Long-Term Follow-Up of Medial Pivot Total Knee Arthroplasty: A Systematic Review of the Current Evidence
Abstract
1. Introduction
2. Materials and Methods
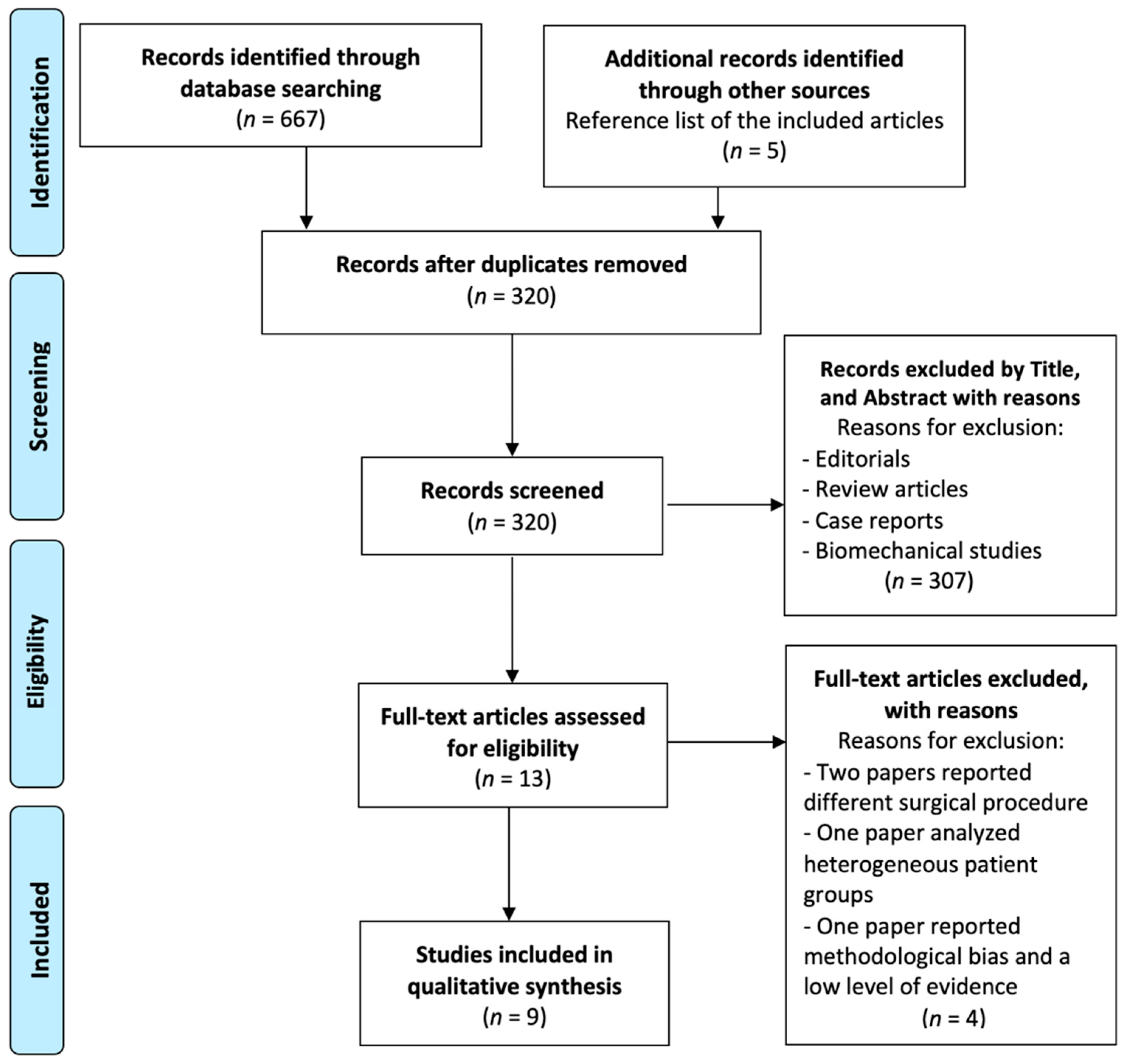
2.1. Search Strategy and Selection Criteria
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Extraction
2.4. Primary and Secondary Outcomes
2.5. Assessment of Study Quality
2.6. Statistical Analysis
3. Results
3.1. Demographics, Survivorship, and Reasons for Revision
3.2. Complications, Reoperations and Revisions
3.3. Causes of Reoperations
3.4. Patient-Reported Outcome Measures (PROMs)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kurtz, S.M.; Ong, K.L.; Lau, E.; Bozic, K.J. Impact of the economic downturn on total joint replacement demand in the United States: Updated projections to 2021. J. Bone Jt. Surg. Am. 2014, 96, 624–630. [Google Scholar] [CrossRef]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Sun, W.; Yuwen, P.; Yang, X.; Chen, W.; Zhang, Y. Changes in epidemiological characteristics of knee arthroplasty in eastern, northern and central China between 2011 and 2020. J. Orthop. Surg. Res. 2023, 18, 104. [Google Scholar] [CrossRef] [PubMed]
- Siviero, P.; Marseglia, A.; Biz, C.; Rovini, A.; Ruggieri, P.; Nardacchione, R.; Maggi, S. Quality of life outcomes in patients undergoing knee replacement surgery: Longitudinal findings from the QPro-Gin study. BMC Musculoskelet. Disord. 2020, 21, 436. [Google Scholar] [CrossRef] [PubMed]
- Piolanti, N.; Polloni, S.; Bonicoli, E.; Giuntoli, M.; Scaglione, M.; Indelli, P.F. Giovanni Alfonso Borelli: The Precursor of Medial Pivot Concept in Knee Biomechanics. Joints 2018, 6, 167–172. [Google Scholar] [CrossRef]
- Schmidt, R.; Ogden, S.; Blaha, J.D.; Alexander, A.; Fitch, D.A.; Barnes, C.L. Midterm clinical and radiographic results of the medial pivot total knee system. Int. Orthop. 2014, 38, 2495–2498. [Google Scholar] [CrossRef]
- Dennis, D.A.; Komistek, R.D.; Colwell, C.E., Jr.; Ranawat, C.S.; Scott, R.D.; Thornhill, T.S.; Lapp, M.A. In vivo anteroposterior femorotibial translation of total knee arthroplasty: A multicenter analysis. Clin. Orthop. Relat. Res. 1998, 356, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Pinskerova, V.; Samuelson, K.M.; Stammers, J.; Maruthainar, K.; Sosna, A.; Freeman, M.A. The knee in full flexion: An anatomical study. J. Bone Jt. Surg. Br. 2009, 91, 830–834. [Google Scholar] [CrossRef]
- Freeman, M.A.; Pinskerova, V. The movement of the normal tibio-femoral joint. J. Biomech. 2005, 38, 197–208. [Google Scholar] [CrossRef]
- Giustra, F.; Bistolfi, A.; Bosco, F.; Fresia, N.; Sabatini, L.; Berchialla, P.; Sciannameo, V.; Massè, A. Highly cross-linked polyethylene versus conventional polyethylene in primary total knee arthroplasty: Comparable clinical and radiological results at a 10-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1082–1088. [Google Scholar] [CrossRef]
