Five-Year Follow-Up of 8 and 6 mm Locking-Taper Implants Treated with a Reconstructive Surgical Protocol for Peri-Implantitis: A Retrospective Evaluation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Inclusion Criteria
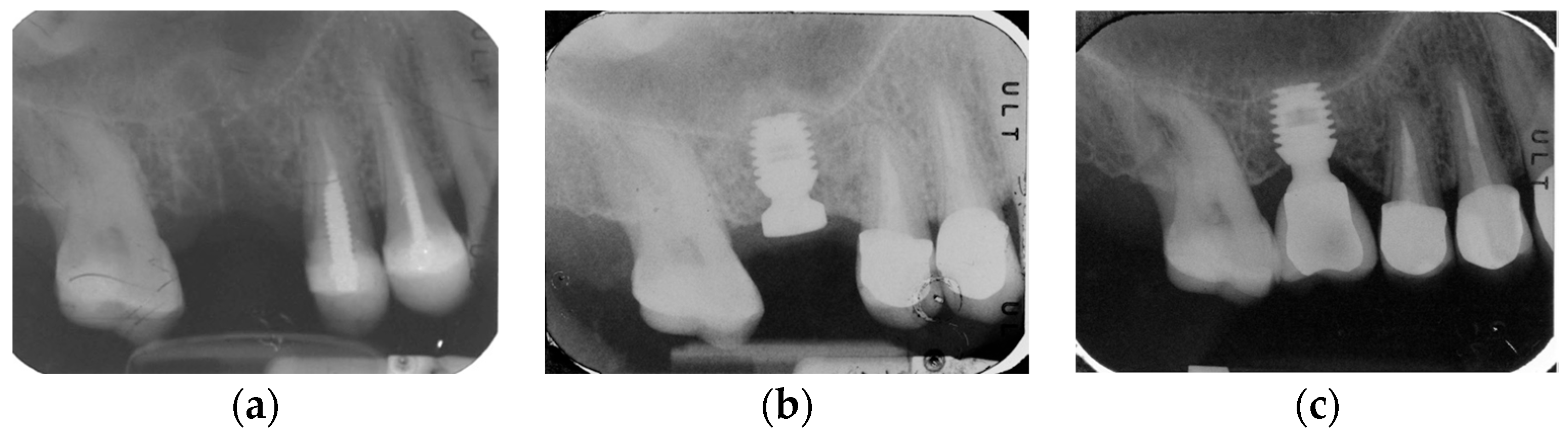
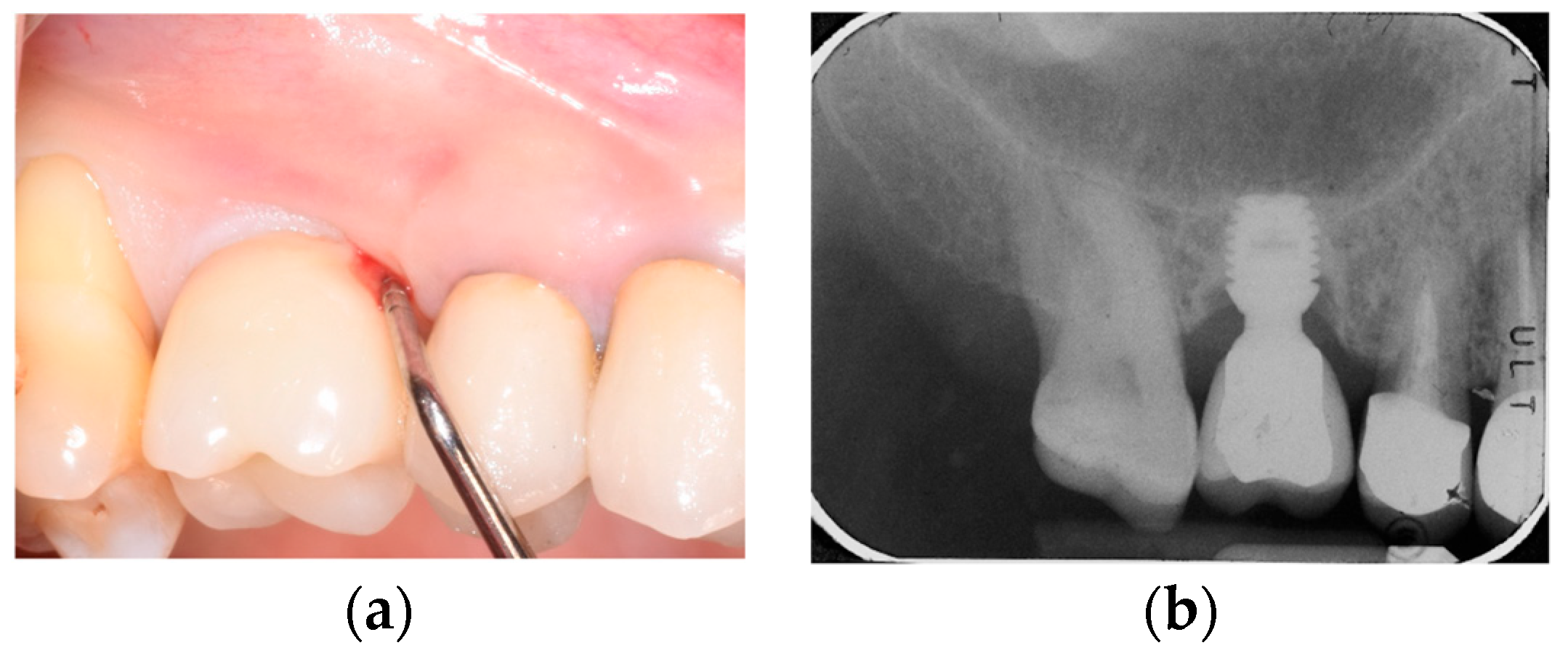
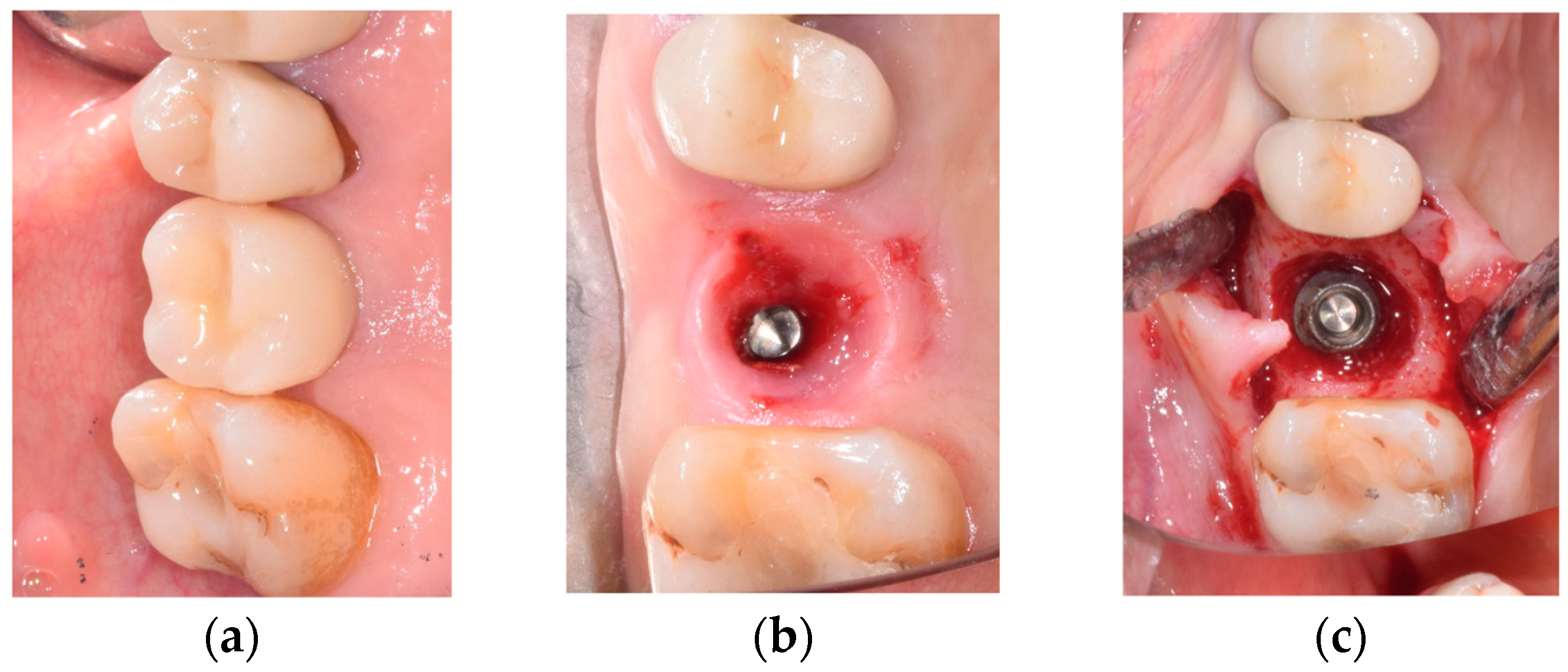
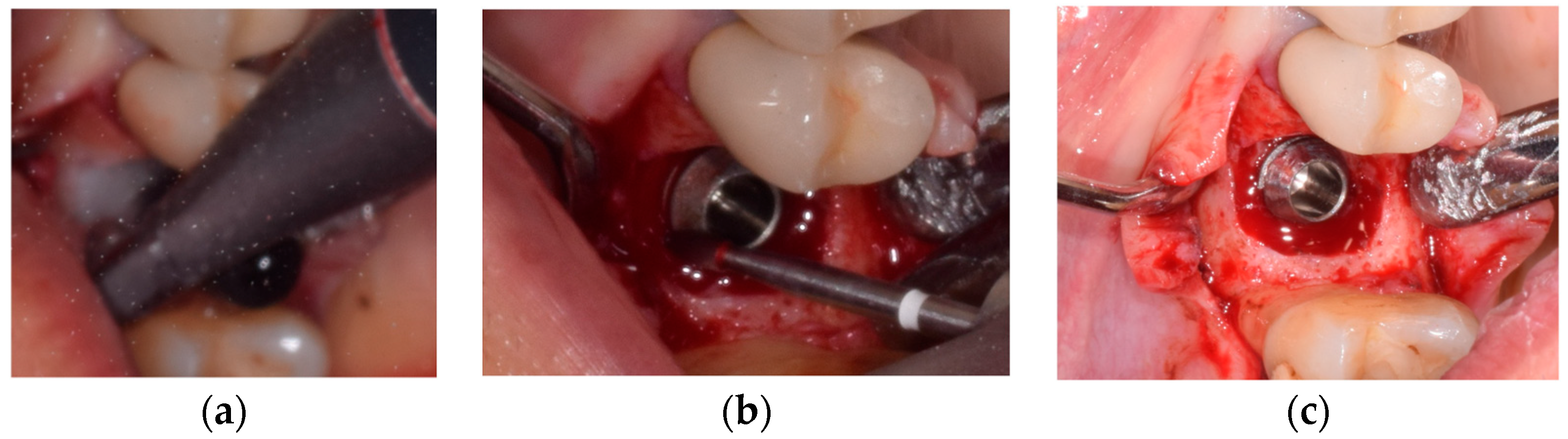
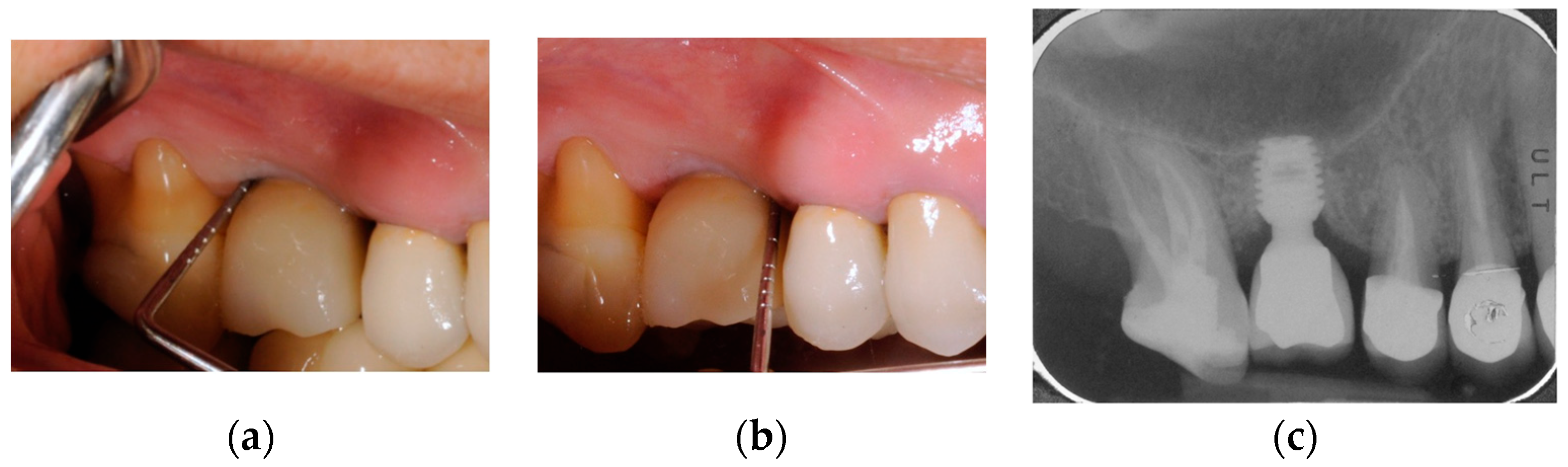
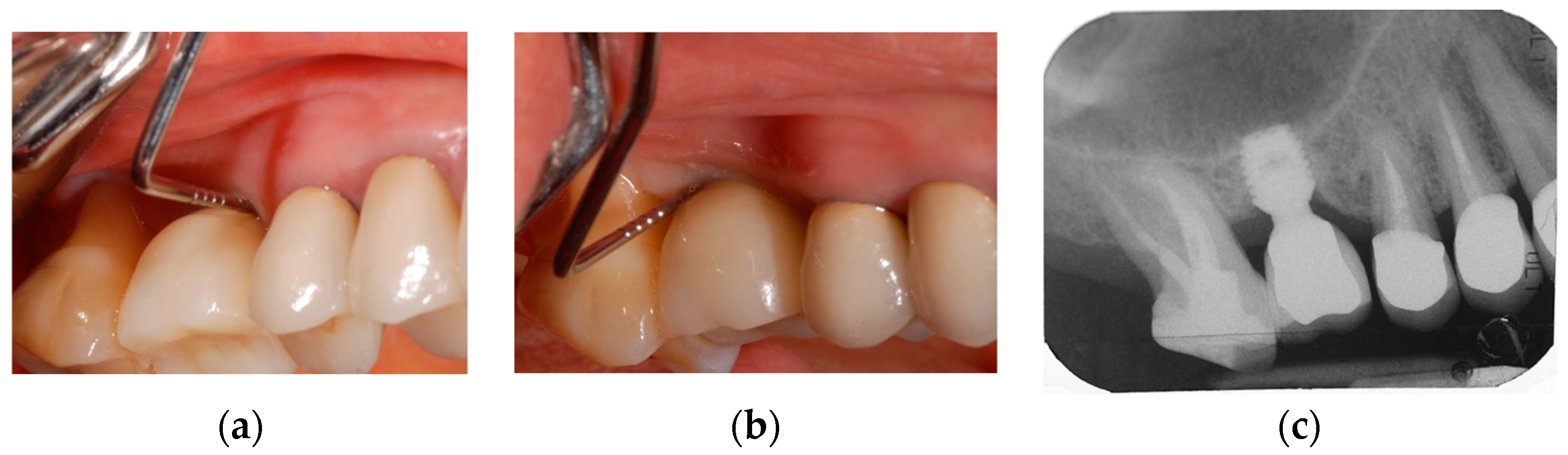
2.2. Surgical Protocol
2.3. Study Variables and Outcomes
2.3.1. Primary Outcome: Treatment Success
2.3.2. Secondary Outcomes: Implant loss
2.3.3. Secondary Outcomes: Clinical and Radiographic Examinations
2.4. Statistical Analysis
3. Results
3.1. Demographics and Implant Loss
3.2. Peri-Implant Bone Levels Variations
3.3. Soft Tissues Conditions
3.4. Treatment Success and Disease Recurrence
4. Discussion
Potential Shortcomings of Peri-Implantitis Diagnosis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| CIR | crown-to-implant ratio |
| PPD | peri-implant probing depth |
| BoP | bleeding on probing |
| Tload | implant loading time |
| Tsurg | time before surgery |
| T3yrs | 3 years after surgery time |
| T5yrs | 5 years after surgery time |
| SUPP | suppuration |
| mBI | Modified Bleeding Index |
| mPLI | Modified Plaque Index |
| KT | keratinized tissue |
| REC | recession of the vestibular mucosal margin |
| CAL | clinical attachment level |
| CBL | crestal bone level |
| F-BIC | first bone-to-implant contact |
| ΔCBL | average bone loss |
| ΔF-BIC | average apical shift of the “first bone-to-implant contact point” position |
| AC | alveolar crest |
| IAI | implant-abutment interface |
| BDD | Bony Defect Depth |
| DEFFILL | Defect Filling |
References
- Chiapasco, M.; Zaniboni, M.; Boisco, M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin. Oral Implants Res. 2006, 17, 136–159. [Google Scholar] [CrossRef]
- Lombardo, G.; Signoriello, A.; Marincola, M.; Liboni, P.; Bonfante, E.A.; Nocini, P.F. Survival rates of ultra-short (<6 mm) compared with short locking-taper implants supporting single crowns in posterior areas: A 5-year retrospective study. Clin. Implant Dent. Relat. Res. 2021, 23, 904–919. [Google Scholar] [CrossRef]
- Jung, R.E.; Al-Nawas, B.; Araujo, M.; Avila-Ortiz, G.; Barter, S.; Brodala, N.; Chappuis, V.; Chen, B.; De Souza, A.; Almeida, R.F.; et al. Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin. Oral Implants Res. 2018, 29, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Renouard, F.; Nisand, D. Impact of implant length and diameter on survival rates. Clin. Oral Implants Res. 2006, 17, 35–51. [Google Scholar] [CrossRef]
- Neugebauer, J.; Nickenig, H.; Zoller, J. Update on short, angulated a diameter-reduced implants. In Proceedings of the 11th European Consensus Conference, European Association of Dental Implantologists, Bonn, Germany, 6 February 2016. [Google Scholar]
- Weng, D.; Jacobson, Z.; Tarnow, D.; Hürzeler, M.B.; Faehn, O.; Sanavi, F.; Barkvoll, P.; Stach, R.M. A prospective multicenter clinical trial of 3i machined-surface implants: Results after 6 years of follow-up. Int. J. Oral Maxillofac. Implants 2003, 18, 417–423. [Google Scholar] [PubMed]
- Tolentino da Rosa de Souza, P.; Binhame Albini Martini, M.; Reis Azevedo-Alanis, L. Do short implants have similar survival rates compared to standard implants in posterior single crown?: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2018, 20, 890–901. [Google Scholar] [CrossRef] [PubMed]
- Ravidà, A.; Wang, I.C.; Barootchi, S.; Askar, H.; Tavelli, L.; Gargallo-Albiol, J.; Wang, H.L. Meta-analysis of randomized clinical trials comparing clinical and patient-reported outcomes between extra-short (≤6 mm) and longer (≥10 mm) implants. J. Clin. Periodontol. 2019, 46, 118–142. [Google Scholar] [CrossRef]
- Naenni, N.; Sahrmann, P.; Schmidlin, P.R.; Attin, T.; Wiedemeier, D.B.; Sapata, V.; Hämmerle, C.H.F.; Jung, R.E. Five-Year Survival of short single-tooth implants (6 mm): A randomized controlled clinical trial. J. Dent. Res. 2018, 97, 887–892. [Google Scholar] [CrossRef]
- Thoma, D.S.; Cha, J.K.; Jung, U.W. Treatment concepts for the posterior maxilla and mandible: Short implants versus long implants in augmented bone. J. Periodontal Implant Sci. 2017, 47, 2–12. [Google Scholar] [CrossRef]
