Abstract
Craniosacral rhythm is a manual therapy technique that focuses on the subtle, rhythmic movement of cerebrospinal fluid as it flows through the central nervous system and musculoskeletal system. Through light and delicate manipulation of the cranial bones, membranes and soft tissues of the head and neck, it promotes rebalancing and release from tension in the body, improving the circulation of the cerebrospinal fluid and the individual’s health. In the field of prosthetic dentistry, in rare cases, such as a full arch or removable partial denture, the patient perceives a sensation of constriction even though all procedures have been used correctly. In this work, a new design fora removable partial denture is proposed that does not interfere with the primary respiratory mechanism, reducing the sensation of constriction in the patient. The materials used are the same as those used for a normal removable partial denture, and the technique used is the “lost wax” one: the novelty is that the prosthesis is made in two separate parts that are joined by a central connection; the result is a removable partial denture with a small central thickening in the main joint represented by the connection of the two pieces. Craniosacral breathing movements are favored with this prosthesis as the metal structure is hyperstatic towards intrusion movements, more or less virtual in the opposite direction, i.e., extrusion towards the vestibule.
1. Introduction
In today’s health and wellness field, there is a growing awareness of the importance of a holistic and integrated approach to maintaining health. More and more people are recognizing osteopathy as a valuable resource for healing and general well-being. This trend reflects a significant shift in health care perspectives as more and more individuals seek unconventional and complementary approaches to improve their overall health status [1]. According to the World Health Organization, osteopathy is a healthcare profession characterized by skills in diagnosis, management, and treatment of patients through an exclusively manual approach. This profession is aimed at all segments of the population, from newborns to the elderly, offering primary care through direct contact with patients. The osteopath’s approach through manipulations in the affected districts seeks to re-establish the primary respiratory mechanism (MRP), i.e., the balance and conditions for which benefits can be obtained from any treatment. The term “primary respiratory mechanism” (MRP) refers to a fundamental principle in the osteopathic and chiropractic theories of cranial movement. According to this theory, the MRP is the main mechanism through which breathing occurs, and this influences the movements of the bones of the skull and the craniosacral system. MRP is considered a subtle, rhythmic movement involving the cerebrospinal fluid and tissues surrounding the central nervous system [2]. The theory holds that proper function of the PRM is essential for the overall well-being of the body and that disturbances of the PRM can affect physical health and well-being [3,4]. Cranial osteopathy was developed by the osteopathic doctor WG Sutherland in the 1930s, while the name craniosacral therapy was coined by John Upledger, who in the 1970s created a discipline distinct from cranial osteopathy. The model of the “craniosacral system” is based on the circulation of liquor, on the movements of the bones and meninges, and on the craniosacral rhythm, or cranial rhythmic impulse, from 6 to 12 cycles per minute [5]. Wójcik M. and collaborators in 2023 in a randomized study demonstrated how the application of craniosacral therapy reduced stress hormone levels in male firefighter cadets [6]. Trine S. and collaborators in 2020, in a study conducted in Norway on severely traumatized patients, demonstrated that patients with complex trauma, including post-traumatic stress disorder, benefited from the multimodal therapeutic approach including craniosacral therapy [7]. In recent years, collaboration between dentistry and osteopathy has become increasingly widespread: there are direct correlations between the alignment of the teeth, the symmetry of the joints, the curves of the spine, the levels of the shoulder blades and pelvis, and the length of the legs. The introduction of the primary respiratory mechanism (MRP) has allowed us to understand how the sutures that join the bones together are compared to mobile hinges that allow a pumping action of the primary respiratory system, without which it could not function as it should. In the literature, there are no prosthetic products, except for the bite, which is made with a view to craniosacral breathing. The objective of our work is to propose, from the perspective of the patient’s holistic vision and the correlation of sphenobasilar synchondrosis with posture, a new design of the removable partial denture (RPD) that takes into account any movements of craniosacral breathing.
