Patients’ Satisfaction with Mandibular Overdentures Retained Using Mini-Implants: An Up-to-16-Year Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Setting, Participants, and Study Size
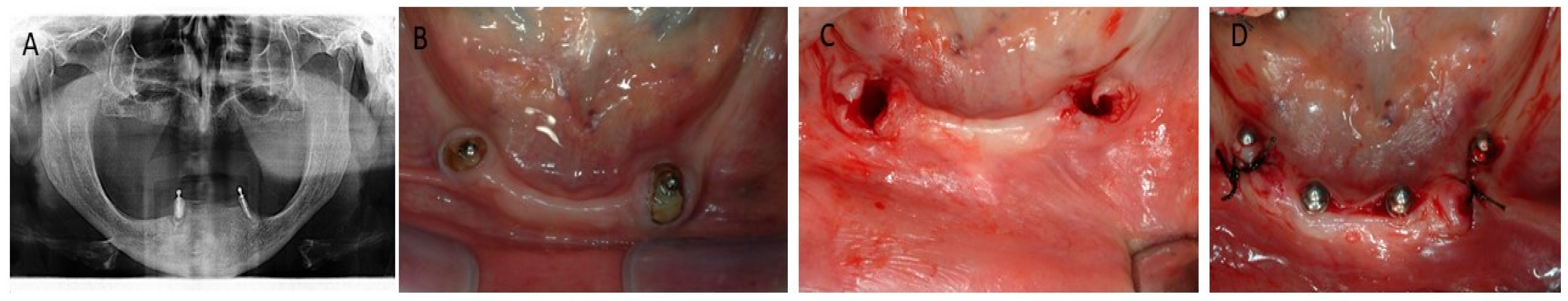
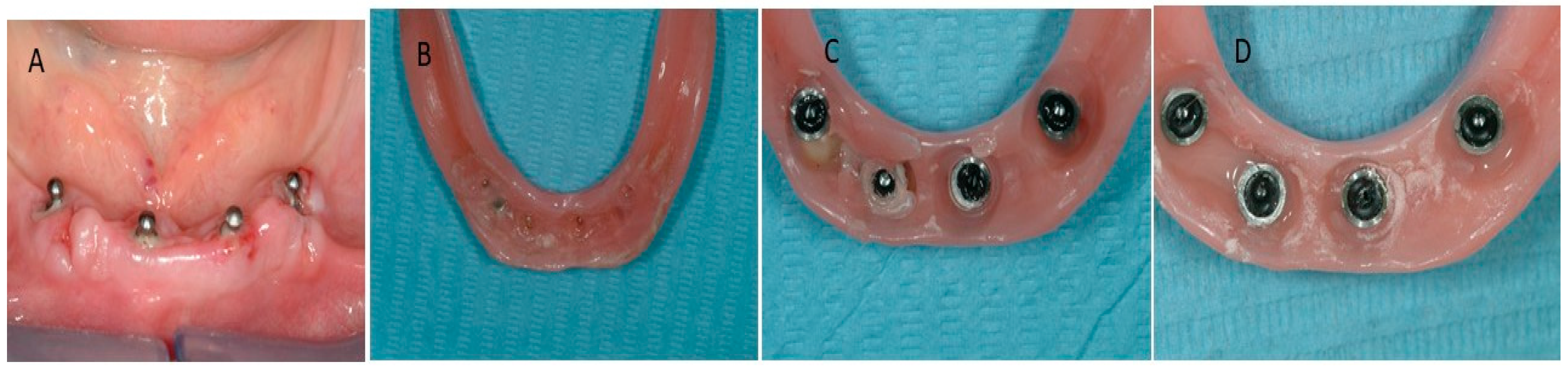
2.3. Surgical Procedure
2.4. Variables
- Patients’ age, gender, and medical histories.
- Mini-implant settings (type, length, diameter, number, location, and attachments type).
- Surgery information (date of implantation, type of anesthesia and drilling, and complications during surgery).
- Post-operative information (data on maintenance sessions, implant loss, and aftercare needs).
