1. Introduction
Humeral resurfacing arthroplasty (HRA) has increasingly become a popular alternative to total shoulder arthroplasty (TSA) or reverse shoulder arthroplasty (RSA) for the treatment of glenohumeral osteoarthritis, rheumatoid arthritis, and avascular necrosis of the humeral head.
Unlike a conventional shoulder joint replacement (being a hemiarthroplasty, a TSA or an RSA) which involves the removal of the humeral head and the placement of an intramedullary stem, HRAs only consist of reaming the epiphyseal region of the humeral head and placing a press-fit or cemented prosthetic cap on the residual portion of the humeral head. In such a surgical procedure, the reconstruction of the humeral head surface is performed without the need to implant a stem or to perform any osteotomy. This implies that the humeral neck and more than half of the humeral head are retained, and the native head-shaft angle remains intact. The resurfacing component may or may not be combined with a glenoid component [
1,
2]. It has been reported that inclination, version, offset, and head-shaft angles remained unchanged after HRA, with respect to pre-operative values [
3,
4,
5,
6]. All those factors are beneficial to restore the biomechanics of the shoulder joint as well as patient satisfaction. Both the wide variability of the normal values of the glenohumeral joint between individuals, and the great challenge in restoring the anatomy with arthroplasty, were well described by Boileau et al. [
7]. With accurate positioning of the HRA, the surgeon aims to reproduce the individual anatomy of the glenohumeral joint (diameter, radius of curvature and version of the humeral head, and lateral offset of the proximal humerus), and to preserve the bone stock. Restoring the normal glenohumeral kinematics enables the avoidance of damage to the rotator cuff and impingement on the glenoid component or on the coracoacromial arch. Achieving a radius of curvature close to normal is essential, as its excessive increase may lead to overstuffing of the joint [