- Cacciola, G.; De Martino, I.; De Meo, F. Does the medial pivot knee improve the clinical and radiographic outcome of total knee arthroplasty? A single centre study on two hundred and ninety seven patients. Int. Orthop. 2020, 44, 291–299. [Google Scholar] [CrossRef]
- Cacciola, G.; Mancino, F.; De Meo, F.; Bruschetta, A.; De Martino, I.; Cavaliere, P. Current Reconstruction Options in Periprosthetic Fractures around the Knee. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 21514593211023996. [Google Scholar] [CrossRef]
- Giustra, F.; Bosco, F.; Cacciola, G.; Risitano, S.; Capella, M.; Bistolfi, A.; Massè, A.; Sabatini, L. No Significant Differences in Clinical and Radiographic Outcomes between PCL Retained or Sacrificed Kinematic Aligned Medial Pivot Total Knee Arthroplasty in Varus Knee. J. Clin. Med. 2022, 11, 6569. [Google Scholar] [CrossRef]
- Xu, Z.; Tian, S.; Zhou, X.; Wei, Y.; Wu, C.; Jia, X.; Wang, H. Medial Pivot versus Posterior-Stabilized Prosthesis Design in Primary Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Indian J. Orthop. 2022, 56, 1506–1524. [Google Scholar] [CrossRef] [PubMed]
- Risitano, S.; Cacciola, G.; Capella, M.; Bosco, F.; Giustra, F.; Fusini, F.; Indelli, P.F.; Massé, A.; Sabatini, L. Comparison between gaits after a medial pivot and posterior stabilized primary total knee arthroplasty: A systematic review of the literature. Arthroplasty 2023, 5, 15. [Google Scholar] [CrossRef]
- Kato, M.; Warashina, H.; Mitamura, S.; Kataoka, A. Medial pivot-based total knee arthroplasty achieves better clinical outcomes than posterior-stabilised total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 998–1010. [Google Scholar] [CrossRef]
- Negrín, R.; Ferrer, G.; Iñiguez, M.; Duboy, J.; Saavedra, M.; Larraín, N.R.; Jabes, N.; Barahona, M. Robotic-assisted surgery in medial unicompartmental knee arthroplasty: Does it improve the precision of the surgery and its clinical outcomes? Systematic review. J. Robot. Surg. 2021, 15, 165–177. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.D.; Quatman, C.E.; Manring, M.M.; Siston, R.A.; Flanigan, D.C. How to write a systematic review. Am. J. Sports Med. 2014, 42, 2761–2768. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, J.M.; Bubra, P.S.; Walker, P.; Walsh, W.R.; Bruce, W.J. Midterm results using a medial pivot total knee replacement compared with the Australian National Joint Replacement Registry data. ANZ J. Surg. 2014, 84, 172–176. [Google Scholar] [CrossRef]
- Nakamura, S.; Minoda, Y.; Nakagawa, S.; Kadoya, Y.; Takemura, S.; Kobayashi, A.; Mizokawa, S.; Ohta, Y.; Takahashi, S.; Yamamura, K.; et al. Clinical results of alumina medial pivot total knee arthroplasty at a minimum follow-up of 10 years. Knee 2017, 24, 434–438. [Google Scholar] [CrossRef]
- Karachalios, T.; Varitimidis, S.; Bargiotas, K.; Hantes, M.; Roidis, N.; Malizos, K.N. An 11- to 15-year clinical outcome study of the Advance Medial Pivot total knee arthroplasty: Pivot knee arthroplasty. Bone Jt. J. 2016, 98, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Park, J.W.; Kim, J.S. Clinical Outcome of Medial Pivot Compared With Press-Fit Condylar Sigma Cruciate-Retaining Mobile-Bearing Total Knee Arthroplasty. J. Arthroplast. 2017, 32, 3016–3023. [Google Scholar] [CrossRef] [PubMed]
