1. Introduction
The purpose of this case report was to highlight how a protocol, which has been in use for a considerable period in rehabilitations involving areas with low aesthetic value, can also be applied in aesthetic zones, such as the anterior sectors. This protocol allows for necessary adjustments to achieve the best possible result without requiring complex procedures. By implementing this protocol, clinicians can minimise and simplify their approach to patients, reducing the number of sessions needed to transfer clinical information to the laboratory and the number of impressions to be taken [
1]. Moreover, it is essential to provide additional information about the historical development of dental implantology and the evolution of dental implant restoration workflows [
2]. Dental implantology has a rich history, with early attempts at tooth replacement dating back thousands of years in ancient civilisations. However, modern dental implantology as we know it today emerged in the 20th century with significant advancements in materials, surgical techniques, and prosthetic components. One of the groundbreaking contributions to dental implantology came in the 1950s when Dr Branemark successfully placed the first modern dental implant [
3]. This achievement introduced the concept of osseointegration, which refers to the direct structural and functional connection between the implant and the surrounding bone. Osseointegration became crucial in developing various implant systems and protocols, revolutionising dental rehabilitation practices. Dental implant restoration follows a comprehensive workflow that includes preoperative planning, implant placement surgery, a healing period, and prosthetic rehabilitation [
4,
5]. Advanced imaging technologies, such as cone beam computed tomography (CBCT), are vital in assessing bone quality and quantity, facilitating precise implant-placement planning. Minimally invasive surgical techniques are commonly employed during implant placement, often performed under local anaesthesia to ensure patient comfort and minimise post-operative complications. Following implant placement, a healing period is necessary for osseointegration and proper bone integration around the implant. Temporary restorations may be utilised during this period to maintain aesthetics and function. Once osseointegration is achieved, the final prosthetic phase commences. This phase involves fabricating custom abutments and designing and creating the final implant-supported prosthesis, including a single crown, bridge, or complete denture. The prosthetic restoration aims to restore the patient’s smile’s functional aspects, aesthetic harmony, and natural appearance [
6,
7].
The congenital absence of lateral incisors, commonly called lateral incisors agenesis, is a dental anomaly that poses significant challenges to oral health professionals. Affecting both aesthetics and function, this condition necessitates a multidisciplinary approach for effective rehabilitation. Among the various treatment options available, dental implants have increasingly become the modality of choice for their longevity, function, and aesthetic potential. The role of high-quality dental impressions in such cases cannot be overstated. Precise impressions are vital for an optimal fit between the implant and surrounding oral structures. The objective is to replicate the natural anatomy as closely as possible, ensuring that the prosthetic element merges seamlessly with the patient’s dental and gingival landscape. Inadequate impressions can lead to misaligned or improperly positioned implants, causing functional issues and affecting the overall aesthetic outcome.
Additionally, the quality of periodontal tissues plays a critical role in the success of dental implants. Healthy gums and bones offer a biocompatible interface for the implant, facilitating osseointegration and long-term stability. A poor periodontal status can compromise the implant’s integrity, potentially leading to failure over time. Therefore, the health of periodontal tissues is assessed rigorously before considering implant-based rehabilitation in cases of lateral incisors agenesis.
In summary, dental implants have revolutionised restorative dentistry by providing a predictable and durable solution for replacing missing teeth. Integrating advanced implant systems and streamlined workflows has resulted in efficient and aesthetically pleasing outcomes, benefiting the mouth’s functional and aesthetic areas.
This case report aimed to demonstrate how this protocol can be implemented to achieve optimal results without complex procedures, thereby reducing the number of sessions and impressions required. This case report also emphasises the importance of integrating advanced implant systems and streamlined workflows to enhance the aesthetic outcomes of dental implant restorations.