8]. Similarly, the height of the humeral head is of paramount importance, since an increase of 5 mm or more is associated with a decrease in range of motion up to 30° due to tendons overstuffing, whilst a decrease could lead to an impingement of the greater tuberosity under the acromion [
9,
10,
11]. The medialization of the humeral head, caused by surface wear, may be counterbalanced by the thickness of HRA implants [
12]. As a consequence, the lever arm of the rotator cuff tendons and the deltoid muscle, as well as the tension of soft tissues, can be restored [
13,
14,
15]. Some authors believe that it is easier to restore the anatomical offset and the height of the center of rotation with a HRA rather than with a TSA. Thomas et al. [
12] reported that HRA resulted in an average increase in the humeral offset of 5 mm (from 23 mm pre-operatively to 28 mm post-operatively). However, a mean pre-operative erosion of 6 mm of the lateral offset was present, so the HRA restored the anatomic offset that had been lost because of the erosion.
Given the benefits of HRA, especially in younger patients, and its successful outcomes in terms of postoperative recovery, this surgical technique has been considered as one of the first choices for the treatment of glenohumeral diseases [
16]. However, long-term assessments of functional outcome and revision rate are essential. The primary aim of the present study is to retrospectively evaluate and to report the results of a series of HRA performed at our institution from a subjective, functional, and radiological point of view, with a minimum follow-up of 2 years, in a consecutive series of patients. Our secondary aim is to the compare the results and revision rate of the present study with those present in the literature.
2. Materials and Methods
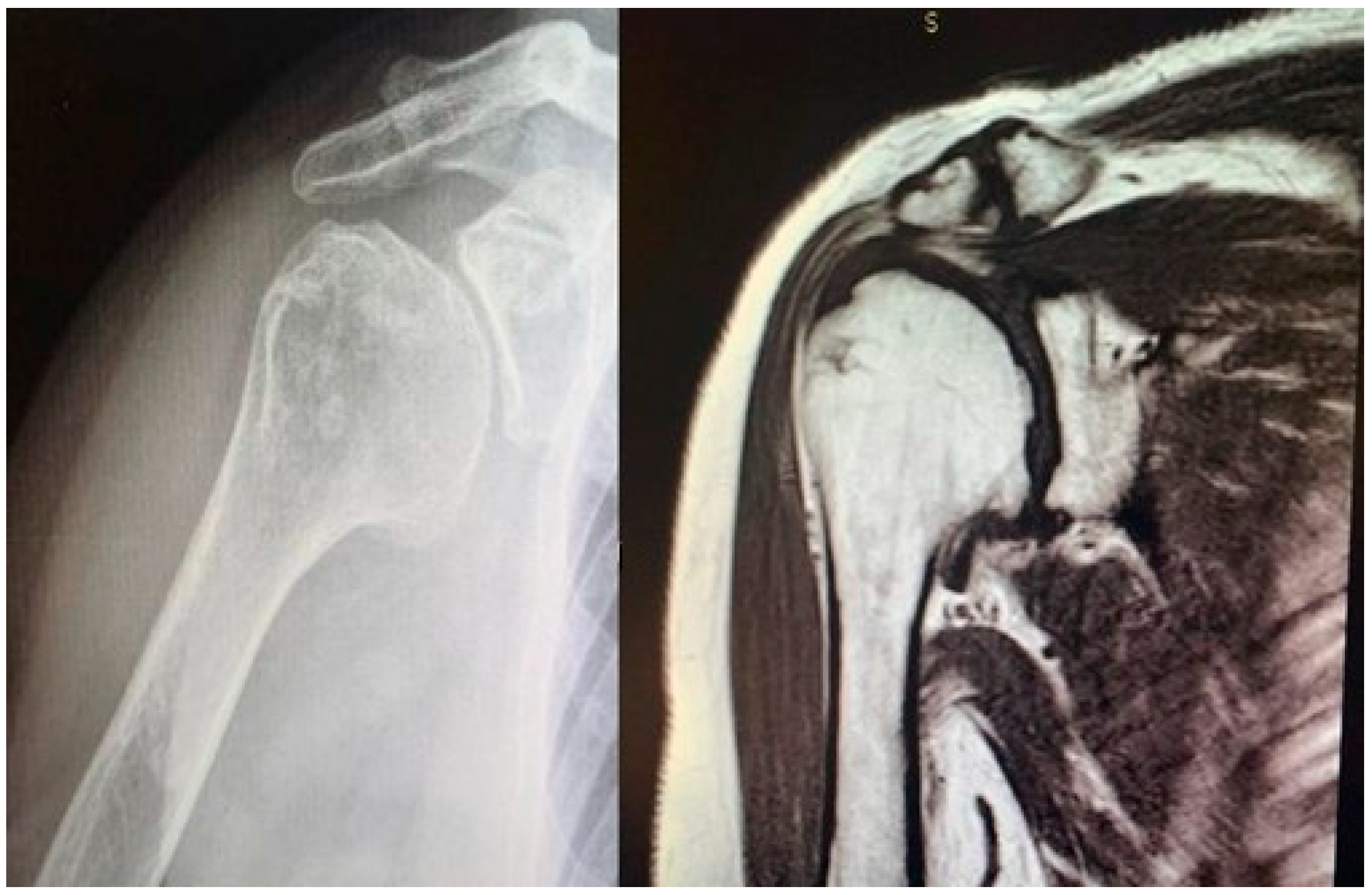
Study design. A retrospective and observational study was performed. The inclusion criteria were as follows: patients with (1) a diagnosis of glenohumeral degeneration with rotator cuff integrity following primary osteoarthritis (
