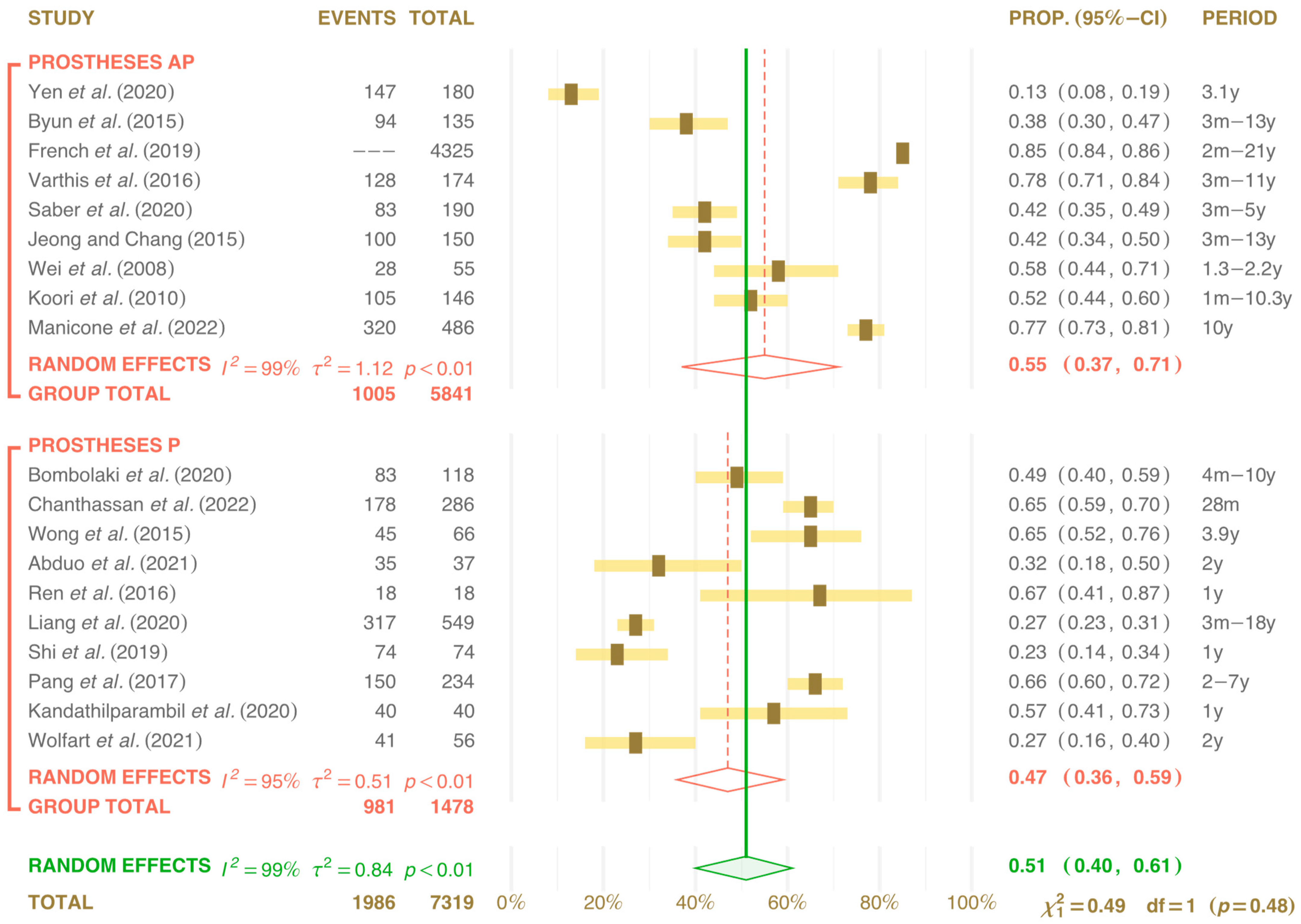
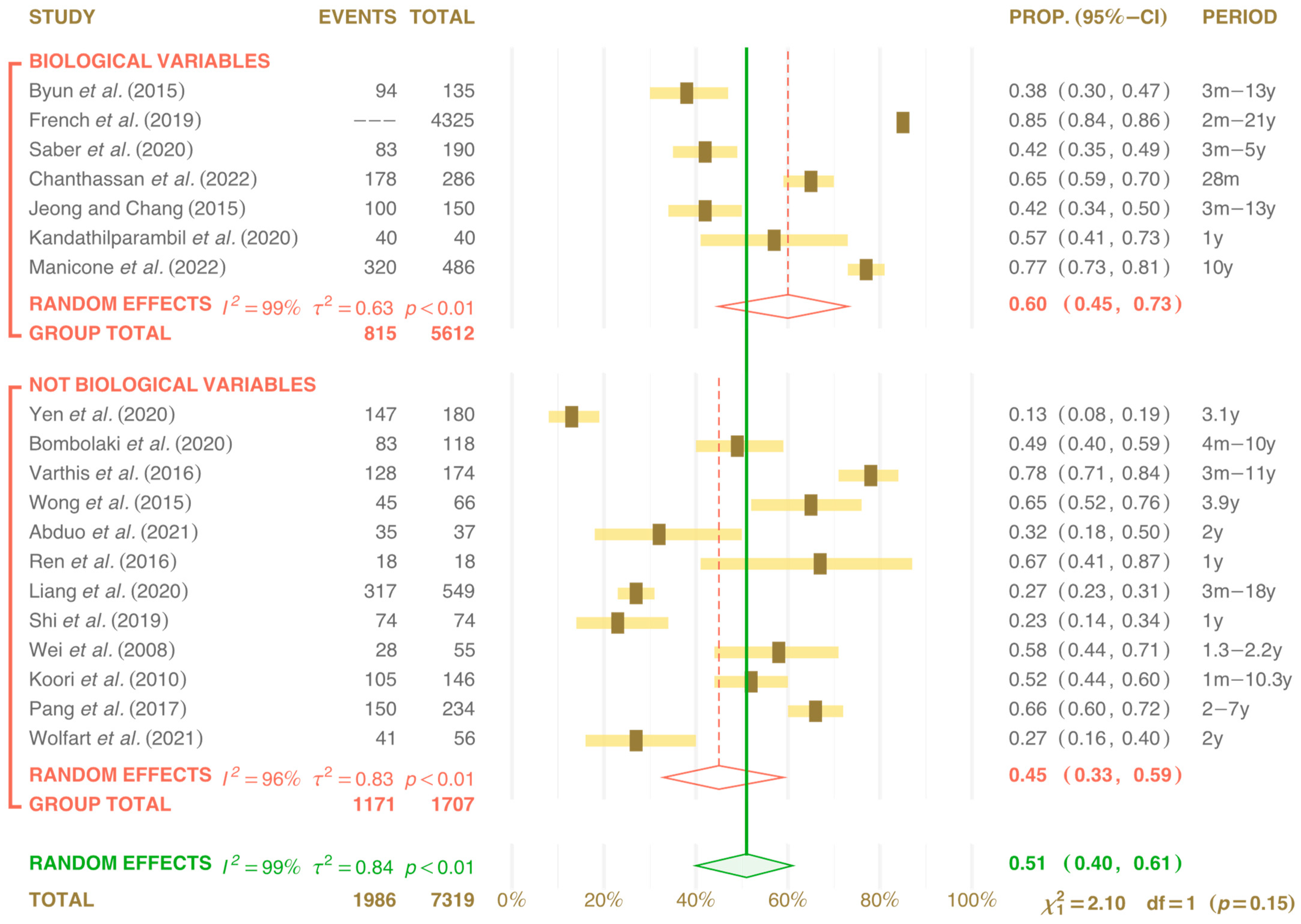
Clinical Effects of Interproximal Contact Loss between Teeth and Implant-Supported Prostheses: Systematic Review and Meta-Analysis
Abstract
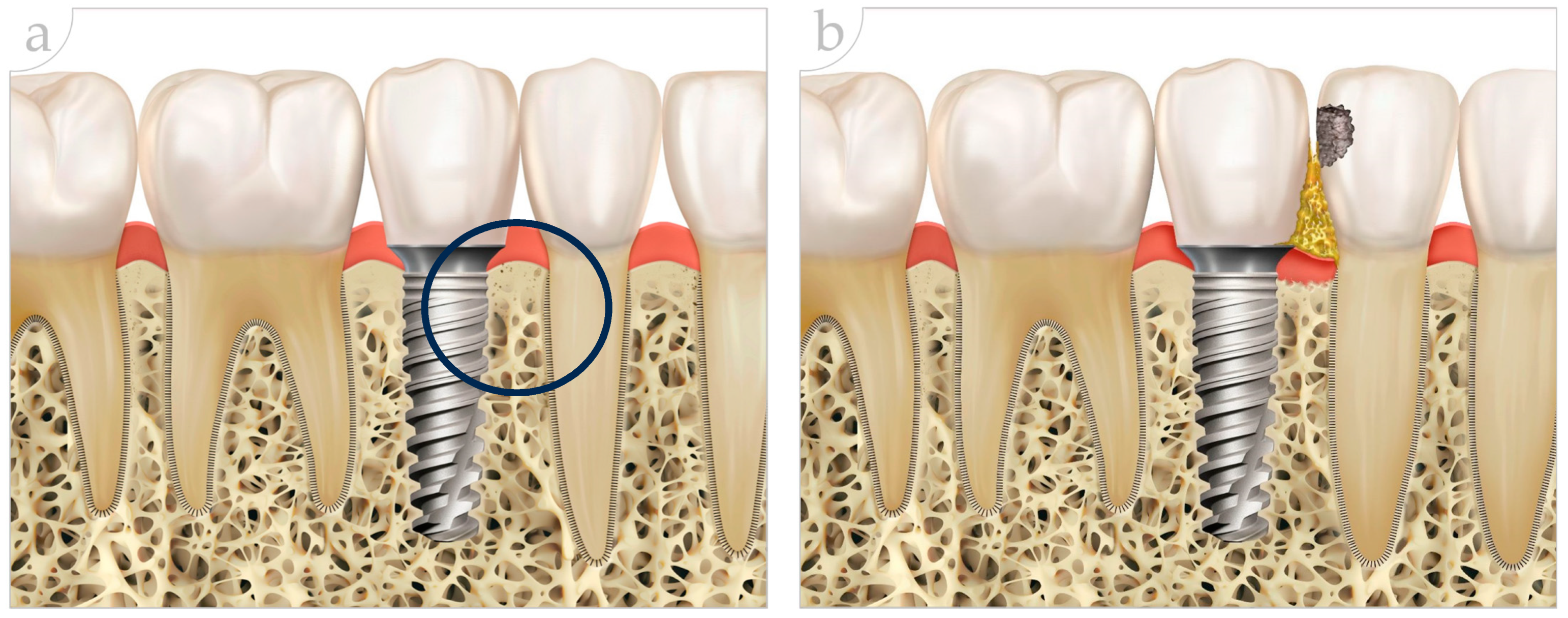
1. Introduction
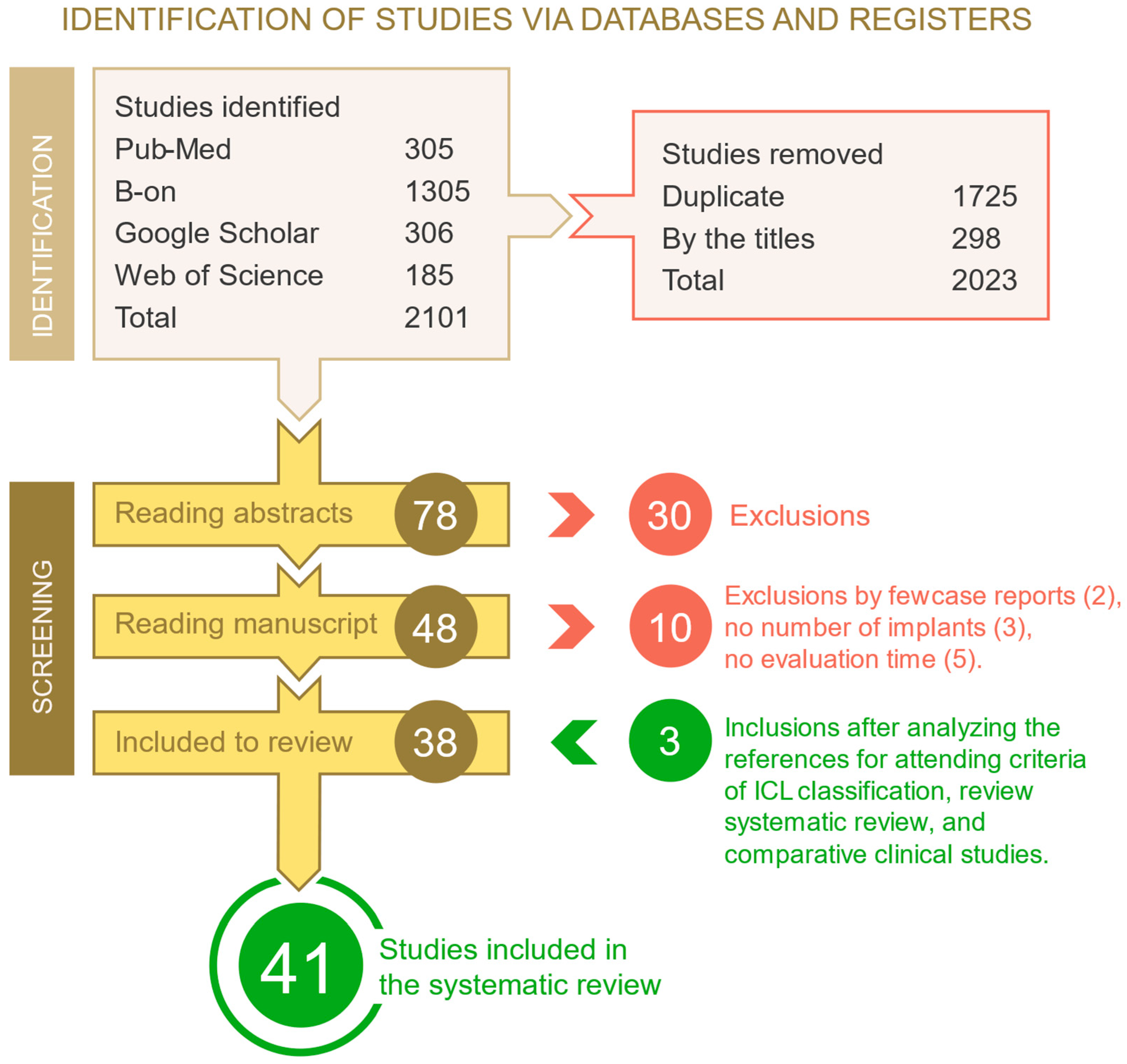
2. Materials and Methods
2.1. Inclusion Criteria, Exclusion Criteria and Eligibility
2.2. Search Strategies
2.3. Selection and Evaluation of Studies
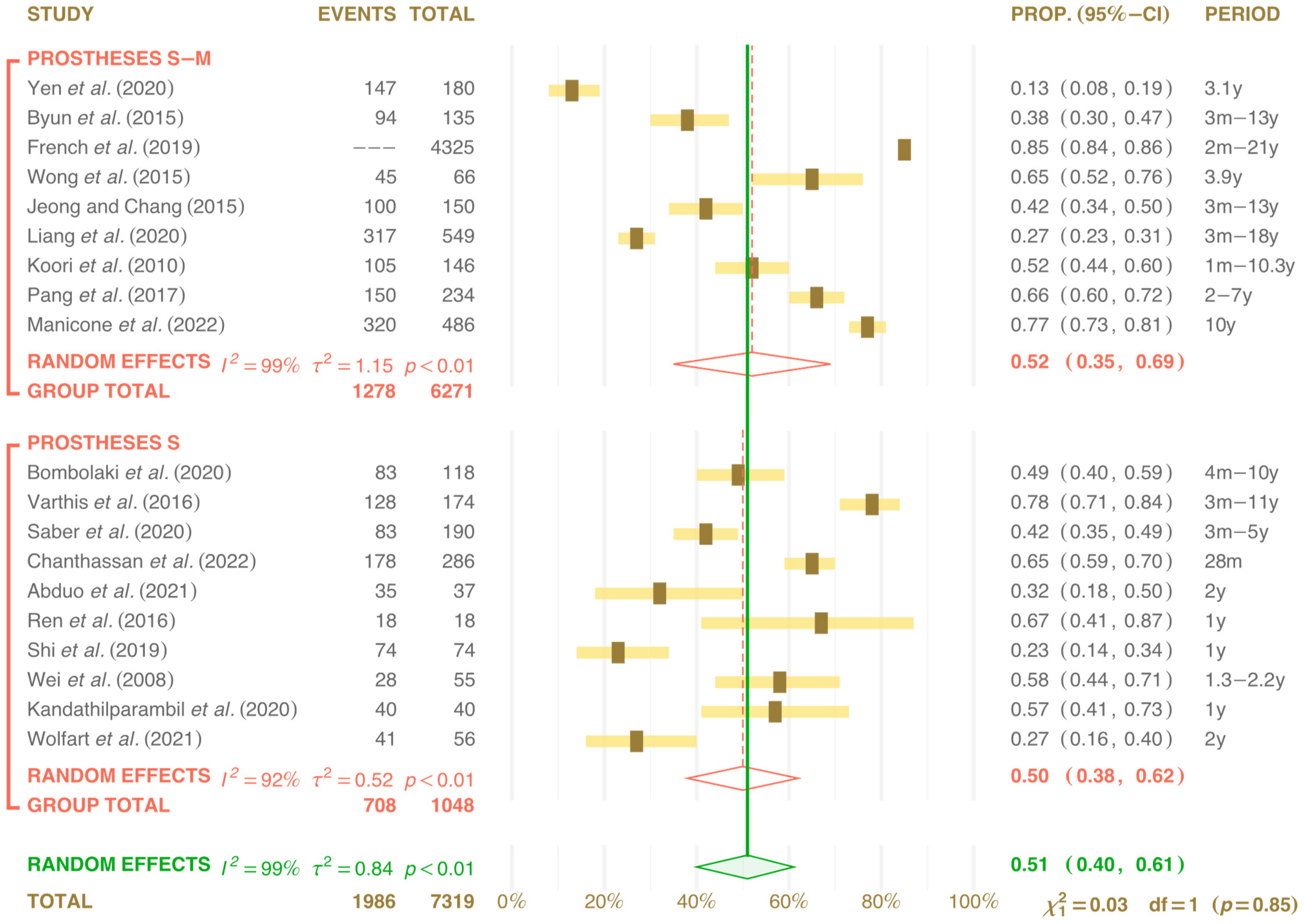
3. Results
| Study/Criteria | 1a | 2a | 3a | 3b | 6a | 6b | 7a | 7b | 8a | 8b | 9 | 10 | 11a | 11b | 12b | 13a | 13b | 15 | 16 | 17a | 17b | 18 | 23 | 24 | 25 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [1] | Yen et al. (2020) | × | × | × | × | |||||||||||||||||||||
| [7] | Byun et al. (2015) | × | × | × | × | × | × | × | ||||||||||||||||||
| [8] | Bombolaki et al. (2020) | × | × | × | × | × | × | |||||||||||||||||||
| [14] | Varthis et al. (2015) | × | × | × | × | × | × | |||||||||||||||||||
| [15] | Saber et al. (2020) | × | × | × | × | × | × | |||||||||||||||||||
| [19] | French et al. (2019) | × | × | × | × | × | × | |||||||||||||||||||
| [20] | Latimer et al. (2020) | × | × | × | × | × | × | × | × | × | × | × | × | |||||||||||||
| [22] | Chanthassan et al. (2020) | × | × | × | × | × | × | × | × | × | ||||||||||||||||
| [23] | Wong et al. (2015) | × | × | × | × | × | × | × | ||||||||||||||||||
| [24] | Liang et al. (2020) | × | × | × | × | × | × | × | × | × | ||||||||||||||||
| [25] | Shi et al. (2019) | × | × | × | × | × | × | × | × | × | × | × | × | × | ||||||||||||
| [26] | Wei et al. (2008) | × | × | × | × | |||||||||||||||||||||
| [27] | Koori et al. (2010) | × | × | × | × | × | × | × | × | |||||||||||||||||
| [28] | Pang et al. (2017) | × | × | × | × | × | × | × | × | × | × | |||||||||||||||
| [29] | Wolfart et al. (2021) | × | × | × | × | × | × | × | × | × | × | × | ||||||||||||||
| [30] | Manicone et al. (2021) | × | × | × | × | × | × | × | ||||||||||||||||||
| [31] | Jeong and Chang (2015) | × | × | × | × | × | × | × | ||||||||||||||||||
| [32] | Abduo et al. (2021) | × | × | × | × | × | × | × | × | × | × | × | × | |||||||||||||
| [33] | Ren et al. (2016) | × | × | × | × | × | × | × | × | |||||||||||||||||
