Abstract
Background: Prosthetic hip replacement is a widely practiced surgical procedure with excellent results. Hip stems based on the Zweymüller design have a long history and their philosophy focuses on achieving long-term stability promoting physiological load transfer. The aim of this study is to evaluate outcomes, survivorship, and complication rates in a cohort of patients treated with this stem. Methods: A retrospective review was conducted to identify patients who underwent primary THA with Zweymüller stems. A total of 86 hips (43%) were implanted in men, and 114 hips (57%) in women. The mean follow-up time was 5.4 years. Patient charts were reviewed for adverse events occurring after primary THA as well as for revision and indication for revision. Patients still implanted with the hip stem were asked to complete the HOOS JR survey. Results: Ten hips (5.0%) were lost to follow up. The mean HOOS JR score at final evaluation was 96.3 points (range, 60.0–100.0). Two revisions were performed during the study for femoral stem loosening due to a periprosthetic Vancouver B2 fracture and for multiple hip dislocations. Conclusions: The Zweymüller design hip stem showed excellent survivorship and favorable clinical outcomes at a mean follow-up of 5.4 years.
1. Introduction
Osteoarthritis is a degenerative disease that leads to a significant reduction in quality of life. It is typically characterized by pain, joint stiffness, a reduction in muscle tone, and a consequent reduction in physical capabilities. The hip and knee are the joints most affected. Women tend to be the most affected gender. Half of the world’s over-65 population suffers from osteoarthritis and 25% of these are unable to carry out normal daily activities.
The European Project on Osteoarthritis (EPOSA) has made it possible to obtain more accurate demographic data on the disease, involving six European countries. It thus recorded that the prevalence of arthrosis is 30.4% [].
Total hip arthroplasty (THA) is a highly effective surgical procedure aimed at relieving pain, improving function, and restoring mobility in patients suffering from debilitating hip disorders []. The surgical techniques and stem designs for THA have evolved over time, with advancements in imaging, materials, and surgical instruments. In recent years, cementless fixation has grown in popularity, especially among older and less active patients []. Cementless fixation relies on initial implant stability from the implant design and its surface roughness to prevent micromotion, which then facilitates long-term implant stability due to osseointegration [,].
Several prosthetic, modular and monobloc, designs have been developed. Monobloc femoral stems are considered more reliable than modular stems, especially in terms of complications. In fact, modular stems can expose the patient to other problems, including trunnionosis, a fear of breakage, and taper disengagement. Mechanical failure at the modular interfaces can subsequently lead to the production of metal debris and cause adverse local tissue reactions (ALTR). On the other hand, the limitations of monobloc stems include limitations in the adjustment of anteversion, offset, and length. In addition, the lack of proximal modularity may influence implant stability and prevent the restoration of the center of rotation [].
The PROFEMUR® Z Classic femoral stem (MicroPort Orthopedics Inc., Arlington, TN, USA) is a cementless, monolithic stem that follows the Zweymüller philosophy. Hip stems based on the Zweymüller design have a long history of clinical usage [,], and their philosophy focuses on achieving long-term stability through the preservation of bone stock and promoting physiological load transfer within the hip joint. The design concept involves a straight stem with a double taper geometry to obtain optimal metaphyseal filling and stability. Because of the rectangular cross section, the proximal aspect provides 4-point rotational stability and initial mechanical fixation. With proximal plasma spray designed for press fit, the square corners of the rectangular cross section wedge into cortical bone for rotational rigidity []. The “trochanteric wing”, an extended lateral shoulder, contributes to proximal fill in addition to rotational stability.
The distal rounded aspect is conical with a tapered tip to reduce the risk of fracture and minimize the potential for an intramedullary point contact and thigh pain. By placing this rectangular cross section into a cylindrical femoral canal, cancellous bone is conserved to allow increased vascularization along the entire length of the stem. The “fit without fill” technique preserves endosteal blood supply, improves initial stability, and fits a variety of bone shapes. The stem is available with two different cervico-diaphyseal angles, 135° and 127°, and with a short or long femoral neck.
Although Zweymüller stems are clinically proven [], few studies report on the outcomes of modern versions of the design in primary THA.
The purpose of this study was to report on the mid-term clinical outcomes of patients treated with a fourth-generation design of a Zweymüller hip stem at a single institution. We reviewed a consecutive series of primary THA that utilized the hip stem designed for rotational rigidity and bone preservation to encourage vascularization. Patient-reported outcomes, survivorship, and complication rates were assessed for the patient cohort.