- Macheras, G.A.; Galanakos, S.P.; Lepetsos, P.; Anastasopoulos, P.P.; Papadakis, S.A. A long term clinical outcome of the Medial Pivot Knee Arthroplasty System. Knee 2017, 24, 447–453. [Google Scholar] [CrossRef]
- Dehl, M.; Bulaïd, Y.; Chelli, M.; Belhaouane, R.; Gabrion, A.; Havet, E.; Mertl, P. Total knee arthroplasty with the Medial-Pivot knee system: Clinical and radiological outcomes at 9.5 years’ mean follow-up. Orthop. Traumatol. Surg. Res. 2018, 104, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Karachalios, T.; Komnos, G.; Amprazis, V.; Antoniou, I.; Athanaselis, S. A 9-Year Outcome Study Comparing Cancellous Titanium-Coated Cementless to Cemented Tibial Components of a Single Knee Arthroplasty Design. J. Arthroplast. 2018, 33, 3672–3677. [Google Scholar] [CrossRef]
- Jenny, J.Y.; Bercovy, M.; Cazenave, A.; Gaillard, T.; Châtain, F.; Jolles, B.E.; Rouvillain, J.L.; Saragaglia, D.; French Society for Hip and Knee Surgery (SFHG). No difference in 13-year survival after medial pivot or central pivot mobile bearing total knee arthroplasty. A propensity matched comparative analysis. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3648–3653. [Google Scholar] [CrossRef]
- Ueyama, H.; Kanemoto, N.; Minoda, Y.; Yamamoto, N.; Taniguchi, Y.; Nakamura, H. No Difference in Postoperative Knee Flexion and Patient Joint Awareness Between Cruciate-Substituting and Cruciate-Retaining Medial Pivot Total Knee Prostheses: A 10-Year Follow-Up Study. J. Arthroplast. 2022, 37, 279–285. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, Y.; Kwong, J.S.; Zhang, C.; Li, S.; Sun, F.; Niu, Y.; Du, L. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid. Based Med. 2015, 8, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Bruschetta, D.; Anastasi, G.; Andronaco, V.; Cascio, F.; Rizzo, G.; Di Mauro, D.; Bonanno, L.; Izzo, V.; Buda, D.; Vermiglio, G.; et al. Human calf muscles changes after strength training as revealed by diffusion tensor imaging. J. Sports Med. Phys. Fit. 2019, 59, 853–860. [Google Scholar] [CrossRef]
- Fitch, D.A.; Sedacki, K.; Yang, Y. Mid- to long-term outcomes of a medial-pivot system for primary total knee replacement: A systematic review and meta-analysis. Bone Jt. Res. 2014, 3, 297–304. [Google Scholar] [CrossRef]
- Cacciola, G.; Mancino, F.; De Meo, F.; Di Matteo, V.; Sculco, P.K.; Cavaliere, P.; Maccauro, G.; De Martino, I. Mid-term survivorship and clinical outcomes of the medial stabilized systems in primary total knee arthroplasty: A systematic review. J. Orthop. 2021, 24, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, Y.; Li, B.; Wang, L.; Wang, Y.; Liu, J. Comparison of the clinical and patient-reported outcomes between medial stabilized and posterior stabilized total knee arthroplasty: A systematic review and meta-analysis. Knee 2022, 36, 9–19. [Google Scholar] [CrossRef]