2. Materials and Methods
The design and construction of an RPD is a complex and customized process. A standardized model is not feasible due to various factors such as the size of the upper jaw and the morphology of the dental elements. The materials used for the creation of the RPD are the same used for the creation of a normal, removable partial prosthesis made of a steel alloy using the manual non-cad/cam technique [8,9]. Only the sequences of manual steps not assisted by cad/cam [10] were modified in order to obtain two separate parts that are articulated by a central pin. The technique used is the lost wax technique. (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5 and Figure 6) illustrates the methodology used to design the prosthesis.
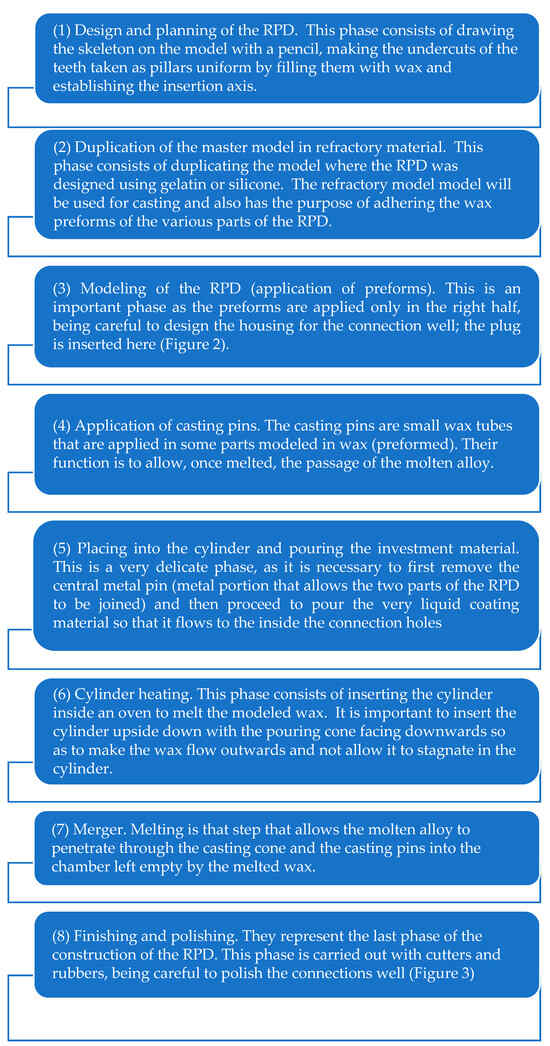
Figure 1.
Illustrates the methodology used to design the first prosthetic portion.

Figure 2.
Design and application of wax for the creation of an RPD (first part).

Figure 3.
The first part of the finished RPD.
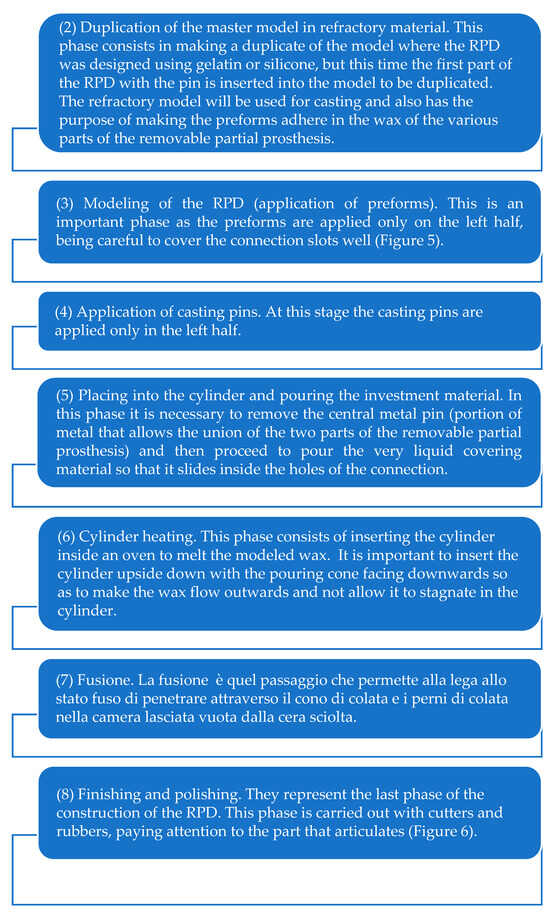
Figure 4.
