Abstract
Today, older adults are routinely classified into different categories based on their degrees of independence. However, due to the extreme heterogeneity of this group, and the fact that ageing is a progressive process, older adults may require customized prosthetic treatment. Older people, during ageing, may quickly pass into a frail condition, with loss of independence and of the manual skills necessary for proper hygiene maintenance. With this in mind, complete arch rehabilitations can make an important contribution to a patient’s quality of life. New treatment strategies are needed which take into account the priorities of ageing. The aim of this case report is to show an adaptable prosthetic treatment protocol that is useful for older adults. This protocol provides individual satisfaction and also aids forecasting of the patient’s future functional and maintenance needs.
1. Introduction
Life expectancy is progressively rising worldwide, especially in developed countries [1]. This phenomenon highlights the social and medical advances of the last century, but also raises new challenges in relation to the diseases and disabilities which affect older people [2]. Among older adults (>60 years old) the prevalence of severe edentulism (less than nine teeth) quickly increases during the seventh decade, with a peak rate of increase at 65 years [3]. This condition may impair the health, social status, and psychological status of individuals; thus, it requires improvements in preventive and treatment modalities. In some studies, edentulism has been associated with higher rates of mortality (RR = 1.66, 95%CI 1.46–1.88), especially due to cardiovascular and pulmonary diseases [4].
In addition, the older adult population can be understood as including a wide range of ages, involving different challenges to health at different ages. From this perspective, Ettinger and Beck proposed a classification based on the degree of independence enjoyed by people older than 65 years. In this classification, older adults were divided into three groups, namely, functionally independent, frail, and functionally dependent [5].
With regard to patient perception, implant-supported rehabilitations can significantly improve patient-centered outcomes (PCOs) when compared with conventional complete dentures [6,7]. Furthermore, a systematic review assessing PCOs found insufficient evidence to claim the superiority of fixed implant-supported restorations over overdentures [8]. These results can be easily expressed in terms of the Ettinger and Beck classification; overdentures are perceived as easier to clean and therefore more suitable for frail older adults, whose dexterity can be partially impaired [9]. The absence of adequate oral hygiene procedures can also promote plaque accumulation and thus the onset of peri-implant diseases, jeopardizing implant survival and rehabilitation management [10]. Consequently, both primary and secondary prevention of peri-implant disease are necessary to avoid functional and biological failure in frail patients [11]. In addition, oral inflammation can have an impact on systemic disease control (e.g., diabetes and cardiovascular disease). This highlights the need for new oral health restoration strategies that take into account the different priorities associated with ageing [12]. Because ageing is a progressive process, individuals may quickly pass into a frail condition, losing independence and the ability to hygienically maintain a long-term rehabilitation [13].
In this regard, any treatment plan for older patients willing to restore a fixed dentition should take into account the ageing process and allow for easier adjustment if and when such patients subsequently experience an ageing-related impairment. In simple terms, the clinician should accurately plan the number and the location of dental implants to allow for the future rehabilitation of both fixed and removable prosthetics in a feasible manner by forecasting the patient’s likely reduction in independence and allowing for short treatment times in the re-intervention stage.
The aim of the current case report is to show an adaptable treatment protocol for older adults that provides individual satisfaction and also helps to pinpoint the future functional and maintenance needs of the patient. The presented method highlights the value of the prototype, which can help clinicians to validate the digital project. Moreover, photographs, Intra Oral Scanner (IOS), and a virtual articulator can facilitate and speed up this procedure. To this end, a single clinical case is described in detail, so that the main conceptual elements of the protocol can be understood.
2. Materials and Methods
A 70-year-old man came to the dental office complaining about mobility issues with his upper jaw prosthetic rehabilitation. The patient did not suffer from any systemic disease or infection and he reported good general health; he was, therefore, classified as ASA1 according to the American Society of Anesthesiologists Classification [14]. Oral anamnesis revealed previous dental treatments intended to recover and replace elements mainly affected by dental caries. The lower jaw presented a complete removable implant-supported restoration in good state with neither tissue discrepancy nor peri-implant disease. In the upper jaw, a Class I Kennedy edentulism [15] treated with a combined prosthetic solution was found (Figure 1). Clinical examination together with radiographic images revealed a hopeless dental condition, which required a complete remake of the upper jaw prosthesis. The patient requested a fixed prosthesis, so the treatment plan could rely only on implant-supported rehabilitation due to the absence of reliable dental support.

Figure 1.
Intra-oral frontal picture showing the patient’s initial condition.
