Development and Effectiveness Testing of a Novel 3D-Printed Multi-Material Orthosis in Nurses with Plantar Foot Pain
Abstract
1. Introduction
2. Materials and Methods
2.1. Demographics
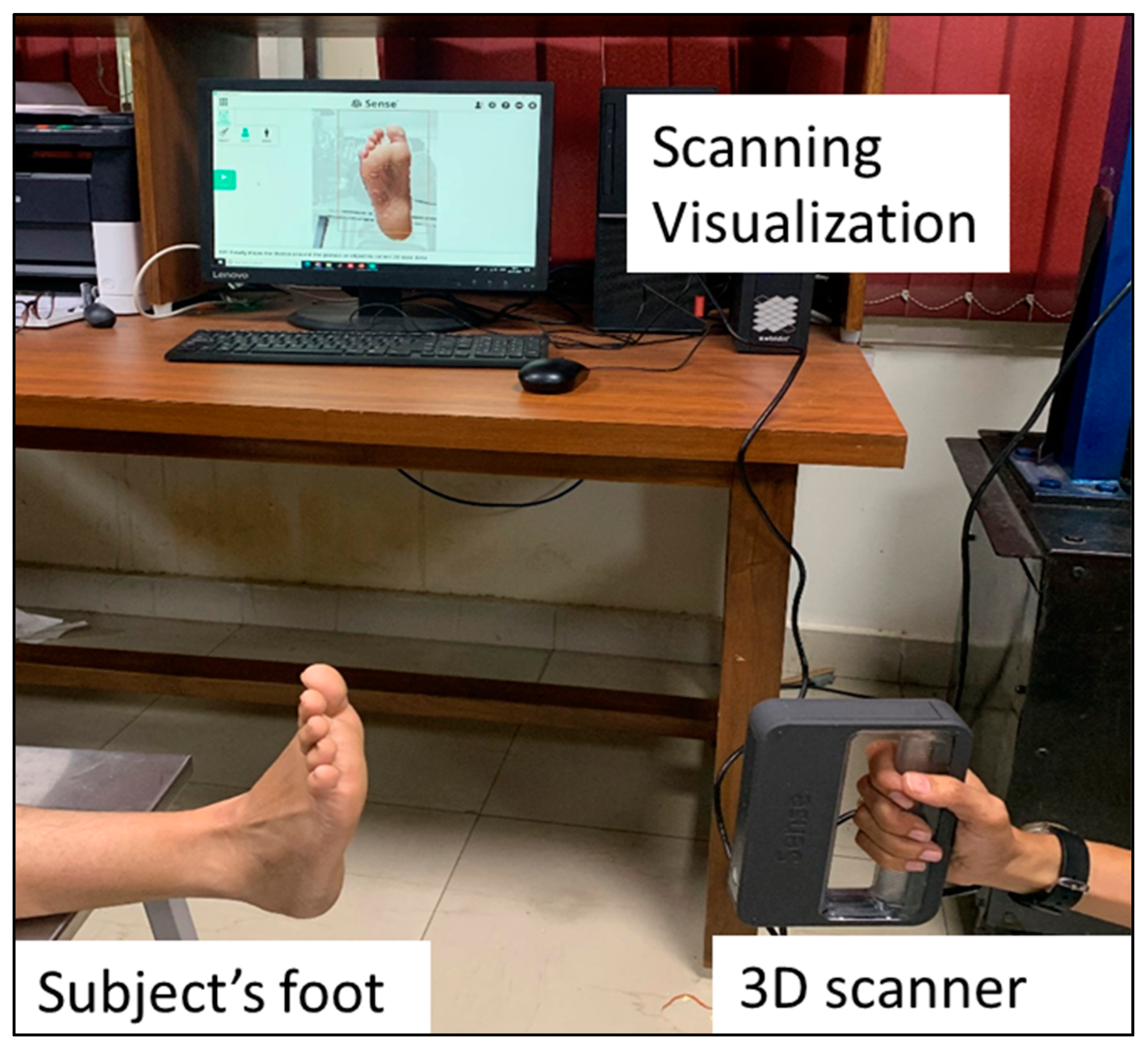
2.2. Design and Fabrication of Orthosis
2.3. Material Selection
2.4. Validation
2.5. Measures
2.6. Data Analysis
3. Results
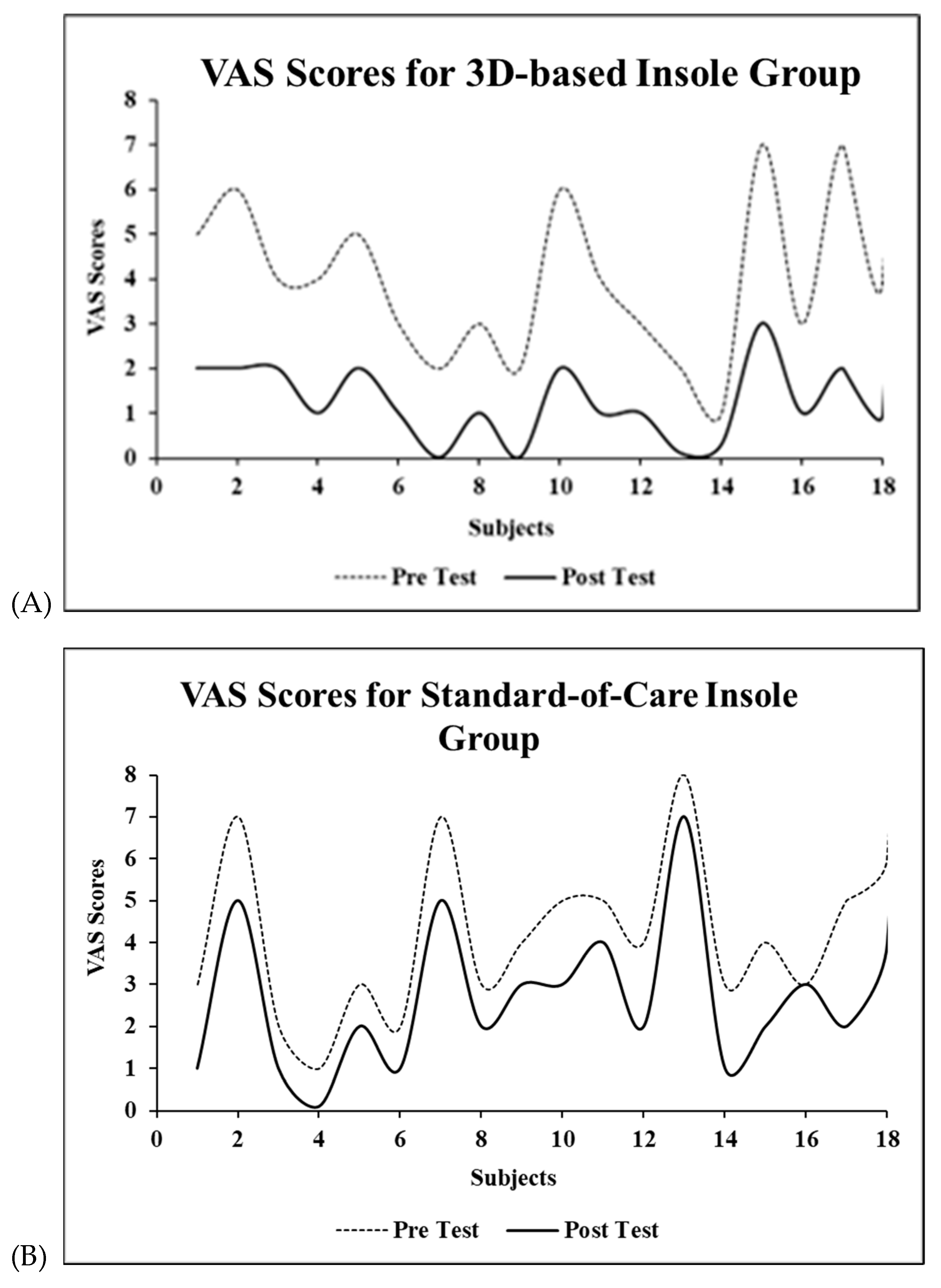
3.1. Pain
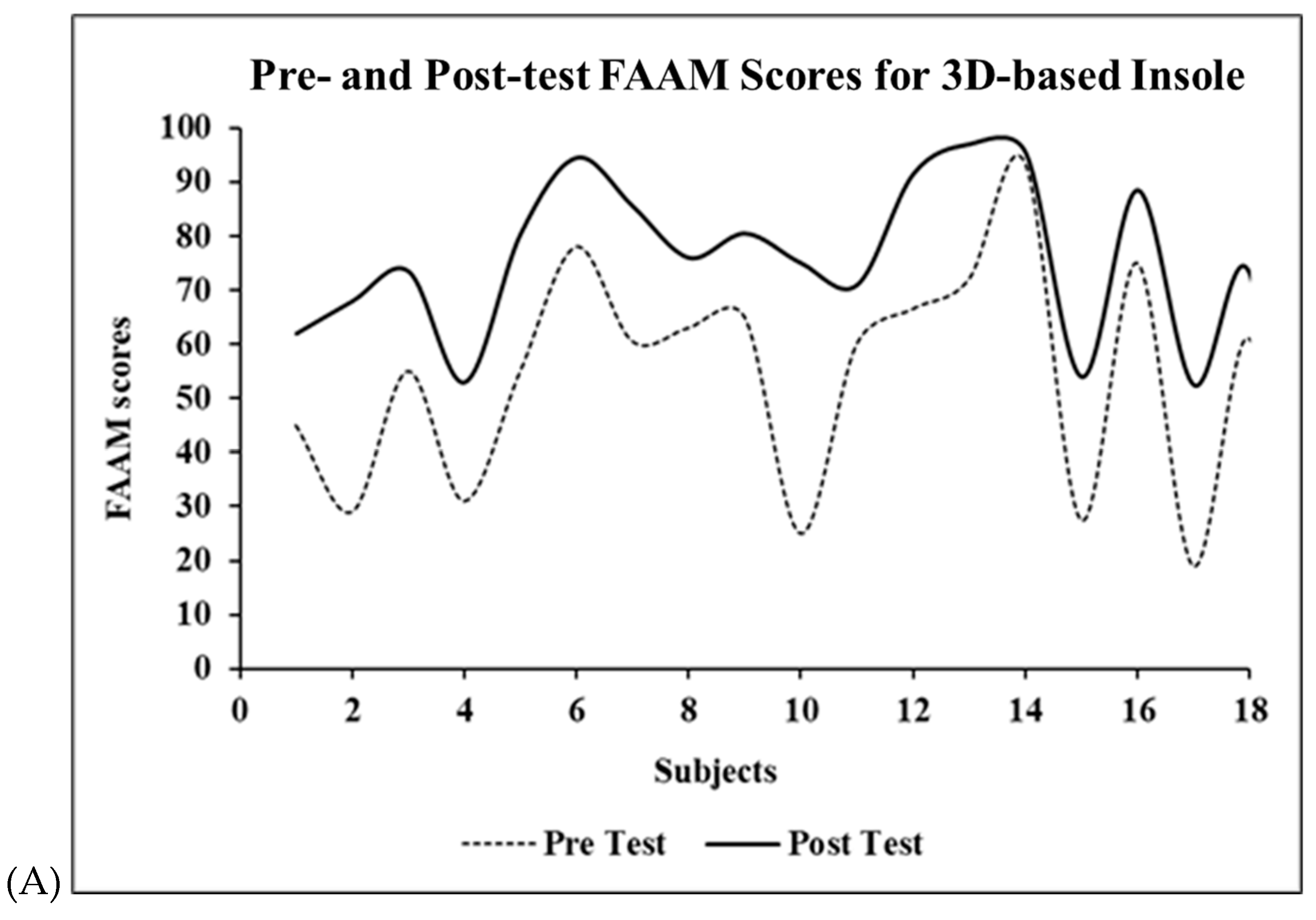
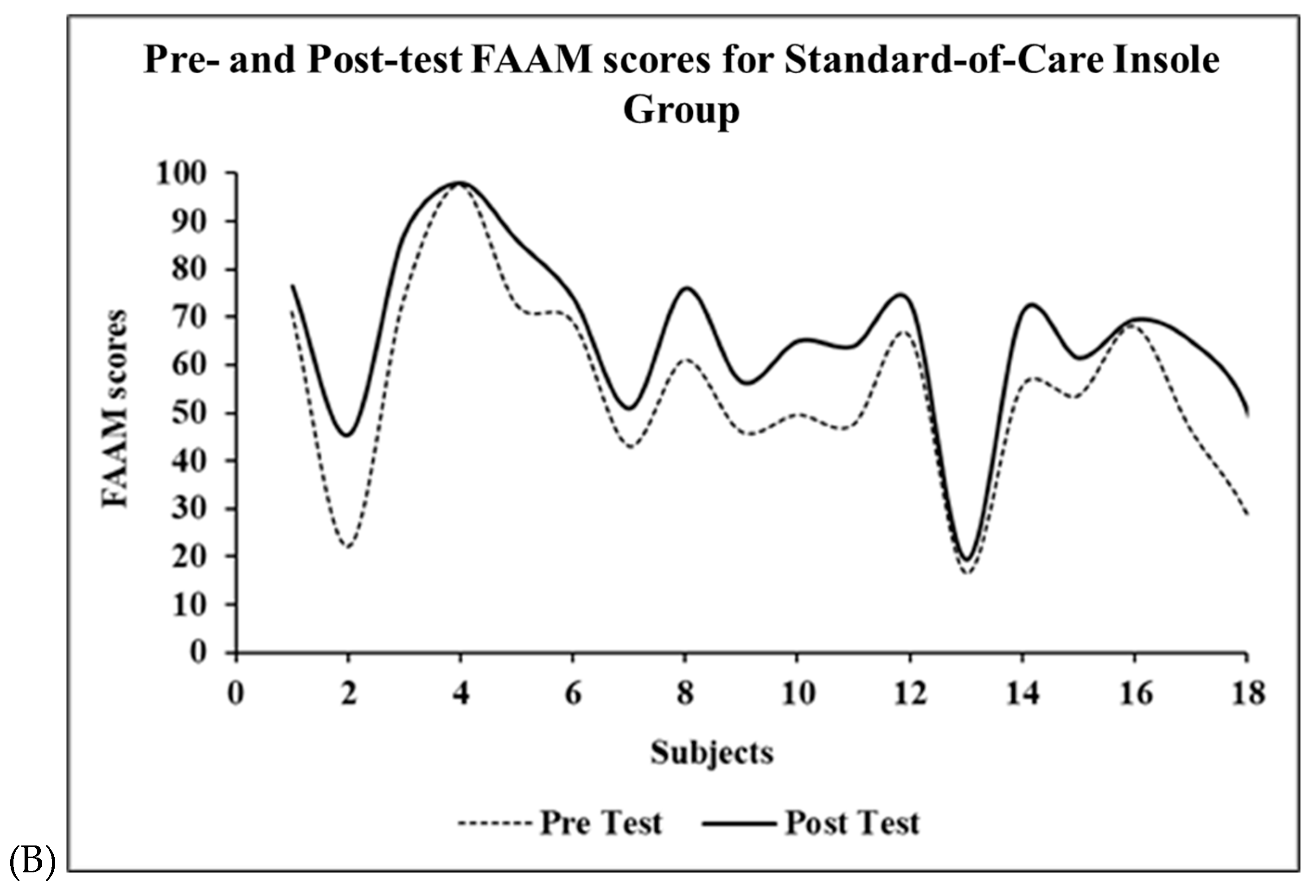
3.2. Functionality
3.3. Plantar Pressure
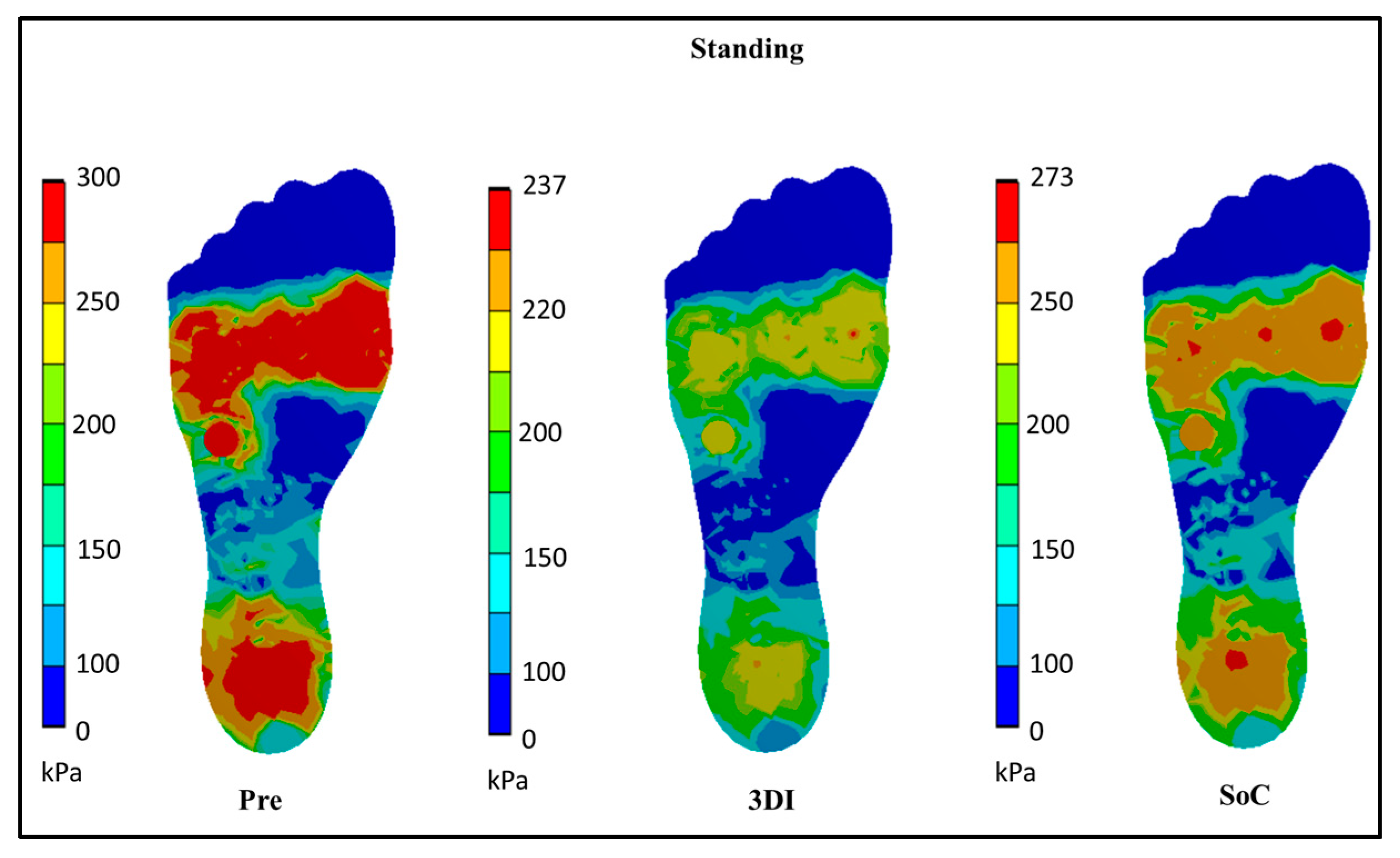
3.3.1. Standing
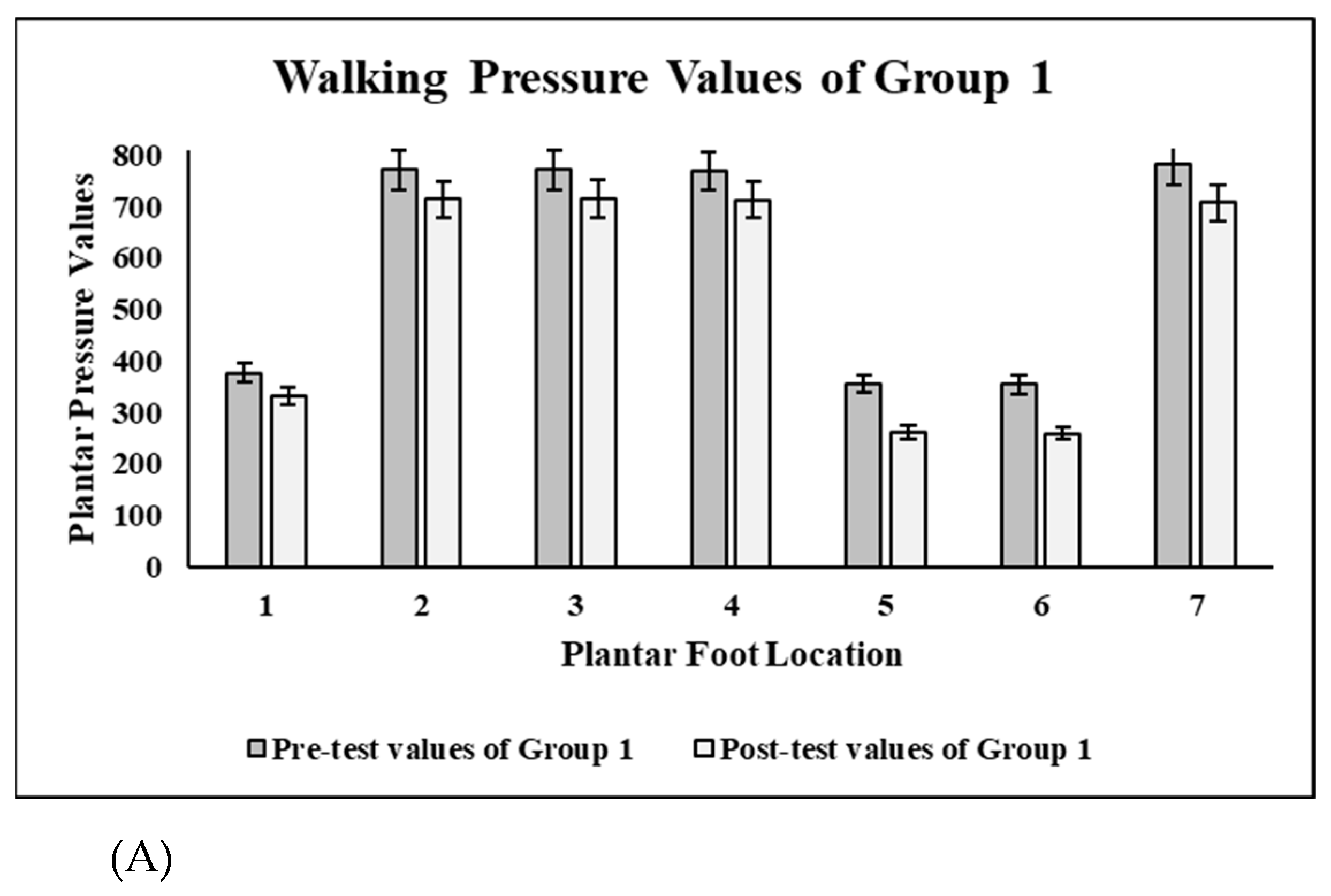
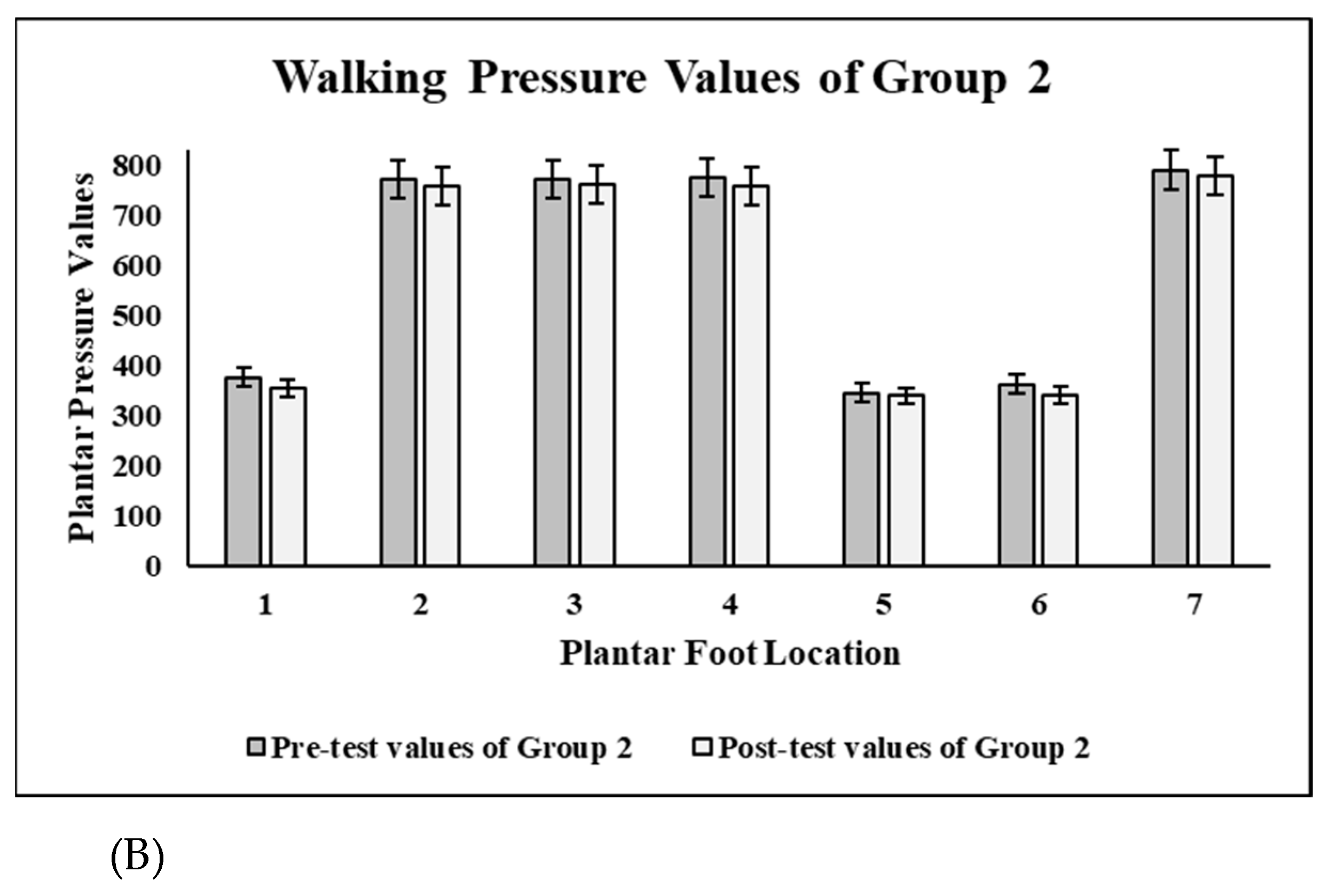