2. Materials and Equipment
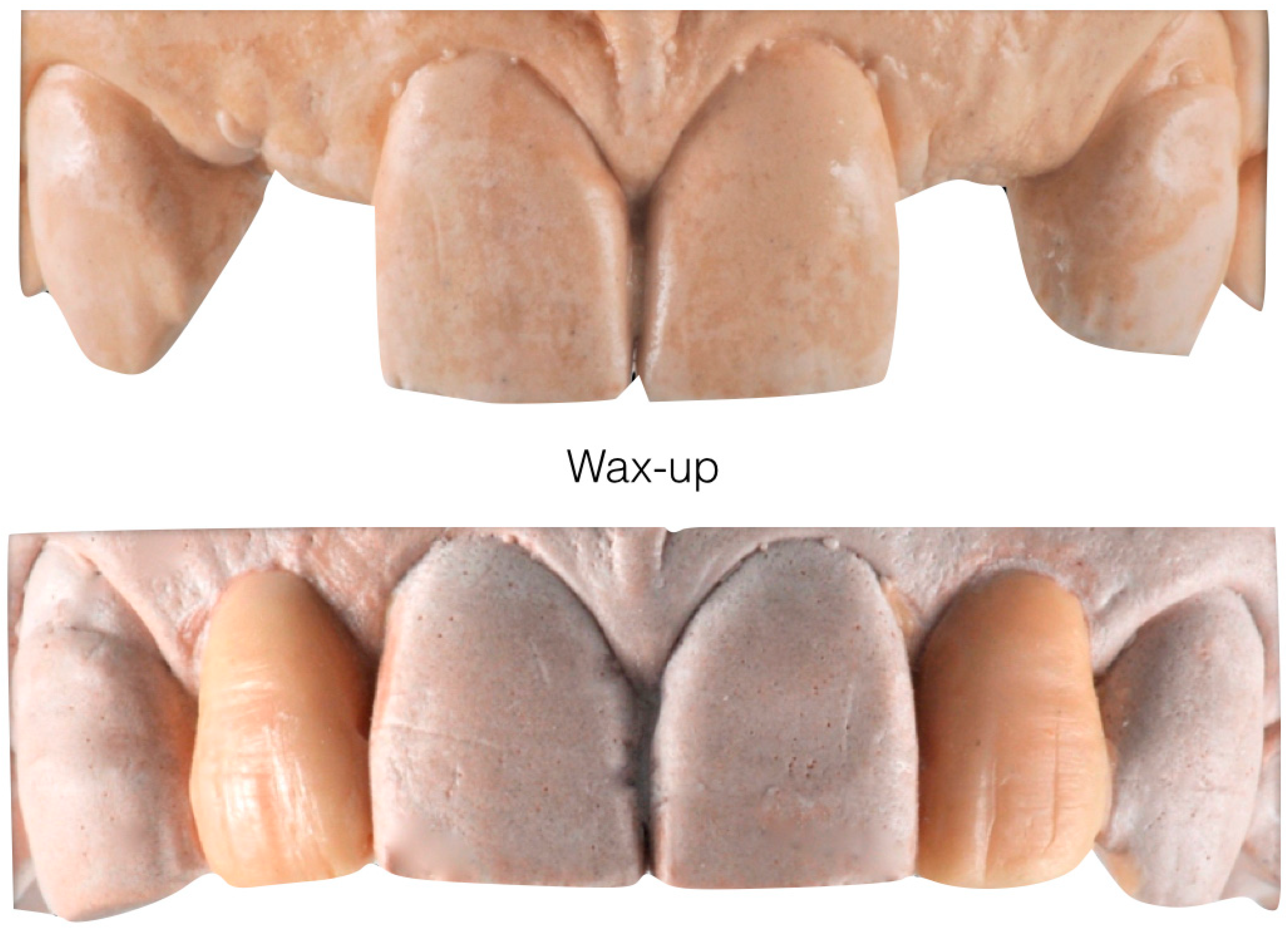
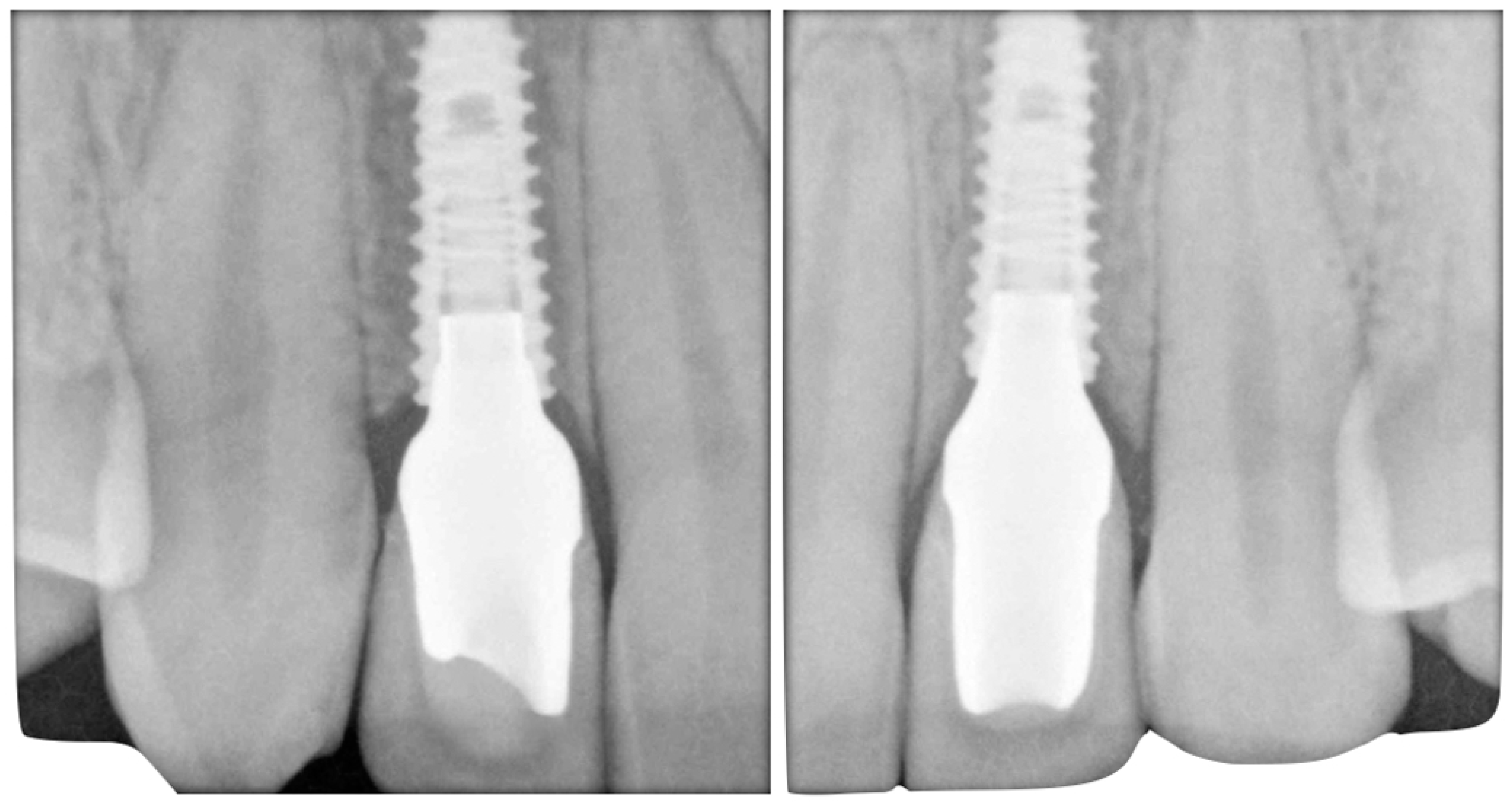
The case describes rehabilitating two congenitally missing lateral incisors in a young patient (38 years old) undergoing orthodontic treatment to create the necessary space for implant placement (
Figure 1 and
Figure 2). Two fibre-reinforced composite Maryland bridges (Tender Fiber Quattro—Micerium) were utilised for provisional rehabilitation (
Figure 3,
Figure 4 and
Figure 5). Two Osstem TSIII 3.5 × 10.0 implants (1.5 mm subcrestal), two straight Osstem Zirconia abutments, and two-layered lithium disilicate crowns were employed for the definitive restoration (
Figure 5,
Figure 6,
Figure 7,
Figure 8,
Figure 9,
Figure 10,
Figure 11,
Figure 12,
Figure 13,
Figure 14,
Figure 15,
Figure 16,
Figure 17,
Figure 18,
Figure 19 and
Figure 20) [
8,
9]. The dental implant position was planned after a three-dimensional radiographic analysis in a prosthetically guided way. Patient rehabilitation was performed with an immediate post-surgery provisional (Maryland-type, cemented with a resinous cement) application. Subsequently, a delayed loading of the new provisional dental implant was retained (cemented with zinc oxide eugenol cement) and finally, definitive crowns (cemented with a definitive resinous cement) on Osstem
® abutments were installed (3 months).
