Implant-Prosthetic Rehabilitation of the Agenesis of Maxillary Lateral Incisors: A 2-Year Prospective Clinical Study with Full Digital Workflow
Abstract
1. Introduction
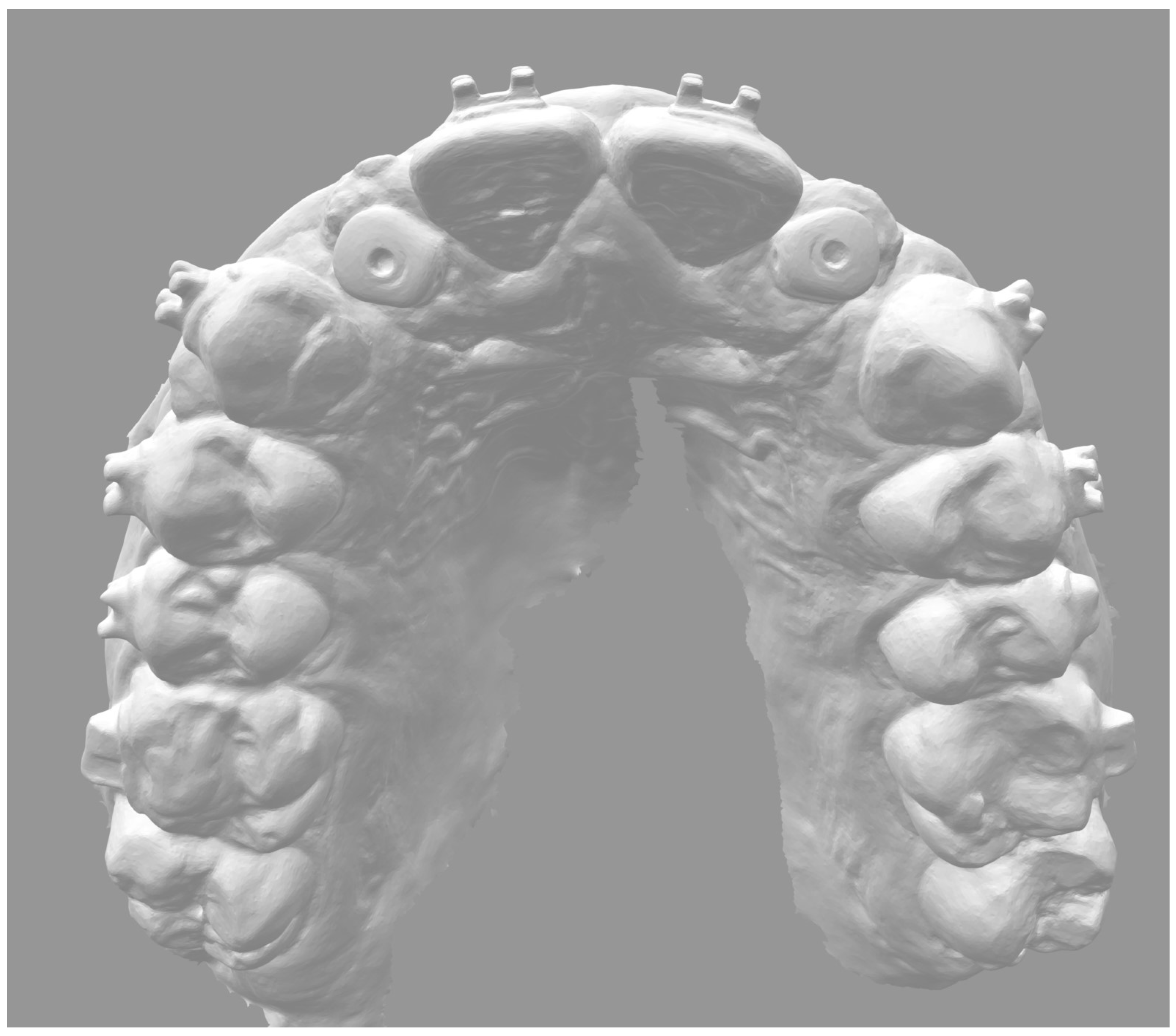
2. Materials and Methods
- -
- minimum age: 18 years (proven completion of facial growth);
- -
- single edentulous space (mono- or bilateral agenesis of maxillary lateral incisors);
- -
- presence of at least 10 pairs of opposing teeth;
- -
- intact adjacent teeth, restored with functionally and esthetically congruous reconstructions or restored with prostheses precluding the possibility of adding missing teeth;
- -
- refusal of alternative treatments (i.e., canine replacement, removable prosthesis, adhesive prosthesis, conventional or cantilevered fixed dental prostheses).