2.5. Questionnaire
2.6. Outcomes
2.7. Statistical Analysis
3. Results
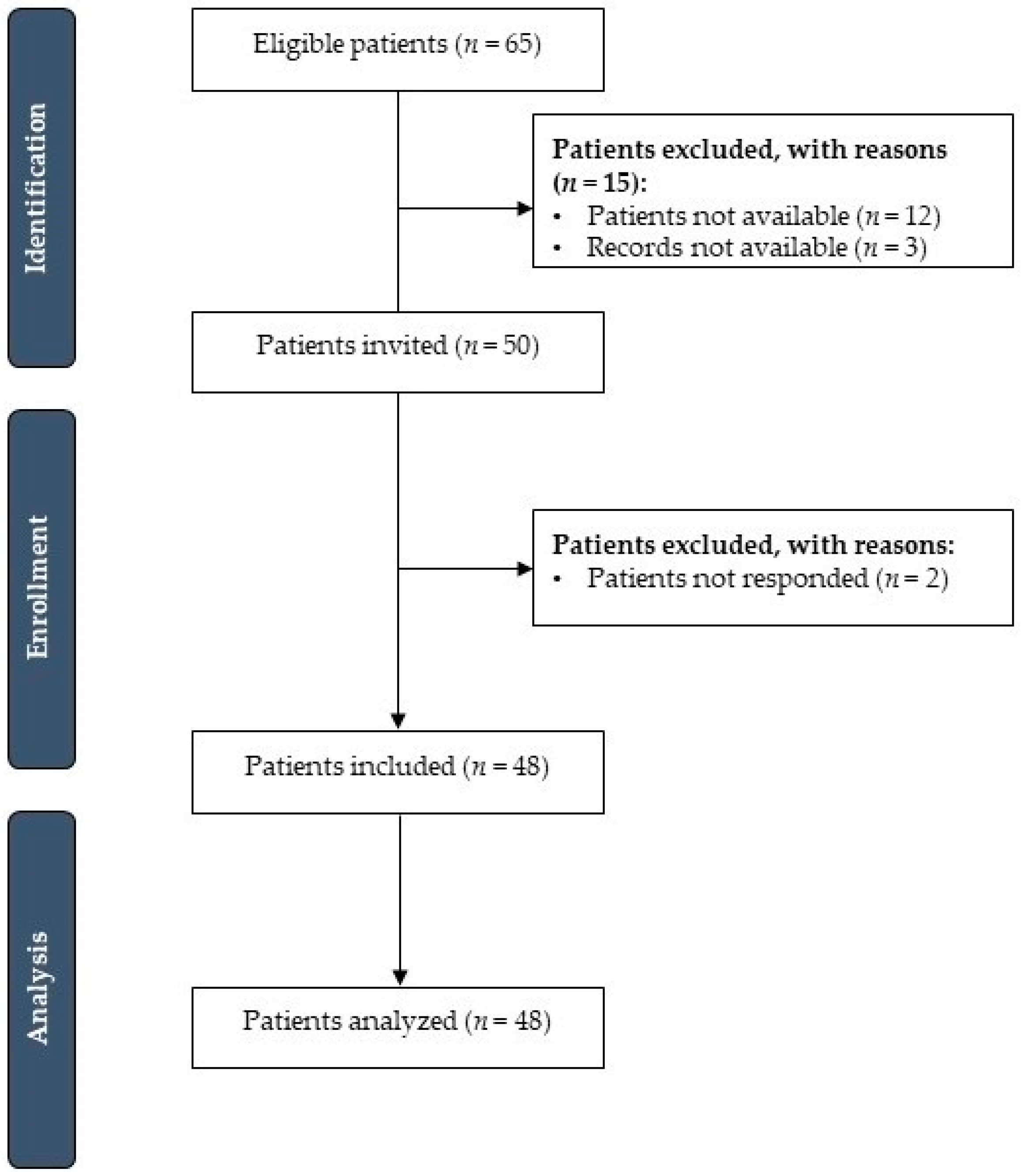
3.1. Participants
3.2. Study Outcomes
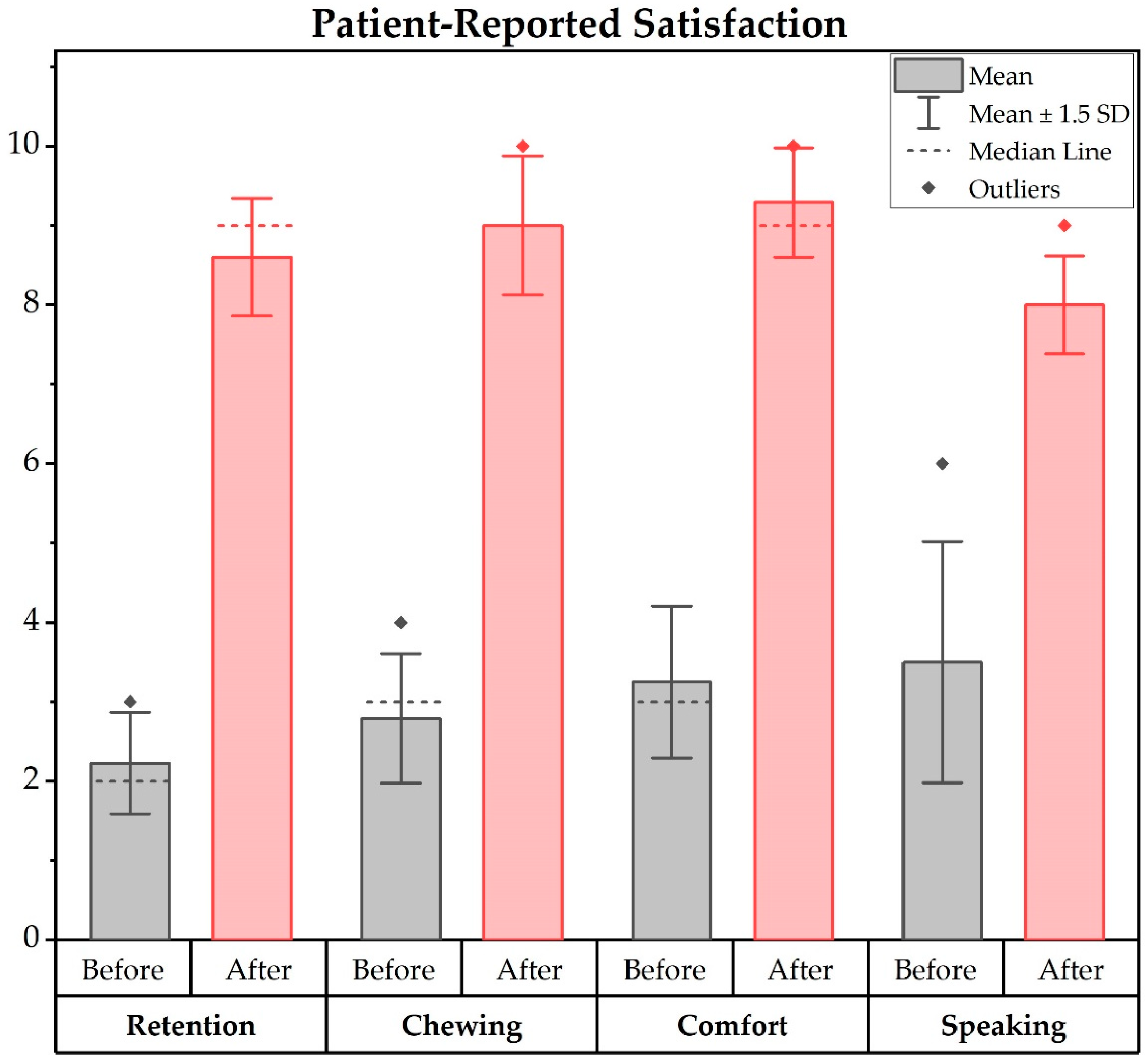
3.2.1. Patient-Reported Satisfaction
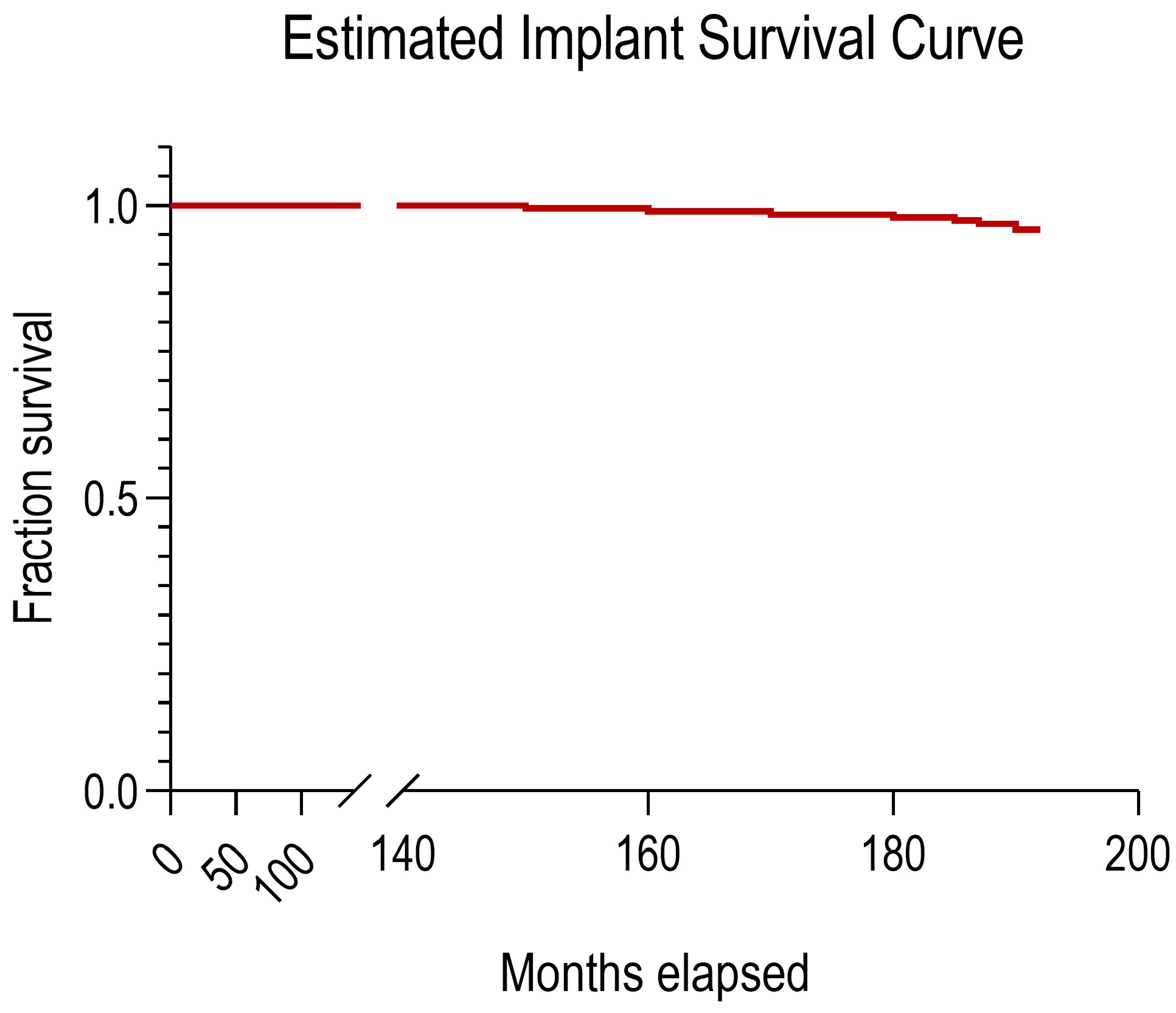
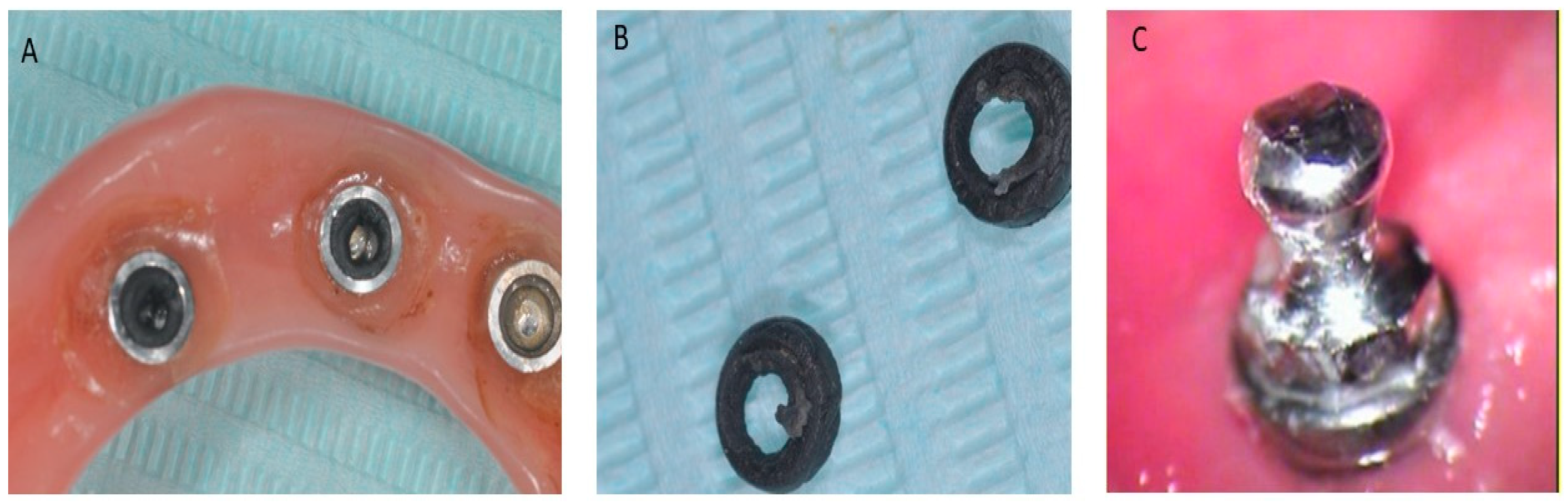
3.2.2. Implant Failure Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Albrektsson, T.; Chrcanovic, B.; Östman, P.-O.; Sennerby, L. Initial and Long-Term Crestal Bone Responses to Modern Dental Implants. Periodontol. 2000 2017, 73, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.-I. A 15-Year Study of Osseointegrated Implants in the Treatment of the Edentulous Jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Froum, S.J.; Cho, S.-C.; Florio, S.; Misch, C.M. Use of Narrow-Diameter Implants in Treatment of Severely Atrophic Maxillary Anterior Region With Implant-Supported Fixed Restorations. Compend. Contin. Educ. Dent. 2016, 37, 334–339. [Google Scholar]
- Greco, G.; Borgia, R.; Casto, C. Occlusal-Vertical Rebalancing for Implantprosthetic Planning: Technical Considerations. Eur. J. Muscoloskel. Dis. 2023, 12, 13–18. [Google Scholar]
- LaBarre, E.E.; Ahlstrom, R.H.; Noble, W.H. Narrow Diameter Implants for Mandibular Denture Retention. J. Calif. Dent. Assoc. 2008, 36, 283–286. [Google Scholar] [CrossRef]
- Kapadia, A.; Wankhade, S.; Khalikar, A.; Deogade, S.; Mukhopadhyay, P.; Dutta, V.; Doibale, P. Comparing the Functional Efficiency of Tooth-Supported Overdentures and Implant-Supported Overdentures in Patients Requiring Oral Rehabilitation: A Systematic Review. Dent. Res. J. 2022, 19, 94. [Google Scholar] [CrossRef]
- Chatrattanarak, W.; Aunmeungtong, W.; Khongkhunthian, P. Comparative Clinical Study of Conventional Dental Implant and Mini Dental Implant-Retained Mandibular Overdenture: A 5- to 8-Year Prospective Clinical Outcomes in a Previous Randomized Clinical Trial. Clin. Implant. Dent. Relat. Res. 2022, 24, 475–487. [Google Scholar] [CrossRef]
