Narrow Implants and Overdentures in the Total Rehabilitation of Atrophic Edentulous Jaws: Review of Clinical Aspects with Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Exclusion Criteria and Outcome Measures
2.3. Search Strategy, Selection Criteria, and Data Extraction
3. Results
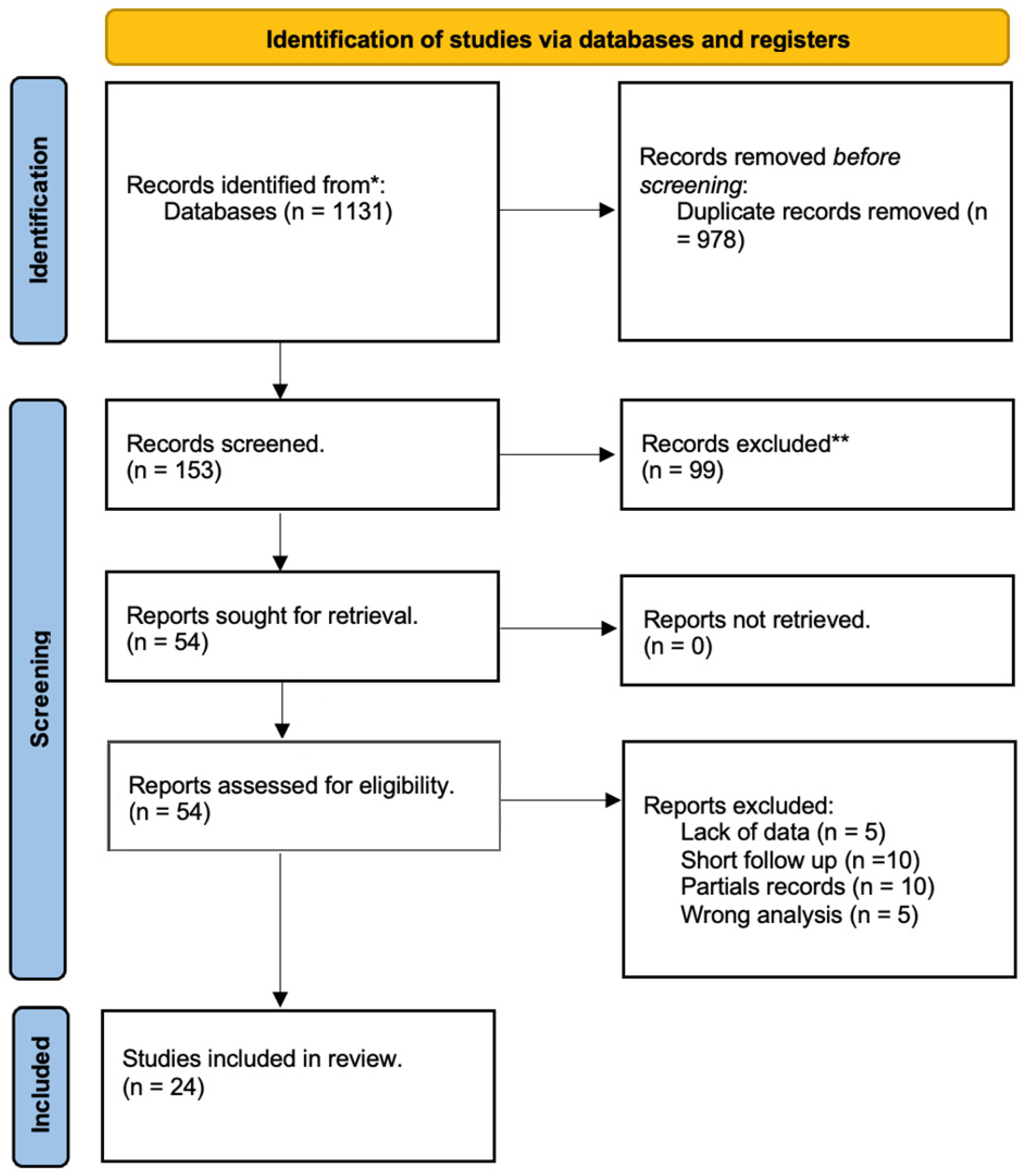
3.1. Identified Articles
3.2. Included Studies and Outcomes
3.3. Biological Complications
3.4. Meta-Analysis
3.5. Quality Assessment and Risk of Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Tallgren, A. The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years. J. Prosthet. Dent. 2003, 89, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Klein, M.O.; Schiegnitz, E.; Al-Nawas, B. Systematic Review on Success of Narrow-Diameter Dental Implants. Int. J. Oral Maxillofac. Implant. 2014, 29, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Juodzbalys, G.; Kubilius, M. Clinical and Radiological Classification of the Jawbone Anatomy in Endosseous Dental Implant Treatment. J. Oral Maxillofac. Res. 2013, 4, e2. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Oller, I.; Suárez, F.; Galindo-Moreno, P.; Torrecillas-Martínez, L.; Monje, A.; Catena, A.; Wang, H. The Influence of Implant Diameter on Its Survival: A Meta-Analysis Based on Prospective Clinical Trials. J. Periodontol. 2014, 85, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Al-Nawas, B.; Araujo, M.; Avila-Ortiz, G.; Barter, S.; Brodala, N.; Chappuis, V.; Chen, B.; De Souza, A.; Almeida, R.F.; et al. Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin. Oral Implant. Res. 2018, 29, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Schiegnitz, E.; Al-Nawas, B. Narrow-diameter implants: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 21–40. [Google Scholar] [CrossRef]
- Faot, F.; Petiz, H.C.F.C.; Bielemann, A.M.; Possebon, A.P.d.R.; Boscato, N.; Chagas-Júnior, O.L.; Pinto, L.d.R. Functional performance and impact on the quality of life of three treatment strategies for mandibular edentulism: Results of a parallel 3-group cross-sectional study. J. Dent. 2023, 136, 104625. [Google Scholar] [CrossRef]
- Ahn, M.-R.; An, K.-M.; Choi, J.-H.; Sohn, D.-S. Immediate Loading With Mini Dental Implants in the Fully Edentulous Mandible. Implant. Dent. 2004, 13, 367–372. [Google Scholar] [CrossRef]
- Scarano, A.; Conte, E.; Mastrangelo, F.; Lorusso, F. Narrow single tooth implants for congenitally missing maxillary lateral incisors: A 5-year follow-up. J. Biol. Regul. Homeost. Agents 2019, 33 (Suppl. S2), 69–76. [Google Scholar]
- Giannakopoulos, N.N.; Ariaans, K.; Eberhard, L.; Klotz, A.; Oh, K.; Kappel, S. Immediate and delayed loading of two-piece reduced-diameter implants with locator-analog attachments in edentulous mandibles: One-year results from a randomized clinical trial examining clinical outcome and patient expectation. Clin. Implant. Dent. Relat. Res. 2017, 19, 643–653. [Google Scholar] [CrossRef]