2.1. First Step: Complete Fixed Rehabilitation
Intra-oral and extra-oral pictures together with analogic impressions and radiographic images were obtained in order to develop a treatment plan. Extra-oral examination did not reveal any asymmetry; however, oral inspection highlighted an oblique occlusal plane with centripetal atrophy of the alveolar crest on posterior maxillary sites. Radiographic exams (orthopantomography and cone beam computed tomography) revealed severely pneumatized maxillary sinuses, which ruled out conventional implant placement in the posterior sites (Figure 2). After the extractions were performed, the residual bone volume was suitable for implant-supported rehabilitation, either fixed (fixed dental prosthesis—FDP) or removable (overdenture).

Figure 2.
Radiographic image of the upper jaw at baseline.
In light of the above, two straight and two tilted implants (4 × 12.5 mm) (Spi Contact Inicell, Thommen Medical; Grechen, Switzerland) were inserted in order to comply with the All-on-4 rehabilitation protocol. Multi-unit abutments (MUAs) were screwed onto the implants as intermediate components to provide passivation for the metal superstructure (Figure 3) [16].
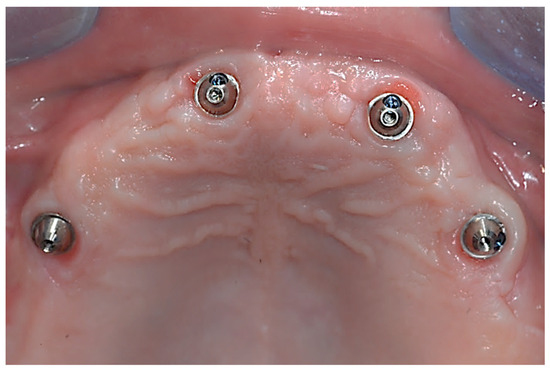
Figure 3.
Upper jaw’s implants equipped with MUAs for prosthetic passivation.
The one-model technique described by Biscaro et al. was used to transfer the implant position onto the previously articulated models [17]. An experienced technician (MO) manufactured the metal superstructure and modeled the teeth anatomy with acrylic resin according to aesthetic and occlusal requests (Figure 4). Immediate loading was performed within 48 h.

Figure 4.
Implant-supported “All-on-4” fixed dental prosthesis.
After the completion of the prosthetic rehabilitation, recalls were scheduled twice a year to perform clinical assessment and professional mechanical plaque removal [18].
2.2. Second Step: From FDP to Implant-Supported Overdenture
Ten years later, the patient came back to the dental practice experiencing severe wear of the resin components of the former prosthesis due to attrition. The patient reported a decrease in masticatory efficiency and expressed concern about aesthetic worsening caused by the resin abrasion, resulting in a reduction in vertical dimension. Besides the prosthesis wear, the only complication reported during the follow-up period was a resin fracture at the upper left lateral incisor, which was subsequently repaired. In discussions with the patient, a shift from a fixed prosthesis to an overdenture was considered, because of the ageing process and dexterity reduction.
Again, diagnostic records were assessed in order to investigate the patient’s functional and anatomical conditions. A digital workflow was applied, and the following records were obtained:
- Intra-oral impressions: an intra-oral scanner (IOS) (Trios3 v1.4.7.5, 3Shape; Copenhagen, Denmark) was used to produce a full-arch digital model of the patient’s upper and lower arches [19];
- Extra-oral photographs were taken according to the technique required by the DSS (Digital Smile System, Just-Digital; Bologna, Italy) software protocol (Figure 5) [20,21,22];
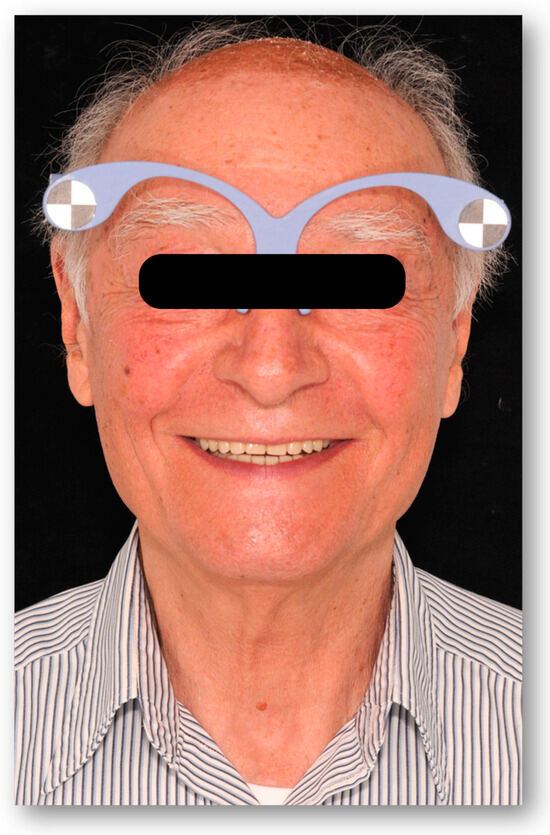 Figure 5. Extra-oral picture obtained according to the DSS procedure.