2. Materials and Methods
2.1. Patient Cohort
A retrospective review was conducted to identify patients who underwent primary THA at a single institution between January 2015 and December 2019. Patients who were indicated for primary THA and were at least 18 years of age at the time of surgery were included in the study. Beginning with the longest follow-up, data were extracted from the database in chronological order, and all patients meeting the inclusion criteria were included. Patients were excluded if they did not have a follow-up history or did not meet the inclusion criteria.
A total of 200 primary THAs were performed during the study period (Table 1). Of those, 86 hips (43%) were implanted in men, and 114 hips (57%) were implanted in women. The mean age was 75 years (range, 49–92). The mean body mass index was 25.1 kg/m2 (range, 16.2–36.3). Indications for primary THA included osteoarthritis (n = 152), congenital hip dysplasia (n = 2), femoral head avascular necrosis (n = 7), and femoral neck fracture (n = 39).

Table 1.
Preoperative characteristics.
2.2. Surgical Procedure
The PROFEMUR® Z classic hip stem (MicroPort Orthopedics, Inc., Arlington, TN) is a monolithic stem made of a titanium (Ti) alloy intended for cementless fixation. The Ti surface has a heavy grit-blast texture with a thickness of 0.5 mm for primary implant stability. The hip stem is available in nine sizes (126–166 mm in length), each with a long or short fixed neck and standard or extended neck offset options. The standard neck offset creates a neutral neck axis of 135° from the femoral component, whereas the extended neck offset decreases the inclination angle to 127° from the femoral component axis.
All procedures were performed at a single institution by two experienced surgeons (LP and VC). The approach used was the posterior–lateral in all the cases []. A total of 2 g of cefazolin was administered as pre-operative antibiotic prophylaxis. The surgical procedures were performed under spinal anesthesia in the lateral decubitus position. Enoxaparin 4000 i.u. per day for 20 days was used for thromboembolic prophylaxis, starting 6 h after the end of the surgical procedure. Intravenous infusion of 1 g of tranexamic acid was performed during and 6 h after surgery to control bleeding.
Upon assessing the range of motion and stability with trial components, the final components were implanted. In some cases, acetabular screws were used for the primary stability of the acetabular up.
The patients began mobilization in the ward a few hours after the surgical procedure and began walking using Canadian sticks the day after the procedure.
All 200 hips were implanted with the hip stem and compatible components (Table 2). Of those, 110 hips (55%) and 90 hips (45%) were implanted on the right and left side, respectively. Most hips were implanted with the 151 mm (n = 63), 146 mm (n = 49), or 141 mm (n = 31) long hip stem. The short standard neck was used in 115 hips (57.5%). The majority of hips (n = 185) were implanted with a ceramic on crosslinked polyethylene bearing surface. Acetabular screws were used in 2 hips (1.0%).

Table 2.
Surgical characteristics.
2.3. Clinical Evaluation
Routine clinical evaluations were scheduled according to the surgeon standard of care. Patient charts were reviewed for adverse events occurring after primary THA as well as for revision and indication for revision. If not available in the patient charts, patients were called and asked for their informed consent to disclose if a revision on the operative hip had occurred. Additionally, patients still implanted with the hip stem were asked to complete the HOOS JR survey.
The HOOS JR are joint-replacement-relevant short forms of the HOOS (Hip dysfunction and Osteoarthritis Outcome Score) survey developed at the Hospital for Special Surgery. HOOS-12 is a 12-item measure derived from the original HOOS. HOOS-12 contains 4 HOOS Pain items, 4 HOOS Function (activities of daily living and sport/recreation) items, and 4 HOOS Quality of Life (QOL) items. HOOS-12 is easier to complete than the original HOOS. As with the full-length HOOS survey, HOOS-12 is intended to elicit people’s opinions about the difficulties they experience due to problems with their hip, and covers aspects of pain, functional limitations, and hip-related quality of life. HOOS-12 has been found to be a reliable and valid alternative to HOOS in THR patients with moderate to severe OA, and to provide three domain-specific and summary hip impact scores with substantially reduced respondent burden. HOOS-12 scale scores are modified, so 0 is the worst possible and 100 is the best possible score, similar to the method used to score the original HOOS scales [].
2.4. Statistical Analyses
Continuous data are presented as means and ranges. Categorical values are given as the number of hips with a percentage. Stem survivorship was estimated using the Kaplan–Meier method [] with the end points of any component revision and stem removal. HOOS JR scores were compared using an ordinary one-way ANOVA with Tukey’s multiple comparison procedure at a significance level of 0.05. All statistical analyses were performed in GraphPad Prism version 9.5.1 (Dotmatics, San Diego, CA, USA).