- dos Reis, T.A.; Zancopé, K.; Karam, F.K.; das Neves, F.D. Biomechanical behavior of extra-narrow implants after fatigue and pull-out tests. J. Prosthet. Dent. 2019, 122, 54.e1–54.e6. [Google Scholar] [CrossRef]
- Payne, A.G.T.; Tawse-Smith, A.A.; Thomson, W.M.W.M.; Duncan, W.D.W.D.; Kumara, R.R. One-Stage Surgery and Early Loading of Three Implants for Maxillary Overdentures: A 1-Year Report. Clin. Implant. Dent. Relat. Res. 2004, 6, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Tymstra, N.; Raghoebar, G.M.; Vissink, A.; Meijer, H.J.A. Dental implant treatment for two adjacent missing teeth in the maxillary aesthetic zone: A comparative pilot study and test of principle. Clin. Oral Implant. Res. 2010, 22, 207–213. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schuster, A.J.; Possebon, A.P.d.R.; Bielemann, A.M.; Chagas-Júnior, O.L.; Faot, F. Effect of mandibular residual ridge regularization on peri-implant wound healing when narrow diameter implants are used as overdenture retainers. J. Prosthet. Dent. 2021, 128, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Shin, S.-W.; Leea, J.-Y. Two-Step Immediate Loading of Mandibular Overdentures Retained by Mini-implants: A Prospective Clinical Study. Int. J. Prosthodont. 2018, 31, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Waddell, J.; Atieh, M.; Alsabeeha, N.; Payne, A. Maxillary Three-Implant Overdentures Opposing Mandibular Two-Implant Overdentures: 10-Year Prosthodontic Outcomes. Int. J. Prosthodont. 2016, 29, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Possebon, A.P.d.R.; Schuster, A.J.; Chagas-Júnior, O.L.; Pinto, L.d.R.; Faot, F. Immediate versus conventional loading of mandibular implant-retained overdentures: A 3-year follow-up of a randomized controlled trial. Clin. Oral Investig. 2023, 27, 5935–5946. [Google Scholar] [CrossRef]
- Marcello-Machado, R.M.; Faot, F.; Schuster, A.J.; Bielemann, A.M.; Júnior, O.L.C.; Cury, A.A.D.B. One-year clinical outcomes of locking taper Equator attachments retaining mandibular overdentures to narrow diameter implants. Clin. Implant. Dent. Relat. Res. 2018, 20, 483–492. [Google Scholar] [CrossRef]
- Bielemann, A.M.; Schuster, A.J.; Possebon, A.P.d.R.; Schinestsck, A.R.; Chagas-Junior, O.L.; Faot, F. Clinical performance of narrow-diameter implants with hydrophobic and hydrophilic surfaces with mandibular implant overdentures: 1-year results of a randomized clinical trial. Clin. Oral Implant. Res. 2021, 33, 21–32. [Google Scholar] [CrossRef]
- Mundt, T.; Schwahn, C.; Biffar, R.; Heinemann, F. Changes in Bone Levels Around Mini-Implants in Edentulous Arches. Int. J. Oral Maxillofac. Implant. 2015, 30, 1149–1155. [Google Scholar] [CrossRef]