Figure 5. Extra-oral picture obtained according to the DSS procedure. - Virtual articulation of the model was performed through a digital facebow (Jaw registration JMA, Zebris Medical GmbH; Isny, Germany) [23].
The task of the clinician was to restore the patient’s masticatory function and achieve an aesthetic improvement, taking into account the ageing process and the new gnathological conditions. Clinical and radiographic examination confirmed healthy implant conditions without any bleeding site, probing depth ≥5 mm or radiographic bone loss (assessed by means of intraoral radiographs).
Following the DSS workflow, we superimposed and imported the extraoral photographs, with and without lip retractors, into the software to conduct a 2D smile analysis and design the proposed rehabilitation digitally. This process involved planning the shape and position of the teeth virtually, based on commercial teeth from the software’s databases (Figure 6). We then overlaid this digital design onto the patient’s smile picture to assess teeth exposure and communicate the final result clearly. After the patient approved the aesthetics and the treatment plan, we proceeded to produce a prototype [22].

Figure 6.
Digital plan of teeth outlines.
The final plan was sent to the digital dental technician (MO) who matched the 2D image to the articulated virtual model using dedicated CAD software (Exocad DentalCAD, Exocad Gmbh; Darmstadt, Germany) (Figure 7). This procedure allowed the technician to transfer the information derived from the digital smile software into a functional environment, where teeth shape and prosthetic space could be checked in static and dynamic occlusion [24].
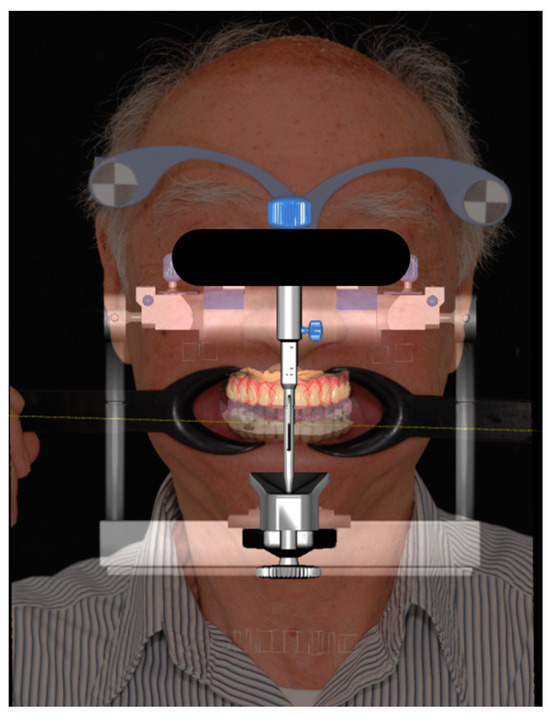
Figure 7.
Two-dimensional digital plan superimposed to the digital articulator.
The prototype was produced with a 3D printer featuring SLA 3D printing technology (Asiga MAX, Asiga; Sydney, NSW, Australia) employing PMMA resin. At this stage, the patient was recalled in order to clinically check the aesthetic and occlusion with the prototype and also to determine the implant position by means of an IOS. Firstly, four scan bodies, mounted on the MUAs, were linked together with light-cured resin: the aim was to improve global accuracy of the impression on the edentulous jaw [25,26]. Next, the resin was removed and the prototype, properly adapted over the scan bodies, was placed in the patient’s mouth for a second intra-oral scan (Figure 8) [27]; these two impressions allowed the technician to merge the information derived from the implant position in the edentulous jaw together with the prototype, resulting in a proper analysis of the spaces needed for the bar and the superstructure in a procedure called “digital cross-mounting” [28].
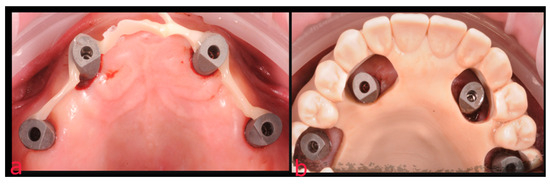
Figure 8.
Technique employed for the digital impression of the edentulous jaw: (a) scan bodies splinted with light-cured resin; (b) prototype adapted to fit together with the scan bodies.