- Mangano, F.; Shibli, J.A.; Sammons, R.L.; Veronesi, G.; Piattelli, A.; Mangano, C. Clinical Outcome of Narrow-Diameter (3.3-Mm) Locking-Taper Implants: A Prospective Study with 1 to 10 Years of Follow-up. Int. J. Oral Maxillofac. Implant. 2014, 29, 448–455. [Google Scholar] [CrossRef]
- Abenavoli, F.M.; Inchingolo, A.D.; Inchingolo, A.M.; Dipalma, G.; Inchingolo, F. A Technical Note for the Use of Small-Diameter Cannula for Lipoaspiration Technique in Aesthetic Reconstructive Post-Oncological Surgery. J. Biol. Regul. Homeost. Agents 2019, 33, 1011–1013. [Google Scholar]
- Schiegnitz, E.; Al-Nawas, B. Narrow-Diameter Implants: A Systematic Review and Meta-Analysis. Clin. Oral Implant. Res. 2018, 29 (Suppl. 16), 21–40. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Al-Nawas, B.; Araujo, M.; Avila-Ortiz, G.; Barter, S.; Brodala, N.; Chappuis, V.; Chen, B.; De Souza, A.; Almeida, R.F.; et al. Group 1 ITI Consensus Report: The Influence of Implant Length and Design and Medications on Clinical and Patient-Reported Outcomes. Clin. Oral Implant. Res. 2018, 29 (Suppl. 16), 69–77. [Google Scholar] [CrossRef]
- Agliardi, E.L.; Romeo, D.; Panigatti, S.; de Araújo Nobre, M.; Maló, P. Immediate Full-Arch Rehabilitation of the Severely Atrophic Maxilla Supported by Zygomatic Implants: A Prospective Clinical Study with Minimum Follow-up of 6 Years. Int. J. Oral Maxillofac. Surg. 2017, 46, 1592–1599. [Google Scholar] [CrossRef] [PubMed]
- Cruz, R.S.; Lemos, C.a.A.; de Batista, V.E.S.; Yogui, F.C.; Oliveira, H.F.F.; Verri, F.R. Narrow-Diameter Implants versus Regular-Diameter Implants for Rehabilitation of the Anterior Region: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Surg. 2021, 50, 674–682. [Google Scholar] [CrossRef] [PubMed]
- Scepanovic, M.; Calvo-Guirado, J.L.; Markovic, A.; Delgardo-Ruiz, R.; Todorovic, A.; Milicic, B.; Misic, T. A 1-Year Prospective Cohort Study on Mandibular Overdentures Retained by Mini Dental Implants. Eur. J. Oral Implantol. 2012, 5, 367–379. [Google Scholar] [PubMed]