- Catalán, A.; Martínez, A.; Marchesani, F.; González, U. Mandibular Overdentures Retained by Two Mini-Implants: A Seven-Year Retention and Satisfaction Study. J. Prosthodont. 2016, 25, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Preoteasa, E.; Marin, M.; Imre, M.; Lerner, H.; Preoteasa, C.T. Patients’ satisfaction with conventional dentures and mini implant anchored overdentures. Rev. Med. Chir. Soc. Med. Nat. Iasi 2012, 116, 310–316. [Google Scholar] [PubMed]
- Jofré, J.; Conrady, Y.; Carrasco, C. Survival of splinted mini-implants after contamination with stainless steel. Int. J. Oral Maxillofac. Implant. 2010, 25, 351–356. [Google Scholar]
- Stanford, C.; Barwacz, C.; Raes, S.; De Bruyn, H.; Cecchinato, D.; Bittner, N.; Brandt, J. Multicenter Clinical Randomized Controlled Trial Evaluation of an Implant System Designed for Enhanced Primary Stability. Int. J. Oral Maxillofac. Implant. 2016, 31, 906–915. [Google Scholar] [CrossRef] [PubMed]
- Maryod, W.; Ali, S.; Shawky, A. Technical Complications and Failures of Zirconia-Based Prostheses Supported by Implants Followed Up to 7 Years: A Case Series. Int. J. Prosthodont. 2014, 27, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Shibli, J.A.; Sammons, R.L.; Veronesi, G.; Piattelli, A.; Mangano, C. Clinical Outcome of Narrow-Diameter (3.3-mm) Locking-Taper Implants: A Prospective Study with 1 to 10 Years of Follow-up. Int. J. Oral Maxillofac. Implant. 2014, 29, 448–455. [Google Scholar] [CrossRef]
- de Souza, R.; Ribeiro, A.; Della Vecchia, M.; Costa, L.; Cunha, T.; Reis, A.; Albuquerque, R. Mini vs. Standard Implants for Mandibular Overdentures: A Randomized Trial. J. Dent. Res. 2015, 94, 1376–1384. [Google Scholar] [CrossRef]
- Hasan, I.; Madarlis, C.; Keilig, L.; Dirk, C.; Weber, A.; Bourauel, C.; Heinemann, F. Changes in biting forces with implant-supported overdenture in the lower jaw: A comparison between conventional and mini implants in a pilot study. Ann. Anat.–Anat. Anz. 2016, 208, 116–122. [Google Scholar] [CrossRef]
- Temizel, S.; Heinemann, F.; Dirk, C.; Bourauel, C.; Hasan, I. Clinical and radiological investigations of mandibular overdentures supported by conventional or mini-dental implants: A 2-year prospective follow-up study. J. Prosthet. Dent. 2017, 117, 239–246.e2. [Google Scholar] [CrossRef]
- Jawad, S.; Clarke, P. Survival of Mini Dental Implants Used to Retain Mandibular Complete Overdentures: Systematic Review. Int. J. Oral Maxillofac. Implant. 2019, 34, 343–356. [Google Scholar] [CrossRef]
- Kanazawa, M.; Feine, J.; Esfandiari, S. Clinical guidelines and procedures for provision of mandibular overdentures on 4 mini-dental implants. J. Prosthet. Dent. 2017, 117, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, D.; Mascolo, A.; Soğancı, G.; Yazıcıoğlu, H.; Mundt, T.; Schwahn, C.; Stark, T.; Biffar, R.; Cope, J.B.; McFadden, D.; et al. The Mini Dental Implant in Fixed and Removable Prosthetics: A Review. J. Oral Implant. 