- Kakoulidis, P.; Panagiotidou, S.; Profitiliotis, G.; Papavasiliou, K.; Tsiridis, E.; Topalis, C. Medial pivot design does not yield superior results compared to posterior-stabilised total knee arthroplasty: A systematic review and meta-analysis of randomised control trials. Knee Surg. Sports Traumatol. Arthrosc. 2022. [Google Scholar] [CrossRef] [PubMed]
- Batra, S.; Malhotra, R.; Kumar, V.; Srivastava, D.N.; Backstein, D.; Pandit, H. Superior patient satisfaction in medial pivot as compared to posterior stabilized total knee arthroplasty: A prospective randomized study. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3633–3640. [Google Scholar] [CrossRef]
- Nisar, S.; Ahmad, K.; Palan, J.; Pandit, H.; van Duren, B. Medial stabilised total knee arthroplasty achieves comparable clinical outcomes when compared to other TKA designs: A systematic review and meta-analysis of the current literature. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 638–651. [Google Scholar] [CrossRef]
- Sartawi, M.; Zurakowski, D.; Rosenberg, A. Implant Survivorship and Complication Rates after Total Knee Arthroplasty with a Third-Generation Cemented System: 15-Year Follow-Up. Am. J. Orthop. 2018, 47. [Google Scholar] [CrossRef]
- Meftah, M.; White, P.B.; Ranawat, A.S.; Ranawat, C.S. Long-term results of total knee arthroplasty in young and active patients with posterior stabilized design. Knee 2016, 23, 318–321. [Google Scholar] [CrossRef]
- Hegde, V.; Stambough, J.B.; Levine, B.R.; Springer, B.D. Highlights of the 2022 American Joint Replacement Registry Annual Report. Arthroplast. Today 2023, 21, 101137. [Google Scholar] [CrossRef]
- Blaha, J.D. The rationale for a total knee implant that confers anteroposterior stability throughout range of motion. J. Arthroplast. 2004, 19 (Suppl. S1), 22–26. [Google Scholar] [CrossRef]
- Ben-Shlomo, Y.; Blom, A.; Boulton, C.; Brittain, R.; Clark, E.; Dawson-Bowling, S.; Deere, K.; Esler, C.; Espinoza, O.; Evans, J.; et al. The National Joint Registry 19th Annual Report 2022; National Joint Registry: London, UK, 2022. [Google Scholar]
- Miyazaki, Y.; Nakamura, T.; Kogame, K.; Saito, M.; Yamamoto, K.; Suguro, T. Analysis of the kinematics of total knee prostheses with a medial pivot design. J. Arthroplast. 2011, 26, 1038–1044. [Google Scholar] [CrossRef]
- Nishio, Y.; Onodera, T.; Kasahara, Y.; Takahashi, D.; Iwasaki, N.; Majima, T. Intraoperative medial pivot affects deep knee flexion angle and patient-reported outcomes after total knee arthroplasty. J. Arthroplast. 2014, 29, 702–706. [Google Scholar] [CrossRef]
- Fan, C.Y.; Hsieh, J.T.; Hsieh, M.S.; Shih, Y.C.; Lee, C.H. Primitive results after medial-pivot knee arthroplasties: A minimum 5-year follow-up study. J. Arthroplast. 2010, 25, 492–496. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Lee, K.W.; Kim, C.H.; Ahn, H.S.; Hwang, J.K.; Kang, J.H.; Han, H.D.; Cho, W.J.; Park, J.S. Long-term Results of Hybrid Total Knee Arthroplasty: Minimum 10-years Follow-up. Knee Surg. Relat. Res. 2012, 24, 79–84. [Google Scholar] [CrossRef]