| [34] | Kandathilparambil et al. (2020) | × | × | × | × | × | × | × | × | |||||||||||||||||
| Study | Type | TP | Mx Md | PN | A/P | M | D | Diagnostic | Prot | Ret | FI | Bio Alt | Evaluation Period | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [1] | Yen et al. (2020) | Re | 147 | Mx/Md | 180 | AP | 13.0% | 2.3% | Rx 50 mm | S-M | CR | OK | NA | 3.1 years |
| [7] | Byun et al. (2015) | Re | 94 | Mx/Md | 135 | AP | 38.1% | 24.6% | Dental floss | S-M | CR | OK | SA | 3 months at 13 years |
| [8] | Bombolaki et al. (2020) | Re | 83 | 33 Mx 50 Md | 118 | P | 48.8% | 26.7% | 12 mm strips | S | SR | OK | SA | 4 months at 10 years |
| [14] | Varthis et al. (2015) | Re | 128 | 57.9% Ma 49.0% Md | 174 | AP | 78.2% | 21.8% | 70 μm floss + Rx | S | CR | OK | NA | 3 months at 11 years |
| [15] | Saber et al. (2020) | Re | 83 | 34.1% Ma 31.5% Md | 190 | AP | 42.1% | 13.5% | 70 μm floss + Rx | S | CR | OK | Mucosite | 3 months at 5 years |
| [19] | French et al. (2019) | Re | NR | 58.0% Mx 42.0% Md | 4325 | AP | 85.4% | 11.6% | 50 μm floss + Rx | S-M | CR | OK | Mucosite | 2 months at 21 years |
| [22] | Chanthassan et al. (2020) | Re | 178 | Mx Md | 286 | P | 64.8% | 35.2% | Floss | S | CR | OK | Mucosite | 28 months |
| [23] | Wong et al. (2015) | Re | 45 | 18 Mx 48 Md | 66 | P | 65.0% | Matrix 38 μm | S-M | CR | OK | NA | 3.9 years | |
| [24] | Liang et al. (2020) | Re | 317 | Mx Md | 549 | P | 27.0% | 5.0% | Dental floss | S-M | CR | OK | NA | 3 months at 18 years |
| [25] | Shi et al. (2019) | Pr | 74 | 34 Ma 40 Md | 74 | P | 23.0% | 25.7% | Dental floss | S | CR | OK | NA | 1 year |
| [26] | Wei et al. (2008) | Re | 28 | 66 Mx 54 Md | 55 | AP | 58.0% | Matrix 50 μm | NA | NA | OK | NA | 1.3 to 2.2 years | |
| [27] | Koori et al. (2010) | Re | 105 | 146 | AP | 51.8% | 15.6% | Matrix 50 μm | S-M | NA | OK | NA | 1 month at 10.3 years | |
| [28] | Pang et al. (2017) | Pr | 150 | 122 Ma 177 Md | 234 | P | 66.2% | 36.9% | Matrix 50 to 100 μm | S-M | CR | OK | SA | 2 at 7 years |
| [29] | Wolfart et al. (2021) | Pr | 41 | Mx Md | 56 | P | 26.4% | 14.6% | Matrix 50 μm | S | SR | OK | SA | 2 years |
| [30] | Manicone et al. (2021) | Re | 320 | Mx Md | 486 | AP | 77.0% | 23.0% | Floss + Rx | S-M | CR | OK | Mucosite | 10 years |