- Nunes, M.; Almeida, R.F.; Felino, A.C.; Malo, P.; de Araújo Nobre, M. The influence of crown-to-implant ratio on short implant marginal bone loss. Int. J. Oral Maxillofac. Implants 2016, 31, 1156–1163. [Google Scholar] [CrossRef]
- Lombardo, G.; Signoriello, A.; Pardo, A.; Serpa Romero, X.Z.; Vila Sierra, L.A.; Arévalo Tovar, L.; Marincola, M.; Nocini, P.F. Short and ultra-short (<6-mm) locking-taper implants supporting single crowns in posterior areas (part II): A 5-year retrospective study on periodontally healthy patients and patients with a history of periodontitis. Clin. Implant Dent. Relat. Res. 2022, 24, 455–467. [Google Scholar] [CrossRef]
- Blanes, R.J. To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin. Oral Implants Res. 2009, 20, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Birdi, H.; Schulte, J.; Kovacs, A.; Weed, M.; Chuang, S.K. Crown-to-implant ratios of short-length implants. J. Oral Implantol. 2010, 36, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Naert, I. Biomechanics/risk management (Working Group 2). Clin. Oral Implants Res. 2009, 20, 107–111. [Google Scholar] [CrossRef]
- Gomez-Polo, M.; Bartens, F.; Sala, L.; Tamini, F.; Celemin, A.; Del Rio, J. The correlation between crown-implant ratios and marginal bone resorption: A preliminary clinical study. Int. J. Prosthodont. 2010, 23, 33–37. [Google Scholar] [PubMed]
- Malchiodi, L.; Caricasulo, R.; Cucchi, A.; Vinci, R.; Agliardi, E.; Gherlone, E. Evaluation of ultrashort and longer implants with microrough surfaces: Results of a 24- to 36-month prospective study. Int. J. Oral Maxillofac. Implants 2017, 32, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Bidez, M.W.; Misch, C.E. Force transfer in implant dentistry: Basic concepts and principles. J. Oral Implantol. 1992, 18, 264–274. [Google Scholar] [PubMed]
- Bidez, M.W.; Misch, C.E. Issues in bone mechanics related to oral implants. Implant Dent. 1992, 1, 289–294. [Google Scholar] [CrossRef]
- Kim, Y.; Oh, T.J.; Misch, C.E.; Wang, H.L. Occlusal considerations in implant therapy: Clinical guidelines with biomechanical rationale. Clin. Oral Implants Res. 2005, 16, 26–35. [Google Scholar] [CrossRef]
- Pellizzer, E.P.; Marcela de Luna Gomes, J.; Araújo Lemos, C.A.; Minatel, L.; de Oliveira Limírio, J.P.; Dantas de Moraes, S.L. The influence of crown-to-implant ratio in single crowns on clinical outcomes: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 126, 497–502. [Google Scholar] [CrossRef]
- Sotto-Maior, B.S.; Senna, P.M.; da Silva, W.J.; Rocha, E.P.; Del Bel Cury, A.A. Influence of crown-to-implant ratio, retention system, restorative material, and occlusal loading on stress concentrations in single short implants. Int. J. Oral Maxillofac. Implants 2012, 27, e13–e18. [Google Scholar]
- Bulaqi, H.A.; Mousavi Mashhadi, M.; Safari, H.; Samandari, M.M.; Geramipanah, F. Effect of increased crown height on stress distribution in short dental implant components and their surrounding bone: A finite element analysis. J. Prosthet. Dent. 2015, 113, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Rokaya, D.; Srimaneepong, V.; Wisitrasameewon, W.; Humagain, M.; Thunyakitpisal, P. Peri-implantitis Update: Risk Indicators, Diagnosis, and Treatment. Eur. J. Dent. 2020, 14, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Rossi, F.; Botticelli, D.; Cesaretti, G.; De Santis, E.; Storelli, S.; Lang, N.P. Use of short implants (6 mm) in a single-tooth replacement: A 5-year follow-up prospective randomized controlled multicenter clinical study. Clin. Oral Implants Res. 2016, 27, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.L.; Lin, G.H.; Suarez, F.; MacEachern, M.; Wang, H.L. Surgical management of peri-implantitis: A systematic review and meta-analysis of treatment outcomes. J. Periodontol. 2014, 85, 1027–1041. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Martins, B.G.; Fernandes, J.C.H.; Martins, A.G.; de Moraes Castilho, R.; de Oliveira Fernandes, G.V. Surgical and Nonsurgical Treatment Protocols for Peri-implantitis: An Overview of Systematic Reviews. Int. J. Oral Maxillofac. Implants 2022, 37, 660–676. [Google Scholar] [CrossRef] [PubMed]