2011, 37, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Emami, E.; Heydecke, G.; Rompre, P.H.; De Grandmont, P.; Feine, J.S. Impact of implant support for mandibular dentures on satisfaction, oral and general health-related quality of life: A meta-analysis of randomized-controlled trials. Clin. Oral Implant. Res. 2009, 20, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Allum, S.R.; Tomlinson, R.A.; Joshi, R. The impact of loads on standard diameter, small diameter and mini implants: A comparative laboratory study. Clin. Oral Implant. Res. 2008, 19, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Sohrabi, K.; Mushantat, A.; Esfandiari, S.; Feine, J. How successful are small-diameter implants? A literature review. Clin. Oral Implants Res. 2012, 23, 515–525. [Google Scholar] [CrossRef] [PubMed]
- Kovačić, I.; Peršić, S.; Kranjčić, J.; Čelebić, A. A cohort study on short mini-implants for mandibular overdentures compared to those of standard length. Clin. Oral Implant. Res. 2020, 31, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Elsyad, M.A. Patient satisfaction and prosthetic aspects with mini-implants retained mandibular overdentures. A 5-year prospective study. Clin. Oral Implant. Res. 2016, 27, 926–933. [Google Scholar] [CrossRef]
- Marcello-Machado, R.M.; Faot, F.; Schuster, A.J.; Nascimento, G.G.; Cury, A.A.D.B. Mini-implants and narrow diameter implants as mandibular overdenture retainers: A systematic review and meta-analysis of clinical and radiographic outcomes. J. Oral Rehabil. 2018, 45, 161–183. [Google Scholar] [CrossRef]
- Song, S.-Y.; Lee, J.-Y.; Shin, S.-W. Effect of Implant Diameter on Fatigue Strength. Implant. Dent. 2017, 26, 59–65. [Google Scholar] [CrossRef]
- Ding, X.; Liao, S.; Zhu, X.; Zhang, X.; Zhang, L. Effect of Diameter and Length on Stress Distribution of the Alveolar Crest around Immediate Loading Implants. Clin. Implant. Dent. Relat. Res. 2009, 11, 279–287. [Google Scholar] [CrossRef]
- Rosa, A.; Pujia, A.M.; Arcuri, C. Complete Full Arch Supported by Short Implant (<8 mm) in Edentulous Jaw: A Systematic Review. Appl. Sci. 2023, 13, 7162. [Google Scholar] [CrossRef]
- Scherer, M.D.; McGlumphy, E.A.; Seghi, R.R.; Campagni, W.V. Comparison of retention and stability of implant-retained overdentures based upon implant number and distribution. Int. J. Oral Maxillofac. Implant. 2013, 28, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Karbach, J.; Hartmann, S.; Jahn-Eimermacher, A.; Wagner, W. Oral Health-Related Quality of Life in Edentulous Patients with Two- vs Four-Locator-Retained Mandibular Overdentures: A Prospective, Randomized, Crossover Study. Int. J. Oral Maxillofac. Implant. 