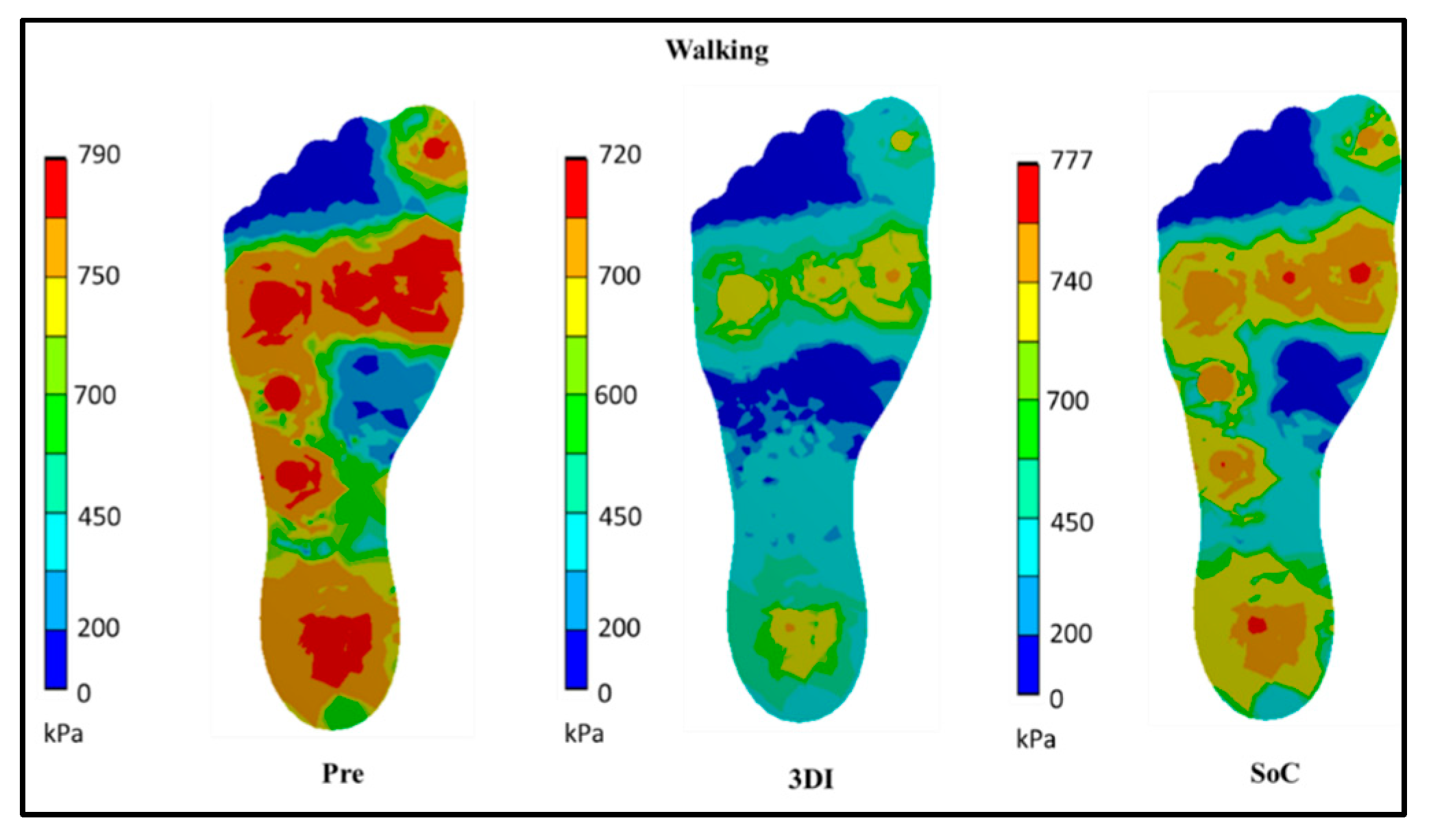
3.3.2. Walking
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rao, S.; Riskowski, J.L.; Hannan, M.T. Musculoskeletal conditions of the foot and ankle: Assessments and treatment options. Best Pract. Res. 2012, 26, 345–368. [Google Scholar] [CrossRef] [PubMed]
- Porter, K.B. Plantar Heel Pain. In Physical Therapy: Treatment of Common Orthopedic Conditions; JP Medical Ltd.: London, UK, 2016; pp. 382–412. [Google Scholar] [CrossRef]
- Chan, C.W.; Rudins, A. Foot Biomechanics During Walking and Running. Mayo Clin. Proc. 1994, 69, 448–461. [Google Scholar] [CrossRef] [PubMed]