- Park, J.-H.; Shin, S.-W.; Lee, J.-Y. Mini-Implant Mandibular Overdentures under a Two-Step Immediate Loading Protocol: A 4-6-Year Retrospective Study. Gerodontology 2023, 40, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Bidra, A.S.; Almas, K. Mini Implants for Definitive Prosthodontic Treatment: A Systematic Review. J. Prosthet. Dent. 2013, 109, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Piattelli, A.; Carinci, F. Clinical Outcome of Narrow Diameter Implants: A Retrospective Study of 510 Implants. J. Periodontol. 2008, 79, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E.; Bastardi, D.J.; Moore, R.; Kakar, A.; Herin, Y.; Delgado-Ruiz, R.A. In Vitro Effect of Drilling Speed on the Primary Stability of Narrow Diameter Implants with Varying Thread Designs Placed in Different Qualities of Simulated Bone. Materials 2019, 12, 1350. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Padial-Molina, M.; Nilsson, P.; King, P.; Worsaae, N.; Schramm, A.; Maiorana, C. The Influence of the Distance between Narrow Implants and the Adjacent Teeth on Marginal Bone Levels. Clin. Oral Implant. Res. 2017, 28, 704–712. [Google Scholar] [CrossRef]
- Dolan, T.A.; Atchison, K.A. Implications of Access, Utilization and Need for Oral Health Care by the Non-Institutionalized and Institutionalized Elderly on the Dental Delivery System. J. Dent. Educ. 1993, 57, 876–887. [Google Scholar] [CrossRef]
- Grad, F.P. The Preamble of the Constitution of the World Health Organization. Bull. World Health Organ. 2002, 80, 981–984. [Google Scholar]
- Reisine, S.T. Theoretical Considerations in Formulating Sociodental Indicators. Soc. Sci. Med. A 1981, 15, 745–750. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions. Available online: https://training.cochrane.org/handbook (accessed on 17 September 2023).
- John, M.T. Health Outcomes Reported by Dental Patients. J. Evid. Based Dent. Pract. 2018, 18, 332–335. [Google Scholar] [CrossRef]