- -
- symptomatic temporo-mandibular dysfunctions;
- -
- inability to undergo surgical procedures;
- -
- pregnancy or breastfeeding;
- -
- abuse of medication and/or drugs;
- -
- psychosis and/or dysmorphophobia;
- -
- unachievable esthetic expectations;
- -
- poor bone quantity and/or quality (i.e., D3 or D4) or unsatisfactory conditions of the implant site (as highlighted by clinical and X-ray examinations);
- -
- bone volume in the implant site not sufficient to position a 3.3 mm × 10 mm narrow-diameter implant;
- -
- mouth opening and/or space between the dental arches insufficient for implant components (>4 cm);
- -
- incomplete facial growth and/or tooth eruption.
- -
- 0–3 months: patient recruitment;
- -
- 4–10 months: periodontal and orthodontic preparation (if necessary) and implant surgery;
- -
- 11–12 months: prosthetic finalization and baseline control (T0);
- -
- 24 months: 1-year follow-up;
- -
- 36 months: 2-year follow-up.
- -
- interproximal conditions (contact areas and papillae);
- -
- occlusion (static and dynamic);
- -
- appearance of the crown (margin and color);
- -
- peri-implant soft tissues (quantity and quality);
- -
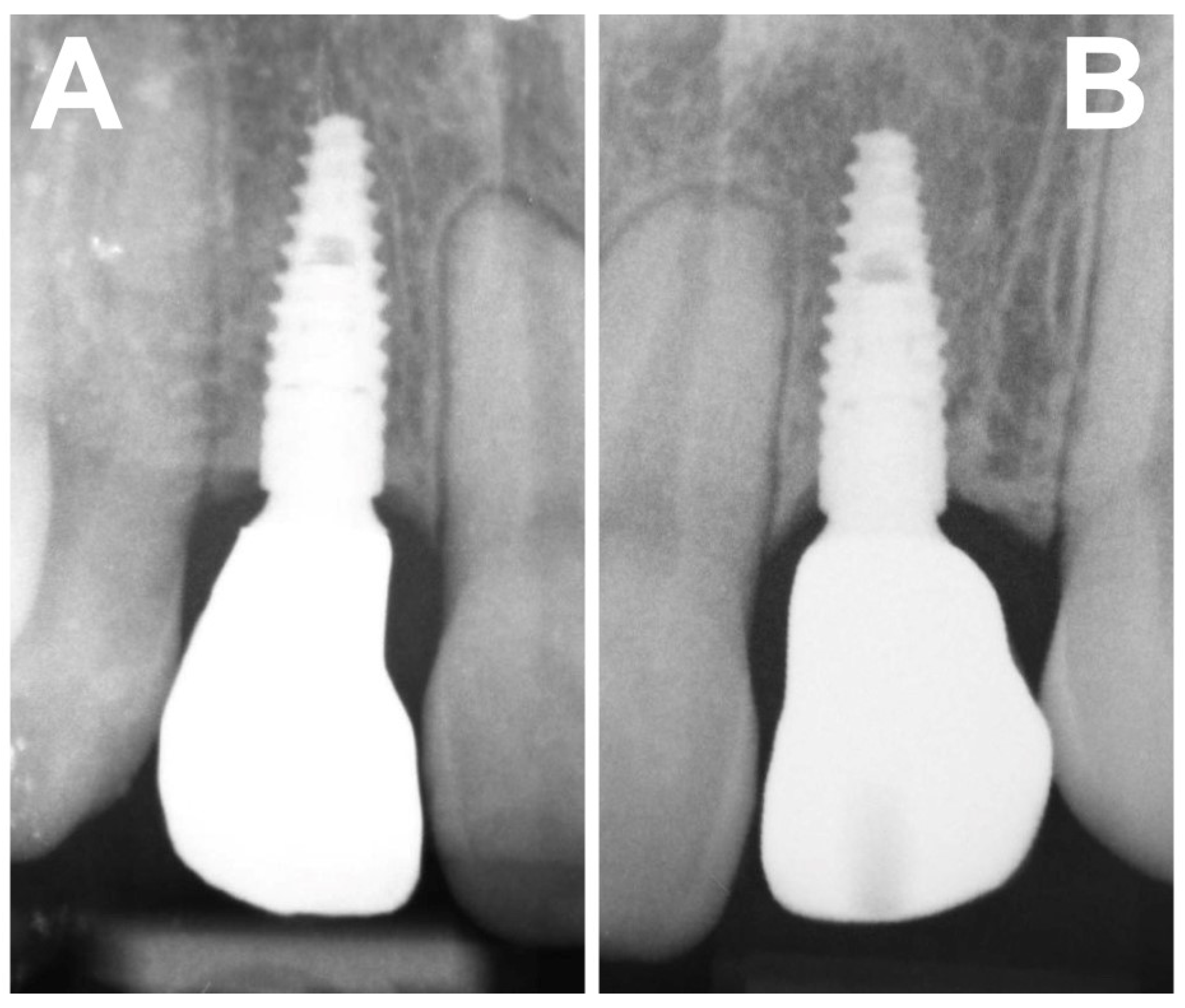
- marginal bone tissue (radiographic evaluation).
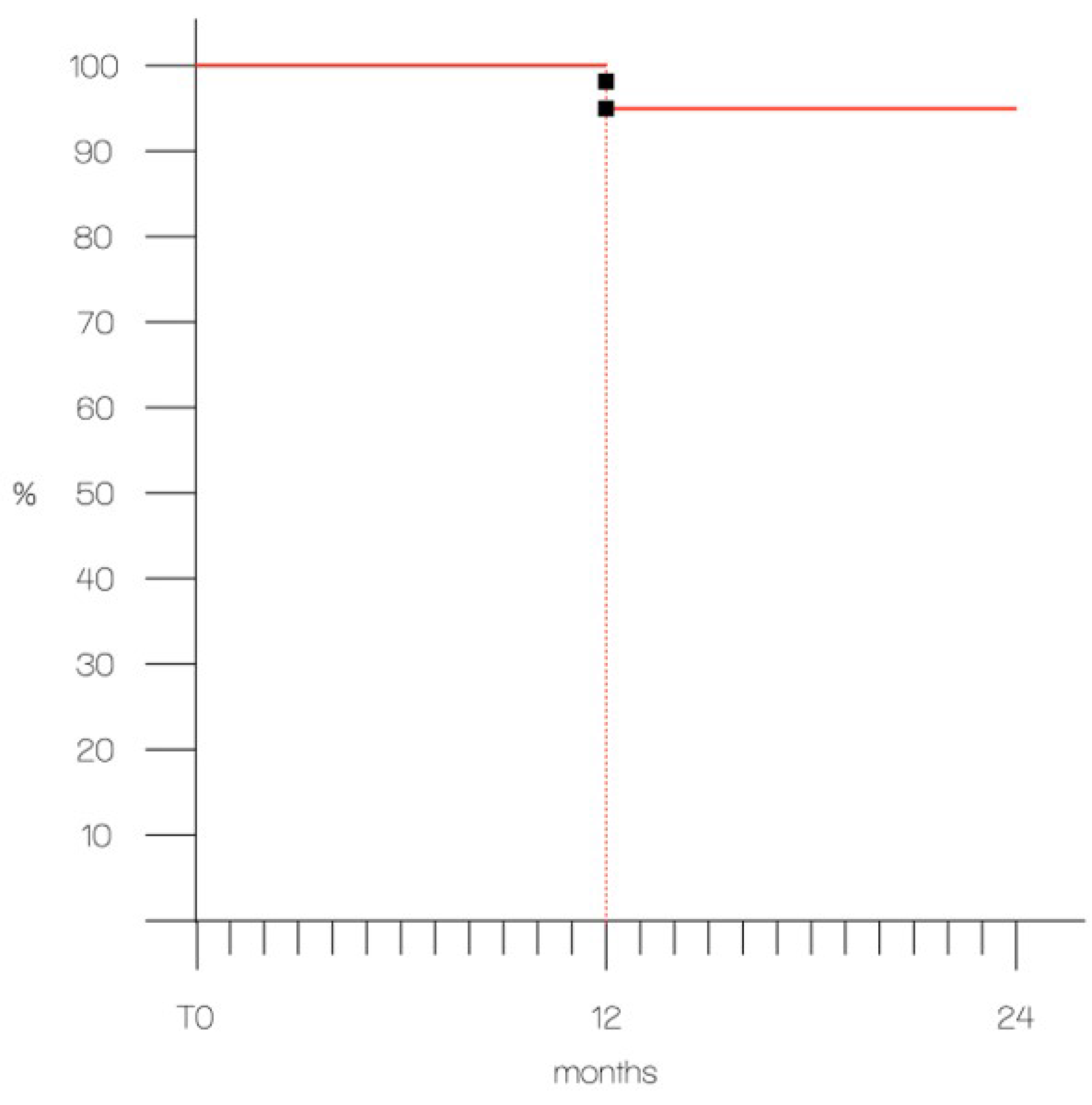
3. Results
- -
- score from 0 to 5: 0 restorations
- -
- score 6: 1 restoration
- -
- score 7: 3 restorations
- -
- score 8: 8 restorations
- -
- score 9: 9 restorations
- -
- score 10: 9 restorations
4. Discussion
5. Conclusions
- -
- in the 2-year short-term, both implants and zirconia crowns did not show significant technical or biological complications, achieving high survival and success rates;
- -
- in standard clinical conditions, the implant-prosthetic rehabilitation can be considered a viable choice option for the treatment of the agenesis of maxillary lateral incisors.
- -
- as regards the subjective evaluation of patients, both the function and esthetics of the restorations were considered fully satisfactory.
- -