- Choo, Y.J.; Park, C.H.; Chang, M.C. Rearfoot disorders and conservative treatment: A narrative review. Ann. Palliat. Med. 2020, 9, 3546–3552. [Google Scholar] [CrossRef] [PubMed]
- Badlissi, F.; Dunn, J.E.; Link, C.L.; Keysor, J.J.; McKinlay, J.B.; Felson, D.T. Foot musculoskeletal disorders, pain, and foot-related functional limitation in older persons. J. Am. Geriatr. Soc. 2005, 53, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Alshami, A.M.; Souvlis, T.; Coppieters, M.W. A review of plantar heel pain of neural origin: Differential diagnosis and management. Man. Ther. 2008, 13, 103–111. [Google Scholar] [CrossRef]
- Gutteck, N.; Schilde, S.; Delank, K.S. Pain on the Plantar Surface of the Foot. Dtsch. Arztebl. International. 2019, 116, 83–88. [Google Scholar] [CrossRef]
- Chia, J.K.; Suresh, S.; Kuah, A.; Ong, J.L.; Phua, J.M.; Seah, A.L. Comparative trial of the foot pressure patterns between corrective orthotics, formthotics, bone spur pads and flat insoles in patients with chronic plantar fasciitis. Ann. Acad. Med. Singapore. 2009, 38, 869. [Google Scholar] [CrossRef]
- Soylar, P. Evaluation of the prevalence of musculoskeletal disorders in nurses: A systematic review. Artic. Med. Sci. Int. Med. J. 2018, 7, 479–485. [Google Scholar] [CrossRef]
- Waters, T.R.; Dick, R.B. Evidence of health risks associated with prolonged standing at work and intervention effectiveness. Rehabil. Nurs. 2015, 40, 148–165. [Google Scholar] [CrossRef]