- Reissmann, D.R. Dental Patient-Reported Outcome Measures Are Essential for Evidence-Based Prosthetic Dentistry. J. Evid. Based Dent. Pract. 2019, 19, 1–6. [Google Scholar] [CrossRef]
- Rozier, R.G.; Pahel, B.T. Patient- and Population-Reported Outcomes in Public Health Dentistry: Oral Health-Related Quality of Life. Dent. Clin. N. Am. 2008, 52, 345–365. [Google Scholar] [CrossRef]
- John, M.T. Standardization of Dental Patient-Reported Outcomes Measurement Using Ohip-5—Validation of “Recommendations for Use and Scoring of Oral Health Impact Profile Versions”. J. Evid. Based Dent. Pract. 2022, 22, 101645. [Google Scholar] [CrossRef]
- Listl, S. Value-Based Oral Health Care: Moving Forward With Dental Patient-Reported Outcomes. J. Evid. Based Dent. Pract. 2019, 19, 255–259. [Google Scholar] [CrossRef]
- Palaiologou, A.; Kotsakis, G.A. Dentist-Patient Communication of Treatment Outcomes in Periodontal Practice: A Need for Dental Patient-Reported Outcomes. J. Evid. Based Dent. Pract. 2020, 20, 101443. [Google Scholar] [CrossRef]
- Stellrecht, E.; Theis-Mahon, N.R.; Schvaneveldt, N. Role of Librarians and Information Professionals in Identifying Dpros in the Evidence. J. Evid. Based Dent. Pract. 2022, 22, 101649. [Google Scholar] [CrossRef]
- John, M.T.; Sekulić, S.; Bekes, K.; Al-Harthy, M.H.; Michelotti, A.; Reissmann, D.R.; Nikolovska, J.; Sanivarapu, S.; Lawal, F.B.; List, T.; et al. Why Patients Visit Dentists—A Study in All World Health Organization Regions. J. Evid. Based Dent. Pract. 2020, 20, 101459. [Google Scholar] [CrossRef]
- Feine, J.S.; Carlsson, G.E.; Awad, M.A.; Chehade, A.; Duncan, W.J.; Gizani, S.; Head, T.; Heydecke, G.; Lund, J.P.; MacEntee, M.; et al. The McGill Consensus Statement on Overdentures. Mandibular Two-Implant Overdentures as First Choice Standard of Care for Edentulous Patients. Gerodontology 2002, 19, 3–4. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- World Health Organization. Handbook for Good Clinical Research Practice (GCP): Guidance for Implementation; World Health Organization: Geneva, Switzerland, 2005; ISBN 978-92-4-159392-2. [Google Scholar]