Figure 1) or rheumatoid arthritis or avascular necrosis of the humeral head, (2) glenoid articular surface type A1 or A2, according to Walch’s classification [
17,
18], (3) more than 60% residual humeral head [
4,
12], (4) who underwent HRA (
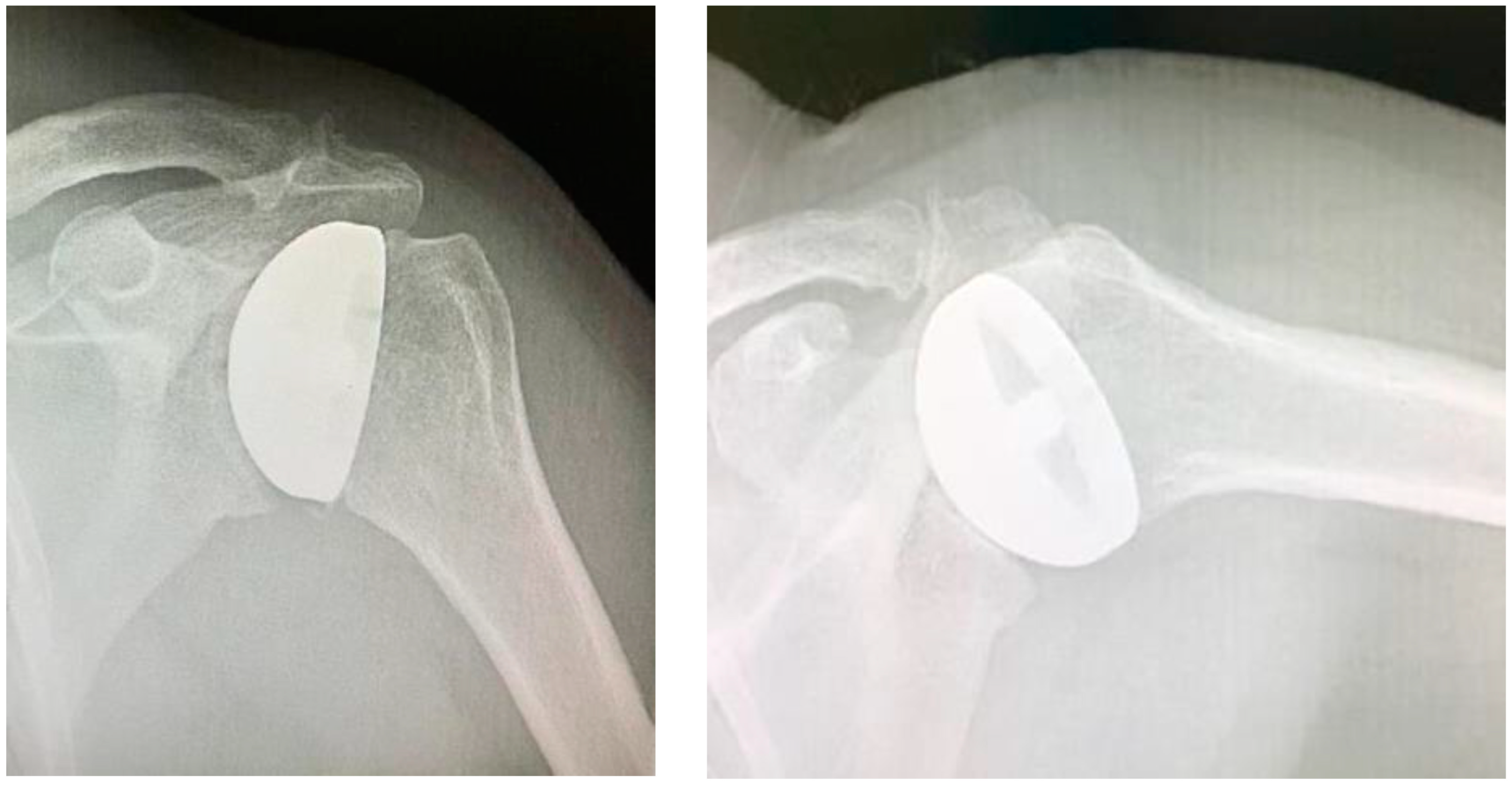
Figure 2) operated on by a single surgeon and (5) who completed a minimum clinical and radiological follow-up of 2 years.
At our institution, no Ethical Committee nor Institutional Review Board approval is necessary for retrospective and observational studies, and all patients gave their informed consent to data collection and their anonymous use for scientific and teaching purposes. This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Surgical procedure. All surgeries were performed by the senior Author (S.G.), implanting a Durom Shoulder Cup (Zimmer Biomet, Warsaw, IN, USA), a Copeland Humeral Resurfacing Head Surgery (Zimmer Biomet, Warsaw, IN, USA) or a SMR Resurfacing Shoulder Prosthesis System (Lima Corporate, Udine, Italy). All patients were pre-operatively evaluated through a clinical examination, plain radiographs in the antero-posterior and axillary views, a computed tomography scan, and magnetic resonance imaging (
Figure 3), in order to determine the correct indication to HRA.
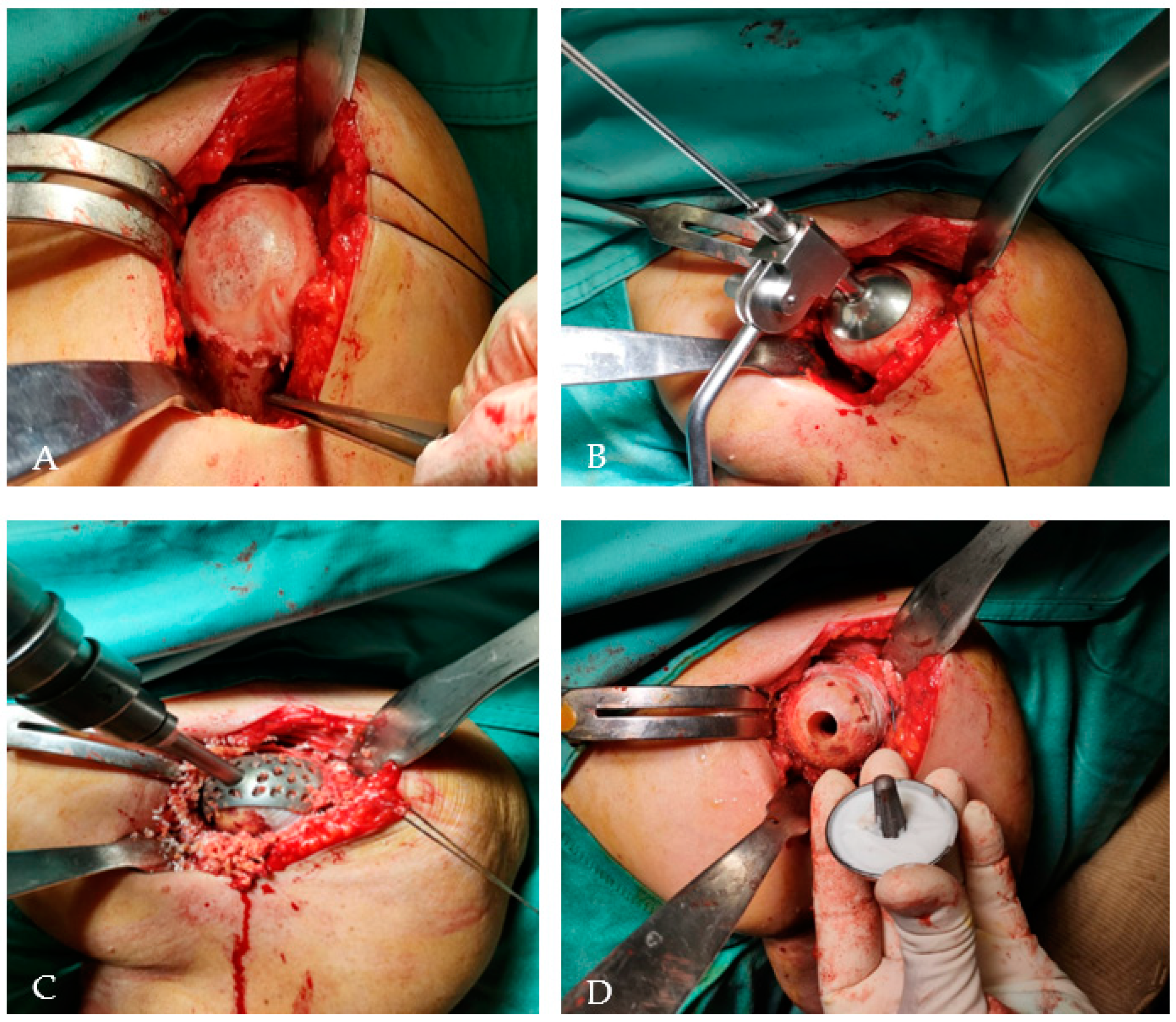
A deltopectoral approach was used in all cases [
19]. After identification of the subscapularis tendon, its tenotomy was performed at approximately 1 cm from its insertion on the lesser tuberosity. Tenotomy of the long head of the biceps was carried on in all cases, and no tenodesis procedures were performed. The humeral head was gently dislocated with gradual release of soft tissues, and any osteophyte was removed to precisely identify the humeral neck and the neck-shaft angle. Attention was paid to restore the correct retroversion and inclination of the head. Also, the lateral and vertical offsets were restored to