Abstract
Patients with lower limb amputation usually use prosthetic feet. Elastomeric material is an important part of prosthetic feet since it can determine their safety and lifetime. The elastomeric material should have high friction for safety, and at the same time it should have low wear for a longer lifetime. This research is aimed to study the optimum formulation of talc-powder-reinforced silicone elastomer to obtain high friction during sliding contact. The Taguchi orthogonal array L9 formula is used to achieve the aforementioned goal. The experiments use multiple parameters, namely, the type of silicone, the type of surface texture, the amount of catalyst, and the amount of talc powder. The results show that the combination of RTV 683, a smooth texture, 4% of catalyst, and 60% of talc powder is the most optimum composition to obtain the highest frictional force. It has a higher friction force in comparison with the imported products, and, at the same time, it has comparable wear with the imported products. The hardness of the optimized materials is comparable with the imported products. However, the tensile and tear strengths of the optimized materials need to be improved.
1. Introduction
Major amputations are suffered by almost 38 million people worldwide, out of which 85% of people are lower-limb amputated [1]. In Indonesia, more than 8.5% of the population suffered from disabilities, which increased by approximately 2.45% from 2012. People with lower limb amputations will have difficulty walking [2] and reduce mobility [3]. The popular solution for patients with lower limb amputation is lower limb prostheses. The main parts of lower limb prostheses are a socket, shank (also known as phylon), and a prosthetic feet. The prosthetic foot is one of the most important parts since it can determine the lifetime of the product.
Different types of prosthetic feet have been developed in past few decades, such as the solid ankle cushion heel (SACH) prosthetic foot, the single-axis-design prosthetic foot, the multiple-axis (multiaxial)-design prosthetic foot, and the microprocessor foot. SACH is a popular type that is used in Indonesia and other developing countries because it offers a lower price than other types of prosthetic feet. The SACH is also simpler than other prosthetic feet due to the absence of mechanical articulation [4]. The local product of SACH that is available on the Indonesian market can be seen in Figure 1.
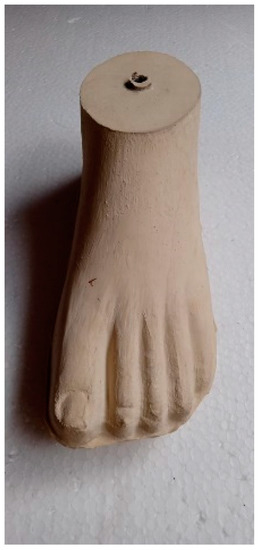
Figure 1.
Local product of SACH in Indonesia market.
The prosthetic foot is a crucial part in determining the lifetime of the lower limb prosthesis. The prosthetic foot will have a longer life if the foot materials have high wear resistance. On the other hand, the prosthetic foot should have high friction to avoid slips. Therefore, material selection of the prosthetic foot is of importance. Elastomeric materials are widely used in prosthetic feet because they can fulfill the requirements [5]. Several types of elastomeric materials have been studied to be used in prosthetic feet, such as natural rubber [6], ethyl-vinyl-acetate [7], polyurethane [8], silicone [9], and the combination of polyurethane and neoprene [10].
Silicone elastomers were used in several medical devices due to their advantageous properties, such as being soft and flexible, highly chemically resistant, and having good biocompatibility [11,12]. Some examples of those elastomeric materials are PDMS and ecoflex [13]. The medical devices that are made of silicone are maxillofacial prosthetic material [7], implant to medialization laryngoplasty [14], finger joints [15], breast implants [16], and catheters [17]. However, in some applications, silicone elastomers cannot fulfill all of the requirements due to their low tensile and tear strengths. Therefore, several studies were conducted to improve the mechanical properties of silicone materials, such as by adding fillers to the silicone [18,19].
The study of prosthetic feet was conducted in several aspects, such as structure [20], cyclic foot (fatigue) [6], and dorsiflexion [21]. While the elastomeric materials of the foot were studied in the aspect of mechanical properties, such as tensile strength, tear strength, and hardness [21]. Although several aspects of prosthetic feet have been studied, the study of the tribological aspects, such as friction and wear, of the elastomeric materials is still limited in the literature. The study of the tribological aspects of prosthetic feet is important due to their influence on the lifetime and safety of the products.