- Daugela, P.; Cicciù, M.; Saulacic, N. Surgical Reconstructive Treatments for Peri-Implantitis: Meta-analysis of Recent Findings in a Systematic Literature Review. J. Oral Maxillofac. Res. 2016, 7, e15. [Google Scholar] [CrossRef] [PubMed]
- Faggion, C.M., Jr.; Chambrone, L.; Listl, S.; Tu, Y.K. Network meta-analysis for evaluating interventions in implant dentistry: The case of peri-implantitis treatment. Clin. Implant Dent. Relat. Res. 2013, 15, 576–588. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.A.; Salvi, G.E.; Mombelli, A.; Loup, P.J.; Heitz, F.; Kruger, E.; Lang, N.P. Supportive peri-implant therapy following anti-infective surgical peri-implantitis treatment: 5-year survival and success. Clin. Oral Implants Res. 2018, 29, 1–6. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Pittoni, D.; Roccuzzo, A.; Charrier, L.; Dalmasso, P. Surgical treatment of peri-implantitis intrabony lesions by means of deproteinized bovine bone mineral with 10% collagen: 7-year-results. Clin. Oral Implants Res. 2017, 28, 1577–1583. [Google Scholar] [CrossRef]
- Berglundh, T.; Wennström, J.L.; Lindhe, J. Long-term outcome of surgical treatment of peri-implantitis. A 2-11-year retrospective study. Clin. Oral Implants Res. 2018, 29, 404–410. [Google Scholar] [CrossRef]
- Andersen, H.; Aass, A.M.; Wohlfahrt, J.C. Porous titanium granules in the treatment of peri-implant osseous defects—A 7-year follow-up study. Int. J. Implant Dent. 2017, 3, 50. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; John, G.; Schmucker, A.; Sahm, N.; Becker, J. Combined surgical therapy of advanced peri-implantitis evaluating two methods of surface decontamination: A 7-year follow-up observation. J. Clin. Periodontol. 2017, 44, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Tomasi, C.; Regidor, E.; Ortiz-Vigón, A.; Derks, J. Efficacy of reconstructive surgical therapy at peri-implantitis-related bone defects. A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 340–356. [Google Scholar] [CrossRef]
- Aljohani, M.; Yong, S.L.; Bin Rahmah, A. The effect of surgical reconstructive treatment for peri-implantitis: A systematic review. Saudi Dent. J. 2020, 32, 109–119. [Google Scholar] [CrossRef]
- Mordini, L.; Sun, N.; Chang, N.; De Guzman, J.P.; Generali, L.; Consolo, U. Peri-Implantitis Regenerative Therapy: A Review. Biology 2021, 10, 773. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Worthington, H.V. Treatment of peri-implantitis: What interventions are effective? A Cochrane systematic review. Eur. J. Oral Implantol. 2012, 5, S21–S41. [Google Scholar] [PubMed]
- Khoury, F.; Keeve, P.L.; Ramanauskaite, A.; Schwarz, F.; Koo, K.T.; Sculean, A.; Romanos, G. Surgical treatment of peri-implantitis—Consensus report of working group 4. Int. Dent. J. 2019, 69, 18–22. [Google Scholar] [CrossRef]
- Lombardo, G.; Marincola, M.; Cicconetti, A.; Simancas-Pallares, M.A.; Pighi, J.; Lehrberg, J.; Signoriello, A.; Corrocher, G.; Serpa, X.; Sierra, L.A.V.; et al. Successful Management of Peri-Implantitis around Short and Ultrashort Single-Crown Implants: A Case Series with a 3-Year Follow-Up. Int. J. Dent. 2019, 2019, 5302752. [Google Scholar] [CrossRef]
- Herrera, D.; Berglundh, T.; Schwarz, F.; Chapple, I.; Jepsen, S.; Sculean, A.; Kebschull, M.; Papapanou, P.N.; Tonetti, M.S.; Sanz, M.; et al. Prevention and treatment of peri-implant diseases-The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2023, 50, 4–76. [Google Scholar] [CrossRef]
- Monje, A.; Pons, R.; Insua, A.; Nart, J.; Wang, H.-L.; Schwarz, F. Morphology and severity of peri-implantitis bone defects. Clin. Implant. Dent. Relat. Res. 2019, 21, 635–643. [Google Scholar] [CrossRef]
- Aghazadeh, A.; Persson, R.G.; Renvert, S. Impact of bone defect morphology on the outcome of reconstructive treatment of peri-implantitis. Int. J. Implant Dent. 2020, 6, 33. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.Y.; Shin, S.I.; Kye, S.B.; Hong, J.; Paeng, J.Y.; Chang, S.W.; Yang, S.M. The Effects of Defect Type and Depth, and Measurement Direction on the Implant Stability Quotient Value. J. Oral Implantol. 2015, 41, 652–656. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Periodontol. 2018, 89, S267–S290. [Google Scholar] [CrossRef] [PubMed]
- Dibart, S.; Warbington, M.; Su, M.F.; Skobe, Z. In vitro evaluation of the implant-abutment bacterial seal: The locking taper system. Int. J. Oral Maxillofac. Implants 2005, 20, 732–737. [Google Scholar]
