, Yemima S, Tan WS, Harito C, Chandra RC, Andhini GK, Putra KB, et al. Applying 3D Scanning and Printing Techniques to Produce Upper Limb Prostheses: Bibliometric Analysis and Scoping Review. Prosthesis. 2025; 7(2):26. https://doi.org/10.3390/prosthesis7020026
Chicago/Turabian StyleChainando, Nico, Marcel Martawidjaja, Raphael Albert Darius, Leonardo Carlos Yahya, Sharon Yemima, Wilson Susanto Tan, Christian Harito, Rafa Callista Chandra, Grasheli Kusuma Andhini, Ketut Bagus Putra, and et al. 2025. "Applying 3D Scanning and Printing Techniques to Produce Upper Limb Prostheses: Bibliometric Analysis and Scoping Review" Prosthesis 7, no. 2: 26. https://doi.org/10.3390/prosthesis7020026
APA StyleChainando, N., Martawidjaja, M., Darius, R. A., Yahya, L. C., Yemima, S., Tan, W. S., Harito, C., Chandra, R. C., Andhini, G. K., Putra, K. B., Lumban Tobing, C. C., Syafi’i, M., & Syafrudin, M. (2025). Applying 3D Scanning and Printing Techniques to Produce Upper Limb Prostheses: Bibliometric Analysis and Scoping Review. Prosthesis, 7(2), 26. https://doi.org/10.3390/prosthesis7020026