- Goecker, R.M.; Banks, A.S. Analysis of release of the first branch of the lateral plantar nerve. J. Am. Podiatr. Med. Assoc. 2000, 90, 281–286. [Google Scholar] [CrossRef]
- Landorf, K.B.; Keenan, A.M.; Herbert, R.D. Effectiveness of Foot Orthoses to Treat Plantar Fasciitis: A Randomized Trial. Arch. Intern. Med. 2006, 166, 1305–1310. [Google Scholar] [CrossRef]
- Elattar, O.; Smith, T.; Ferguson, A.; Farber, D.; Wapner, K. Uses of Braces and Orthotics for Conservative Management of Foot and Ankle Disorders. Foot Ankle Orthop. 2018, 3. [Google Scholar] [CrossRef]
- Hawke, F.; Burns, J.; Radford, J.A.; Toit, V.D. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst. Rev. 2008, 3. [Google Scholar] [CrossRef]
- Healy, A.; Dunning, D.N.; Chockalingam, N. Materials used for footwear orthoses: A review. Footwear Sci. 2010, 2, 93–110. [Google Scholar] [CrossRef]
- Bus, S.A.; Ulbrecht, J.S.; Cavanagh, P.R. Pressure relief and load redistribution by custom-made insoles in diabetic patients with neuropathy and foot deformity. Clin. Biomech. 2004, 19, 629–638. [Google Scholar] [CrossRef]
- Chhikara, K.; Singh, G.; Gupta, S.; Chanda, A. Progress of Additive Manufacturing in Fabrication of Foot Orthoses for Diabetic Patients: A Review. Ann. 3D Print. Med. 2022, 8, 100085. [Google Scholar] [CrossRef]