In the present study, an elastomeric material based on silicone elastomer reinforced by talc powder was investigated in the tribological aspect. The Taguchi method was used to find an optimum parameter for tribological characteristics. The Taguchi method is very effective and efficient for an experiment that uses many variables. It can reduce the number of samples and the test. So, it saves time and cost. Many researchers use the Taguchi method to find the optimum parameter value or composition [22,23,24]. The Taguchi method uses several basic formulas to calculate the optimum result. The formula is called the S/N ratio (signal to noise ratio). There are three characteristics of the S/N ratio. There are normal-is-better, larger-is-better, and smaller-is-better. The normal-is-better is used when a specified value is most desired. Equation (1) shows the S/N ratio formula for normal-is-better. The larger-is-better and the smaller-is-better equation are used when the largest or smallest value is the most desired. Equations (2) and (3) show the S/N ratio formula for larger-is-better and smaller-is-better, respectively.
where n is the number of replicas and y is the test result. In the present study, the main material characteristic to be achieved is high friction. Four parameters were varied to achieve the goal. Moreover, the wear mass and mechanical properties of the silicone were investigated.
2. Materials and Methods
The present study uses four independent variables: the type of silicone elastomer, the surface texture, the percentage of catalyst, and the percentage of talc powder. The type of silicone elastomer and the amount of catalyst will significantly influence the mechanical and tribological properties of the elastomer. Therefore, the selection of silicone and the percentage of the catalyst are important. The talc powders were added to the silicone elastomer to improve the mechanical and tribological properties of the silicone elastomer. While the surface textures were varied to obtain high friction. Each variable is varied by three levels, as shown in Table 1. The number of the test run is derived from the variables and the levels following the Taguchi orthogonal array L9 formula. The details of the test run can be seen in Table 2. The materials were made based on the composition shown in Table 2. Three tests were conducted for each run number to check the repeatability.

Table 1.
The control factors and their levels.

Table 2.
The composition of the run number based on Taguchi orthogonal array L9.
The textured surface of the testing sample consists of three types. The first one is a smooth surface, a flat surface without texture. The other two are an equilateral triangle and a circle. The geometric shape and size of the triangle and circle are shown in Table 3.

Table 3.
The textured geometry.
A pin-on-disc tribometer is used to investigate the tribological characteristics of the materials. The sliding contact occurs between a silicone pin and a smooth tile. The silicone pin was manufactured with three different textures at the end of the tip. The arithmetic roughness of the tile is 0.045 μm. The pin and the disc used in this study are shown in Figure 2. The load of 7 N was used in the sliding contact experiments; it is based on the force distribution of the 54 cm2 cross-section foot during mid-foot loading [25]. The angular speed of the disc is 20 rpm, and the radius of the wear track is 20 mm, resulting in a linear speed of 42 mm/s. The tests were conducted at ambient temperature. The tribometer tests were stopped once the sliding distance reached 200 m (~80 min). The tensile, tear, and hardness tests of the silicone elastomers were conducted by following the ISO 37:2015, ISO 34-1: 2015, and ISO 7619-1: 2010, respectively.

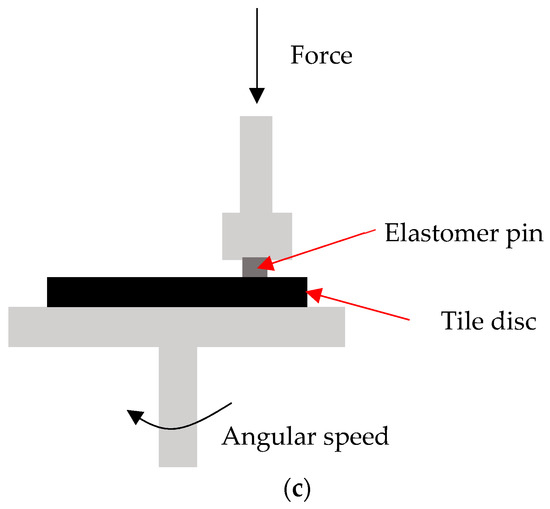
Figure 2.