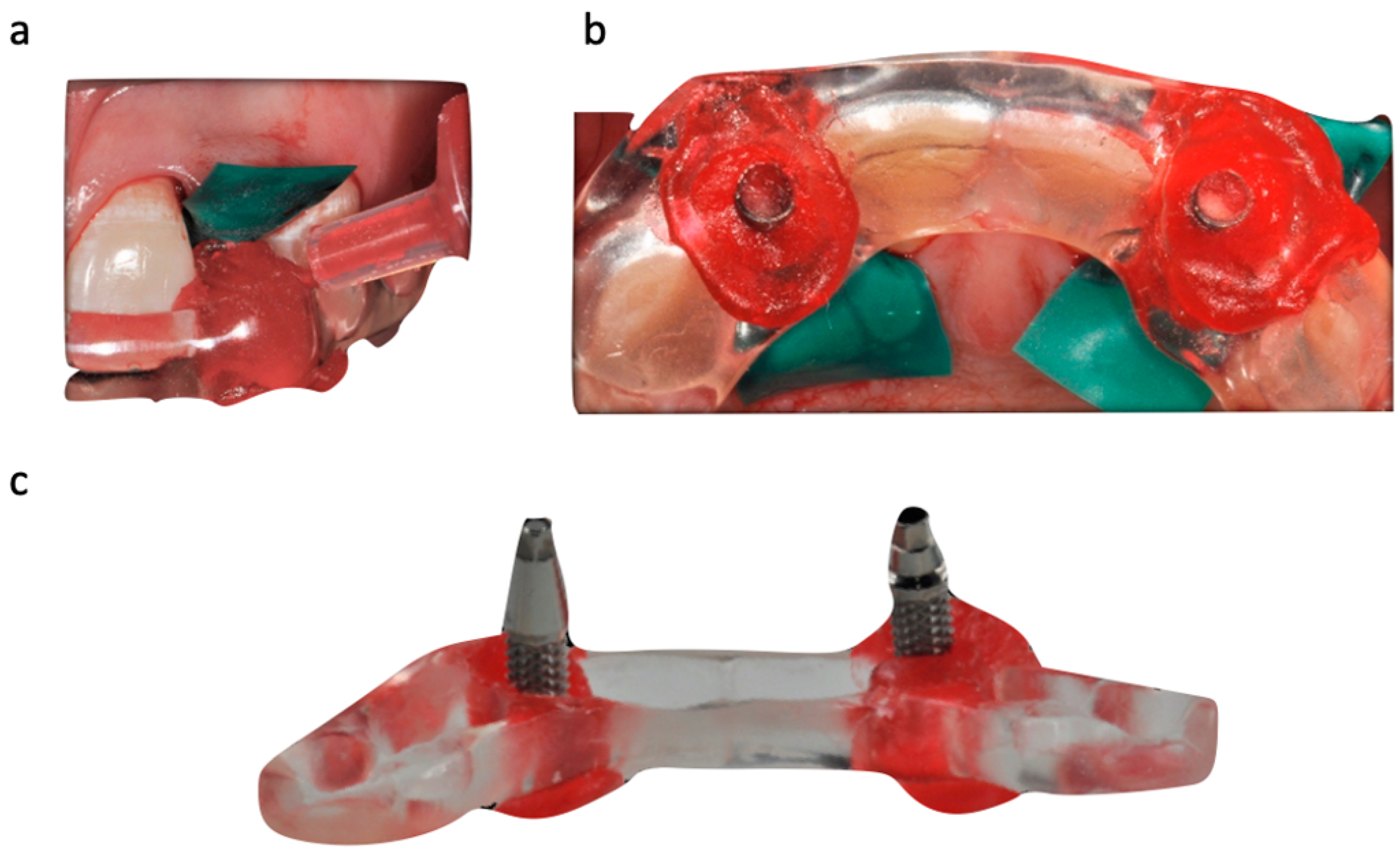
The position of the dental implants was recorded during the surgical insertion using a transfer key fabricated based on the initial model (before surgery). Subsequently, our technician duplicated the wax-up and soft tissues with precision systems and transferred the implant positions to the working model, providing us with a provisional restoration that had already been inserted during implant uncovering (
Figure 6,
Figure 7,
Figure 8 and
Figure 9). We transferred the definitive emergence profile, conditioned by the provisional without periodontal surgery techniques, to the laboratory by recasting the artificial gum on the model (
Figure 11,
Figure 12 and
Figure 13) through the finalized provisionals (
Figure 14). At this point, the laboratory had all the information required to construct an individualised and treated abutment, using appropriate processing techniques to achieve a natural-looking response together with the metal-free prosthetic crown.
3. Detailed Procedure
Initial models and diagnostic wax-ups were created using silicone (Elite HD+, Zhermack) with a closed tray technique, and provisional restorations were fabricated using different colours of acrylic resin (Jet Kit
®, Lang, IL, USA). Temporary restorations were then placed in position (
Figure 5). A transparent resin transfer key was employed to streamline the implant’s placement. The information regarding the implant’s position was conveyed to the laboratory through a series of specialized steps. These included the installation of titanium temporary abutments sourced from Osstem
® in South Korea, securing the workpiece within the transfer key using pattern resin, precision drilling on the master hard stone model (