re-establish the appropriate lever arm of the deltoid and supraspinatus muscles, in order to achieve adequate active mobility of the shoulder. Since stemless resurfacing prostheses were implanted without interfering with the humeral diaphysis, the posterior offset was not considered during this procedure. Although the surgical instrumentation provided a standardized neck-shaft angle of 135°, it could be adjusted to appropriately fit the patient’s morphology within a range of 115–150°. The humeral head version could be tailored within a range of 20–50° of retroversion to the forearm axis, as well. Then, the humeral head was prepared. A pin guide wire was placed at the center of the humeral head, parallel to the anatomical neck, and passed down through the humeral head to the lateral cortex to provide stability. Using a cannulated humeral surface cutter of the appropriate size over the guide wire, the articular cartilage was completely removed to expose the subchondral bone. Afterwards, the central peg hole was drilled. If sclerotic subchondral bone remained after the reaming phase, additional multiple perforations were performed to allow a better penetration of the cement into the humeral bone to ensure a higher prosthetic adhesion. At this point, the trial humeral prosthesis was placed onto the prepared bone and a trial reduction was performed. Implant stability and range of motion were checked, and a size adjustment was performed if needed. Then, the trial cup was replaced by the definitive component, which was cemented with 1-millimiter-thick low-viscosity bone cement (
Figure 4). The glenoid was never resurfaced. Nevertheless, all the osteophytes were removed and, in some cases of glenoid chondral lesions, microfractures were performed. The subscapularis tendon was re-attached with multiple non-resorbable sutures, and the wound was closed in layers. To control bleeding, in the absence of contraindications, tranexamic acid was administered both intravenously and locally, as previously described [
20].