- Scarano, A.; Conte, E.; Mastrangelo, F.; Greco Lucchina, A.; Lorusso, F. Narrow Single Tooth Implants for Congenitally Missing Maxillary Lateral Incisors: A 5-Year Follow-up. J. Biol. Regul. Homeost. Agents 2019, 33, 69–76. [Google Scholar]
- Scarano, A.; Murmura, G.; Carinci, F.; Lauritano, D. Immediately Loaded Small-Diameter Dental Implants: Evaluation of Retention, Stability and Comfort for the Edentulous Patient. Eur. J. Inflamm. 2012, 10, 19–23. [Google Scholar]
- Dilek, O.C.; Tezulas, E. Treatment of a Narrow, Single Tooth Edentulous Area with Mini-Dental Implants: A Clinical Report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, e22–e25. [Google Scholar] [CrossRef]
- Flanagan, D. Fixed Partial Dentures and Crowns Supported by Very Small Diameter Dental Implants in Compromised Sites. Implant. Dent. 2008, 17, 182–191. [Google Scholar] [CrossRef]
- Brandt, R.; Hollis, S.; Ahuja, S.; Adatrow, P.; Balanoff, W. Short-Term Objective and Subjective Evaluation of Small-Diameter Implants Used to Support and Retain Mandibular Prosthesis. J. Tenn. Dent. Assoc. 2012, 92, 34–38; quiz 38–39. [Google Scholar]
- Allum, S.R.; Tomlinson, R.A.; Joshi, R. The Impact of Loads on Standard Diameter, Small Diameter and Mini Implants: A Comparative Laboratory Study. Clin. Oral Implant. Res. 2008, 19, 553–559. [Google Scholar] [CrossRef]
- Davarpanah, M.; Martinez, H.; Tecucianu, J.F.; Celletti, R.; Lazzara, R. Small-Diameter Implants: Indications and Contraindications. J. Esthet. Dent. 2000, 12, 186–194. [Google Scholar] [CrossRef]
- Barber, H.D.; Seckinger, R.J. The Role of the Small-Diameter Dental Implant: A Preliminary Report on the Miniplant System. Compendium 1994, 15, 1390, 1392. [Google Scholar]
- Erwood, I. Denture Stabilization with Small-Diameter Implants. Dent. Today 2010, 29, 116–118. [Google Scholar]