Illustrates the methodology used to design the second prosthetic portion.

Figure 5.
Wax model of the second prosthetic part.

Figure 6.
Finished RPD.
Once the first half of the RPD has been obtained and finished, it will be necessary to make the other part of the prosthesis starting from the duplication of the master model with the first finished metal part inserted and the metal pin in the connection so as to keep the holes of the mechanism free during modeling, and then proceed to retrace the same steps performed for the first part (Figure 4).
3. Results
The movements of craniosacral breathing in the maxilla are outwards in the vestibular direction following normal breathing as reported in the literature (Figure 7).
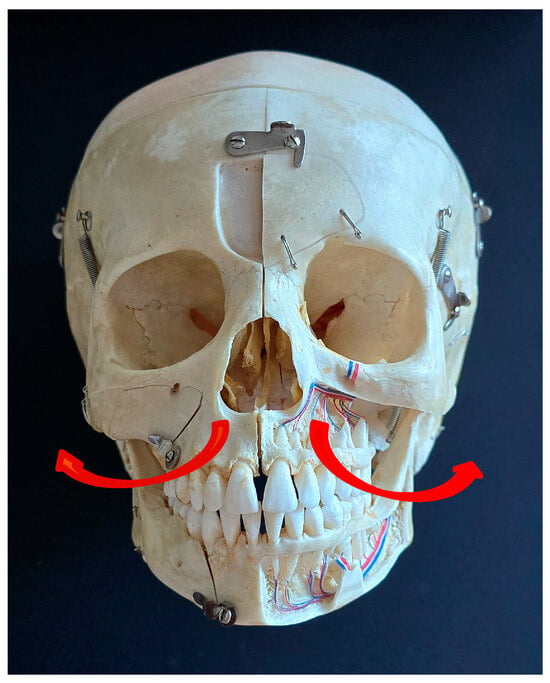
Figure 7.
Direction of jaw movements during craniosacral breathing.
The prosthetic product obtained with this technique is an RPD made up of two distinct parts that join in the center via an appropriately designed hinge having a central pin that allows movement only in the direction of the vestibule (Figure 8).

Figure 8.
View of the central part opened in the vestibular direction.
4. Discussion
The concept of cranial osteopathy was introduced by WG Sutherland, establishing the rules for the use of cranial palpation and techniques in the types of dysfunctional patterns that craniosacral therapy treats. The mechanism of primary respiration and the movement of neurocranial and viscerocranial sutures are phenomena intrinsic to the field and can be found in every vital organism, regardless of thoracic respiration and cardiac impulse [11]. According to the osteopathic and craniosacral perspectives, the flexion-extension of the skull occurs mainly thanks to the movement of the spheno-occipital synchondrosis joint [12]. These flexor movements that occur during craniosacral breathing affect all the bones of the skull, and in particular the palatine bones would undergo an outward and backward movement while the maxillary, mandibular, and temporal oxazygomatic bones would undergo an external rotation [13]. The use of skull palpation has been used over several years to improve chronic pain disorders such as low back pain, neck pain, headaches, and migraines, which considerably affect all age groups, from the beginning of adolescence to adults middle-aged and older. Haller H. et al. in 2019 in a systematic review and meta-analysis of randomized controlled trials evaluated craniosacral therapy in ten randomized trials for a total of 681 patients with neck and back pain, migraine, headache, fibromyalgia, epicondylitis, and pelvic girdle pain. The authors found significant, small and medium cumulative effects from craniosacral therapy directly after the end of the intervention for pain intensity, functional disability, and physical quality of life [14]. Terrell Z. T. and collaborators in 2022 conducted a randomized controlled study that aimed to evaluate whether a single session of osteopathic manipulative treatment or manipulative treatment of osteopathic + osteopathic cranial manipulative medicine could improve the gait of subjects suffering from Parkinson’s disease by resolving joint restrictions in the sagittal plane and increasing the range of motion in the lower limb. Study results showed that individuals with Parkinson’s disease experienced a significant increase in total hip sagittal range of motion (p = 0.038) after a single session of the standardized treatment protocol of osteopathic manipulative treatment + cranial manipulative medicine. osteopathic, concluding that the two combined therapies can be useful on the characteristics of parkinsonian gait [15]. Ceraulo S. and collaborators in a retrospective study conducted in 2022 in patients hospitalized in some social care residences (RSA) where there are residents suffering from various systemic pathologies, including Parkinson’s disease, demonstrated how the aspects of socialization and nutrition after the creation of new, more comfortable prostheses without constraints or after modification of existing prostheses [16]. Govardhan C. and collaborators in 2019 in a case report regarding labial, lingual, and maxillary frenuloplasty with myofunctional therapy as a treatment for oral breathing and snoring reported how some therapeutic interventions, including craniosacral therapy, can address the functional and behavioral factors that contribute to breathing oral [17]. The primary respiratory mechanism