| [31] | Jeong and Chang (2015) | Re | 100 | Mx/Md | 150 | AP | 42.0% | Dental floss | S-M | CR | OK | Bio Alt | 3 months | |
| [32] | Abduo et al. (2021) | Pr | 35 | NR | 37 | P | 63.2% | 36.2% | Dental floss | S | SR | NA | SA | 2 years |
| [33] | Ren et al. (2016) | Pr | 18 | NR | 18 | P | 64.8% | Matrix 50 μm | S | CR | OK | NA | 1 year | |
| [34] | Kandathilparambil et al. (2020) | Pr | 40 | Md | 40 | P | 57.9% | 38.9% | Matrix 50 μm + dig | S | CR | OK | NA | 1 year |
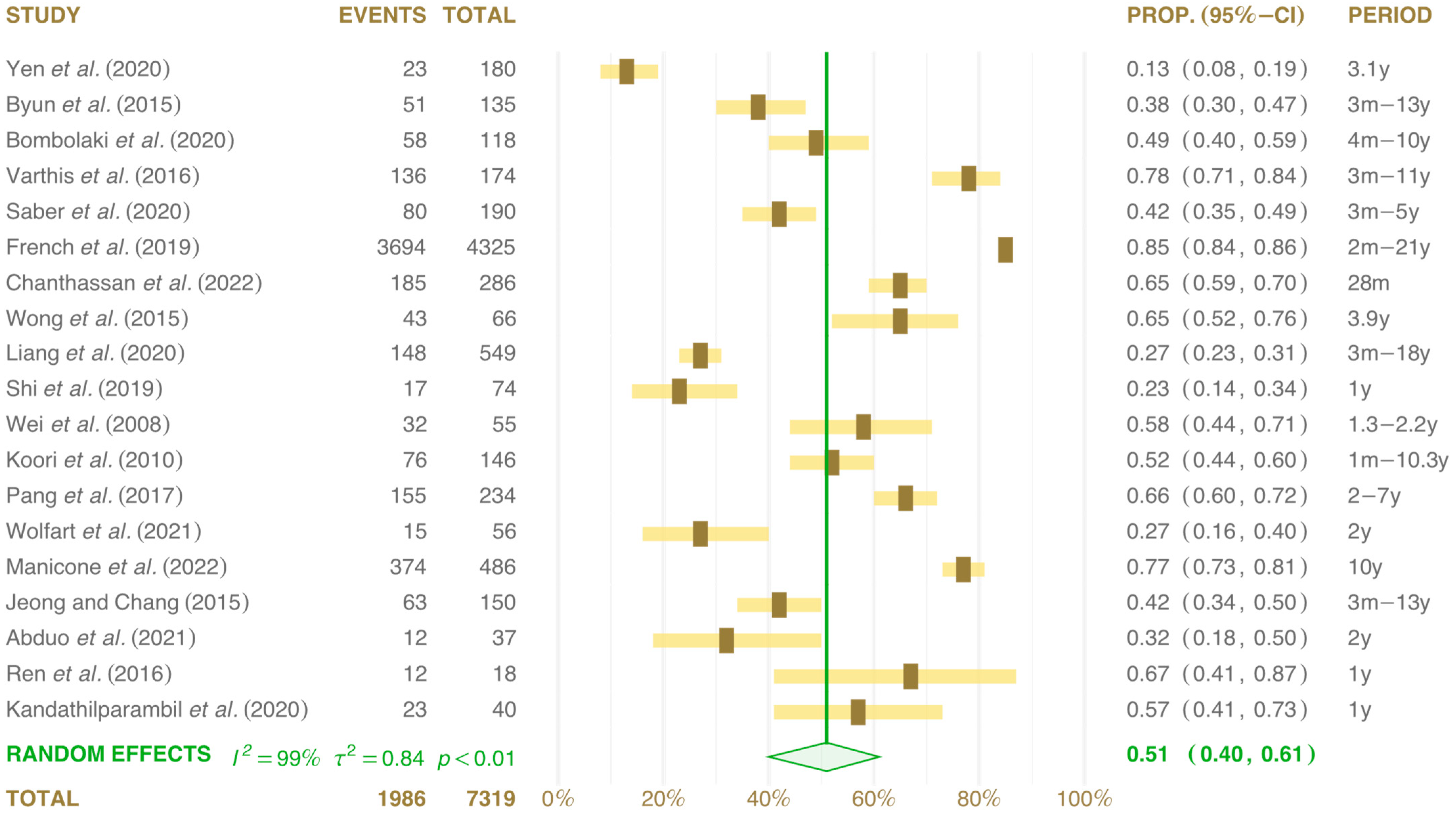
4. Discussion
4.1. Evaluation of Interproximal Contact Loss (ICL)
4.2. Food Impaction (FI)
4.3. Factors for Interproximal Contact Loss (ICL)
4.4. Clinical Effects of Interproximal Contact Loss (ICL)
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Yen, J.Y.; Kang, L.; Chou, I.C.; Lai, Y.L.; Lee, S.Y. Risk assessment of interproximal contact loss between implant-supported fixed prostheses and adjacent teeth. A retrospective radiographic study. J. Prosthet. Dent. 2022, 127, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Khairnar, M. Classification of food impaction-revisited and its management. Indian J. Dent. Adv. 2013, 5, 113–119. [Google Scholar] [CrossRef]
- Jo, D.W.; Kwon, M.J.; Kim, J.H.; Kim, Y.K.; Yi, Y.J. Evaluation of adjacent tooth displacement in the posterior implant restoration with proximal contact loss by superimposition of digital models. J. Adv. Prosthodont. 2019, 11, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Lu, X. The influence of contact area between implant and its adjacent teeth on finite element analysis. Vibroeng. PROCEDIA 2019, 22, 182–187. [Google Scholar] [CrossRef]
- Gasser, T.J.W.; Papageorgiou, S.N.; Eliades, T.; Hämmerle, C.H.F.; Thoma, D.S. Interproximal contact loss at implant sites: A retrospective clinical study with a 10-year follow-up. Clin. Oral Implant. Res. 2022, 33, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Chopra, A.; Sivaraman, K.; Narayan, A.I.; Balakrishnan, D. Etiology and classification of food impaction around implants and implant-retained prosthesis. Clin. Implant. Dent. Relat. Res. 2019, 21, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Byun, S.J.; Heo, S.M.; Ahn, S.G.; Chang, M. Analysis of proximal contact loss between implant-supported fixed dental prostheses and adjacent teeth in relation to influential factors and effects. A cross-sectional study. Clin. Oral Implant. Res. 2015, 26, 709–714. [Google Scholar] [CrossRef]