- Varadarajan, K.M.; Moynihan, A.L.; D’Lima, D.; Colwell, C.W.; Li, G. In vivo contact kinematics and contact forces of the knee after total knee arthroplasty during dynamic weight-bearing activities. J. Biomech. 2008, 41, 2159–2168. [Google Scholar] [CrossRef] [PubMed]
- Deckard, E.R.; Ziemba-Davis, M.; Meneghini, R.M. Tibiofemoral Contact Forces Influence Intraoperative Kinematic Pivot Pattern Dependent on Posterior Cruciate Ligament Resection in Primary Total Knee Arthroplasty. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2022, 6, e22.00033. [Google Scholar] [CrossRef]
- Sabatini, L.; Bosco, F.; Barberis, L.; Camazzola, D.; Bistolfi, A.; Risitano, S.; Massè, A.; Indelli, P.F. Kinetic Sensors for Ligament Balance and Kinematic Evaluation in Anatomic Bi-Cruciate Stabilized Total Knee Arthroplasty. Sensors 2021, 21, 5427. [Google Scholar] [CrossRef]
- Longo, U.G.; Ciuffreda, M.; Mannering, N.; D’Andrea, V.; Locher, J.; Salvatore, G.; Denaro, V. Outcomes of Posterior-Stabilized Compared with Cruciate-Retaining Total Knee Arthroplasty. J. Knee Surg. 2018, 31, 321–340. [Google Scholar] [CrossRef] [PubMed]
- Boettner, F.; Sculco, P.; Faschingbauer, M.; Rueckl, K.; Windhager, R.; Kasparek, M.F. Clinical outcome of posterior-stabilized total knee arthroplasty using an increased flexion gap in patients with preoperative stiffness. Bone Jt. J. 2020, 102, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Muneta, T.; Koga, H.; Horie, M.; Nakamura, T.; Otabe, K.; Nakagawa, Y.; Katakura, M.; Sekiya, I. In-vivo kinematics of high-flex posterior-stabilized total knee prosthesis designed for Asian populations. Int. Orthop. 2016, 40, 2295–2302. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Yoon, S.H.; Kim, J.S. Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin. Orthop. Relat. Res. 2009, 467, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Kulshrestha, V.; Sood, M.; Kanade, S.; Kumar, S.; Datta, B.; Mittal, G. Early Outcomes of Medial Pivot Total Knee Arthroplasty Compared to Posterior-Stabilized Design: A Randomized Controlled Trial. Clin. Orthop. Surg. 2020, 12, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Zou, D.; Zhang, X.; Zheng, N.; Pan, Y.; Ling, Z.; Tsai, T.Y.; Chen, Y. Loss of Knee Flexion and Femoral Rollback of the Medial-Pivot and Posterior-Stabilized Total Knee Arthroplasty during Early-Stance of Walking in Chinese Patients. Front. Bioeng. Biotechnol. 2021, 9, 675093. [Google Scholar] [CrossRef]

| Authors (Year of Publication) | Study Design (LoE) | N of Knees Initial/Final | N of Knee Died/Lost to Follow-Up | Male/Female Ratio | Mean Age at the Time of Surgery; (Years Old) | Mean Follow-Up (Years) |
|---|---|---|---|---|---|---|
| N/N | N/N | N/N | Mean ± SD (Range) | Mean ± SD (Range) | ||