- Bozkaya, D.; Muftu, S.; Muftu, A. Evaluation of load transfer characteristics of five different implants in compact bone at different load levels by finite elements analysis. J. Prosthet. Dent. 2004, 92, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Coelho, P.G.; Bonfante, E.A.; Marin, C.; Granato, R.; Giro, G.; Suzuki, M. A human retrieval study of plasma-sprayed hydroxyapatite-coated plateau root form implants after 2 months to 13 years in function. J. Long Term Eff. Med. Implants 2010, 20, 335–342. [Google Scholar] [CrossRef]
- Chou, H.Y.; Romanos, G.; Müftü, A.; Müftü, S. Peri-implant bone remodeling around an extraction socket: Predictions of bone maintenance by finite element method. Int. J. Oral Maxillofac. Implants 2012, 27, e39–e48. [Google Scholar]
- Traini, T.; Valentini, P.; Iezzi, G.; Piattelli, A. A histologic and histomorphometric evaluation of anorganic bovine bone retrieved 9 years after a sinus augmentation procedure. J. Periodontol. 2007, 78, 955–961. [Google Scholar] [CrossRef]
- Orsini, G.; Ricci, J.; Scarano, A.; Pecora, G.; Petrone, G.; Iezzi, G.; Piattelli, A. Bone-defect healing with calcium-sulfate particles and cement: An experimental study in rabbit. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 68, 199–208. [Google Scholar] [CrossRef]
- Orsini, G.; Traini, T.; Scarano, A.; Degidi, M.; Perrotti, V.; Piccirilli, M.; Piattelli, A. Maxillary sinus augmentation with Bio-Oss particles: A light, scanning, and transmission electron microscopy study in man. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 74, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Teughels, W.; Van Assche, N.; Sliepen, I.; Quirynen, M. Effect of material characteristics and/or surface topography on biofilm development. Clin. Oral Implants Res. 2006, 17, 68–81. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Signoretto, C.; Corrocher, G.; Pardo, A.; Pighi, J.; Rovera, A.; Caccuri, F.; Nocini, P.F. A topical desiccant agent in association with ultrasonic debridement in the initial treatment of chronic periodontitis: A clinical and microbiological study. New Microbiol. 2015, 38, 393–407. [Google Scholar] [PubMed]
- Isola, G.; Matarese, G.; Williams, R.C.; Siciliano, V.I.; Alibrandi, A.; Cordasco, G.; Ramaglia, L. The effects of a desiccant agent in the treatment of chronic periodontitis: A randomized, controlled clinical trial. Clin. Oral Investig. 2018, 22, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Pini-Prato, G.; Magnani, C.; Rotundo, R. Nonsurgical Treatment of Peri-implantitis Using the Biofilm Decontamination Approach: A Case Report Study. Int. J. Periodontics Restor. Dent. 2016, 36, 383–391. [Google Scholar] [CrossRef][Green Version]
- Tastepe, C.S.; van Waas, R.; Liu, Y.; Wismeijer, D. Air powder abrasive treatment as an implant surface cleaning method: A literature review. Int. J. Oral Maxillofac. Implants 2012, 27, 1461–1473. [Google Scholar] [PubMed]
- Duarte, P.M.; Reis, A.F.; de Freitas, P.M.; Ota-Tsuzuki, C. Bacterial adhesion on smooth and rough titanium surfaces after treatment with different instruments. J. Periodontol. 2009, 80, 1824–1832. [Google Scholar] [CrossRef]
- Khoshkam, V.; Suárez-López Del Amo, F.; Monje, A.; Lin, G.H.; Chan, H.L.; Wang, H.L. Long-term Radiographic and Clinical Outcomes of Reconstructive Approach for Treating Peri-implantitis: A Systematic Review and Meta-analysis. Int. J. Oral Maxillofac. Implants 2016, 31, 1303–1310. [Google Scholar] [CrossRef]
- Renvert, S.; Persson, G.R.; Pirih, F.Q.; Camargo, P.M. Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations. J. Periodontol. 2018, 89, S304–S312. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Layton, D.M.; Roccuzzo, A.; Heitz-Mayfield, L.J. Clinical outcomes of peri-implantitis treatment and supportive care: A systematic review. Clin. Oral Implants Res. 2018, 29, 331–350. [Google Scholar] [CrossRef]
- Matarasso, S.; Iorio Siciliano, V.; Aglietta, M.; Andreuccetti, G.; Salvi, G.E. Clinical and radiographic outcomes of a combined resective and reconstructive approach in the treatment of peri-implantitis: A prospective case series. Clin. Oral Implants Res. 2014, 25, 761–767. [Google Scholar] [CrossRef]