- an interdisciplinary approach to the treatment plan represents an essential pre-requisite for achieving functional and esthetic success.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- The Glossary of Prosthodontic Terms: Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [CrossRef] [PubMed]
- Stamatiou, J.; Symons, A.L. Agenesis of the permanent lateral incisor: Distribution, number and sites. J. Clin. Pediatr. Dent. 1991, 15, 244–246. [Google Scholar] [PubMed]
- Pandey, P.; Ansari, A.A.; Choudhary, K.; Saxena, A. Familial aggregation of maxillary lateral incisor agenesis (MLIA). BMJ Case Rep. 2013, 2013, bcr2012007846. [Google Scholar] [CrossRef] [PubMed]
- Hua, F.; He, H.; Ngan, P.; Bouzid, W. Prevalence of peg-shaped maxillary permanent lateral incisors: A meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 97–109. [Google Scholar] [CrossRef]
- Rosa, M.; Olimpo, A.; Fastuca, R.; Caprioglio, A. Perceptions of dental professionals and laypeople to altered dental esthetics in cases with congenitally missing maxillary lateral incisors. Prog. Orthod. 2013, 14, 34. [Google Scholar] [CrossRef]
- Laverty, D.P.; Thomas, M.B. The restorative management of microdontia. Br. Dent. J. 2016, 221, 160–166. [Google Scholar] [CrossRef]
- Kinzer, G.A.; Kokich, V.O., Jr. Managing congenitally missing lateral incisors. Part II: Tooth-supported restorations. J. Esthet. Restor. Dent. 2005, 17, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Pithon, M.M.; Vargas, E.O.A.; da Silva Coqueiro, R.; Lacerda-Santos, R.; Tanaka, O.M.; Maia, L.C. Impact of oral-health-related quality of life and self-esteem on patients with missing maxillary lateral incisor after orthodontic space closure: A single-blinded, randomized, controlled trial. Eur. J. Orthod. 2021, 43, 208–214. [Google Scholar] [CrossRef]
- Priest, G. The treatment dilemma of missing maxillary lateral incisors-Part II: Implant restoration. J. Esthet. Restor. Dent. 2019, 31, 319–326. [Google Scholar] [CrossRef]
- Šikšnelytė, J.; Guntulytė, R.; Lopatienė, K. Orthodontic canine substitution vs. implant-supported prosthetic replacement for maxillary permanent lateral incisor agenesis: A systematic review. Stomatologija 2021, 23, 106–113. [Google Scholar]