Post-operative care. After surgery, the arm was rested in an internal rotation and adduction sling for 3 weeks. Passive range of motion exercises from the sling were allowed from the 1st post-operative day. After 3 weeks, active range of motion exercises in forward elevation and abduction were allowed. Both passive and active external and internal rotation exercises were not allowed until 3 weeks after surgery. Also, strengthening exercises with light weights were permitted thereafter. Returns to everyday activities and sedentary jobs were permitted at 6 to 8 weeks after surgery. Patients were asked to wait 3 months before returning to more physically demanding jobs, such as those that involve heavy lifting or manual labor, and to sports activities.
Clinical and radiological assessment. All patients were evaluated clinically and radiographically at 1, 3, 6, and 12 months after surgery, and then annually. Shoulder function was assessed using the disabilities of the arm, shoulder and hands (DASH) [
11] and Constant scoring system [
12]. Plain radiographs in the true antero-posterior and axillary views were obtained at each follow-up visit. The distance between the humeral diaphyseal axis and the line through the medial wall of the coracoid process was measured, to analyze the morphological changes in the glenoid.
Statistical analysis. The Wilcoxon signed rank test was used to identify any statistical difference between the values of the Constant and DASH scores assessed before surgery and at the last follow-up. The level of significance was set at p < 0.05 and the data were analyzed by use of SPSS software (IBM, Armonk, New York, NY, USA).
3. Results
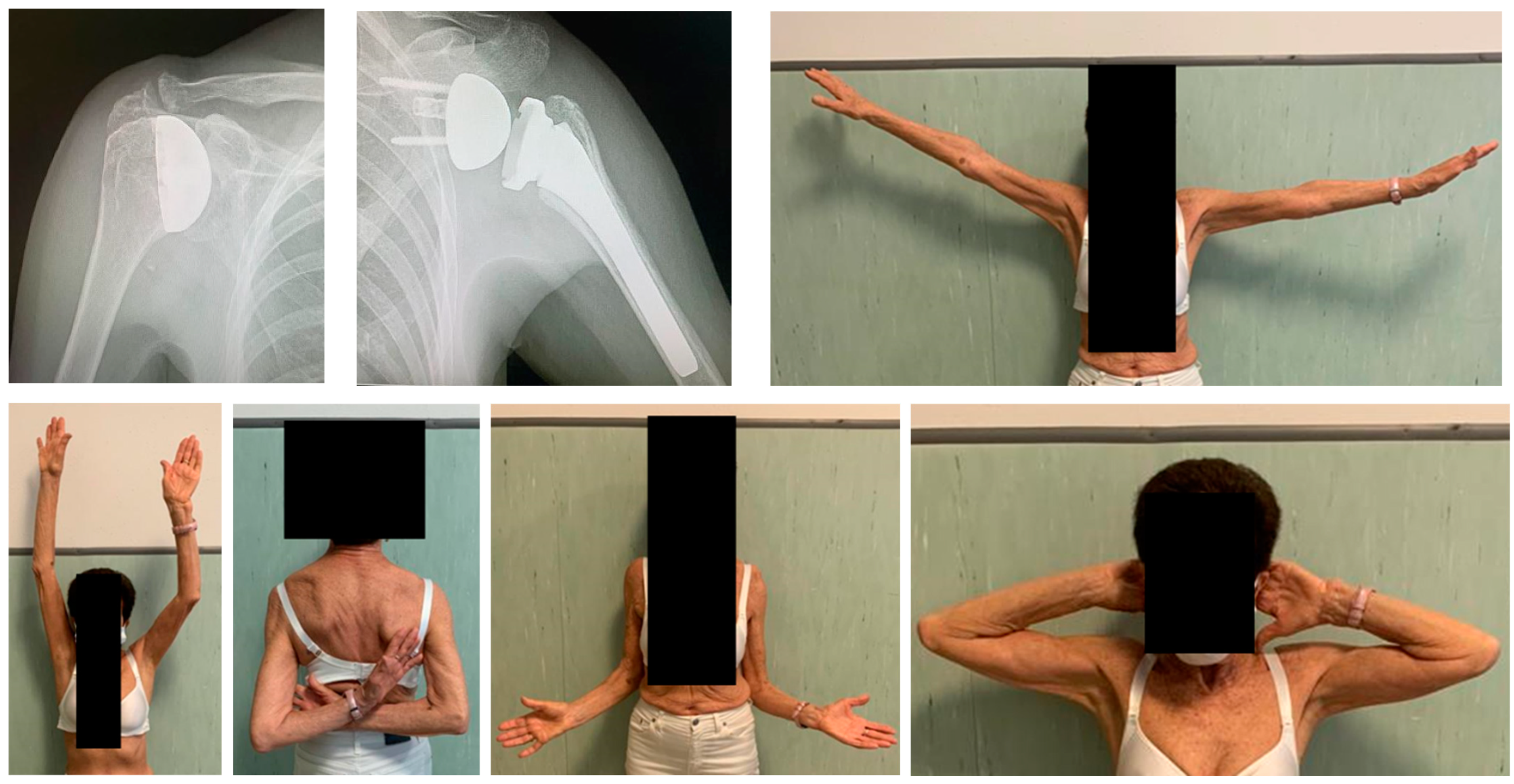
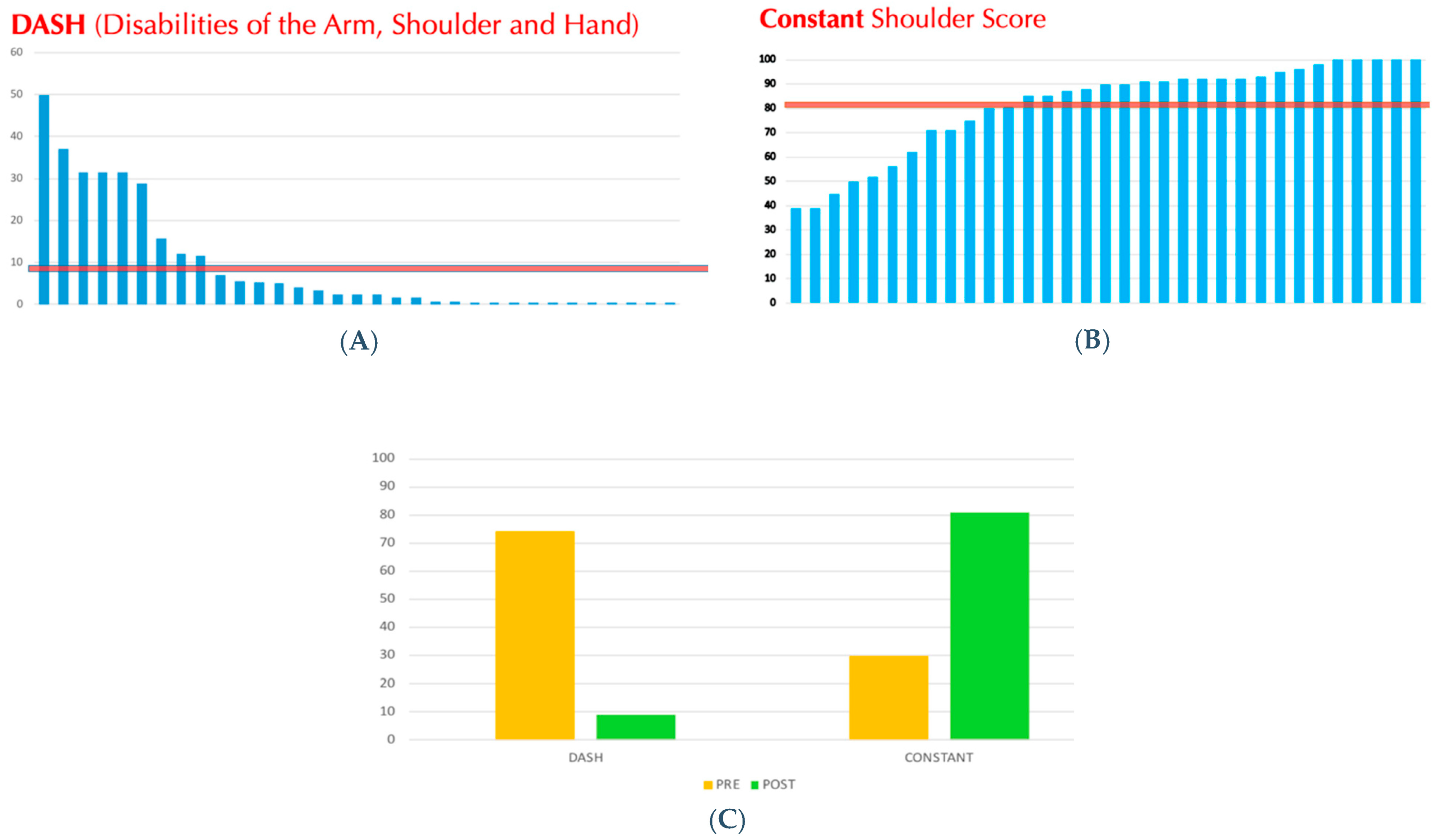
From July 2005 to August 2021, a total of 76 patients (78 shoulders) who underwent HRA were identified, but only 33 (44%) completed the clinical and radiological follow-up at more than 2 years after surgery; they were included in the present study (
Figure 5). However, all the 78 patients (or if deceased, their relatives) were contacted by phone to obtain information on their medical history after the prosthetic surgery, namely regarding the need of further surgery. The operative time was less than 1 h for all surgeries, mean 45 ± standard deviation 9.6 (range 35–58) minutes. As regard to peri-operative complications, no blood transfusion was required