| Brinkman et al. (2013) [21] | Prospective (III) | 50/45 | 5/0 | 35/15 | 69 (45 to 82) | 9.96 (1.7 to 14) |
| Nakamura et al. (2016) [22] | Retrospective (IV) | 107/70 | 23/14 | 5/102 | 72 (45 to 85) | 11.1 (19 to 13) |
| Karachalios et al. (2016) [23] | Retrospective (IV) | 284/251 | 20/10 | 41/184 | 71 (52 to 84) | 13.4 (11 to 15) |
| Kim et al. (2016) [24] | Prospective (IV) | 195/182 | 5/8 | 52/130 | 65.6 (55 to 79) | 11 (11 to 12.6) |
| Macheras et al. (2017) [25] | Retrospective (IV) | 385/347 | 11/14 | 125/225 | 78 (58 to 86) | 15.2 (15 to 17) |
| Dehl et al. (2017) [26] | Retrospective (IV) | 74/50 | 9/15 | 13/35 | 66.8 (38 to 83) | 9.5 (7.7 to 11) |
| Karachalios et al. (2018) [27] | Prospective (III) | 54/54 | 0/0 | 18/36 | 63.2 (52 to 70) | 8.6 (8 to 9) |
| Jenny et al. (2020) [28] | Retrospective (IV) | 577/336 | 109/132 | 138/198 | 70.1 ± 7.2 | 13 (10 to 15) |
| Ueyama et al. (2020) [29] | Retrospective (IV) | 283/257 | 14/12 | 16/241 | 76.2 ± 7.3 | 10.1 ± 1.7 |
| Overall | 2009/1592 | 192/221 | 27.5%/72.5% | 71.9 | 12.6 |
| Authors (Year of Publication) | MP-TKA Design Used | PCL Retained/ Sacrificed | Patella Resurfacing/ Not Resurfacing |
|---|---|---|---|
| N/N | N/N | ||
| Brinkman et al. (2013) [21] | Advance MP (MicroPort) | 27/23 | 42/8 |
| Nakamura et al. (2016) [22] | MPK (Kyocera Corporation) | 0/107 | 107/0 |
| Karachalios et al. (2016) [23] | Advance MP (MicroPort) | 207/77 | 0/284 |
| Kim et al. (2016) [24] | Advance MP (MicroPort) | 0/182 | 182/0 |
| Macheras et al. (2017) [25] | Advance MP (MicroPort) | 205/180 | 0/285 |
| Dehl et al. (2017) [26] | Advance MP (MicroPort) | 0/50 | 40/10 |
| Karachalios et al. (2018) [27] | Advance MP (MicroPort) | NS | 0/54 |
| Jenny et al. (2020) [28] | Aesculap MP (B.Braun) | NS | NS |
| Ueyama et al. (2020) [29] | Advance MP (MicroPort) | 0/257 | 257/0 |
| Overall | 33.4%/66.6% | 49.5%/50.5% |
| Authors (Year of Publication) | N of Knees | AL | PPF | PJI | KI | AKP | PF | AF | CM | IW | DVP/ PE | Wound Dehiscence or Postoperative Effusion | Overall Complications | Overall Reoperations | Overall Revisions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Brinkman et al. (2013) [21] | 45 | 0 (0%) | 1 (2.2%) | 1 (2.2%) | 0 (0%) | 0 (0%) | 1 (2.2%) | 7 (15.6%) | 0 (0%) | 0 (0%) | 2/0 (4.4%) | 0 (0%) | 12 (26.7%) | 3 (6.7%) | 1 (2.2%) |
| Nakamura et al. (2016) [22] | 70 | 0 (0%) | 1 + 1 (2.9%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0/0 (0%) | 1 (1.4%) | 3 (17.1%) | 3 (4.3%) | 1 (1.4%) |
| Karachalios et al. (2016) [23] | 251 | 3 (1.2%) | 0 (0%) | 2 (0.8%) | 1 (0.4%) | 2 + 10 (4.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0/0 (0%) | 0 (0%) | 18 (4.8%) | 8 (3.2%) | 8 (3.2%) |
| Kim et al. (2016) [24] | 182 | 0 (0%) | 0 (0%) | 2 + 5 (3.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0/0 (0%) | 17 (9.3%) | 24 (6.6%) | 7 (3.8%) | 2 (1.1%) |
| Macheras et al. (2017) [25] | 347 | 0 (0%) | 1 (0.3%) | 0 (0%) | 0 (0%) | 3 (0.9%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2/2 (1.2%) | 7 (2%) | 15 (3.5%) | 4 (1.2%) | 4 (1.2%) |