The contacting materials (a) several silicone pins with various textures, (b) the tile disc, and (c) pin-on-disc tribometer, schematically.
3. Results and Discussions
Figure 3 shows the result of the tribometer test. It can be seen that at a certain sliding distance, the friction force reaches a constant value. In the present study, the value of the friction force is determined when the friction force reaches a steady-state phase.
Figure 3.
Friction force as a function of sliding friction, the red line shows a steady state phase.
Table 4 shows the result of the sliding friction test for each run number. The friction force is determined when the signal reaches a steady state phase. The experiment was repeated three times for each run number. The result of frictional force was used to calculate the S/N ratio. The S/N ratio was calculated by using the larger is better equation (Equation (2)) since the purpose of the optimization is to have a higher friction force. The higher the friction force, the safer the prosthetic feet. The average S/N ratio for all run numbers is 13.92; see Table 4.

Table 4.
The frictional force and S/N calculation.
After calculating the S/N ratio, the results are grouped by the parameters and their levels. Where A is the type of silicone, B is the surface texture, C is the percentage of catalyst, and D is the percentage of talc powder. The number label is the level of each parameter. For example, the code A1 means RTV683, A2 means RTV M4503, and so on. Table 5 shows the grouping result of the S/N ratio and the mean of the frictional force.

Table 5.
The average S/N ratio for the frictional force.
Figure 4 shows the plotting results of Table 5. The combination of the highest value of each control factor is a prediction of the optimum composition. Therefore, combining the RTV 683, a smooth texture, 4% of catalyst, and 60% of talc powder may achieve the highest friction force. Generally, the friction force of the contacting materials depends on adhesive friction and hysteresis friction [26]. In the previous research, the friction of elastomeric materials is significantly influenced by the adhesive component, while the hysteresis component plays a minor role [27]. The smooth texture of the elastomer will result in a larger real contact area between surfaces [28]. For adhesive friction, the larger the real contact area, the higher the friction force. The smallest amount of talc powder (60%) was found to be the best composition to obtain the highest friction force. A small amount of filler, such as talc powder, will result in low mechanical properties. As a result, a larger real contact area will be found on the contacting surface since the elastomer will fill the cavity of the tile roughness. The ratio of the optimum composition was calculated by the following Equation:
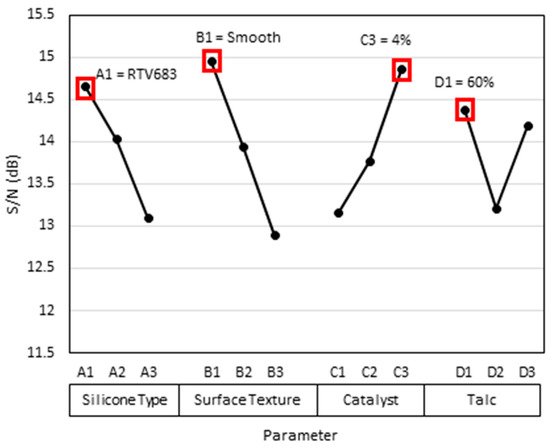
Figure 4.
The ratio graph for frictional force in the smooth tile.
The Popt is the ratio prediction of the optimum composition; is the mean-of-signal-to-noise ratio for the evaluated process parameters; n is the number of process parameters, which is equal to 4; and is the mean of signal-to-noise ratio for all of the process parameters. The calculated Popt in the present study is 17.06, as can be seen in Table 6. The prediction of the friction force value for the optimum composition material can be calculated by the inversion of Equation (2), and the result is 7.07 N.

Table 6.
Prediction of optimum ratio.
Since the optimum composition (A1, B1, C3, and D1) is outside of the run number composition (see Table 2), it has to be validated by additional experiments. The samples with the optimum composition were produced and tested. The validation experiment is shown in Table 7. The result shows that the average friction force (6.75 N) is near the prediction results (~7 N). The improvement of the friction force is 33.40% in comparison with the average friction force of all run numbers.