- Wiltfang, J.; Zernial, O.; Behrens, E.; Schlegel, A.; Warnke, P.H.; Becker, S.T. Reconstructive treatment of peri-implantitis bone defects with a combination of autologous bone and a demineralized xenogenic bone graft: A series of 36 defects. Clin. Implant Dent. Relat. Res. 2012, 14, 421–427. [Google Scholar] [CrossRef]
- Caubet, J.; Ramis, J.M.; Ramos-Murguialday, M.; Morey, M.Á.; Monjo, M. Gene expression and morphometric parameters of human bone biopsies after maxillary sinus floor elevation with autologous bone combined with Bio-Oss® or BoneCeramic®. Clin. Oral Implants Res. 2015, 26, 727–735. [Google Scholar] [CrossRef]
- Leventis, M.D.; Fairbairn, P.; Dontas, I.; Faratzis, G.; Valavanis, K.D.; Khaldi, L.; Kostakis, G.; Eleftheriadis, E. Biological response to β-tricalcium phosphate/calcium sulfate synthetic graft material: An experimental study. Implant Dent. 2014, 23, 37–43. [Google Scholar] [CrossRef]
- Stein, J.M.; Fickl, S.; Yekta, S.S.; Hoischen, U.; Ocklenburg, C.; Smeets, R. Clinical evaluation of a biphasic calcium composite grafting material in the treatment of human periodontal intrabony defects: A 12-month randomized controlled clinical trial. J. Periodontol. 2009, 80, 1774–1782. [Google Scholar] [CrossRef]
- Melcher, A.H. On the repair potential of periodontal tissues. J. Periodontol. 1976, 47, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Dimitriou, R.; Mataliotakis, G.I.; Calori, G.M.; Giannoudis, P.V. The role of barrier membranes for guided bone regeneration and restoration of large bone defects: Current experimental and clinical evidence. BMC Med. 2012, 10, 81. [Google Scholar] [CrossRef] [PubMed]
- Meinig, R.P. Clinical use of resorbable polymeric membranes in the treatment of bone defects. Orthop. Clin. N. Am. 2010, 41, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Isler, S.C.; Soysal, F.; Ceyhanlı, T.; Bakırarar, B.; Unsal, B. Efficacy of concentrated growth factor versus collagen membrane in reconstructive surgical therapy of peri-implantitis: 3-year results of a randomized clinical trial. Clin. Oral Investig. 2022, 26, 5247–5260. [Google Scholar] [CrossRef]
- Schwarz, F.; Sahm, N.; Schwarz, K.; Becker, J. Impact of defect configuration on the clinical outcome following surgical reconstructive therapy of peri-implantitis. J. Clin. Periodontol. 2010, 37, 449–455. [Google Scholar] [CrossRef]
- Roos-Jansåker, A.M.; Persson, G.R.; Lindahl, C.; Renvert, S. Surgical treatment of peri-implantitis using a bone substitute with or without a resorbable membrane: A 5-year follow-up. J. Clin. Periodontol. 2014, 41, 1108–1114. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Bieling, K.; Nuesry, E.; Sculean, A.; Becker, J. Clinical and histological healing pattern of peri-implantitis lesions following non-surgical treatment with an Er:YAG laser. Lasers Surg. Med. 2006, 38, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Serino, G.; Turri, A.; Lang, N.P. Maintenance therapy in patients following the surgical treatment of peri-implantitis: A 5-year follow-up study. Clin. Oral Implants Res. 2015, 26, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Polyzois, I.N. Clinical approaches to treat peri-implant mucositis and peri-implantitis. Periodontology 2000 2015, 68, 369–404. [Google Scholar] [CrossRef] [PubMed]
- Heitz-Mayfield, L.J.A.; Heitz, F.; Lang, N.P. Implant Disease Risk Assessment IDRA-a tool for preventing peri-implant disease. Clin. Oral Implants Res. 2020, 31, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, M.; Bonino, F.; Bonino, L.; Dalmasso, P. Surgical therapy of peri-implantitis lesions by means of a bovine-derived xenograft: Comparative results of a prospective study on two different implant surfaces. J. Clin. Periodontol. 2011, 38, 738–745. [Google Scholar] [CrossRef]
- Schwarz, F.; Sahm, N.; Bieling, K.; Becker, J. Surgical reconstructive treatment of peri-implantitis lesions using a nanocrystalline hydroxyapatite or a natural bone mineral in combination with a collagen membrane: A four-year clinical follow-up report. J. Clin. Periodontol. 2009, 36, 807–814. [Google Scholar] [CrossRef]
- Echeverría, J.J.; Echeverría, A.; Caffesse, R.G. Adherence to supportive periodontal treatment. Periodontology 2000 2019, 79, 200–209. [Google Scholar] [CrossRef]