Figure 6,
Figure 7 and
Figure 8), and an accurate placement of analogues in this model by employing a recasting technique with hard stone material (
Figure 9). After revealing the implanted components, provisional restorations were promptly delivered as part of the uncovering procedure to encourage optimal soft tissue healing (
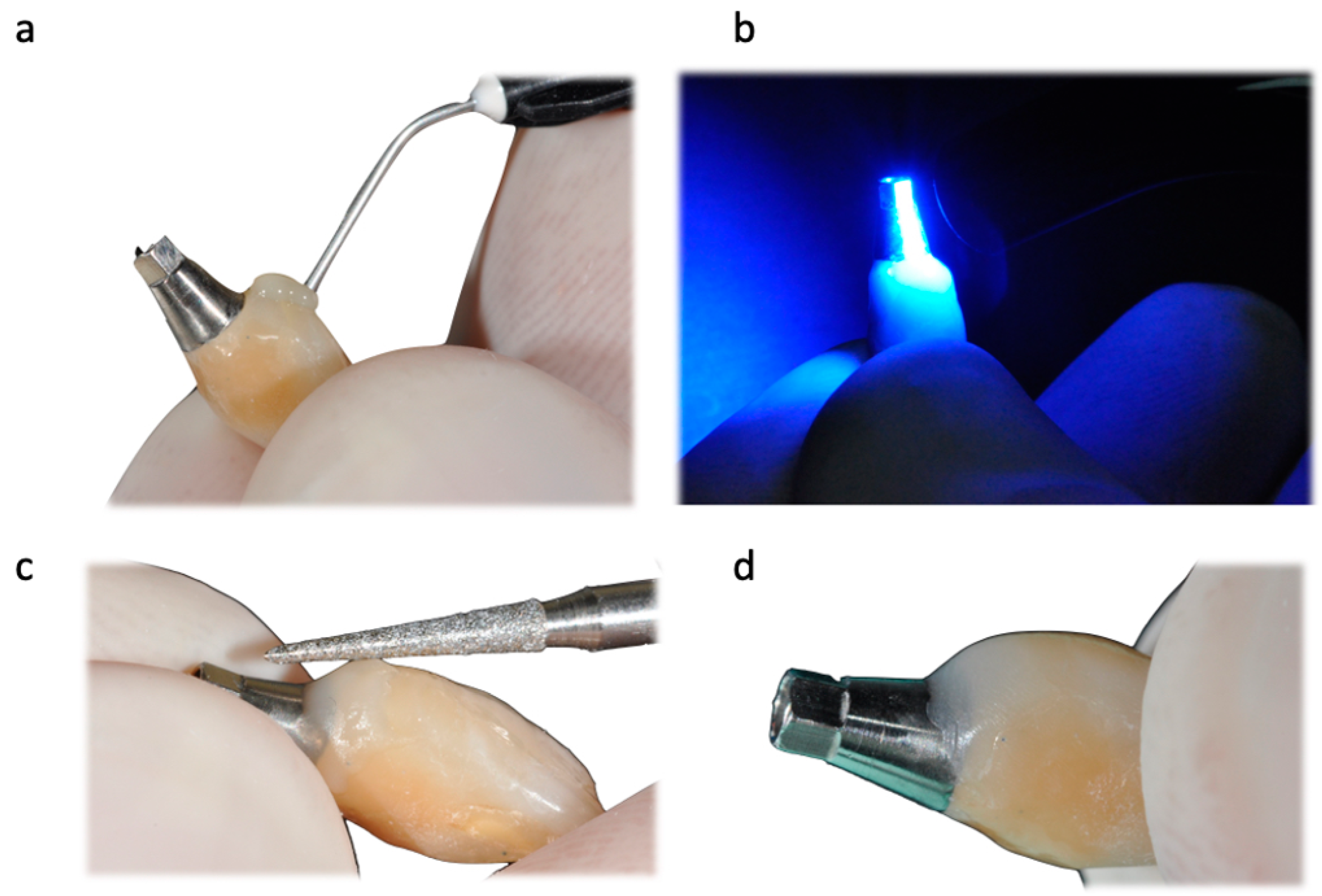
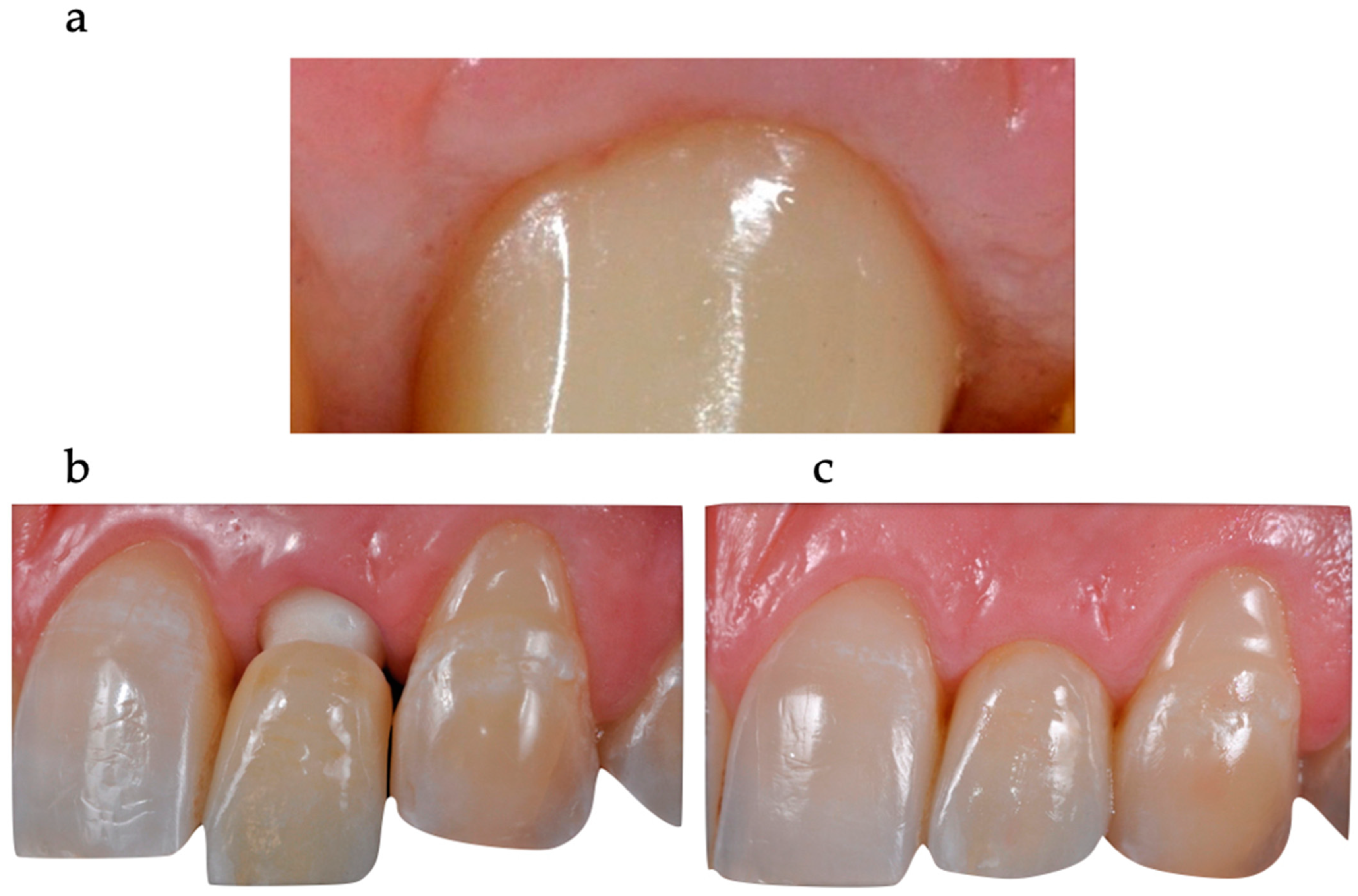
Figure 10). Adjustments were made to the emergence profile to condition the surrounding soft tissues properly, and specialized conditioning procedures were carried out (
Figure 11 and 12). Before and after conditioning, the changes in the profiles were documented (
Figure 13). The new profiles obtained were transferred to the master model by mounting the modified provisional restorations with analogues, and a new artificial gum was created through recasting (
Figure 14). Once the soft tissues had healed correctly, guided by the modified and polished provisional as in
Figure 11, it was possible to transfer the mucosal profile onto the master model. By removing the provisionals from the oral cavity, they were then positioned on the master model, corresponding to the dental implant analogues in the master model. The master model that had previously been modified and freed from any over contours or undercuts was relined at this point with a laboratory silicone to simulate the profile of the mucosa. The abutments were customised using ceramic and fluorescence techniques to achieve optimal emergence profiles (
Figure 15). Gingival profiles were assessed, and the abutments were inserted accordingly (
Figure 16 and
Figure 17). The final stage involved the placement of crowns, which were fabricated using ceramic material (E.max ceram