- Bompolaki, D.; Edmondson, S.A.; Katancik, J.A. Interproximal contact loss between implant-supported restorations and adjacent natural teeth: A retrospective cross-sectional study of 83 restorations with an up to 10-year follow-up. J. Prosthet. Dent. 2022, 127, 418–424. [Google Scholar] [CrossRef]
- Li, Q.L.; Ying Cao, C.; Xu, Q.J.; Xu, X.H.; Yin, J.L. Atraumatic Restoration of Vertical Food Impaction with an Open Contact Using Flowable Composite Resin Aided by Cerclage Wire under Tension. Scientifica 2016, 2016, 4127472. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, G.; Carpentieri, J.; Cavallaro, J. Open contacts adjacent to dental implant restorations: Etiology, incidence, consequences, and correction. J. Am. Dent. Assoc. 2016, 147, 28–34. [Google Scholar] [CrossRef]
- Sfondouris, T.; Prestipino, V. Chairside management of an open proximal contact on an implant-supported ceramic crown using direct composite resin. J. Prosthet. Dent. 2019, 122, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Fathi, A.; Mosharraf, R.; Ebadian, B.; Javan, M.; Isler, S.; Dezaki, S.N. Prevalence of Proximal Contact Loss between Implant-Supported Prostheses and Adjacent Natural Teeth: An Umbrella Review. Eur. J. Dent. 2022, 16, 742–748. [Google Scholar] [CrossRef] [PubMed]
- Manicone, P.F.; De Angelis, P.; Rella, E.; Papetti, L.; D’Addona, A. Proximal Contact Loss in Implant-Supported Restorations: A Systematic Review and Meta-Analysis of Prevalence. J. Prosthodont. 2022, 31, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Varthis, S.; Randi, A.; Tarnow, D.P. Prevalence of Interproximal Open Contacts Between Single-Implant Restorations and Adjacent Teeth. Int. J. Oral Maxillofac. Implant. 2016, 31, 1089–1092. [Google Scholar] [CrossRef] [PubMed]