- Amerio, E.; Mainas, G.; Petrova, D.; Giner Tarrida, L.; Nart, J.; Monje, A. Compliance with supportive periodontal/peri-implant therapy: A systematic review. J. Clin. Periodontol. 2020, 47, 81–100. [Google Scholar] [CrossRef]
- Ramanauskaite, A.; Fretwurst, T.; Schwarz, F. Efficacy of alternative or adjunctive measures to conventional non-surgical and surgical treatment of peri-implant mucositis and peri-implantitis: A systematic review and meta-analysis. Int. J. Implant Dent. 2021, 7, 112. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.; Mombelli, A. The therapy of peri-implantitis: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 325–345. [Google Scholar] [CrossRef]
- Jepsen, S.; Berglundh, T.; Genco, R.; Aass, A.M.; Demirel, K.; Derks, J.; Figuero, E.; Giovannoli, J.L.; Goldstein, M.; Lambert, F.; et al. Primary prevention of peri-implantitis: Managing peri-implant mucositis. J. Clin. Periodontol. 2015, 42, S152–S157. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, M.; Grasso, G.; Dalmasso, P. Keratinized mucosa around implants in partially edentulous posterior mandible: 10-year results of a prospective comparative study. Clin. Oral Implants Res. 2016, 27, 491–496. [Google Scholar] [CrossRef]
- Monje, A.; Insua, A.; Wang, H.L. Understanding Peri-Implantitis as a Plaque-Associated and Site-Specific Entity: On the Local Predisposing Factors. J. Clin. Med. 2019, 8, 279. [Google Scholar] [CrossRef] [PubMed]
- Fransson, C.; Tomasi, C.; Pikner, S.S.; Gröndahl, K.; Wennström, J.L.; Leyland, A.H.; Berglundh, T. Severity and pattern of peri-implantitis-associated bone loss. J. Clin. Periodontol. 2010, 37, 442–448. [Google Scholar] [CrossRef]
- Albrektsson, T.; Tengvall, P.; Amengual, L.; Coli, P.; Kotsakis, G.A.; Cochran, D. Osteoimmune regulation underlies oral implant osseointegration and its perturbation. Front. Immunol. 2023, 13, 1056914. [Google Scholar] [CrossRef] [PubMed]
- Menini, M.; Setti, P.; Pera, P.; Pera, F.; Pesce, P. Peri-implant Tissue Health and Bone Resorption in Patients with Immediately Loaded, Implant-Supported, Full-Arch Prostheses. Int. J. Prosthodont. 2018, 31, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Coli, P.; Sennerby, L. Is Peri-Implant Probing Causing Over-Diagnosis and Over-Treatment of Dental Implants? J. Clin. Med. 2019, 8, 1123. [Google Scholar] [CrossRef]
- Jemt, T.; Sundén Pikner, S.; Gröndahl, K. Progression Rate of Progressive Bone Loss in Peri-Implantitis Patients. Clin. Implant Dent. Relat. Res. 2015, 17, 619–628. [Google Scholar] [CrossRef]
- Coli, P.; Jemt, T. Are marginal bone level changes around dental implants due to infection? Clin. Implant Dent. Relat. Res. 2021, 23, 171–178. [Google Scholar] [CrossRef]
- Qian, J.; Wennerberg, A.; Albrektsson, T. Marginal Bone Loss around Oral Implants. Clin. Implant Dent. Relat. Res. 2012, 14, 792–807. [Google Scholar] [CrossRef] [PubMed]



| OVERALL | LENGTH-GROUPS | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 6 mm | 8 mm | Test Statistic | d.f. | p Value | |||||
| VARIABLE | n | % | n | % | n | % | |||
| SEX | |||||||||
| Male | 14 | 66.67 | 8 | 66.67 | 6 | 66.67 | χ2 = 0.001 | 1 | 0.67 |
| Female | 7 | 33.33 | 4 | 33.33 | 3 | 33.33 | |||
| SMOKING | |||||||||
| No | 12 | 57.14 | 7 | 58.33 | 5 | 55.56 | χ2 = 0.01 | 1 | 0.62 |
| Yes | 9 | 42.86 | 5 | 41.67 | 4 | 44.44 | |||
| ASA STATUS | |||||||||
| I | 11 | 52.38 | 7 | 58.33 | 4 | 44.44 | χ2 = 0.39 | 1 | 0.42 |
| II | 10 | 47.62 | 5 | 41.67 | 5 | 55.56 | |||
| PERIO HISTORY | |||||||||
| No | 8 | 38.1 | 5 | 41.67 | 3 | 33.33 | χ2 = 0.15 | 1 | 0.52 |
| Yes | 13 | 61.9 | 7 | 58.33 | 6 | 66.67 | |||
| ARCH | |||||||||
| Maxilla | 12 | 57.14 | 6 | 50 | 6 | 66.67 | χ2 = 0.58 | 1 | 0.37 |
| Mandible | 9 | 42.86 | 6 | 50 | 3 | 33.33 | |||
| TYPE OF TOOTH | |||||||||
| Incisor | 2 | 9.52 | 0 | 0 | 2 | 22.22 | χ2 = 4.40 | 2 | |
| Premolar | 13 | 61.9 | 7 | 58.33 | 6 | 66.67 | 0.12 | ||
| Molar | 6 | 28.57 | 5 | 41.67 | 1 | 11.11 | |||
| IMPLANT DIAMETER | |||||||||
| 3.5 mm | 1 | 4.76 | 0 | 0 | 1 | 11.11 | χ2 = 3.07 | ||
| 4 mm | 8 | 38.1 | 5 | 41.67 | 3 | 33.33 | 3 | ||
| 4.5 mm | 7 | 33.33 | 3 | 25 | 4 | 44.44 | 0.45 | ||
| 5 mm | 5 | 23.81 | 4 | 33.33 | 1 | 11.11 | |||
| CROWN | |||||||||
| Resin | 3 | 14.29 | 2 | 16.67 | 1 | 11.11 | χ2 = 0.12 | 1 | 0.61 |