as well as craniosacral breathing in the last 10 years have been the topics studied by some branches of medicine in order to evaluate the veracity of the movements of the bone structures. This is the case with Rasmussen TR and collaborators, who, in 2021, conducted an experiment on 50 healthy individuals who underwent monitoring of rhythmic cranial movements measured in real time for 42 min in a supine resting state without any intervention using a newly developed machine. The authors found a third rhythm observed as a dynamic physiological phenomenon with a narrow range in healthy individuals at rest with an average of 6.16 cycles/minute (4.25–7.07) in addition to the respiratory breathing rhythm and the breathing rhythm. of arterial pulsation [18]. There are no studies in the literature that correlate craniosacral breathing and prosthetic rehabilitation; consequently, there is no data that can describe how to build a prosthesis that follows the movements of craniosacral breathing. There are only indications that suggest not to join the teeth because it could increase stress on the maxillary or mandibular bone and on the natural teeth and to keep them separate to adapt to the natural variations of the bones. In this work, a metal RPD was taken into consideration, which facilitates the movement of craniosacral breathing unlike the traditional RPD, which normally appears rigid and static once inserted into the oral cavity. Despite new technologies and new construction techniques for dental prostheses, many patients are forced due to systemic, anatomical, and economic conditions to choose for rehabilitation of the oral cavity a social prosthesis such as the RPD, and this, in rare cases, after its creation, is not accepted both from a functional point of view because in these subjects it created parafunctions or headaches and from an aesthetic point of view because the hooks were visible we therefore resort to design strategies that allow acceptance by the patient [19,20,21,22]. In some cases, patients spontaneously resolve the discomfort of the constriction or discomfort caused by the parafunctions that they perceive by removing the prosthesis, even though they know that they alter the occlusion with a possible consequence of oro-facial pain creating TMJ disorders [23]. The patients who mostly present partial or total edentulism are the elderly, who often, for social reasons or the presence of systemic pathologies, find themselves forced to no longer wear the prosthesis for various reasons, including feeling a “vise in the mouth” or an “annoying bulk”. To improve these sensations of discomfort in the maxilla, in the context of RPD, a prosthesis was created that considered the movement of the maxillary bone outwards in a vestibular direction, allowing the movements of craniosacral breathing. The prosthetic metal structure obtained is mechanically labile and inserted into the model, i.e., into the oral cavity depending on the patient’s physiological conditions (state of the mucous membranes and teeth), is hyperstatic for intrusion movements towards the midline, with the possibility of more or less virtual movements in the opposite direction, i.e., extrusion towards the vestibule. These movements favor craniosacral breathing, provided that in the starting position the prosthesis is placed in conditions of minimal extension during breathing. This prosthesis, however, presents some problems relating to the hygiene of the prosthesis itself, the presence of the swelling in the central part where there is the union of the two cast pieces, and the creation of the pin that joins the two parts. Due to the presence of the joint, the central part is subject to the accumulation of food during chewing as the thickness favors its retention and possible accumulation of plaque and microorganisms on the surface of the RPD due to the presence of two different surfaces [24]. Furthermore, unlike the traditional RPD, which has the upper main joint thin and adherent to the palate, in this prosthesis built for craniosacral respiratory movements, the main joint is thicker in the central portion due to the presence of eyelets in one part and eyelets and metal covers in the other side. These problems could be overcome with the new digital CAD/CAM technologies by constructing the articulated part more easily, thus avoiding difficulties in the millimetric precision manual construction to create the joint of the two parts.