®, Ivoclar, Naturno, Italy). A last radiographic check was performed to ensure a proper alignment and fit of the restorations. The case was considered completed, and aesthetic integration was achieved. Overall, this case report encompassed various steps, including an initial assessment, diagnostic procedures, provisional restorations, implant placement, emergence profile modifications, abutment customisation, crown placement, and the final evaluation of the completed case.
4. Expected Results
The discussion regarding aesthetic dental implant restoration encompasses several key aspects, including the materials used, the types of dental implants, surgical techniques for soft tissue improvements, and prosthetic or impression techniques. Each factor is crucial in achieving optimal aesthetic outcomes for dental implant restorations. Aesthetic dental implant restorations often utilise materials that mimic the natural appearance of teeth and soft tissues. Ceramic materials, such as zirconia and lithium disilicate, are commonly chosen for their lifelike translucency, strength, and durability. These materials offer excellent aesthetic properties, allowing for a seamless integration with the surrounding natural dentition [
10,
11]. Various types of dental implants are available for aesthetic restorations, including tapered, narrow-diameter, and short implants. Tapered implants are preferred for their ability to provide primary stability in compromised bone situations, while narrow-diameter implants are suitable for cases with limited interdental space. Short implants are employed when the vertical bone height is insufficient, allowing for more conservative surgical procedures [
12].