- de Sá, B.C.M.; Andrighetto, A.R.; Bernardes, S.R.; Tiossi, R. Fracture Strength of Standard and Small Diameter Prosthetic Abutments for Full-Arch Implant-Supported Restorations. J. Oral Implantol. 2017, 43, 175–179. [Google Scholar] [CrossRef]
- Christensen, G.J. The Increased Use of Small-Diameter Implants. J. Am. Dent. Assoc. 2009, 140, 709–712. [Google Scholar] [CrossRef]
- Teodorescu, C.; Preoteasa, E.; Preoteasa, C.T.; Murariu-Măgureanu, C.; Teodorescu, I.M. The Biomechanical Impact of Loss of an Implant in the Treatment with Mandibular Overdentures on Four Nonsplinted Mini Dental Implants: A Finite Element Analysis. Materials 2022, 15, 8662. [Google Scholar] [CrossRef]
- Comfort, M.B.; Chu, F.C.S.; Chai, J.; Wat, P.Y.P.; Chow, T.W. A 5-Year Prospective Study on Small Diameter Screw-Shaped Oral Implants. J. Oral Rehabil. 2005, 32, 341–345. [Google Scholar] [CrossRef]
- Moris, I.C.M.; Faria, A.C.L.; de Mattos, M. da G.C.; Ribeiro, R.F.; Rodrigues, R.C.S. Mechanical Analysis of Conventional and Small Diameter Conical Implant Abutments. J. Adv. Prosthodont. 2012, 4, 158–161. [Google Scholar] [CrossRef][Green Version]
- Erwood, I. Stabilizing Partial Dentures Using Small-Diameter Implants. Dent. Today 2010, 29, 116, 118–119. [Google Scholar]
| Characteristic | Value |
|---|---|
| Age—(years) | |
| Range | 60–92 |
| Mean (SD) | 69 |
| Sex—no. (%) | |
| Male | 17 (35.4%) |
| Female | 31 (64.6%) |
| Follow-up—(years) | |
| Range | 12–16 |
| Mean (SD) | 15 (2.3) |
| Implant settings | |
| Diameter (mm) | 2.7 |
| Length (mm) | 10–13 |
| Systemic diseases—no. (%) | |
| Severe hypertension | 26 (54.75) |
| Atrial fibrillation | 21 (43.75) |
| Stroke | 4 (8.43) |
| Respiratory failure | 3 (6.25) |
| Chronic kidney disease | 3 (6.25) |
| Hyperthyroidism | 1 (2.08) |
| Liver failure | 2 (4.17) |
| Drug allergies | 1 (2.08) |
| Patient-Reported Satisfaction | Variable | Mean | Std. Err. | Std. Dev. | [95% Con. Interval] | t-Statistic (DF) | p-Value |
|---|---|---|---|---|---|---|---|
| Retention | Before | 2.23 | 0.06 | 0.42 | [2.11, 2.35] | −62.7969 (47) | 0.0000 |