3. Results
3.1. Clinical Outcomes
For the 200 hips included in the study, the mean follow-up time was 5.4 years (range, 0.8–7.5) (Table 3, Figure 1). No intraoperative complications were reported. Ten hips (5.0%) were lost to follow-up due to the death of the patient which occurred prior to collecting the HOOS JR survey. Of the remaining hips still implanted with the hip stem, the mean HOOS JR score at final evaluation was 96.3 points (range, 60.0–100.0), with 95.7% of patients achieving the patient acceptable symptom state threshold of 76.7 []. A further sub-group analysis found that there was no significant difference in scores between hips with 2–5 years, 5–7 years, and greater than 7 years follow-up (p = 0.99), indicating early and sustained patient-reported outcomes.

Table 3.
Clinical outcomes.

Figure 1.
(a) Osteoarthritis of the right hip, grade III by Kelgren and Lawrence. (b) The same patient with right hip replacement at 7 years of follow-up. The hip stem appears to be stably fixed, with evidence of spot welds, mild signs of stress shielding on the greater trochanteric area, and no signs of subsidence.
3.2. Complications
Some complications have been recorded. In particular, two patients complained of hip instability, but only one of these was revised. In both cases, the first dislocation episode was traumatic. Furthermore, a 6% incidence of heterotopic ossification was recorded, which, however, did not cause any discomfort for the patient. All recorded complications occurred in female patients.
3.3. Stem Survivorship
Two revisions were performed during the study: the first for femoral stem loosening (n = 1) due to a periprosthetic Vancouver B2 fracture (Figure 2), and the second for multiple hip dislocations (n = 1) (Table 3). The revisions for femoral periprosthetic fracture and multiple hip dislocations were performed at 0.8 years and 4.5 years, respectively. At 7 years, the Kaplan–Meier survivorship is 98.8% (95% CI, 95.1–99.7%) with the endpoint of any revision and 99.5% (95% CI, 96.5–99.9%) with the endpoint of stem removal (Figure 3).
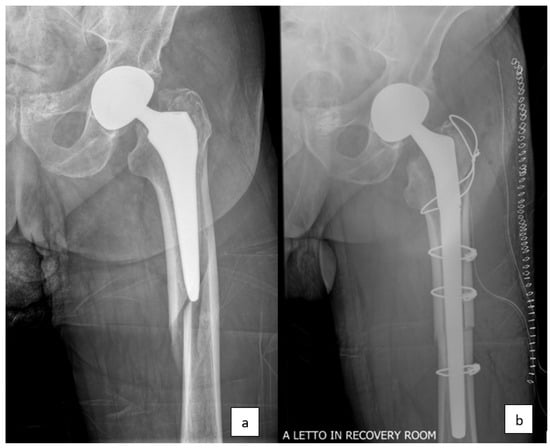
Figure 2.
(a) Periprosthetic femur fracture around the left hip, type Vancouver B2. (b) Revision stem arthroplasty.
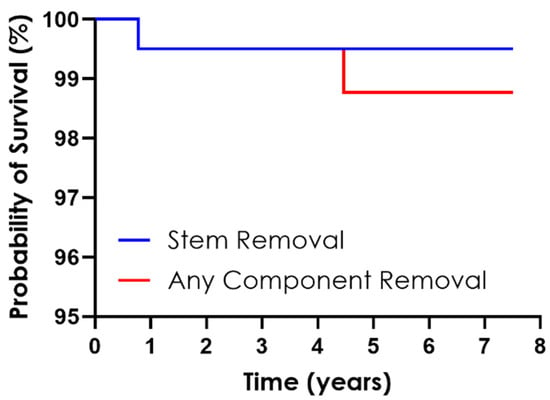
Figure 3.
Kaplan–Meier survival curve for any component and stem removal.
4. Discussion
Over the past two decades, cementless fixation for primary THA has been growing in popularity []. The current study reviewed a consecutive series of primary THA performed at a single center using a monolithic, cementless hip stem based on a modern Zweymüller design. Of the 200 primary THA with a mean follow-up of 5.4 years, only one revision was reported for femoral stem complications. Furthermore, 95.7% of patients reached the threshold for an acceptable symptom status, equal to 76.7 for HOOS JR []. Survivorship was 98.8% with the endpoint of any revision and 99.5% with the endpoint of stem removal, well surpassing the acceptable revision rate of 5.5% at 5 years reported by the Orthopedic Data Evaluation Panel (ODEP).