| Porcelain | 18 | 85.71 | 10 | 83.33 | 8 | 88.89 | |||
| TYPE OF DEFECT | |||||||||
| 1-wall | 3 | 14.29 | 1 | 8.33 | 2 | 22.22 | χ2 = 0.93 | 3 | |
| 2-walls | 7 | 33.33 | 4 | 33.33 | 3 | 33.33 | 0.92 | ||
| 3-walls | 5 | 23.81 | 3 | 25 | 2 | 22.22 | |||
| circumferential | 6 | 28.57 | 4 | 33.33 | 2 | 22.22 | |||
| Variable/ | CBL | F-BIC | BDD | DEFFILL | CIR |
|---|---|---|---|---|---|
| Examination Time | |||||
| Tload | 1.37 | 0.03 | 1.86 | ||
| [0.92; 1.73] | [0.01; 0.06] | [1.04; 2.6] | |||
| Tsurg | 0.66 | 2.49 | 3.16 | 3.57 | |
| [0.19; 1.07] | [1.05; 4.13] | [2.53; 3.78] | [2.05; 7.72] | ||
| test statistic | Z = 0.97 | Z = 0.47 | Z = −4.01 | ||
| p value | 0.0003 | 0.0003 | 0.0003 | ||
| T3yrs | 0.28 | 0.73 | 1.01 | 33.91 | 2.21 |
| [−0.5; 0.85] | [0.1; 2.43] | [0.85; 1.27] | [26.48; 46.77] | [1.47; 3.12] | |
| test statistic | Z = 1.92 | Z = −4.01 | Z = 4.01 | Z = 4.01 | |
| p value | 0.18 | 0.0003 | 0.0002 | 0.0003 | |
| T5yrs | 0.36 | 0.63 | 1.00 | 32.89 | 2.15 |
| [−0.43; 0.96] | [0.05; 2.26] | [0.56; 1.45] | [18.73; 44.1] | [1.43; 3.26] | |
| test statistic | Z = 0.08 | Z = −0.75 | Z = 0.57 | Z = 0.1 | Z = 0.78 |
| p value | 0.93 | 0.45 | 0.56 | 0.12 | 0.43 |
| VARIABLE | LENGTH-GROUPS | |||
|---|---|---|---|---|
| 6 mm | 8 mm | Test Statistic | p Value | |
| BDD Tsurg | 2.92 | 3.49 | Z = −1.35 | 0.17 |
| [2.48; 3.46] | [2.91; 4.13] | |||
| BDD T3yrs | 1.06 | 0.96 | Z = 0.1 | 0.91 |
| [0.87; 1.51] | [0.45; 1.27] | |||
| BDD T5yrs | 1.13 | 0.82 | Z = 1.42 | 0.15 |
| [0.69; 1.52] | [0.35; 1.35] | |||
| DEFFILL T3yrs | 39.85 | 25.98 | Z = 1.35 | 0.17 |
| [25.6; 58.78] | [23.48; 35.97] | |||
| DEFFILL T5yrs | 40.77 | 22.37 | Z = 2.06 | 0.03 |
| [20.04; 55.16] | [15.24; 31.5] | |||
| CIR | ||||
| Tload | 2.13 | 1.49 | Z = 0.99 | 0.31 |
| [1.61; 2.6] | [1.04; 1.8] | |||
| Tsurg | 4.05 | 2.92 | Z = −1.27 | 0.2 |
| [2.66; 7.72] | [2.05; 4.28] | |||
| T3yrs | 2.44 | 1.91 | Z = −0.82 | 0.41 |
| [1.74; 3.12] | [1.47; 2.67] | |||
| T5yrs | 2.36 | 1.87 | Z = −1.49 | 0.13 |
| [1.7; 3.26] | [1.43; 2.38] | |||
| VARIABLE | DEFECT TYPE-GROUPS | ||||||
|---|---|---|---|---|---|---|---|
| 1-Wall | 2-Walls | 3-Walls | Circumferential | Test Statistic | d.f. | p Value | |
| BDD Tsurg | 2.27 | 2.98 | 3.40 | 3.62 | χ2 = 4.49 | 3 | 0.21 |
| [1.48; 2.91] | [2.03; 4.03] | [2.56; 3.78] | [3.22; 3.95] | ||||
| BDD T3yrs | 1.19 | 0.62 | 1.22 | 1.22 | χ2 = 2.99 | 3 | 0.39 |
| [0.45; 1.97] | [0.04; 1.08] | [0.85; 2.03] | [0.9; 1.61] | ||||
| BDD T5yrs | 1.06 | 0.52 | 1.46 | 1.13 | χ2 = 8.49 | 3 | 0.07 |
| [0.3; 1.54] | [0.35; 0.82] | [1.02; 1.75] | [0.74; 1.45] | ||||
| DEFFILL T3yrs | 50.65 | 23.15 | 37.86 | 34.79 | χ2 = 2.95 | 3 | 0.39 |
| [30.4; 81.23] | [10.96; 39.02] | [33.2; 48.71] | [24.29; 46.77] | ||||
| DEFFILL T5yrs | 43.36 | 18.95 | 46.79 | 32.33 | χ2 = 5.67 | 3 | 0.12 |
| [20.27; 63.5] | [8.46; 27.35] | [33.3; 69.23] | [18.73; 42.54] | ||||
| CIR | |||||||
| Tload | 2.15 | 2.13 | 1.52 | 1.43 | χ2 = 5.87 | 3 | 0.92 |
| [1.79; 1.64] | [1.63; 2.05] | [0.98; 1.82] | [1.37; 2.14] | ||||
| Tsurg | 4.02 | 4.03 | 3.75 | 3.07 | χ2 = 4.21 | 3 | 0.75 |
| [3.91; 5.07] | [3.57; 4.98] | [3.26; 4.62] | [2.75; 3.93] | ||||
| T3yrs | 2.47 | 2.06 | 2.38 | 2.09 | χ2 = 3.92 | 3 | 0.28 |
| [1.98; 3.25] | [1.84; 3.24] | [2.04; 3.51] | [1.89; 2.52] | ||||
| T5yrs | 2.25 | 2.02 | 2.16 | 1.98 | χ2 = 2.56 | 3 | 0.18 |
| [2.17; 2.99] | [1.96; 3.01] | [2.08; 3.2] | [0.94; 1.66] | ||||
| VARIABLE | Tsurg | T3yrs | Test Statistic | p Value | T5yrs | Test Statistic | p Value |
|---|---|---|---|---|---|---|---|
| PPD | 8.14 | 3.66 | Z = 4.03 | 0.0003 | 3.71 | Z = −0.72 | 0.46 |
| [7; 9] | [3; 4] | [3; 5] | |||||
| mBI | 2.47 | 0.23 | Z = 4.07 | 0.0003 | 0.33 | Z = −0.94 | 0.34 |
| [2; 3] | [0; 1] | [0; 1] | |||||
| mPLI | 1.85 | 0.47 | Z = 3.97 | 0.0003 | 0.46 | Z = −0.51 | 0.6 |
| [1; 2] | [0; 1] | [0; 1] | |||||
| REC | 0.09 | 1.04 | Z = −3.76 | 0.0006 | 1.14 | Z = −1.41 | 0.45 |
| [0; 1] | [1; 2] | [1; 2] | |||||
| KT | 3.19 | 2.47 | Z = 3.71 | 0.0006 | 2.38 | Z = 1.41 | 0.45 |
| [3; 4] | [2; 3] | [2; 3] | |||||
| CAL | 8.23 | 4.70 | Z = 4.02 | 0.0003 | 4.85 | Z = 0.93 | 0.79 |
| [7; 9] | [2; 5] | [2; 5] |
| VARIABLE | LENGTH GROUPS | |||
|---|---|---|---|---|
| 6 mm | 8 mm | Test Statistic | p Value | |
| PPD | ||||