- Momberger, N.; Mukaddam, K.; Zitzmann, N.U.; Bornstein, M.A.; Filippi, A.; Kühl, S. Esthetic and functional outcomes of narrowdiameter implants compared in a cohort study to standard diameter implants in the anterior zone of the maxilla. Quintessence Int. 2022, 53, 502–509. [Google Scholar] [PubMed]
- Parize, H.N.; Bohner, L.O.L.; Gama, L.T.; Porporatti, A.L.; Mezzomo, L.A.M.; Martin, W.C.; Gonçalves, T.M.S.V. Narrow-diameter implants in the anterior region: A meta-analysis. Int. J. Oral Maxillofac. Implant. 2019, 34, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Telles, L.H.; Portella, F.F.; Rivaldo, E.G. Longevity and marginal bone loss of narrow-diameter implants supporting single crowns: A systematic review. PLoS ONE 2019, 14, e0225046. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, R.; Galli, M.; Chen, Z.; Mendonça, G.; Meirelles, L.; Wang, H.L.; Chan, H.L. Intraoral scanning reduces procedure time and improves patient comfort in fixed prosthodontics and implant dentistry: A systematic review. Clin. Oral Investig. 2021, 25, 6517–6531. [Google Scholar] [CrossRef] [PubMed]
- Haddadi, Y.; Bahrami, G.; Isidor, F. Evaluation of Operating Time and Patient Perception Using Conventional Impression Taking and Intraoral Scanning for Crown Manufacture: A Split-mouth, Randomized Clinical Study. Int. J. Prosthodont. 2018, 31, 55–59. [Google Scholar] [CrossRef]
- Resende, C.C.D.; Barbosa, T.A.Q.; Moura, G.F.; Tavares, L.D.N.; Rizzante, F.A.P.; George, F.M.; Neves, F.D.D.; Mendonça, G. Influence of operator experience, scanner type, and scan size on 3D scans. J. Prosthet. Dent. 2021, 125, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Bishti, S.; Tuna, T.; Rittich, A.; Wolfart, S. Patient-reported outcome measures (PROMs) of implant-supported reconstructions using digital workflows: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2021, 32 (Suppl. S21), 318–335. [Google Scholar] [CrossRef]
- Barros Vde, M.; Costa, N.R.; Martins, P.H.; Vasconcellos, W.A.; Discacciati, J.A.; Moreira, A.N. Definitive Presurgical CAD/CAM-Guided Implant-Supported Crown in an Esthetic Area. Braz. Dent. J. 2015, 26, 695–700. [Google Scholar] [CrossRef]