Table 7.
The validation results.
The results of multifactor optimization show that the combination of RTV 683, a smooth texture, 4% of catalyst, and 60% of talc powder is the most optimum composition to obtain the highest frictional force. This optimized material was compared to the existing products, namely, imported product A and imported product B. The tribometer tests of the imported products were conducted by using the same operating conditions as the optimized material. The comparison of the friction force is shown in Figure 5. It can be seen that the optimized material has a higher friction force compared to the other products. This high friction will improve the safety of the product since it can avoid the slip during the usage of prosthetic feet.
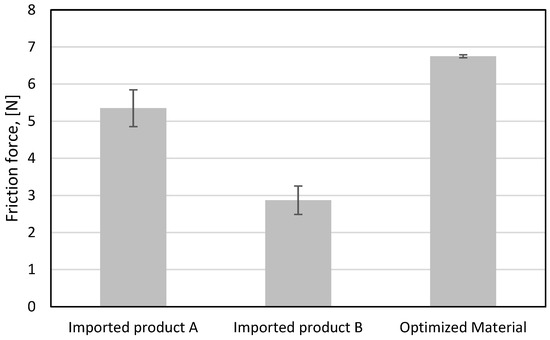
Figure 5.
The comparison of friction force between the imported products and the optimized material.
The important parameter for prosthetic foot material is not only high friction but also low wear. The low wear of material will affect the lifetime of the product. The lower the wear, the longer the lifetime. The high friction will be obtained by the weak mechanical properties, but at the same time, it will result in high wear. A similar case was found in the tire product [29]. Achieving both goals is very challenging since they are a contradiction. Therefore, optimization is needed to compromise both goals. The comparison of wear mass between the imported products and the optimized material can be seen in Figure 6. It shows that the imported product B has the lowest wear, while the wear of optimized material is slightly higher than the imported product A. The wear mass of the optimized material is still higher than that of the imported products. However, the value is comparable to the imported product A when the standard deviation is considered. The result of the friction force of imported product A is lower than that of the optimized material, see Figure 5.
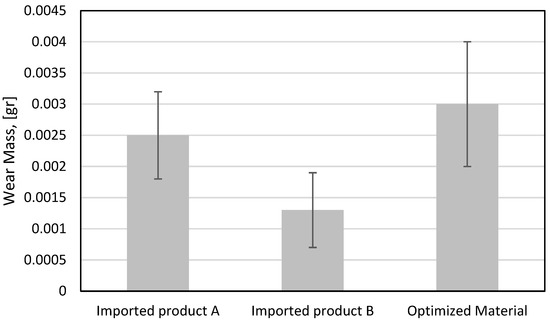
Figure 6.
The comparison of wear mass between the imported products and the optimized material.
The pin on the disc tribometer tests shows that the optimum composition has better characteristics for the frictional force, but the wear mass is still worse than the imported products as the benchmark. Furthermore, the mechanical characteristics of the optimized material are still lower than the imported product. Figure 7 shows the comparison of the tensile strength test between the imported products and the optimized material. The tensile strength of the optimized material is only around half that of the imported product A. The reinforcement of talc powder without any coating on the talc surface will result in a weak bond between the talc powder and the silicone elastomers. A previous study indicates that the use of silane coating on the filler will improve those bonds, and as a result, the mechanical properties of the composites will improve [30]. The use of the silane coating on the talc surface will be conducted in a future study.
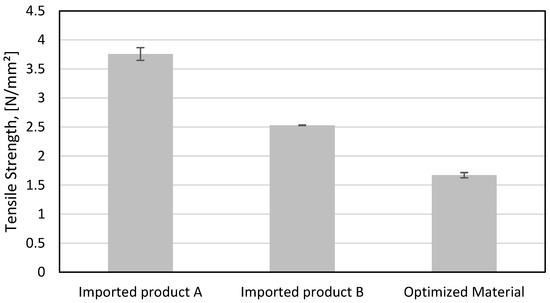
Figure 7.
The comparison of tensile strength between the imported products and the optimized material.