Hip stems based on the Zweymüller design have a long clinical history [,]. In addition to the rotational stability provided by its rectangular cross section, one of the key principles of the design philosophy is the concept of proximal load transfer []. The hip stem is designed to transfer load from the implant to the proximal femur through its lateral proximal flare [], similar to the native load distribution within the hip joint [,]. By promoting physiological load transfer, the Zweymüller stem design minimizes stress shielding, ensuring long-term stability and implant survival [].
Several studies report excellent outcomes and the long-term survival of stems based on the Zweymüller design [,,,]. In an early study of implant stability, one group found that Zweymüller stems maintained bone mineral density in the lateral-proximal femur at 3 years follow-up, indicating an absence of stress shielding []. Delauney et al. followed a cohort of 129 patients and found that the stem survivorship was 99.3% at 8 years follow-up []. Similarly, Schmolders et al. reported the overall survival rate with the endpoint of any revision was 96.8% at 10 years, and no cases were revised due to the failure of the femoral component []. In a study reporting on 30-year outcomes, only three stems were revised for aseptic loosening, resulting in 98.38% survival for the endpoint of stem removal []. The excellent survival and patient reported outcomes reported in this study demonstrate the clinical success of this modern hip stem based on the Zweymüller design.
While the hip stem is safe and efficacious, one potential disadvantage of the shouldered implant is its compatibility with tissue-sparing approaches. In particular, this type of stem could not be ideal with mini-invasive anterior approaches, which require a more curved design of stem. In our experience, however, the PFZ stems have been safely and handily implanted using a minimal incision (8 to 10 cm) and a tissue-sparing approach []. The shoulder of the PFZ stem is downsized with respect to the original Zweymüller design, allowing a major preservation of bone stock, in particular of the greater trochanteric area. The new feature of the metaphyseal zone of the stem is designed to reduce stress-shielding and allow a more physiological load transfer []. With only one patient revised for stem loosening, this study illustrates the adequate fixation of the cementless stem and a lack of stress shielding.
On the other hand, traditional monolithic stems may seem outdated compared to more modern short femoral stems. In fact, the latter are known for having obtained excellent results in the medium- and long-term follow-up in practically any type of patient, from the youngest to the oldest. Furthermore, the optimal load distribution and the preservation of the bone stock have made the short stems a valid alternative to traditional designs [].
Several authors have compared traditional stems with newer shorter designs. Tottas et al. in their article analyzed clinically and radiographically the stem object of this study with a common short stem. The two stems were compared in terms of clinical scores, Charlson Index score, pre-operative diagnosis, radiographic evaluation, the days of hospitalization, operating time, incision length, blood loss, blood transfusion requirements, and complication rates. The results demonstrated a non-inferiority of the short stem compared to the traditional one. Indeed, the authors reported relatively better short-term outcomes compared with the TL standard femoral stem, confirming what was previously reported [].
The “fit and fill” feature of the stem is reported to be associated with an increased risk of periprosthetic fractures (PPF), due to the higher rate of proximal meta-physeal fractures including intraoperative calcar fractures and postoperative Vancouver B type fractures [,]. In our cohort of patients, this complication occurred only in one case (0.5%) as a result of a big-energy trauma. The strength of the association between the stem geometry and the unstable type of periprosthetic fracture is, however, still debated in the literature, and new evidence is arising regarding additional factors able to influence the fracture pattern. The anteversion of the stem, for example, seems to be an important factor in influencing the resistance to the PPF. In particular, increasing stem anteversion could decrease the fracture risk [].
To our knowledge, this is the first study and longest follow-up report on this hip stem in primary THA. However, there are several limitations to this study. The procedures were performed at a single institution, and thus the findings may not be readily generalizable. In addition, baseline clinical data were not collected, so we were not able to assess clinical scores for improvement. Radiographic analysis was not conducted either, so we cannot report on radiolucencies. Nonetheless, only one hip was revised for femoral stem loosening, caused by a periprosthetic fracture type Vancouver B2, suggesting a significative implant stability at midterm follow-up.
5. Conclusions
In conclusion, the hip stem used in this study showed excellent survivorship with the endpoint of stem removal and favorable clinical outcomes at a mean follow-up of 5.4 years. The majority of patients achieved the patient acceptable symptom state at final follow-up. Taken together, these findings suggest that the fourth-generation Zweymüller-based design demonstrates the continued clinical success of hip stems based on this design philosophy.