in any case. The mean follow-up was 128 ± 61 (range 24–216) months. The mean age at surgery was 63.4 ± 12.5 (range 31–83) years. There were 17 females and 14 males, two of which had bilateral surgeries (one male and one female). The Constant score significantly improved, from a mean pre-operative score of 29.9 ± 12.1 (range 10–63) points to a mean post-operative score of 81.2 ± 18.9 (range 39–100) points (
p < 0.05). The DASH score also improved significantly, from a mean pre-operative score of 46.7 ± 2.9 (range 45–50) points to a mean post-operative score of 8.9 ± 13.5 (range 0–50) points (
p < 0.05) (
Figure 6). Considering the three different implants, patients were equally distributed according to age and gender, and no statistically significant differences among the clinical outcomes nor complication rate were found. Only one patient was diagnosed with rheumatoid arthritis. To highlight the medialization of the joint line at follow-up visits, the distance between the humeral diaphyseal axis and the line through the medial wall of the coracoid process was measured. It was significant only in one case, in which the patient developed a rotator cuff deficiency and consequently needed a revision procedure to an RSA.
Only 2 out of the 78 cases (3%) had to be subjected to a surgical revision procedure. One patient developed a shoulder instability due to a subscapularis insufficiency, 2 years after index surgery, while the other one developed a rotator cuff arthropathy due to a rotator cuff degenerative tear, 9 years after index surgery. In both cases, the surgical revision procedure consisted of RSA.
However, in all 33 implants, at final radiological follow-up, no radiolucent lines were noticed, nor aseptic loosening of the prosthetic cup, nor clinically relevant central migration of the humeral head due to progressive glenoid degenerative changes.
4. Discussion
HRA has become a popular treatment strategy for primary glenohumeral osteoarthritis, rheumatoid arthritis, and osteonecrosis of the humeral head. One of its main advantages is its capability to preserve the bone stock, since no humeral neck osteotomy is performed, while restoring the articular humeral surface and joint function. This concept is of particular importance, especially for younger patients, who may need future surgical interventions [
21,