Another mechanical characteristic is tear strength. This characteristic is important to avoid tears when a prosthetic foot comes into contact with a sharp material. Figure 8 shows the result of the tear strength of the imported products and the optimized material. It shows that the tear strength of the optimized material is lower than that of the imported products. The tear strength of the optimized material is only approximately a quarter smaller than that of the imported products. For future study, the use of long filler, such as fiber, needs to be investigated to improve the tear strength. Some studies reported that fiber could improve the tear strength of the composites [31,32].
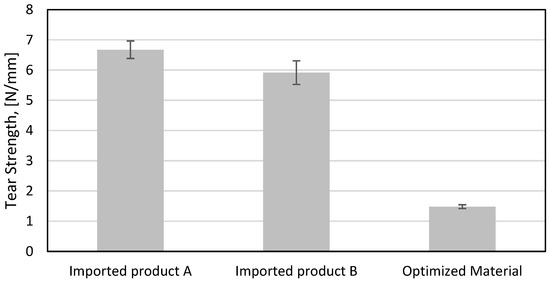
Figure 8.
The comparison of tear strength between the imported products and the optimized material.
Figure 9 shows that the optimized material has a similar hardness to the imported product B, but it is lower than the imported product A. Overall, some mechanical characteristics of the optimized material are inferior to the imported products. Therefore, some research needs to be conducted to improve the mechanical properties of the material, and at the same time, the material has high friction and low wear. A coating process on the talc surface and the use of long filler, such as fibers, in the material is an alternative way to achieve the aforementioned goals.
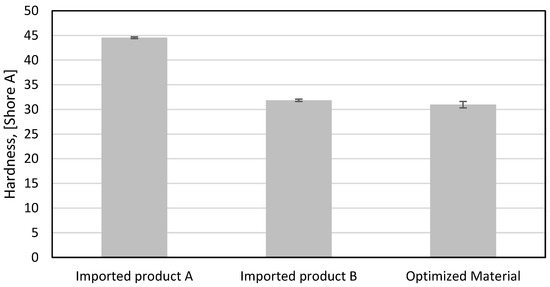
Figure 9.
The comparison of hardness between the imported products and the optimized material.
4. Conclusions
In this work, silicone elastomer-reinforced talc powder for prosthetic feet was studied. The main goal of the present study is to obtain an optimum formulation that has high friction force. The Taguchi orthogonal array L9 formula was used to obtain the optimum formulation of silicone elastomer. The key conclusions can be drawn as follows:
- The combination of RTV 683, a smooth texture, 4% of catalyst, and 60% of talc powder is the most optimum composition.
- The friction force of the optimized material is 6.75 N. The improvement of the friction force is 33.40% in comparison with the average friction force of all the run numbers.
- The friction force of the optimized material is higher than the imported products.
- The tensile and tear strengths of the optimized material are lower than the imported products.
- The low tensile and tear strengths can be caused by the weak bond between talc powder and silicone rubber. In future works, a coating of talc powder will be conducted to improve the bond between talc powder and silicone rubber. Moreover, a relatively long filler, such as fibers, will be used to improve the tensile and tear strengths of the composites.