- Saber, A.; Chakar, C.; Mokbel, N.; Nohra, J. Prevalence of Interproximal Contact Loss Between Implant-Supported Fixed Prostheses and Adjacent Teeth and Its impact on Marginal Bone Loss: A Retrospective Study. Int. J. Oral Maxillofac. Implant. 2020, 35, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, G.; Carpenter, J.R.; Rücker, G. Meta-Analysis with R, Use R! Springer: Cham, Switzerland, 2015. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- French, D.; Naito, M.; Linke, B. Interproximal contact loss in a retrospective cross-sectional study of 4325 implants: Distribution and incidence and the effect on bone loss and peri-implant soft tissue. J. Prosthet. Dent. 2019, 122, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Latimer, J.M.; Gharpure, A.S.; Kahng, H.J.; Aljofi, F.E.; Daubert, D.M. Interproximal open contacts between implant restorations and adjacent natural teeth as a risk-indicator for peri-implant disease—A cross-sectional study. Clin. Oral Implant. Res. 2021, 32, 598–607. [Google Scholar] [CrossRef]
- Mehanna, S.; Habre-Hallage, P. Proximal contact alterations between implant-supported restorations and adjacent teeth in the posterior region: A 3-month prospective study. J. Clin. Exp. Dent. 2021, 13, 479–486. [Google Scholar] [CrossRef]
- Chanthasan, S.; Mattheos, N.; Pisarnturakit, P.P.; Pimkhaokham, A.; Subbalekha, K. Influence of interproximal peri-implant tissue and prosthesis contours on food impaction, tissue health and patients quality of life. Clin. Oral Implant. Res. 2022, 33, 768–781. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.T.; Way, P.Y.; Pow, E.H.; Leung, K.C. Proximal contact loss between implant-supported prostheses and adjacent natural teeth: A retrospective study. Clin. Oral Implant. Res. 2015, 26, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.H.; Nien, C.Y.; Chen, Y.L.; Hsu, K.W. The prevalence and associated factors of proximal contact loss between implant restoration and adjacent tooth after function: A retrospective study. Clin. Implant. Dent. Relat. Res. 2020, 22, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.Y.; Zhu, Y.; Gu, Y.X.; Lai, H.C. Proximal Contact Alterations between Implant-Supported Restorations and Adjacent Natural Teeth in the Posterior Region: A 1-Year Preliminary Study. Int. J. Oral Maxillofac. Implant. 2019, 34, 165–168. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.; Tomotake, Y.; Nagao, K.; Ichikawa, T. Implant prostheses and adjacent tooth migration: Preliminary retrospective survey using 3-dimensional occlusal analysis. Int. J. Prosthodont. 2008, 21, 302–304. [Google Scholar] [PubMed]