22]. In case a revision is needed, the humeral head prosthesis can be easily removed and converted into a TSA or an RSA. Clearly, the disease must be limited to the humeral head, and the quality of the subchondral bone should be taken into account when considering such a procedure. In fact, the subchondral surface must be capable of supporting at least 60% of the implant [
3]. Other than being a bone-stock preserving procedure, HRA allows for the reduction of the risk of significant complications associated with stemmed arthroplasties, including humeral diaphyseal fractures and significant bleeding. Accordingly, HRAs could be considered minimally invasive procedures with an almost absent blood loss and short recovery times. Besides that, biomechanical studies have demonstrated the better capability of HRA to adapt and restore the native glenohumeral anatomy, compared to stemmed prostheses [
22]. On the other hand, technical difficulties associated with HRA are predominantly a result of incorrectly sizing and orienting the prosthesis, resulting in ‘over-stuffing’ of the joint. Moreover, normal shoulder anatomy can vary considerably, both inter- and intra-individually. The humeral head is retroverted (range 0–55°) and inclined medially (range 30–55°) with respect to the humeral shaft, and the offset of the humerus in relation to the glenoid may vary in three dimensions, and the radius of curvature ranges from 20 to 30 mm [
1]. Consequently, a precise pre-operative planning before performing an arthroplasty procedure is essential in order to obtain good functional outcomes and to limit complications.
As regard to functional outcomes, good results were observed in the study population at a mean follow-up of almost 11 years. The results in terms of DASH and Constant scores were similar or even better than those already present in the literature [
16]. Lebon et al. [
1], in a study with 41 HRA at a mean follow-up of 44 months, noted a Constant score higher than 75 points in 56% of the patients and a DASH score of 17 ± 15. Levy et al. [
3], in their study, analyzed 19 HRA with a mean follow-up of 6.8 years (5 to 10 years), and they found a post-operative Constant score of 73.5 in primary osteoarthritis and 72.1 in rheumatoid arthritis. In a study conducted from 2005 to 2009 by Mansat et al. [
20] on 64 shoulders with an average follow-up of 36 months, the post-operative Constant score reached 68 points and the post-operative DASH score reached 28 points.