Author Contributions
Conceptualization, M.K., L.K. and D.S.; methodology, M.K.; validation, M.N. and M.K.; investigation, M.N.; data curation, M.N. and D.S.; writing—original draft preparation, D.S. and M.K.; writing—review and editing, M.K. and R.I.; supervision, R.I.; and funding acquisition, M.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Ministry of Education, Culture, Research, and Technology, Republic of Indonesia, grant number 071/E5/PG.02.00.PT/2022.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chauhan, P.; Singh, A.K.; Raghuwanshi, N.K. The state of art review on prosthetic feet and its significance to imitate the biomechanics of human ankle-foot. Mater. Today Proc. 2022, 62, 6364–6370. [Google Scholar] [CrossRef]
- Waters, R.L.; Mulroy, S. The energy expenditure of normal and pathologic gait. Gait Posture 1999, 9, 207–231. [Google Scholar] [CrossRef] [PubMed]
- Stepien, J.M.; Cavenett, S.; Taylor, L.; Crotty, M. Activity Levels Among Lower-Limb Amputees: Self-Report Versus Step Activity Monitor. Arch. Phys. Med. Rehabil. 2007, 88, 896–900. [Google Scholar] [CrossRef] [PubMed]
- Staros, A. The SACH (solid-ankle cushion-heel) foot. Ortho. Pros. Appl. J. 1957, 11, 23–31. [Google Scholar]
- Nishi, T. Rubber wear mechanism discussion based on the relationship between the wear resistance and the tear resistance with consideration of the strain rate effect. Wear 2019, 426–427, 37–48. [Google Scholar] [CrossRef]
- Sasaki, K.; Pinitlertsakun, J.; Rattanakoch, J.; Sukthomya, S.; Guerra, G.; Latt, T.; De Silva, N.; Kanagarandnam, B.; Suntharalingam, S. The development and testing of a modified natural rubber CR solid ankle–cushion heel prosthetic foot for developing countries. J. Rehabil. Assist. Technol. Eng. 2017, 4, 2055668317712978. [Google Scholar] [CrossRef]
- Andreopoulos, A.G.; Evangelatou, M.; Tarantili, P.A. Properties of maxillofacial silicone elastomers reinforced with silica powder. J. Biomater. Appl. 1998, 13, 66–73. [Google Scholar] [CrossRef]
- Jensen, J.S.; Nilsen, R.; Thanh, N.H.; Saldana, A.; Hartz, C. Clinical field testing of polyurethane feet for trans-tibial amputees in tropical low-income countries. Prosthet. Orthot. Int. 2006, 30, 182–194. [Google Scholar] [CrossRef]
- Kulkarni, J.; Curran, B.; Ebdon-Parry, M.; Harrison, D. Total contact silicone partial foot prostheses for partial foot amputations. Foot 1995, 5, 32–35. [Google Scholar] [CrossRef]
- Ramli, W.S.W.; Zin, M.I.I.M.; Desa, M.S.Z.M.; Ramli, A. “Return-To-Work”: Application of New Materials to Develop the Durable and Low Cost of Solid Ankle Cushion Heel (SACH) Prosthetic Foot. In Human-Centered Technology for a Better Tomorrow; Springer: Singapore, 2022; pp. 475–483. [Google Scholar]
- Zare, M.; Ghomi, E.R.; Venkatraman, P.D.; Ramakrishna, S. Silicone-based biomaterials for biomedical applications: Antimicrobial strategies and 3D printing technologies. J. Appl. Polym. Sci. 2021, 138, 50969. [Google Scholar] [CrossRef]
- Colas, A.; Curtis, J. 7-Silicones. In Handbook of Polymer Applications in Medicine and Medical Devices; Modjarrad, K., Ebnesajjad, S., Eds.; William Andrew Publishing: Oxford, UK, 2013; pp. 131–143. [Google Scholar] [CrossRef]
- Mariello, M.; Fachechi, L.; Guido, F.; De Vittorio, M. Conformal, Ultra-thin Skin-Contact-Actuated Hybrid Piezo/Triboelectric Wearable Sensor Based on AlN and Parylene-Encapsulated Elastomeric Blend. Adv. Funct. Mater. 2021, 31, 2101047. [Google Scholar] [CrossRef]
- Ustundag, E.; Boyaci, Z.; Keskin, G.; Kaur, A.; Ozkarakas, H. Soft Tissue Response of the Larynx to Silicone, Gore-Tex, and Irradiated Cartilage Implants. Laryngoscope 2005, 115, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- Swanson, A. Finger joint replacement by silicone rubber implants and the concept of implant fixation by encapsulation. J. Ann. Rheum. Dis. 1969, 28 (Suppl. S5), 47. [Google Scholar]