2015, 30, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- Choong, E.K.M.; Gallagher, J.E.; Patel, R. Methodology and outcome of trials involving older adults in UK care homes: A rapid review. Gerodontology 2023, 40, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mifsud, D.P.; Cortes, A.R.G.; Attard, N.J. Patient-based outcomes with conventional or mini-implants immediately loaded with locator-retained mandibular overdentures: A cohort study. Clin. Implant. Dent. Relat. Res. 2020, 22, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.B.; Della Vecchia, M.P.; Cunha, T.R.; Sorgini, D.B.; dos Reis, A.C.; Muglia, V.A.; de Albuquerque, R.F.; de Souza, R.F. Short-term post-operative pain and discomfort following insertion of mini-implants for retaining mandibular overdentures: A randomized controlled trial. J. Oral Rehabil. 2015, 42, 605–614. [Google Scholar] [CrossRef]
- Rosa, A.; Pujia, A.M.; Docimo, R.; Arcuri, C. Managing Dental Phobia in Children with the Use of Virtual Reality: A Systematic Review of the Current Literature. Children 2023, 10, 1763. [Google Scholar] [CrossRef]
- Akca, K.; Cavusoglu, Y.; Sagirkaya, E.; Cehreli, M.C. Early-loaded one-stage implants retaining mandibular overdentures by two different mechanisms: 5-year results. Int. J. Oral Maxillofac. Implant. 2013, 28, 824–830. [Google Scholar] [CrossRef]
- Shady, M.M.A.; Eltorky, I.R.; Abd Eaal, Z.M. Comparative study of two types of attachments for mandibular implant-retained single complete overdenture. Tanta Dent. J. 2016, 13, 157. [Google Scholar] [CrossRef]
- Alsabeeha, N.H.M.; Payne, A.G.T.; De Silva, R.K.; Thomson, W.M. Mandibular single-implant overdentures: Preliminary results of a randomised-control trial on early loading with different implant diameters and attachment systems. Clin. Oral Implant. Res. 2011, 22, 330–337. [Google Scholar] [CrossRef]
- Kovačić, I.; Peršić, S.; Kranjčić, J.; Disha, V.; Rener-Sitar, K.; Čelebić, A. Short-term Postoperative Pain and Swelling Associated with Mini and Standard-Size Implants in the Same Patients. Int. J. Prosthodont. 2018, 31, 117–119. [Google Scholar] [CrossRef] [PubMed]
- Franco, R.; Rosa, A.; Lupi, E.; Capogreco, M. The Influence of Dental Implant Roughness on Biofilm Formation: A Comprehensive Strategy. Dent. Hypotheses 2023, 14, 90. [Google Scholar] [CrossRef]
- Jofre, J.; Valenzuela, D.; Quintana, P.; Asenjo-Lobos, C. Protocol for Immediate Implant Replacement of Infected Teeth. Implant. Dent. 2012, 21, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Mundt, T.; Schwahn, C.; Stark, T.; Biffar, R. Clinical response of edentulous people treated with mini dental implants in nine dental practices. Gerodontology 2013, 32, 179–187. [Google Scholar] [CrossRef]

| Study | Type of Studies | Implant Test Groups
| Implant Control Groups
| Type and Diameter of Implants
| Type of Attachments | Type of Prosthesis | MBL
| Follow-Up |
|---|---|---|---|---|---|---|---|---|
| Faot [7] | Comparative study |
|
| X | Locator | Overdenture | 0.2 + (−1.2) | 3 Y |
| Ahn [8] | Longitudinal prospective study |
|
|
| Locator | Overdenture |
| 36 m |
| Scarano [9] | Longitudinal prospective study |
|
|
| Ball | Overdenture | X | 5 m |
| Giannakopoulos [10] | Randomized clinical trial |
|
|