- da Silva Salomão, G.V.; Chun, E.P.; Panegaci, R.D.S.; Santos, F.T. Analysis of Digital Workflow in Implantology. Case Rep. Dent. 2021, 2021, 6655908. [Google Scholar] [CrossRef]
- Gianfreda, F.; Pesce, P.; Marcano, E.; Pistilli, V.; Bollero, P.; Canullo, L. Clinical Outcome of Fully Digital Workflow for Single-Implant-Supported Crowns: A Retrospective Clinical Study. Dent. J. 2022, 10, 139. [Google Scholar] [CrossRef]
- Joda, T.; Zarone, F.; Zitzmann, N.U.; Ferrari, M. The Functional Implant Prosthodontic Score (FIPS): Assessment of reproducibility and observer variability. Clin. Oral Investig. 2018, 22, 2319–2324. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Bäumer, D.; Ozga, A.K.; Körner, G.; Bäumer, A. Patient satisfaction and oral health-related quality of life 10 years after implant placement. BMC Oral Health 2021, 21, 30. [Google Scholar] [CrossRef] [PubMed]
- King, P.; Maiorana, C.; Luthardt, R.G.; Sondell, K.; Øland, J.; Galindo-Moreno, P.; Nilsson, P. Clinical and radiographic evaluation of a small-diameter dental implant used for the restoration of patients with permanent tooth agenesis (hypodontia) in the maxillary lateral incisor and mandibular incisor regions: A 36-month follow-up. Int. J. Prosthodont. 2016, 29, 147–153. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sorrentino, R.; Di Mauro, M.I.; Leone, R.; Ruggiero, G.; Annunziata, M.; Zarone, F. Implant–Prosthetic Rehabilitation of Maxillary Lateral Incisor Agenesis with Narrow Diameter Implants and Metal–Ceramic vs. All-Ceramic Single Crowns: A 16-Year Prospective Clinical Study. Appl. Sci. 2023, 13, 964. [Google Scholar] [CrossRef]
- Branzén, M.; Eliasson, A.; Arnrup, K.; Bazargani, F. Implant-Supported Single Crowns Replacing Congenitally Missing Maxillary Lateral Incisors: A 5-Year Follow-Up. Clin. Implant Dent. Relat. Res. 2015, 17, 1134–1140. [Google Scholar] [CrossRef]