The last step before delivery consisted in the passivation test conducted by means of an aluminum test drive produced with CAD-CAM technology; this structure was created to verify the implant position and the accuracy of the digital impressions (Figure 9).
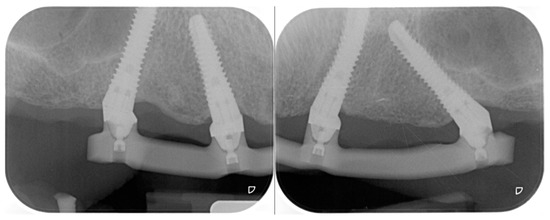
Figure 9.
Radiographic assessment of the impression’s accuracy with the aluminum test drive in place.
The bar was produced by a milling center (New Anchorvis SRL; Calderara di Reno (BO), Italy) from a chromium–cobalt disk and was therefore equipped with screwed ball attachments (Rhein 83 srl; Bologna, Italy) (Figure 10).
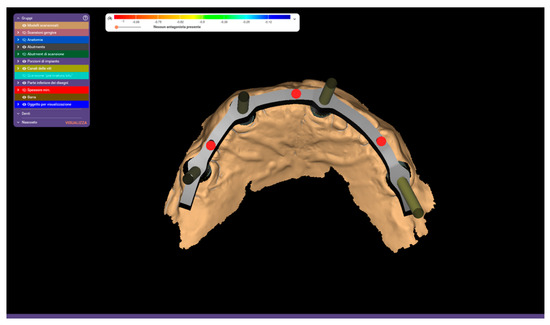
Figure 10.
CAD project for the implant-supported chromium−cobalt bar.
Next, the superstructure’s castable pattern was digitally designed and printed via SLA technology (Figure 11); a chromium–cobalt alloy was injected into a mold obtained from the pattern. Five retentive caps with their related metal housing were cemented to the superstructure to provide a retentive component on the removable prosthesis.
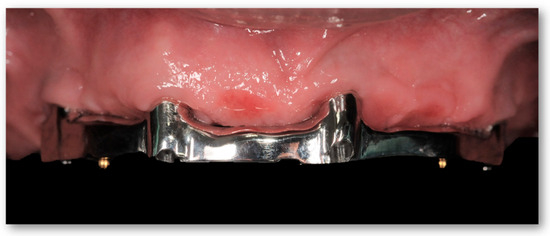
Figure 11.
Metal bar screwed onto the MUAs and equipped with ball attachments.
Passive fit of the metal bar was verified with clinical and radiographic tests (Figure 12).
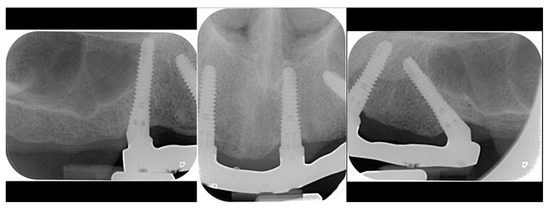
Figure 12.
Radiographic fit assessment of the metal bar.
Once the bar and the superstructure were completed, the technician finalized the overdenture by replicating the prototype’s teeth positions (Figure 13). In order to transfer teeth position on the prosthesis, resin models were 3D printed based on the recorded maxillomandibular relationship and were then placed on an analogue articulator to perform the mounting. An acrylic resin flange was subsequently cast over the removable superstructure.

Figure 13.
Digitally designed superstructure taking teeth planned volumes into account.
Finally, before prosthesis delivery, the aesthetic and function were clinically checked. Individually tailored oral hygiene instructions were then given to the patient (Figure 14).

Figure 14.
Final aspect of the overdenture before delivery.
Clinical and laboratory steps were summarized in Figure 15.
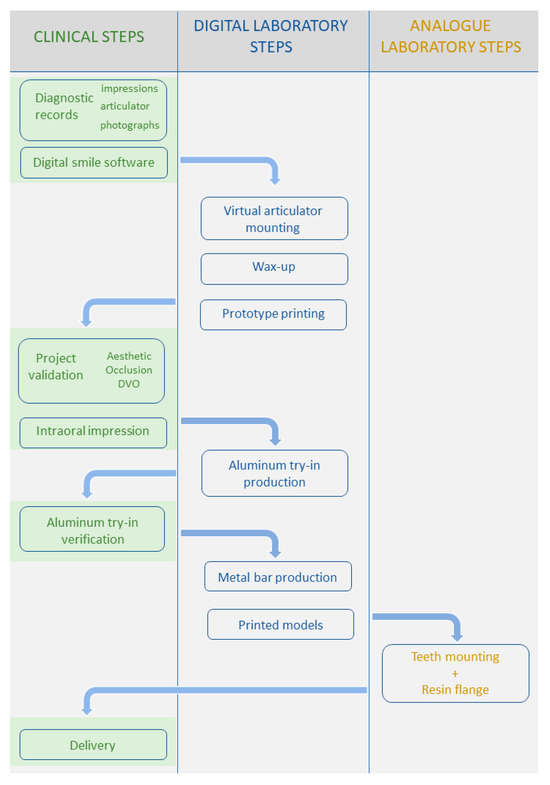
Figure 15.