5. Conclusions
In the literature, there are currently no specific dental prostheses designed not to interfere with craniosacral breathing. This new design presents itself as an RPD proposal for selected patients who experience discomfort, presumably due to the blockage of the primary respiratory mechanism. Clinical studies based on the use of this new type of prosthesis on patients will be necessary to verify the real benefit of the same over time for orofacial problems, favoring the CAD-CAM method for the construction of the device.
Author Contributions
Conceptualization and methodology, S.C.; validation, F.C.; writing—original draft preparation, A.B.; writing—review and editing, D.L. and G.C., supervision, R.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval was waived for this manuscript as it is not an experimental case but a novel design.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data from this study are available upon reasonable request by writing to the corresponding.
Acknowledgments
The authors thank the dental technician, Giovanni Ceraulo, for his precious contribution to the creation of the prosthetic product.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Brough, N.; Lindenmeyer, A.; Thistlethwaite, J.; Lewith, G.; Stewart-Brown, S. Perspectives on the effects and mechanisms of craniosacral therapy: A qualitative study of users’ views. Eur. J. Integr. Med. 2015, 7, 172–183. [Google Scholar] [CrossRef]
- Whedon, J.M.; Glassey, D. Cerebrospinal fluid stasis and its clinical significance. Altern. Ther. Health Med. 2009, 15, 54–60. [Google Scholar] [PubMed] [PubMed Central]
- Bordoni, B.; Escher, A.R. Rethinking the Origin of the Primary Respiratory Mechanism. Cureus 2023, 15, e46527. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Frymann, V.M. A study of the rhythmic motions of the living cranium. J. Am. Osteopath. Assoc. 1971, 70, 928–945. [Google Scholar] [PubMed]
- Upledger, J.E. CranioSacral Therapy. Semin. Integr. Med. 2004, 2, 159–166. [Google Scholar] [CrossRef]
- Wójcik, M.; Bordoni, B.; Siatkowski, I.; Żekanowska, E. The Effect of Craniosacral Therapy on Blood Levels of Stress Hormones in Male Firefighter Cadets: A Randomized Clinical Trial. Behav. Sci. 2023, 13, 914. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stub, T.; Kiil, M.A.; Lie, B.; Kristoffersen, A.E.; Weiss, T.; Hervik, J.B.; Musial, F. Combining psychotherapy with craniosacral therapy for severe traumatized patients: A qualitative study from an outpatient clinic in Norway. Complement. Ther. Med. 2020, 49, 102320. [Google Scholar] [CrossRef]
- Marino, G. Alessandro Canton. La ProtesiParzialeRimovibile dalla Teoria alla Pratica; Edizioni Martina: Bologna, Italy, 2002. [Google Scholar]
- Ceraulo, G.; Ceraulo, S. La protesischeletrata, lo scheletrato con ritenzioni a lamelle. In Progettazione-Disegno-Costruzione-Clinica; Wide Snc: Palermo, Italy, 2014; ISBN 978-88-9728-416-1. [Google Scholar]