- Koori, H.; Morimoto, K.; Tsukiyama, Y.; Koyano, K. Statistical analysis of the diachronic loss of interproximal contact between fixed implant prostheses and adjacent teeth. Int. J. Prosthodont. 2010, 23, 535–540. [Google Scholar] [PubMed]
- Pang, N.S.; Suh, C.S.; Kim, K.D.; Park, W.; Jung, B.Y. Prevalence of proximal contact loss between implant-supported fixed prostheses and adjacent natural teeth and its associated factors: A 7-year prospective study. Clin. Oral Implant. Res. 2017, 28, 1501–1508. [Google Scholar] [CrossRef] [PubMed]
- Wolfart, S.; Rittich, A.; Gro, B.K.; Hartkamp, O.; von der Stück, A.; Raith, S.; Reich, S. Cemented versus screw-retained posterior implant-supported single crowns: A 24-month randomized controlled clínical trial. Clin. Oral Implant. Res. 2021, 32, 1484–1495. [Google Scholar] [CrossRef]
- Manicone, P.F.; De Angelis, P.; Papetti, L.; Rella, E.; De Angelis, S.; D’Addona, A. Analysis of Proximal Contact Loss Between Implant Restorations and Adjacent Teeth: A 10-Year Retrospective Study. Int. J. Periodont. Restor. Dent. 2022, 42, 113–119. [Google Scholar] [CrossRef]
- Jeong, J.S.; Chang, M. Food Impaction and Periodontal/Peri-Implant Tissue Conditions in Relation to the Embrasure Dimensions Between Implant-Supported Fixed Dental Prostheses and Adjacent Teeth: A Cross-Sectional Study. J. Periodontol. 2015, 86, 1314–1320. [Google Scholar] [CrossRef]
- Abduo, J.; Lee, C.L.; Sarfarazi, G.; Xue, B.; Judge, R.; Darby, I. Encode Protocol Versus Conventional Protocol for Single-Implant Restoration: A Prospective 2-Year Follow-Up Randomized Controlled Trial. J. Oral Implant. Implantol. 2021, 47, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Ren, S.; Lin, Y.; Hu, X.; Wang, Y. Changes in proximal contact tightness between fixed implant prostheses and adjacent teeth: A 1-year prospective study. J. Prosthet. Dent. 2016, 115, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Kandathilparambil, M.R.; Nelluri, V.V.; Vayadadi, B.C.; Gajjam, N.K. Evaluation of biological changes at the proximal contacts between single-tooth implant-supported prosthesis and the adjacent natural teeth—An in vivo study. J. Indian Prosthodont. Soc. 2020, 20, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Lau, D. Proximal contact loss between implant prostheses and adjacent natural teeth: A qualitative systematic review of prevalence, influencing factors and implications. Heliyon 2022, 8, e10064. [Google Scholar] [CrossRef]