Flow chart of the treatment steps.
3. Discussion
According to the World Health Organization, the global population of individuals aged 60 years and older will double from 1 billion in 2019 to 2.1 billion in 2050 [29]. Ageing is a major issue for modern societies, and the provision of age-friendly environments and improved social and healthcare facilities is recommended to promote healthier—as well as longer—human lives. Primary and secondary prevention of diseases must be implemented to allow the easier management of this population cohort; however, epidemiological data suggest that such an outcome is far from being achieved [30]. Caries and periodontitis are two of the most prevalent pathologies worldwide, and tooth loss is their ultimate sequela. This condition creates several imbalances such as loss of vertical dimension, increase in masticatory muscle tone, and decreases in both biting force and masticatory efficiency, leading to nutritional, anatomical, and aesthetical impairments [13]. A recent cross-sectional study investigated the nutritional status of 1325 community-living older adults (>75 years old); the authors showed that the complexity of patients’ care needs was correlated with the risk of suffering malnutrition, and that these patients were more likely to report chewing difficulties [31]. However, patients with dependency and functional limitation lack the ability to self-report prosthetic quality (related to stability, cleanability, and occlusion) [32], which means that trained nurses, together with regular check-ups, could be necessary in order to maintain a healthy condition. In this regard, the case report presented here suggests that prosthetic features should be adapted to the patient’s age and general health condition. The All-on-4 protocol has been validated both on maxillary and mandibular arches, allowing for a predictable treatment plan for FDP [33]. The management of such rehabilitation requires the strict control of a patient’s oral health as well as the use of reliable techniques and materials [11]. The primary prevention of biological complications around implants plays a pivotal role in achieving the long-term success of implant-supported prostheses, especially when prosthetic frameworks rely on only a small number of dental implants, as in the All-on-4 procedure. Long-term implant survival rates have been widely demonstrated [34] and satisfying results have been achieved with full-arch rehabilitations [35]. Older adults could benefit from the conversion from a fixed solution to a removable one, resulting in improved access to oral hygiene procedures with minimal decrease in quality of life [36]. In fact, despite being comparable for PCOs, there is a tendency to perceive the overdentures as more cleansable compared to FDPs [8]. Zitzmann et al. compared patients’ perspectives when fixed or removable implant-supported restorations were used in the edentulous maxilla, finding no statistically significant difference in the patient’s denture assessments between the two groups [37]. With regard to masticatory performance, this was significantly reduced when implant-supported FDPs were compared with natural dentition [38]. However, when the color-mixing analysis test was used to compare the masticatory performance of conventional complete dentures and implant-supported rehabilitations, the implant-supported rehabilitations performed better; nevertheless, there are no data supporting the greater efficacy of the fixed over removable implant-supported prostheses [39]. In a cross-over study, Feine et al. examined the masticatory function of 15 participants using standard-sized test foods. Both types of implant-supported rehabilitations (FDP and overdenture) were assessed, and no statistical differences were found between the two groups [40]. These findings support the choice taken in the present case report to switch from a fixed rehabilitation to a bar-supported overdenture, which is unlikely to affect the quality of an older patient’s food comminution.
The current article demonstrates how the Interaction between different devices together with accurate planning can achieve a digital workflow allowing treatment time reduction and accurate management of functional and aesthetic features. During the first visit, extraoral pictures were taken and used to create an aesthetic plan. This plan was discussed with the patient and modified according to his preferences. Then, the relevant information was sent to the laboratory to make a personalized prototype. This step reduces the risk of subsequent modifications and clearly guides the technician in the project. Using the aesthetic outlines designed by the clinician, together with a dynamic assessment of mandibular movements, made it possible to design a digital wax up with properly adapted occlusal contacts, cusp inclinations, and anterior determinants. This planning phase resulted in a printed prototype resembling the digital wax up that aimed to clinically verify the acquired records. Once the prototype was printed, its appearance, phonetics and function could be quickly checked at the same visit. This means fewer appointments were needed.