- Herdman, R.; Ernster, V.; Bondurant, S. Safety of Silicone Breast Implants; National Academy of Sciences: Washington, DC, USA, 2000. [Google Scholar]
- Curtis, J.; Colas, A. Chapter II.5.18—Medical Applications of Silicones. In Biomaterials Science, 3rd ed.; Ratner, B.D., Hoffman, A.S., Schoen, F.J., Lemons, J.E., Eds.; Academic Press: Cambridge, MA, USA, 2013; pp. 1106–1116. [Google Scholar] [CrossRef]
- He, Q.; Li, A.; Zhang, Y.; Liu, S.; Guo, Y.; Kong, L. A study on mechanical and tribological properties of silicone rubber reinforced with white carbon black. Tribol.-Mater. Surf. Interfaces 2018, 12, 9–16. [Google Scholar] [CrossRef]
- Silva, V.P.; Gonçalves, M.C.; Yoshida, I.V.P. Biogenic silica short fibers as alternative reinforcing fillers of silicone rubbers. J. Appl. Polym. Sci. 2006, 101, 290–299. [Google Scholar] [CrossRef]
- Naseri, A.; Moghaddam, M.M.; Grimmer, M.; Sharbafi, M.A. Passive hydraulic prosthetic foot to improve the push-off during walking. Mech. Mach. Theory 2022, 172, 104777. [Google Scholar] [CrossRef]
- Yousif, L.E.; Resan, K.K.; Fenjan, R.M. Temperature Effect on Mechanical Characteristics of A New Design Prosthetic Foot. Int. J. Mech. Eng. Technol. 2018, 9, 1431–1447. [Google Scholar]
- Mitra, A.C.; Jawarkar, M.; Soni, T.; Kiranchand, G.R. Implementation of Taguchi Method for Robust Suspension Design. Procedia Eng. 2016, 144, 77–84. [Google Scholar] [CrossRef]
- Mohsin, I.; He, K.; Li, Z.; Zhang, F.; Du, R. Optimization of the Polishing Efficiency and Torque by Using Taguchi Method and ANOVA in Robotic Polishing. Appl. Sci. 2020, 10, 824. [Google Scholar] [CrossRef]
- Abd Maleque, M.; Harina, L.; Bello, K.; Azwan, M.; Rahman, M.M. Tribological properties of surface modified Ti-6Al-4V alloy under lubricated condition using Taguchi approach. J. Tribol. 2018, 17, 15–28. [Google Scholar]
- Lidstone, D.E.; DeBerardinis, J.; Dufek, J.S.; Trabia, M.B. Electronic measurement of plantar contact area during walking using an adaptive thresholding method for Medilogic® pressure-measuring insoles. Foot 2019, 39, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.F. The Friction and Lubrication of Elastomers; Pergamon: Oxford, UK, 1972; Volume 9. [Google Scholar]
- Khafidh, M.; Schipper, D.J.; Masen, M.A. The Formation of a Modified Surface Layer on Elastomeric Materials. Tribol. Lett. 2019, 67, 27. [Google Scholar] [CrossRef] [PubMed]
- Mokhtari, M.; Schipper, D.J.; Tolpekina, T.V. On the Friction of Carbon Black- and Silica-Reinforced BR and S-SBR Elastomers. Tribol. Lett. 2014, 54, 297–308. [Google Scholar] [CrossRef]
- Weng, P.; Tang, Z.; Guo, B. Solving “magic triangle” of tread rubber composites with phosphonium-modified petroleum resin. Polymer 2020, 190, 122244. [Google Scholar] [CrossRef]
- Liu, K.; Stadlbauer, W.; Zitzenbacher, G.; Paulik, C.; Burgstaller, C. Effects of surface modification of talc on mechanical properties of polypropylene/talc composites. AIP Conf. Proc. 2016, 1713, 120008. [Google Scholar] [CrossRef]
- Jacob, M.; Thomas, S.; Varughese, K.T. Mechanical properties of sisal/oil palm hybrid fiber reinforced natural rubber composites. Compos. Sci. Technol. 2004, 64, 955–965. [Google Scholar] [CrossRef]
- Kalapakdee, A.; Amornsakchai, T. Mechanical properties of preferentially aligned short pineapple leaf fiber reinforced thermoplastic elastomer: Effects of fiber content and matrix orientation. Polym. Test. 2014, 37, 36–44. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).