Author Contributions
Conceptualization: V.C., A.F.-P. and C.M. Data curation: L.P., E.L. and V.C. Formal analysis and writing of the original draft: A.F.-P., C.M., M.S. and V.C. Writing—review and editing: M.S., V.C. and G.L. Funding acquisition: L.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by MicroPort Orthopedics, Inc.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee “Comitato Etico Interaziendale A.O “Canta Croce e Carle” di Cuneo, AA.SS.LL. Cuneo 1, Cuneo 2, Asti” (protocol code 75-2021, date of approval: 28th April 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare that this study received funding from MicroPort Orthopedics Inc. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication. Author Allison Fetz-Palazola and Chase Mareno were employed by the company MicroPort Orthopedics Inc. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Siviero, P.; Veronese, N.; Smith, T.; Stubbs, B.; Limongi, F.; Zambon, S.; Dennison, E.M.; Edwards, M.; Cooper, C.; Timmermans, E.J.; et al. Association Between Osteoarthritis and Social Isolation: Data from the EPOSA Study. J. Am. Geriatr. Soc. 2020, 68, 87–95. [Google Scholar] [CrossRef]
- Rasmussen, M.B.; El-Galaly, A.; Daugberg, L.; Nielsen, P.T.; Jakobsen, T. Projection of Primary and Revision Hip Arthroplasty Surgery in Denmark from 2020 to 2050. Acta Orthop. 2022, 93, 849–853. [Google Scholar] [CrossRef]
- Wang, J.; Deng, Z.; Huang, B.; Zhao, Z.; Wan, H.; Ding, H. The Short-Term Outcomes of Cementless Stem for Hip Arthroplasty in the Elderly Patients: Comparison with Patients < 65 Years. BMC Musculoskelet Disord. 2022, 23, 1070. [Google Scholar] [CrossRef]
- Galante, J.; Rostoker, W.; Lueck, R.; Ray, R.D. Sintered Fiber Metal Composites as a Basis for Attachment of Implants to Bone. J. Bone Jt. Surg. Am. 1971, 53, 101–114. [Google Scholar] [CrossRef]
- Engh, C.A.; O’Connor, D.; Jasty, M.; McGovern, T.F.; Bobyn, J.D.; Harris, W.H. Quantification of Implant Micromotion, Strain Shielding, and Bone Resorption with Porous-Coated Anatomic Medullary Locking Femoral Prostheses. Clin. Orthop. Relat. Res. 1992, 285, 13–29. [Google Scholar] [CrossRef]
- Wang, D.; Li, H.; Zhang, W.; Li, H.; Xu, C.; Liu, W.; Li, J. Efficacy and Safety of Modular versus Monoblock Stems in Revision Total Hip Arthroplasty: A Systematic Review and Meta-Analysis. J. Orthop. Traumatol. 2023, 24, 50. [Google Scholar] [CrossRef]
- Huo, M.H.; Martin, R.P.; Zatorski, L.E.; Keggi, K.J. Total Hip Arthroplasty Using the Zweymuller Stem Implanted without Cement. J. Arthroplast. 1995, 10, 793–799. [Google Scholar] [CrossRef]
- Vervest, T.M.J.S.; Anderson, P.G.; Van Hout, F.; Wapstra, F.-H.; Louwerse, R.T.; Koetsier, J.W.A. Ten to Twelve-Year Results With the Zweymüller Cementless Total Hip Prosthesis. J. Arthroplast. 2005, 20, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Zweymüller, K.A.; Lintner, F.K.; Semlitsch, M.F. Biologic Fixation of a Press-Fit Titanium Hip Joint Endoprosthesis. Clin. Orthop. Relat. Res. 1988, 235, 195–206. [Google Scholar] [CrossRef]
- Roškar, S.; Antolič, V.; Mavčič, B. Surgeon-Stratified Cohort Analysis of 1976 Cementless Zweymüller Total Hip Arthroplasties from a Single Hospital with 23,255 Component Years of Follow-Up. Arch. Orthop. Trauma Surg. 2020, 140, 1275–1283. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, W.M.; Branson, J.J. Posterior-Lateral Approach to Minimal Incision Total Hip Arthroplasty. Orthop. Clin. N. Am. 2004, 35, 131–136. [Google Scholar] [CrossRef]