Achieving harmonious soft tissue contours around dental implants is crucial for aesthetic success. Socket preservation, guided bone regeneration, and soft tissue grafting can enhance soft tissue outcomes. Socket preservation techniques, such as ridge preservation or immediate implant placement, help maintain the soft tissues’ natural architecture following tooth extraction. Guided bone regeneration involves using barrier membranes and bone grafts to promote bone growth and augment soft tissue support. Soft tissue grafting techniques, such as connective tissue grafts or free gingival grafts, can correct deficiencies in the peri-implant mucosa and create an aesthetically pleasing emergence profile [
13,
14]. Accurate prosthetic and impression techniques are vital to achieving optimal aesthetics in dental implant restorations. Procedures like digital dentistry, computer-aided designs, and computer-aided manufacturing (CAD/CAM) allow for the precise fabrication of implant-supported restorations, ensuring optimal fit and aesthetics. In addition, custom abutments and provisional restorations can aid in developing the emergence profile and evaluating the final aesthetic outcome before the placement of definitive restorations. Different impression techniques, such as closed-tray or open-tray impressions, are selected based on the clinical situation and the clinician’s preference [
15,
16,
17].
According to our protocol, working with a single impression in this specific case is possible. Once the implants have been positioned, proceed with the rebasing of the plaster model in such a way as to obtain a correct and harmonious emergence profile to transfer the accurate and updated information to the dental technician, who will be able to create an exact copy of the provisional artefact or at least with the same emergence profile, thus respecting the soft tissues.
Implant-prosthetic-impression techniques in dentistry are crucial for achieving accurate and predictable results in fabricating implant-supported restorations. These impressions capture the exact position and orientation of dental implants, adjacent teeth, and the surrounding oral tissues. In the aesthetic zone, where the appearance of the final restoration is of utmost importance, proper oral tissue management before taking impressions becomes even more critical. Before proceeding with implant-prosthetic impressions, it is essential to ensure that the oral tissues in the aesthetic zone are healthy and adequately managed [
18,
19]. This involves a comprehensive assessment of the soft tissues, including the gingiva and the interdental papillae. The goal is to establish an ideal soft tissue architecture that supports the final restoration and creates a natural, harmonious appearance. Several techniques and procedures can be employed to manage the oral tissues effectively. One commonly used technique is the use of provisional restorations. Provisional restorations can be customized to shape and contour the soft tissues, promoting proper healing and adaptation. They can be modified to guide the growth of interdental papillae, shape the gingival contours, and establish an optimal emergence profile. Soft tissue augmentation procedures may sometimes be necessary to enhance the aesthetics and achieve an ideal soft tissue foundation [
20]. Techniques such as connective tissue grafts, free gingival grafts, or guided bone regeneration can correct deficiencies in the soft tissues and create an optimal peri-implant environment [
21]. Proper oral hygiene is another essential consideration in oral tissue management before taking impressions. Adequate plaque control and oral hygiene practices prevent inflammation, infection, and peri-implant complications. Patients should be educated on proper oral hygiene techniques and a healthy oral environment. Once the oral tissues have been adequately managed, implant-prosthetic impressions can be taken using various techniques. These may include open-tray or closed-tray impression techniques, depending on the specific clinical situation and the type of implant system being used. Care must be taken to accurately capture the position and angulation of the implants, surrounding soft tissues and adjacent teeth. Precision and attention to detail during the impression process are critical to ensure an optimal fit, aesthetics, and the functionality of the final restoration. Implant-prosthetic-impression techniques in dentistry require proper oral tissue management in the aesthetic zone. This involves assessing and optimizing the soft tissue architecture through provisional restorations and augmentation procedures. Additionally, maintaining good oral hygiene is crucial for long-term success. Clinicians can achieve accurate and predictable results by effectively managing the oral tissues before taking impressions, leading to aesthetically pleasing and functionally successful implant-supported restorations.