- De-Marchi, L.M.; Pini, N.I.; Ramos, A.L.; Pascotto, R.C. Smile attractiveness of patients treated for congenitally missing maxillary lateral incisors as rated by dentists, laypersons, and the patients themselves. J. Prosthet. Dent. 2014, 112, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, A.; Perillo, L.; Rosa, M. Missing upper incisors: A retrospective study of orthodontic space closure versus implant. Prog. Orthod. 2015, 16, 2. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Bragger, U. Digital vs. conventional implant prosthetic workflows: A cost/time analysis. Clin. Oral Implant. Res. 2015, 26, 1430–1435. [Google Scholar] [CrossRef]
- Joda, T.; Gintaute, A.; Brägger, U.; Ferrari, M.; Weber, K.; Zitzmann, N.U. Time-efficiency and cost-analysis comparing three digital workflows for treatment with monolithic zirconia implant fixed dental prostheses: A double-blinded RCT. J. Dent. 2021, 113, 103779. [Google Scholar] [CrossRef]








| Variable | 0 | 1 | 2 |
|---|---|---|---|
| Interproximal conditions (contact areas and papillae) | Major discrepancies (2x incomplete) | Minor discrepancies (1x incomplete) | No discrepancy (2x complete) |
| Occlusion (static and dynamic) | Major discrepancies (precontact) | Minor discrepancies (infraocclusion) | No discrepancy |
| Appearance of the crown (margin and color) | Major discrepancies (margin) | Minor discrepancies (color) | No discrepancy |
| Peri-implant soft tissues (quantity and quality) | Non-keratinized, non-adherent | Non-keratinized, adherent | Keratinized, adherent |
| Marginal bone tissue (RX) | Marginal resorption > 1.5 mm | Marginal resorption < 1.5 mm | No marginal resorption |
SATISFACTION VISUAL ANALOG SCALE (VAS) | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 10 | 20 | 30 | 40 | 50 | 60 | 70 | 80 | 90 | 100 | |||||||||||
| Not satisfied | Most satisfied | ||||||||||||||||||||
| # | INTER PROXIMAL | OCCLUSION | DESIGN | MUCOSA | BONE | TOTAL |
|---|---|---|---|---|---|---|
| 1a | 2 | 2 | 2 | 2 | 2 | 10 |
| 1b | 2 | 2 | 2 | 2 | 2 | 10 |
| 2a | 1 | 1 | 2 | 2 | 2 | 8 |
| 2b | 2 | 1 | 2 | 2 | 2 | 9 |
| 3a | 2 | 2 | 2 | 2 | 2 | 10 |
| 3b | 2 | 2 | 1 | 2 | 1 | 8 |
| 4a | 2 | 2 | 2 | 1 | 2 | 9 |
| 4b | 2 | 2 | 2 | 2 | 2 | 10 |
| 5a | 2 | 1 | 2 | 2 | 2 | 9 |
| 5b | 2 | 2 | 2 | 2 | 2 | 10 |
| 6a | 2 | 2 | 2 | 1 | 1 | 8 |
| 6b | 1 | 2 | 2 | 1 | 1 | 7 |