- Hage, A.; Hage, F. Kaplan-Meier Survival, Actuarial Survival, Censoring, and Competing Events—What Is What? Ann. Thorac. Surg. 2022, 114, 40–43. [Google Scholar] [CrossRef]
- Kunze, K.N.; Fontana, M.A.; MacLean, C.H.; Lyman, S.; McLawhorn, A.S. Defining the Patient Acceptable Symptom State for the HOOS JR and KOOS JR After Primary Total Joint Arthroplasty. J. Bone Jt. Surg. 2022, 104, 345–352. [Google Scholar] [CrossRef]
- Troelsen, A.; Malchau, E.; Sillesen, N.; Malchau, H. A Review of Current Fixation Use and Registry Outcomes in Total Hip Arthroplasty: The Uncemented Paradox. Clin. Orthop. Relat. Res. 2013, 471, 2052–2059. [Google Scholar] [CrossRef]
- Khanuja, H.S.; Vakil, J.J.; Goddard, M.S.; Mont, M.A. Cementless Femoral Fixation in Total Hip Arthroplasty. J. Bone Jt. Surg. 2011, 93, 500–509. [Google Scholar] [CrossRef]
- Inaba, Y.; Kobayashi, N.; Oba, M.; Ike, H.; Kubota, S.; Saito, T. Difference in Postoperative Periprosthetic Bone Mineral Density Changes Between 3 Major Designs of Uncemented Stems: A 3-Year Follow-Up Study. J. Arthroplast. 2016, 31, 1836–1841. [Google Scholar] [CrossRef]
- Liu, B.; Wang, H.; Zhang, N.; Zhang, M.; Cheng, C.-K. Femoral Stems With Porous Lattice Structures: A Review. Front. Bioeng. Biotechnol. 2021, 9, 772539. [Google Scholar] [CrossRef]
- Schmolders, J.; Amvrazis, G.; Pennekamp, P.H.; Strauss, A.C.; Friedrich, M.J.; Wimmer, M.D.; Rommelspacher, Y.; Wirtz, D.C.; Wallny, T. Thirteen Year Follow-up of a Cementless Femoral Stem and a Threaded Acetabular Cup in Patients Younger than Fifty Years of Age. Int. Orthop. (SICOT) 2017, 41, 39–45. [Google Scholar] [CrossRef]
- Delaunay, C.; Kapandji, A.I. Survival Analysis of Cementless Grit-Blasted Titanium Total Hip Arthroplasties. J. Bone Jt. Surg. Br. Vol. 2001, 83-B, 408–413. [Google Scholar] [CrossRef]
- Pisecky, L.; Hipmair, G.; Schauer, B.; Böhler, N. 30-Years of Experience with the Cementless Implanted Alloclassic Total Hip Arthroplasty System—An Ultra-Long-Term Follow-Up. J. Orthop. 2018, 15, 18–23. [Google Scholar] [CrossRef]
- Logroscino, G.; Donati, F.; Campana, V.; Saracco, M. Stemless Hip Arthroplasty versus Traditional Implants: A Comparative Observational Study at 30 Months Follow-Up. HIP Int. 2018, 28, 21–27. [Google Scholar] [CrossRef]
- Tottas, S.; Ververidis, A.; Kougioumtzis, I.; Tilkeridis, K.; Tsigalou, C.; Karaglani, M.; Drosos, G. MINIMA Short Stem Versus Standard Profemur (TL) Stem in Primary Total Hip Replacement: A Comparative Study. Cureus 2022, 14, 23771. [Google Scholar] [CrossRef]
- Calkins, T.E.; Goetz, D.D.; Zalewski, J.T.; Jones, C.A.; Gaumer, P.R.; Ford, M.C.; Toy, P.C.; Crockarell, J.R.; Harkess, J.W.; Mihalko, W.M.; et al. Hip Arthroplasty Femoral Stem Designs and Their Association With Early Postoperative Periprosthetic Femoral Fractures. J. Arthroplast. 2023, 38, 849–854. [Google Scholar] [CrossRef]
- Sershon, R.A.; McDonald, J.F.; Ho, H.; Hamilton, W.G. Periprosthetic Femur Fracture Risk: Influenced by Stem Choice, Not Surgical Approach. J. Arthroplast. 2021, 36, S363–S366. [Google Scholar] [CrossRef]
- Čengić, T. Impact of Cementless Zweymüller Stem Anteversion on Resistance to Periprosthetic Fracture in Total Hip Arthroplasty. Acta Clin. Croat. 2021, 60, 429–434. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).