- Bento, V.A.A.; Gomes, J.M.L.; Lemos, C.A.A.; Limirio, J.P.J.O.; Rosa, C.D.D.R.D.; Pellizzer, E.P. Prevalence of proximal contact loss between implant-supported prostheses and adjacent natural teeth: A systematic review and meta-analysis. J. Prosthet. Dent. 2023, 129, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, J.; Zhou, J.; Tan, J. Closing open contacts adjacent to an implant-supported restoration. J. Dent. Sci. 2019, 14, 216–218. [Google Scholar] [CrossRef] [PubMed]
- Oh, W.S.; Oh, J.; Valcanaia, A.J. Open Proximal Contact with Implant-Supported Fixed Prostheses Compared with Tooth-Supported Fixed Prostheses: A Systematic Review and Meta-analysis. Int. J. Oral Maxillofac. Implant. 2020, 30, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, S.; Oveisi-Oskouei, L.; Torab, A.; Salehi-Pourmehr, H.; Babaloo, A.; Vahed, N.; Abolhasanpour, N.; Taghilou, S.; Ghasemi, A. Prevalence of proximal contact loss between implant-supported fixed prosthesis and adjacent teeth and associated factors: A systematic review and meta-analysis. J. Adv. Periodont. Implant. Dent. 2022, 14, 119–133. [Google Scholar] [CrossRef] [PubMed]
- Murugan Jeyasree, R.; Muthuraj, T. An Insight into Classification, Diagnosis and Comprehensive Management of Food Impaction. In Periodontology—New Insights; IntechOpen: London, UK, 2022. [Google Scholar] [CrossRef]
- Kim, J.Y.; Lim, Y.J.; Heo, Y.K. Modification of framework design for an implant-retained fixed restoration helps when proximal contact loss occurs. J. Dent. Sci. 2019, 14, 213–215. [Google Scholar] [CrossRef] [PubMed]
- Papalexopoulos, D.; Samartzi, T.K.; Tsirogiannis, P.; Sykaras, N.; Sarafianou, A.; Kourtis, S.; Mikeli, A. Impact of maxillofacial growth on implants placed in adults: A narrative review. J. Esthet. Restor. Dent. 2023, 35, 467–478. [Google Scholar] [CrossRef]