| Dehl et al. (2017) [26] | 50 | 0 (0%) | 1 (2%) | 1 (2%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (2%) | 1 (2%) | 0 (0%) | 0/0 (0%) | 0 (0%) | 4 (25%) | 4 (8%) | 3 (6%) |
| Karachalios et al. (2018) [27] | 54 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (5.6%) | 0 (0%) | 1 + 2 (5.6%) | 0 (0%) | 0 (0%) | 0/1 (1.9%) | 2 (3.7%) | 9 (22.2%) | 0 (0%) | 0 (0%) |
| Jenny et al. (2020) [28] | 336 | 4 (1.2%) | 0 (0%) | 0 (0%) | 2 + 2 (1.2%) | 0 (0%) | 0 (0%) | 1 (0.3%) | 0 (0%) | 1 (0.3%) | 0/0 (0%) | 0 (0%) | 10 (3.6%) | 10 (3%) | 7 (2.1%) |
| Ueyama et al. (2020) [29] | 257 | 0 (0%) | 1 + 2 (1.2%) | 2 (0.8%) | 1 + 3 (1.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0/0 (0%) | 1 (0.4%) | 10 (4.7%) | 10 (3.9%) | 4 (1.6%) |
| Overall | 1592 | 7 (0.4%) | 4 + 4 (0.5%) | 7 + 6 (0.8%) | 4 + 5 (0.6%) | 5 + 13 (1.1%) | 1 (0.06%) | 1 + 1 + 10 (0.7%) | 1 (0.06%) | 1 (0.06%) | 4/3 (0.4%) | 2 + 26 (1.8%) | 105 (6.6%) | 49 (3.1%) | 29 (1.8%) |
| PROMs | N of Studies/ Knees | N of Knees | Preoperative | Postoperative | Delta Pre-Postoperative |
|---|---|---|---|---|---|
| N/N | N | ||||
| KSS knee score [21,22,23,24,25,26,27,28,29] | 9/1592 | 1592 | 32.8 | 88.1 | 55.3 |
| KSS function score [21,22,23,24,25,26,27,28,29] | 8/1492 | 1492 | 42.6 | 78.5 | 35.9 |
| WOMAC [21,23,24,25,27] | 5/870 | 870 | 37.2 | 61.1 | 23.9 |
| OKS [23,25,27] | 3/652 | 652 | 23.2 | 44.5 | 21.3 |
| ROM knee flexion (°) [21,22,24,25,26,29] | 6/951 | 951 | 103.2 | 117.6 | 14.4 |
| SF-12 PCS [23,25,27] | 3/652 | 652 | 25.8 | 47.1 | 21.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cacciola, G.; Giustra, F.; Bosco, F.; Sabatini, L.; Risitano, S.; De Meo, F.; Braconi, L.; Cavaliere, P.; Massè, A.; Solarino, G. Long-Term Follow-Up of Medial Pivot Total Knee Arthroplasty: A Systematic Review of the Current Evidence. Prosthesis 2023, 5, 622-634. https://doi.org/10.3390/prosthesis5030044
Cacciola G, Giustra F, Bosco F, Sabatini L, Risitano S, De Meo F, Braconi L, Cavaliere P, Massè A, Solarino G. Long-Term Follow-Up of Medial Pivot Total Knee Arthroplasty: A Systematic Review of the Current Evidence. Prosthesis. 2023; 5(3):622-634. https://doi.org/10.3390/prosthesis5030044
Chicago/Turabian StyleCacciola, Giorgio, Fortunato Giustra, Francesco Bosco, Luigi Sabatini, Salvatore Risitano, Federico De Meo, Lorenzo Braconi, Pietro Cavaliere, Alessandro Massè, and Giuseppe Solarino. 2023. "Long-Term Follow-Up of Medial Pivot Total Knee Arthroplasty: A Systematic Review of the Current Evidence" Prosthesis 5, no. 3: 622-634. https://doi.org/10.3390/prosthesis5030044
APA StyleCacciola, G., Giustra, F., Bosco, F., Sabatini, L., Risitano, S., De Meo, F., Braconi, L., Cavaliere, P., Massè, A., & Solarino, G. (2023). Long-Term Follow-Up of Medial Pivot Total Knee Arthroplasty: A Systematic Review of the Current Evidence. Prosthesis, 5(3), 622-634. https://doi.org/10.3390/prosthesis5030044