Dental implant management in the aesthetic zone poses unique challenges due to the high aesthetic expectations of patients. The aesthetic zone refers to the area in the mouth visible when smiling or speaking, typically involving the anterior teeth. Achieving natural-looking and harmonious outcomes in this region requires careful planning, precise execution, and a multidisciplinary approach involving the implant surgeon, prosthodontist, and dental technician. One of the primary considerations in dental implant management in the aesthetic zone is the selection of appropriate materials. Ceramic materials are often preferred for their lifelike translucency, their ability to mimic a natural tooth colour and shape, and biocompatibility. These materials blend seamlessly with the surrounding natural dentition, ensuring a natural and aesthetic appearance. Choosing dental implants is also crucial in achieving optimal aesthetic outcomes [
22]. Tapered implants offer primary stability in compromised bone situations and are commonly used in the aesthetic zone. Narrow-diameter implants are suitable for cases with limited interdental space, while short implants are employed when the vertical bone height is insufficient. Selecting the right implant type ensures proper implant positioning and stability, which is essential for achieving an aesthetic result. Surgical techniques are vital in enhancing soft tissue contours around dental implants in the aesthetic zone. Dental implant management in the aesthetic zone requires careful consideration of materials, implant selection, surgical techniques, and prosthetic procedures. By integrating advanced technologies, adopting a patient-centred approach, and collaborating with a multidisciplinary team, clinicians can achieve predictable and aesthetically pleasing outcomes for patients undergoing dental implant restorations in the aesthetic zone. By carefully selecting appropriate materials, utilising suitable dental implant types, employing advanced surgical techniques for soft tissue enhancement, and employing accurate prosthetic and impression techniques, clinicians can enhance the aesthetic outcomes of dental implant restorations [
23].
Periodontal tissue management with provisional restorations is crucial in prosthodontics and implant-prosthetic treatment. Provisional restorations serve as temporary replacements for missing teeth or as intermediate restorations during the healing phase of dental implant placement [
7]. Effective management of the periodontal tissues around these provisional restorations plays a significant role in achieving optimal treatment outcomes. One important aspect of periodontal tissue management with provisional restorations is preserving the emergence profile. Provisional restorations should be designed to replicate the natural emergence profile of the teeth. The emergence profile refers to the contour of the tooth visible in the oral cavity, including the shape and position of the soft tissues. A proper emergence profile supports the surrounding soft tissues and helps create an aesthetically pleasing appearance, as in [
24]. It aids in developing harmonious gingival contours and facilitates the final fabrication of definitive restorations. Another aspect of periodontal tissue management is the control of gingival contours. Provisional restorations can be modified to influence the shape and position of the gingival tissues. By carefully adjusting the contours of the provisional restoration, it is possible to guide the healing and maturation of the gingival tissues. This process is critical in cases where the gingival margin needs to be shaped or repositioned for optimal aesthetics and oral hygiene access. Soft tissue conditioning is also vital in periodontal tissue management with provisional restorations. The provisional restorations can condition the soft tissues and create an ideal environment for healing and tissue maturation. This may involve adjustments to the provisional restoration to promote proper tissue adaptation, contouring the emergence profile, and ensuring good oral hygiene access. Effective periodontal tissue management with provisional restorations requires a close collaboration between the prosthodontist, implant surgeon, and dental technician [
25]. Preserving the emergence profile, control of gingival contours, and soft tissue conditioning are essential to achieving optimal treatment outcomes. By carefully managing the periodontal tissues during the provisional phase, clinicians can lay the foundation for successful final restorations with optimal aesthetics and long-term stability [
26,
27].
A multidisciplinary approach involving a collaboration between the implant surgeon, prosthodontist, and dental technician is often necessary to achieve the desired aesthetic results. Understanding the patient’s expectations and communication throughout treatment is vital for successful aesthetic dental implant restorations.
Limitations and Biases
While the presented protocol for dental implant restoration offers numerous advantages and contributes to achieving optimal aesthetic outcomes, it is essential to acknowledge certain limitations that should be considered. These limitations include the following.
Generalizability: The protocol presented in this manuscript is based on a specific case report and may not be universally applicable to all patients or clinical scenarios. Variations in patient anatomy, bone quality, and treatment goals may require modifications to the protocol.
Case Report: The case report described in this manuscript represents a single case with specific circumstances. The findings and outcomes observed in this case may not necessarily indicate outcomes in larger patient populations.
Long-term follow-up: The presented report primarily focuses on the immediate outcomes and short-term success of dental implant restorations. Long-term follow-up data, including the stability of soft tissue contours, aesthetic durability, and implant success rates, are necessary to fully assess the protocol’s efficacy.
Operator expertise: The successful implementation of the protocol relies on the clinician’s experience, skill, and knowledge in dental implantology and restorative procedures. The outcomes may vary based on the proficiency and expertise of the treating clinician.
Cost considerations: The materials and techniques employed in the protocol, such as zirconia abutments and disilicate lithium crowns, may involve higher costs compared to alternative options. Economic factors and patient affordability may influence the feasibility and widespread adoption of the protocol.
Despite these limitations, the presented protocol offers valuable insights for achieving aesthetic and functional success in dental implant restorations. Further research involving larger sample sizes and long-term follow-ups is warranted to validate the findings and address the limitations identified in this report. By acknowledging these limitations and continuing to refine and adapt the protocol based on future research and clinical experiences, clinicians can optimise outcomes and provide the best possible care for patients undergoing dental implant restorations in aesthetic zones.