Monaco et al. had already described a prototype to verify aesthetic, functional movements and implant position in order to make an FDP [41]. However, in the current case report, the treatment target was to switch from an FDP to a bar-supported overdenture, and it was therefore necessary to schedule another appointment in order to check the accuracy of the implant position before construction of the final restoration.
Finally, the digital workflow employed in the present case report may improve communication with the patient and reduce procedure discomfort. A recent systematic review showed that the use of intra-oral scanners (IOSs) leads to lower levels of nausea, pain, and discomfort compared with the conventional impression technique [42]. This intrinsic characteristic of the IOS, together with pre-visualization tools, can positively affect the patient’s acceptance. Indeed, digital smile software, in addition to its diagnostic benefits, can also be employed to approximate the aesthetic final result, and thus provide an effective way to communicate with the patient.
4. Conclusions
Due to the increasing older and frail population, prosthodontic strategies must follow global trends by adapting their protocols to demographic and socioeconomic conditions. The present case report takes advantage of new technologies, while taking future maintenance intervention into account, and finds them suitable for use in addressing the needs of frail older adults.
Author Contributions
Conceptualization, L.O.; methodology, L.O.; software, M.O. and C.B.; writing—original draft preparation, R.M.; writing—review and editing, R.M.; supervision, T.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The IRB approval was not required for this Case Report, since we did not test any experimental technique, in accordance with relevant legislation “artt. 10 e 320 cod.civ.” and “artt. 96 e 97 legge 22.4.1941, n. 633”.
Informed Consent Statement
Written informed consent was obtained from the patient to publish this paper.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Correction Statement
This article has been republished with a minor correction to the Institutional Review Board Statement. This change does not affect the scientific content of the article.
References
- Kontis, V.; Bennett, J.E.; Mathers, C.D.; Li, G.; Foreman, K.; Ezzati, M. Future Life Expectancy in 35 Industrialised Countries: Projections with a Bayesian Model Ensemble. Lancet 2017, 389, 1323–1335. [Google Scholar] [CrossRef] [PubMed]
- Meyer, A.C.; Drefahl, S.; Ahlbom, A.; Lambe, M.; Modig, K. Trends in Life Expectancy: Did the Gap between the Healthy and the Ill Widen or Close? BMC Med. 2020, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.L.; Marcenes, W. Global Burden of Severe Tooth Loss: A Systematic Review and Meta-Analysis. J. Dent. Res. 2014, 93, 20S–28S. [Google Scholar] [CrossRef] [PubMed]
- Romandini, M.; Baima, G.; Antonoglou, G.; Bueno, J.; Figuero, E.; Sanz, M. Periodontitis, Edentulism, and Risk of Mortality: A Systematic Review with Meta-Analyses. J. Dent. Res. 2021, 100, 37–49. [Google Scholar] [CrossRef]
- Ettinger, R.L.; Beck, J.D. Geriatric Dental Curriculum and the Needs of the Elderly. Spec. Care Dent. 1984, 4, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Reissmann, D.R.; Dard, M.; Lamprecht, R.; Struppek, J.; Heydecke, G. Oral Health-Related Quality of Life in Subjects with Implant-Supported Prostheses: A Systematic Review. J. Dent. 2017, 65, 22–40. [Google Scholar] [CrossRef]
- Zembic, A.; Wismeijer, D. Patient-Reported Outcomes of Maxillary Implant-Supported Overdentures Compared with Conventional Dentures. Clin. Oral Implant. Res. 2014, 25, 441–450. [Google Scholar] [CrossRef]
- Yao, C.J.; Cao, C.; Bornstein, M.M.; Mattheos, N. Patient-reported Outcome Measures of Edentulous Patients Restored with Implant-supported Removable and Fixed Prostheses: A Systematic Review. Clin. Oral Implant. Res. 2018, 29, 241–254. [Google Scholar] [CrossRef]