- Tregerman, I.; Renne, W.; Kelly, A.; Wilson, D. Evaluation of removable partial denture frameworks fabricated using 3 different techniques. J. Prosthet. Dent. 2019, 122, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Bordoni, B.; Zanier, E. Sutherland’s legacy in the new millennium: The osteopathic cranial model and modern osteopathy. Adv. Mind Body Med. 2015, 29, 15–21. [Google Scholar] [PubMed]
- Greenman, P.E. Roentgen findings in the craniosacral mechanism. J. Am. Osteopath. Assoc. 1970, 70, 60–71. [Google Scholar] [PubMed]
- Sutherland, W.G. The cranial bowl. 1944. J. Am. Osteopath. Assoc. 2000, 100, 568–573. [Google Scholar] [PubMed]
- Haller, H.; Lauche, R.; Sundberg, T.; Dobos, G.; Cramer, H. Craniosacral therapy for chronic pain: A systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet. Disord. 2019, 21, 1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Terrell, Z.T.; Moudy, S.C.; Hensel, K.L.; Patterson, R.M. Effects of osteopathic manipulative treatment vs. osteopathic cranial manipulative medicine on Parkinsonian gait. J. Osteopath. Med. 2022, 122, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Ceraulo, S.; Caccianiga, P.; Casto, C.; Ceraulo, I.; Caccianiga, G. Dental Prosthetic Rehabilitation Interventions in Elderly Patients Hospitalized in the Nursing Homes of the Lombardy Region: A Retrospective Study. Healthcare 2022, 10, 2328. [Google Scholar] [CrossRef] [PubMed]
- Govardhan, C.; Murdock, J.; Norouz-Knutsen, L.; Valcu-Pinkerton, S.; Zaghi, S. Lingual and Maxillary Labial Frenuloplasty with Myofunctional Therapy as a Treatment for Mouth Breathing and Snoring. Case Rep. Otolaryngol. 2019, 2019, 3408053. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rasmussen, T.R.; Meulengracht, K.C. Direct measurement of the rhythmic motions of the human head identifies a third rhythm. J. Bodyw. Mov. Ther. 2020, 26, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Ceraulo, S. Aesthetics in Removable Partial Dentures: Modification of the Proximal Plate and Retentive Lamellae in Kennedy Class II Scenarios. Prosthesis 2024, 6, 107–118. [Google Scholar] [CrossRef]
- Greco, G.; Borgia, R.; Casto, C. Oral Rehabilitation with Removable Partial Denture: Technical Consideration. Eur. J. Musculoskelet. Dis. 2023, 12, 19–23. [Google Scholar]
- Chan, A.K.Y.; Tsang, Y.C.; Lai, E.H.; Chu, C.H. Tooth Wear in Older Adults: A Review of Clinical Studies. Geriatrics 2024, 9, 12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ohrbach, R.; Michelotti, A. The Role of Stress in the Etiology of Oral Parafunction and Myofascial Pain. Oral. Maxillofac. Surg. Clin. N. Am. 2018, 30, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Golanska, P.; Saczuk, K.; Domarecka, M.; Kuć, J.; Lukomska-Szymanska, M. Sindrome del dolore miofascialetemporomandibolare: Eziologia e modulazionebiopsicosociale. Una recensionenarrativa. Int. J. Environ. Res. Public Health 2021, 18, 7807. [Google Scholar] [CrossRef]
- Schmutzler, A.; Rauch, A.; Nitschke, I.; Lethaus, B.; Hahnel, S. Cleaning of Removable Dental Prostheses—A Systematic Review. J. Evid. Based Dent. Pract. 2021, 21, 101644. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).