| Locator | Overdenture | 0.4 + (−1.3) | 1 Y |
| Reis [11] | Randomized clinical trial |
|
|
| Ball | Overdenture | 0.34 + (−1.3) | X |
| Payne [12] | Randomized clinical trial |
|
| X | Ball | Overdenture |
| 1 Y |
| Tymstra [13] | Comparative study |
|
| X | Ball | Overdenture | X | 5 m |
| Schuster [14] | Cohort study |
|
|
| Locator | Overdenture | 0.23 + (−0.8) | 3 m |
| Park [15] | Randomized clinical trial |
|
|
| Ball | Overdenture | 0.34 + (−0.88) | 1 Y |
| Ma [16] | Randomized clinical trial |
|
| X | Ball | Overdenture | X | 1 Y |
| Possebon [17] | Cohort study |
|
| X | Ball | Overdenture |
| 1 Y |
| Marcello-Machado [18] | Longitudinal prospective study |
|
|
| Locator | Overdenture | 0.6 + 1.2 | 1 Y |
| Bielemann [19] | Randomized clinical trial |
|
| X | Locator | Overdenture | 0.6–1.4 | 1 Y |
| Mundt [20] | Comparative study |
|
|
| Ball | Overdenture | X | 2 Y |
| Catalan [21] | Randomized clinical trial |
|
|
| Ball | Overdenture | X | 1 Y |
| Preoteasa [22] | Longitudinal prospective study |
|
|
| Ball | Overdenture | 0.89 + (−1.96) | 3 Y |
| Jofre [23] | Randomized clinical trial |
|
|
| Ball-bar | Overdenture | X | 36 m |
| Stanford [24] | Randomized clinical trial |
|
|
| Ball | Overdenture | X | 24 m |
| Maryod [25] | Longitudinal prospective study |
|
|
| Ball | Overdenture |
| 36 m |
| Mangano [26] | Longitudinal prospective study |
|
|
| Ball | Overdenture | 0.8 + (−0.95) | 3 Y |
| De Souza [27] | Randomized clinical trial |
|
|
| Ball | Overdenture | X | 12 m |
| Hasan [28] | Longitudinal prospective study |
|
|
| Ball | Overdenture |
| 1 Y |
| Temizel [29] | Longitudinal prospective study |
|
|
| Ball | Overdenture | X | 2 Y |
| Jawad [30] | Randomized clinical trial |
|
|
| Ball | Overdenture | X | 6 m |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosa, A.; Pujia, A.M.; De Angelis, R.; Arcuri, C. Narrow Implants and Overdentures in the Total Rehabilitation of Atrophic Edentulous Jaws: Review of Clinical Aspects with Meta-Analysis. Prosthesis 2024, 6, 41-52. https://doi.org/10.3390/prosthesis6010003
Rosa A, Pujia AM, De Angelis R, Arcuri C. Narrow Implants and Overdentures in the Total Rehabilitation of Atrophic Edentulous Jaws: Review of Clinical Aspects with Meta-Analysis. Prosthesis. 2024; 6(1):41-52. https://doi.org/10.3390/prosthesis6010003
Chicago/Turabian StyleRosa, Alessio, Alberto Maria Pujia, Riccardo De Angelis, and Claudio Arcuri. 2024. "Narrow Implants and Overdentures in the Total Rehabilitation of Atrophic Edentulous Jaws: Review of Clinical Aspects with Meta-Analysis" Prosthesis 6, no. 1: 41-52. https://doi.org/10.3390/prosthesis6010003
APA StyleRosa, A., Pujia, A. M., De Angelis, R., & Arcuri, C. (2024). Narrow Implants and Overdentures in the Total Rehabilitation of Atrophic Edentulous Jaws: Review of Clinical Aspects with Meta-Analysis. Prosthesis, 6(1), 41-52. https://doi.org/10.3390/prosthesis6010003