| After | 8.60 | 0.07 | 0.49 | [8.46, 8.75] | |||
| Difference | −6.38 | 0.10 | 0.70 | [−6.58, −6.17] | |||
| Chewing ability | Before | 2.79 | 0.08 | 0.54 | [2.63, 2.95] | −47.8883 (47) | 0.0000 |
| After | 9.00 | 0.08 | 0.58 | [8.83, 9.17] | |||
| Difference | −6.21 | 0.13 | 0.90 | [−6.47, −5.95] | |||
| Comfort | Before | 3.25 | 0.09 | 0.64 | [3.07, 3.43] | −61.2970 (47) | 0.0000 |
| After | 9.29 | 0.07 | 0.46 | [9.16, 9.43] | |||
| Difference | −6.04 | 0.10 | 0.68 | [−6.24, −5.84] | |||
| Speaking ability | Before | 3.50 | 0.15 | 1.01 | [3.21, 3.79] | −29.6401 (47) | 0.0000 |
| After | 8.00 | 0.06 | 0.41 | [7.88, 8.12] | |||
| Difference | −4.50 | 0.15 | 1.05 | [−4.81, −4.19] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarano, A.; Inchingolo, F.; Alla, I.; Lorusso, F.; Tari, S.R.; Gehrke, S.A.; Khater, A.G.A. Patients’ Satisfaction with Mandibular Overdentures Retained Using Mini-Implants: An Up-to-16-Year Cross-Sectional Study. Prosthesis 2024, 6, 251-262. https://doi.org/10.3390/prosthesis6020019
Scarano A, Inchingolo F, Alla I, Lorusso F, Tari SR, Gehrke SA, Khater AGA. Patients’ Satisfaction with Mandibular Overdentures Retained Using Mini-Implants: An Up-to-16-Year Cross-Sectional Study. Prosthesis. 2024; 6(2):251-262. https://doi.org/10.3390/prosthesis6020019
Chicago/Turabian StyleScarano, Antonio, Francesco Inchingolo, Iris Alla, Felice Lorusso, Sergio Rexhep Tari, Sergio Alexandre Gehrke, and Ahmad G. A. Khater. 2024. "Patients’ Satisfaction with Mandibular Overdentures Retained Using Mini-Implants: An Up-to-16-Year Cross-Sectional Study" Prosthesis 6, no. 2: 251-262. https://doi.org/10.3390/prosthesis6020019
APA StyleScarano, A., Inchingolo, F., Alla, I., Lorusso, F., Tari, S. R., Gehrke, S. A., & Khater, A. G. A. (2024). Patients’ Satisfaction with Mandibular Overdentures Retained Using Mini-Implants: An Up-to-16-Year Cross-Sectional Study. Prosthesis, 6(2), 251-262. https://doi.org/10.3390/prosthesis6020019