- Curtis, D.A.; Lin, G.H.; Rajendran, Y.; Gessese, T.; Suryadevara, J.; Kapila, Y.L. Treatment Planning Considerations in the Older Adult with Periodontal Disease. Periodontol 2000 2021, 87, 157–165. [Google Scholar] [CrossRef]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-Implant Diseases and Conditions: Consensus Report of Workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S286–S291. [Google Scholar] [CrossRef]
- Monje, A.; Aranda, L.; Diaz, K.T.; Alarcón, M.A.; Bagramian, R.A.; Wang, H.L.; Catena, A. Impact of Maintenance Therapy for the Prevention of Peri-Implant Diseases. J. Dent. Res. 2016, 95, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Blanco, C.; Liñares, A.; Dopico, J.; Pico, A.; Sobrino, T.; Leira, Y.; Blanco, J. Peri-Implantitis, Systemic Inflammation, and Dyslipidemia: A Cross-Sectional Biochemical Study. J. Periodontal Implant. Sci. 2021, 51, 342. [Google Scholar] [CrossRef] [PubMed]
- Catapano, S.; Ortensi, L.; Mobilio, N.; Grande, F. The New Elderly Patient: A Necessary Upgrade. Prosthesis 2021, 3, 99–104. [Google Scholar] [CrossRef]
- Doyle, D.J.; Hendrix, J.M.; Garmon, E.H. American Society of Anesthesiologists Classification; StatPearls Publishing: Tampa, FL, USA, 2023. [Google Scholar]
- Miller, E.L. Systems for Classifying Partially Dentulous Arches. J. Prosthet. Dent. 1970, 24, 25–40. [Google Scholar] [CrossRef] [PubMed]
- Catapano, S.; Ferrari, M.; Mobilio, N.; Montanari, M.; Corsalini, M.; Grande, F. Comparative Analysis of the Stability of Prosthetic Screws under Cyclic Loading in Implant Prosthodontics: An in Vitro Study. Appl. Sci. 2021, 11, 622. [Google Scholar] [CrossRef]
- Biscaro, L.; Becattelli, A.; Poggio, P.M.; Soattin, M.; Rossini, F. The One-Model Technique: A New Method for Immediate Loading with Fixed Prostheses in Edentulous or Potentially Edentulous Jaws. Int. J. Periodontics Restor. Dent. 2009, 29, 307–313. [Google Scholar]
- Monje, A.; Wang, H.-L.; Nart, J. Association of Preventive Maintenance Therapy Compliance and Peri-Implant Diseases: A Cross-Sectional Study. J. Periodontol. 2017, 88, 1030–1041. [Google Scholar] [CrossRef]
- Celeghin, G.; Franceschetti, G.; Mobilio, N.; Fasiol, A.; Catapano, S.; Corsalini, M.; Grande, F. Complete-Arch Accuracy of Four Intraoral Scanners: An in Vitro Study. Healthcare 2021, 9, 246. [Google Scholar] [CrossRef]
- Ortensi, L.; Ortensi, M.; Minghelli, A.; Grande, F. Implant-Supported Prosthetic Therapy of an Edentulous Patient: Clinical and Technical Aspects. Prosthesis 2020, 2, 140–152. [Google Scholar] [CrossRef]
- Ortensi, L.; Vitali, T.; Bonfiglioli, R.; Grande, F. New Tricks in the Preparation Design for Prosthetic Ceramic Laminate Veeners. Prosthesis 2019, 1, 29–40. [Google Scholar] [CrossRef]
- Ortensi, L.; Fisichella, M.L.; Ortensi, M.; Grande, F.; Pellegrino, G.; Ferri, A.; La Rosa, G.R.; Pedullà, E. A Comparison of Accuracy between Three Different Facial Detection Systems for Prosthodontic Esthetic Preview: A Single-Blinded in Vitro Study. Minerva Dent. Oral Sci. 2021, 71, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Petre, A.; Drafta, S.; Stefanescu, C.; Oancea, L. Virtual Facebow Technique Using Standardized Background Images. J. Prosthet. Dent. 2019, 121, 724–728. [Google Scholar] [CrossRef] [PubMed]
- Ortensi, L.; Sigari, G.; La Rosa, G.R.M.; Ferri, A.; Grande, F.; Pedullà, E. Digital Planning of Composite Customized Veneers Using Digital Smile Design: Evaluation of Its Accuracy and Manufacturing. Clin. Exp. Dent. Res. 2022, 8, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Paratelli, A.; Vania, S.; Gómez-Polo, C.; Ortega, R.; Revilla-León, M.; Gómez-Polo, M. Techniques to Improve the Accuracy of Complete-Arch Implant Intraoral Digital Scans: A Systematic Review. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef]
- Albayrak, B.; Sukotjo, C.; Wee, A.G.; Korkmaz, İ.H.; Bayındır, F. Three-Dimensional Accuracy of Conventional Versus Digital Complete Arch Implant Impressions. J. Prosthodont. 2021, 30, 163–170. [Google Scholar] [CrossRef]