With respect to revision rate and complications, different parameters should be considered, such as the center of rotation, inclination angle, and concomitant or previous shoulder pathologies. Alolabi et al. [
23] found in their study that 65.1% of the HRAs demonstrated an inadequate reaming of the humeral head, resulting in overstuffing of the glenohumeral joint. Geervliet et al. [
24] agreed that, after HRA, the normal glenohumeral anatomy, regarding the center of rotation, is not completely reproduced. They found a significant increase in the center of rotation in the revision group, compared to the non-revision group (8.0 mm versus 4.9 mm, respectively). In other words, the probability of revision will increase significantly with an increased center of rotation. Overstuffing has always been a suspect for failure.
Lebon et al. [
1], in a study with a mean follow-up of 44 months, detected a revision rate of 9.8%; they also noted the tendency towards varus positioning of the implants and the increase in lateral offset of the humeral head as possible radiologic prognostic factors for future failure. Delaney et al. [
25] reported that patients operated on with HRA without any concomitant shoulder pathology showed good clinical outcomes. Shoulders in which concomitant procedures (rotator cuff repair, capsular shift, or biceps tenodesis) were performed still achieved acceptable clinical outcomes. However, shoulders that had undergone prior surgery (for example arthroscopic debridement, Bankart repair, rotator cuff repair, subacromial decompression, acromioclavicular joint or distal clavicle resection and biceps tenodesis) had worse clinical outcomes and were at increased risk of failure.
In the present series, the revision rate was 3% (2 out of 78 cases, with all patients—or their relatives—having been contacted by telephone, if no clinical and radiological follow-up was obtained). Both cases were revised to RSA, and in both cases the procedure did not show technical difficulties and it could be performed with bone-stock sparing, because the humeral cap could be easily removed with minimal bone resection.
Only one patient who was diagnosed with rheumatoid arthritis was included in the study. Although shoulder replacement represents a solid treatment for rheumatoid arthritis, there is still no consensus about the most appropriate implant. HRA is often the preferred choice, but it is not suitable in severely damaged joints with massive bone loss or poor bone quality [
26]. It should be stated that in our only rheumatoid case, the joint damage was managed with minimal bone resection, not to decrease the offset.
Rasmussen et al. [
27] analyzed 1210 HRAs between 2006 and 2013 and they noticed a revision rate of 8.84%, while the mean time to revision was 27 ± 19 months. Hwang et al. [
28] considered 101 cases between 2007 and 2020, with a median follow-up of 7 years, and they found a revision rate of 7%. Levy et al. [
3], in their cohort of 103 HRAs operated from 1990 to 1994, highlighted a revision rate of 8.16% with a mean follow-up of 6.8 years.
The results depend directly on correct indications, which for these implants are limited, and on the correct surgical technique, with a precise sizing and positioning of the implant. In our opinion, the major difficulty consists of finding the adequate landmarks on a pathologic shoulder, and in the accurate placement of the guide-pin, on which drilling and subsequent implant positioning rely. An experienced surgeon, and a complete prosthetic system, are key to achieving good results in terms of clinical scores, patient satisfaction, and a low revision rate. The humeral component cementation represents a fundamental step during this procedure, as well. In our opinion, cementation prevents the risks of aseptic mobilization, and, at the same time, it does not cause further difficulties during a possible revision surgery. In addition, this surgical procedure has to be considered minimally invasive for both the saving of the epiphyseal and diaphyseal bone stock and the limited blood loss.
Limitations are present in this study. First, it is a retrospective study with a small sample size: it may be difficult to generalize the obtained results. In addition, about half of patients were lost during the clinical and radiological follow-up. This situation can be explained by two factors: the retrospective nature of the study, and the long follow-up period considered. Surgeries were performed over an 18-year period and many patients became unavailable or died. Also, the surgeon’s experience and the surgical technique have increased and improved over time, eventually leading to better outcomes. Additionally, the time frame of the follow-up can also be considered as a limitation. The mean follow-up was 128 months, but the range (24–216 months) was rather wide, and this could influence the results. Also, three different implants were used to perform HRAs in the present study. The types of implants were adapted over time, due to the fact that our regional Public Health System regulates the tendering procedure for buying in medical devices, and therefore implants may vary in their availability over time. However, despite the use of these three distinct systems, no statistically significant differences were obtained with regard to patient distribution in terms of age, gender, and clinical outcome.
On the other hand, the strengths of the present study are, in our opinion, the single surgeon design, which limits biases with regard to indications and technical execution of the procedure, a thorough subjective clinical and radiographical follow-up (with complete information about revision rate even for patients clinically and radiologically lost), and the long mean follow-up (almost 11 years), which is the longest one for HRA in the literature.