| Tsurg | 7.83 [7; 9] | 8.55 [7; 9] | ||
| T3yrs | 3.41 [3; 4] | 4 [3; 4] | ||
| T5yrs | 3.41 [3; 5] | 4.11 [3; 5] | ||
| Δ Tsurg-T5yrs | 4.41 [4; 5] | 4.44 [4; 5] | Z = −0.28 | 0.97 |
| mBI | ||||
| Tsurg | 2.50 [2; 3] | 2.44 [2; 3] | ||
| T3yrs | 0.16 [0; 1] | 0.33 [0; 1] | ||
| T5yrs | 0.25 [0; 1] | 0.44 [0; 1] | ||
| Δ Tsurg-T5yrs | 2.25 [2; 3] | 2.00 [2; 3] | Z = −0.56 | 0.3 |
| mPLI | ||||
| Tsurg | 1.75 [1; 2] | 2.00 [1; 2] | ||
| T3yrs | 0.50 [0; 1] | 0.44 [0; 1] | ||
| T5yrs | 0.41 [0; 1] | 0.55 [0; 1] | ||
| Δ Tsurg-T5yrs | 1.33 [1; 2] | 1.44 [1; 2] | Z = −1.05 | 0.84 |
| REC | ||||
| Tsurg | 0.16 [0; 1] | 0.01 [0; 1] | ||
| T3yrs | 1.16 [1; 2] | 0.88 [1; 2] | ||
| T5yrs | 1.25 [1; 2] | 1.00 [1; 2] | ||
| Δ Tsurg-T5yrs | (−)1.08 [1; 2] | (−)1.00 [1; 2] | Z = −0.36 | 0.65 |
| KT | ||||
| Tsurg | 3.08 [3; 4] | 3.33 [3; 4] | ||
| T3yrs | 2.25 [2; 3] | 2.77 [2; 3] | ||
| T5yrs | 2.16 [2; 3] | 2.66 [2; 3] | ||
| Δ Tsurg-T5yrs | 0.91 [0; 1] | 0.66 [0; 1] | Z = −1.82 | 0.28 |
| CAL | ||||
| Tsurg | 8.47 [7; 9] | 8.15 [7; 9] | ||
| T3yrs | 4.56 [2; 5] | 4.77 [2; 5] | ||
| T5yrs | 4.74 [2; 5] | 4.86 [2; 5] | ||
| Δ Tsurg-T5yrs | 3.73 [2; 5] | 3.29 [2; 5] | Z = −0.92 | 0.97 |
| Disease Recurrence | Treatment Success | ||||||
|---|---|---|---|---|---|---|---|
| VARIABLE | n | % | n | % | Test Statistic | d.f. | p Value |
| SEX | |||||||
| Male | 2 | 14.29 | 12 | 87.51 | χ2 = 0.61 | 1 | 0.4 |
| Female | 2 | 28.57 | 5 | 71.43 | |||
| SMOKING | |||||||
| No | 3 | 25 | 9 | 75 | χ2 = 0.64 | 1 | 0.41 |
| Yes | 1 | 11.11 | 8 | 88.89 | |||
| ASA STATUS | |||||||
| I | 2 | 18.18 | 9 | 81.82 | χ2 = 0.01 | 1 | 0.66 |
| II | 2 | 20 | 8 | 80 | |||
| PERIO HISTORY | |||||||
| No | 1 | 12.5 | 7 | 87.5 | χ2 = 0.35 | 1 | 0.5 |
| Yes | 3 | 23.08 | 10 | 76.92 | |||
| ARCH | |||||||
| Maxilla | 2 | 16.67 | 10 | 83.33 | χ2 = 0.1 | 1 | 0.58 |
| Mandible | 2 | 22.22 | 7 | 77.78 | |||
| TYPE OF TOOTH | |||||||
| Incisor | 0 | 0 | 2 | 100 | |||
| Premolar | 2 | 15.38 | 11 | 84.62 | χ2 = 1.37 | 2 | 0.71 |
| Molar | 2 | 33.33 | 4 | 66.67 | |||
| IMPLANT LENGTH | |||||||
| 6 mm | 1 | 8.33 | 11 | 91.67 | χ2 = 2.08 | 1 | 0.18 |
| 8 mm | 3 | 33.33 | 6 | 66.67 | |||
| IMPLANT DIAMETER | |||||||
| 3.5 mm | 0 | 0 | 1 | 100 | |||
| 4 mm | 1 | 12.5 | 7 | 87.5 | χ2 = 0.87 | 3 | 0.83 |
| 4.5 mm | 2 | 28.57 | 5 | 71.43 | |||
| 5 mm | 1 | 20 | 4 | 80 | |||
| CROWN | |||||||
| Resin | 0 | 0 | 3 | 100 | χ2 = 0.82 | 1 | 0.51 |
| Porcelain | 4 | 22.22 | 14 | 77.78 | |||
| CIR | |||||||
| <2 | 3 | 27.27 | 8 | 72.73 | χ2 = 1.01 | 1 | 0.33 |
| >2 | 1 | 10 | 9 | 90 | |||
| TYPE OF DEFECT | |||||||
| 1-wall | 1 | 33.33 | 2 | 66.67 | |||
| 2-walls | 3 | 42.86 | 4 | 57.14 | χ2 = 5.55 | 3 | 0.13 |
| 3-walls | 0 | 0 | 5 | 100 | |||
| circumferential | 0 | 0 | 6 | 100 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lombardo, G.; Signoriello, A.; Marincola, M.; Bonfante, E.A.; Díaz-Caballero, A.; Tomizioli, N.; Pardo, A.; Zangani, A. Five-Year Follow-Up of 8 and 6 mm Locking-Taper Implants Treated with a Reconstructive Surgical Protocol for Peri-Implantitis: A Retrospective Evaluation. Prosthesis 2023, 5, 1322-1342. https://doi.org/10.3390/prosthesis5040091
Lombardo G, Signoriello A, Marincola M, Bonfante EA, Díaz-Caballero A, Tomizioli N, Pardo A, Zangani A. Five-Year Follow-Up of 8 and 6 mm Locking-Taper Implants Treated with a Reconstructive Surgical Protocol for Peri-Implantitis: A Retrospective Evaluation. Prosthesis. 2023; 5(4):1322-1342. https://doi.org/10.3390/prosthesis5040091
Chicago/Turabian StyleLombardo, Giorgio, Annarita Signoriello, Mauro Marincola, Estevam Augusto Bonfante, Antonio Díaz-Caballero, Nicolò Tomizioli, Alessia Pardo, and Alessandro Zangani. 2023. "Five-Year Follow-Up of 8 and 6 mm Locking-Taper Implants Treated with a Reconstructive Surgical Protocol for Peri-Implantitis: A Retrospective Evaluation" Prosthesis 5, no. 4: 1322-1342. https://doi.org/10.3390/prosthesis5040091
APA StyleLombardo, G., Signoriello, A., Marincola, M., Bonfante, E. A., Díaz-Caballero, A., Tomizioli, N., Pardo, A., & Zangani, A. (2023). Five-Year Follow-Up of 8 and 6 mm Locking-Taper Implants Treated with a Reconstructive Surgical Protocol for Peri-Implantitis: A Retrospective Evaluation. Prosthesis, 5(4), 1322-1342. https://doi.org/10.3390/prosthesis5040091