- Tallarico, M.; Lumbau, A.I.; Scrascia, R.; Demelas, G.; Sanseverino, F.; Amarena, R.; Meloni, S.M. Feasibility of Using a Prosthetic-Based Impression Template to Improve the Trueness and Precision of a Complete Arch Digital Impression on Four and Six Implants: An in Vitro Study. Materials 2020, 13, 3543. [Google Scholar] [CrossRef]
- Venezia, P.; Torsello, F.; D’Amato, S.; Cavalcanti, R. Digital Cross-Mounting: A New Opportunity in Prosthetic Dentistry. Quintessence Int. 2017, 48, 701–709. [Google Scholar] [CrossRef]
- United Nations. World Population, Ageing; United Nations: New York, NY, USA, 2015. [Google Scholar]
- Kassebaum, N.J.; Smith, A.G.C.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.J.L.; Marcenes, W.; Abyu, G.Y.; Alsharif, U.; et al. Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990–2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef]
- Bakker, M.H.; Vissink, A.; Spoorenberg, S.L.W.; Jager-Wittenaar, H.; Wynia, K.; Visser, A. Are Edentulousness, Oral Health Problems and Poor Health-Related Quality of Life Associated with Malnutrition in Community-Dwelling Elderly (Aged 75 Years and over)? A Cross-Sectional Study. Nutrients 2018, 10, 1965. [Google Scholar] [CrossRef]
- Lantto, A.; Lundqvist, R.; Wårdh, I. Quality of Life Related to Tooth Loss and Prosthetic Replacements among Persons with Dependency and Functional Limitations. Acta Odontol. Scand. 2020, 78, 173–180. [Google Scholar] [CrossRef]
- Patzelt, S.B.M.; Bahat, O.; Reynolds, M.A.; Strub, J.R. The All-on-Four Treatment Concept: A Systematic Review. Clin. Implant Dent. Relat. Res. 2014, 16, 836–855. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Brägger, U.; Lang, N.P.; Zwahlen, M. Comparison of Survival and Complication Rates of Tooth-Supported Fixed Dental Prostheses (FDPs) and Implant-Supported FDPs and Single Crowns (SCs). Clin. Oral Implants Res. 2007, 18 (Suppl. 3), 97–113. [Google Scholar] [CrossRef] [PubMed]
- Rojas Vizcaya, F. Retrospective 2- to 7-Year Follow-Up Study of 20 Double Full-Arch Implant-Supported Monolithic Zirconia Fixed Prostheses: Measurements and Recommendations for Optimal Design. J. Prosthodont. 2018, 27, 501–508. [Google Scholar] [CrossRef]
- Mumcu, E.; Dayan, S.C.; Genceli, E.; Geckili, O. Comparison of Four-Implant-Retained Overdentures and Implant-Supported Fixed Prostheses Using the All-on-4 Concept in the Maxilla in Terms of Patient Satisfaction, Quality of Life, and Marginal Bone Loss: A 2-Year Retrospective Study. Quintessence Int. 2020, 51, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, N.U.; Marinello, C.P. Treatment Outcomes of Fixed or Removable Implant-Supported Prostheses in the Edentulous Maxilla. Part I: Patients’ Assessments. J. Prosthet. Dent. 2000, 83, 424–433. [Google Scholar] [CrossRef]
- Homsi, G.; Karlsson, A.; Almotairy, N.; Trulsson, M.; Kumar, A.; Grigoriadis, A. Subjective and Objective Evaluation of Masticatory Function in Patients with Bimaxillary Implant-Supported Prostheses. J. Oral Rehabil. 2022, 50, 140–149. [Google Scholar] [CrossRef]
- ELsyad, M.A.; Tella, E.A.E.S.; Mohamed, S.S.; Mahrous, A.I. Within-Patient Evaluation of Chewing Efficiency and Maximum Bite Force of Conventional Dentures, Fixed Prostheses, and Milled Bar Overdentures Used for All-on-4 Implant Rehabilitation of Atrophied Mandibular Ridges: A Short-Term Randomized Trial. Clin. Implant. Dent. Relat. Res. 2022, 24, 522–531. [Google Scholar] [CrossRef]
- Feine, J.S.; Maskawi, K.; de Grandmont, P.; Donohue, W.B.; Tanguay, R.; Lund, J.P. Within-Subject Comparisons of Implant-Supported Mandibular Prostheses: Evaluation of Masticatory Function. J. Dent. Res. 1994, 73, 1646–1656. [Google Scholar] [CrossRef]
- Monaco, C.; Scheda, L.; Ciocca, L.; Zucchelli, G. The Prototype Concept in a Full Digital Implant Workflow. J. Am. Dent. Assoc. 2018, 149, 918–923. [Google Scholar] [CrossRef]
- Bishti, S.; Tuna, T.; Rittich, A.; Wolfart, S. Patient-Reported Outcome Measures (PROMs) of Implant-Supported Reconstructions Using Digital Workflows: A Systematic Review and Meta-Analysis. Clin. Oral Implant. Res. 2021, 32, 318–335. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).