- Manouchehri, E.; Alirezaei, S.; Roudsari, R.L. Compliance of Published Randomized Controlled Trials on the Effect of Physical Activity on Primary Dysmenorrhea with the Consortium’s Integrated Report on Clinical Trials Statement: A Critical Appraisal of the Literature. Iran. J. Nurs. Midwifery Res. 2020, 25, 445–454. [Google Scholar] [CrossRef] [PubMed]
- French, D.; French, M.-C.; Linke, B.; Lizotte, J. Two-center observational case series describing Decay Adjacent to Fixed Implant Restations (DATFIR) and evaluation of case parameters. J. Oral Sci. 2018, 4, 32–41. Available online: https://www.researchgate.net/publication/325021520_Two-Center_Observational_Case_Series_Describing_Decay_Adjacent_to_Fixed_Implant_Restorations_DATFIR_and_Evaluation_of_Case_Parameters (accessed on 10 June 2024).

| Exclusion Criteria | Number of Studies Excluded |
|---|---|
| Clinical data < 1 year follow up | 2 |
| Case reports without number of implants | 3 |
| Experimental laboratory studies | 5 |
| Animal studies | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nery, J.C.; Manarte-Monteiro, P.; Aragão, L.; da Silva, L.P.; Brandão, G.S.P.; Lemos, B.F. Clinical Effects of Interproximal Contact Loss between Teeth and Implant-Supported Prostheses: Systematic Review and Meta-Analysis. Prosthesis 2024, 6, 825-840. https://doi.org/10.3390/prosthesis6040059
Nery JC, Manarte-Monteiro P, Aragão L, da Silva LP, Brandão GSP, Lemos BF. Clinical Effects of Interproximal Contact Loss between Teeth and Implant-Supported Prostheses: Systematic Review and Meta-Analysis. Prosthesis. 2024; 6(4):825-840. https://doi.org/10.3390/prosthesis6040059
Chicago/Turabian StyleNery, James Carlos, Patrícia Manarte-Monteiro, Leonardo Aragão, Lígia Pereira da Silva, Gabriel Silveira Pinto Brandão, and Bernardo Ferreira Lemos. 2024. "Clinical Effects of Interproximal Contact Loss between Teeth and Implant-Supported Prostheses: Systematic Review and Meta-Analysis" Prosthesis 6, no. 4: 825-840. https://doi.org/10.3390/prosthesis6040059
APA StyleNery, J. C., Manarte-Monteiro, P., Aragão, L., da Silva, L. P., Brandão, G. S. P., & Lemos, B. F. (2024). Clinical Effects of Interproximal Contact Loss between Teeth and Implant-Supported Prostheses: Systematic Review and Meta-Analysis. Prosthesis, 6(4), 825-840. https://doi.org/10.3390/prosthesis6040059