| 7a | 2 | 2 | 2 | 2 | 2 | 10 |
| 7b | 2 | 2 | 2 | 2 | 2 | 10 |
| 8a | 2 | 2 | 1 | 2 | 2 | 9 |
| 8b | 2 | 2 | 2 | 2 | 2 | 10 |
| # | INTER PROXIMAL | OCCLUSION | DESIGN | MUCOSA | BONE | TOTAL |
|---|---|---|---|---|---|---|
| 9 | 2 | 2 | 2 | 2 | 2 | 10 |
| 10 | 1 | 2 | 2 | 2 | 2 | 9 |
| 11 | 2 | 1 | 2 | 2 | 2 | 9 |
| 12 | 2 | 2 | 1 | 2 | 2 | 9 |
| 13 | 2 | 2 | 2 | 2 | 2 | 10 |
| 14 | 2 | 2 | 2 | 0 | 1 | 7 |
| 15 | 2 | 2 | 2 | 2 | 2 | 10 |
| 16 | 2 | 1 | 2 | 1 | 2 | 8 |
| 17 | 2 | 2 | 2 | 2 | 2 | 10 |
| 18 | 2 | 2 | 2 | 2 | 2 | 10 |
| 19 | 2 | 2 | 2 | 2 | 2 | 10 |
| 20 | 2 | 2 | 1 | 2 | 2 | 9 |
| 21 | 2 | 2 | 2 | 2 | 2 | 10 |
| 22 | 2 | 2 | 2 | 2 | 1 | 9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sorrentino, R.; Di Mauro, M.I.; Ruggiero, G.; Leone, R.; Ferrari Cagidiaco, E.; Annunziata, M.; Ferrari, M.; Zarone, F. Implant-Prosthetic Rehabilitation of the Agenesis of Maxillary Lateral Incisors: A 2-Year Prospective Clinical Study with Full Digital Workflow. Prosthesis 2024, 6, 803-816. https://doi.org/10.3390/prosthesis6040057
Sorrentino R, Di Mauro MI, Ruggiero G, Leone R, Ferrari Cagidiaco E, Annunziata M, Ferrari M, Zarone F. Implant-Prosthetic Rehabilitation of the Agenesis of Maxillary Lateral Incisors: A 2-Year Prospective Clinical Study with Full Digital Workflow. Prosthesis. 2024; 6(4):803-816. https://doi.org/10.3390/prosthesis6040057
Chicago/Turabian StyleSorrentino, Roberto, Maria Irene Di Mauro, Gennaro Ruggiero, Renato Leone, Edoardo Ferrari Cagidiaco, Marco Annunziata, Marco Ferrari, and Fernando Zarone. 2024. "Implant-Prosthetic Rehabilitation of the Agenesis of Maxillary Lateral Incisors: A 2-Year Prospective Clinical Study with Full Digital Workflow" Prosthesis 6, no. 4: 803-816. https://doi.org/10.3390/prosthesis6040057
APA StyleSorrentino, R., Di Mauro, M. I., Ruggiero, G., Leone, R., Ferrari Cagidiaco, E., Annunziata, M., Ferrari, M., & Zarone, F. (2024). Implant-Prosthetic Rehabilitation of the Agenesis of Maxillary Lateral Incisors: A 2-Year Prospective Clinical Study with Full Digital Workflow. Prosthesis, 6(4), 803-816. https://doi.org/10.3390/prosthesis6040057