- Telfer, S.; Woodburn, J. The use of 3D surface scanning for the measurement and assessment of the human foot. J. Foot Ankle Res. 2010, 3, 1–9. [Google Scholar] [CrossRef]
- Hale, L.; Linley, E.; Kalaskar, D.M. A digital workflow for design and fabrication of bespoke orthoses using 3D scanning and 3D printing, a patient-based case study. Sci. Rep. 2020, 101, 1–7. [Google Scholar] [CrossRef]
- Chanda, A.; Unnikrishnan, V. Novel insole design for diabetic foot ulcer management. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2018, 232, 1182–1195. [Google Scholar] [CrossRef]
- Chanda, A.; McClain, S. Mechanical Modeling of Healthy and Diseased Calcaneal Fat Pad Surrogates. Biomimetics 2019, 4, 1. [Google Scholar] [CrossRef]
- Chanda, A.; Unnikrishnan, V. Customized Insoles for Diabetic and Pressure Ulcers. US Patent US20180008000A1, 2017. [Google Scholar]
- Stolt, M.; Suhonen, R.; Virolainen, P.; Leino-Kilpi, H. Lower extremity musculoskeletal disorders in nurses: A narrative literature review. Scand. J. Public Health 2016, 44, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Ajibade, B.L.; Alao, M. Prevalence of musculo-skeletal disorders among nurses in Osun State, Nigeria. J. Biol. Agric. Healthc. 2013, 3, 170–175. Available online: https://www.iiste.org/Journals/index.php/JBAH/article/view/6331 (accessed on 4 January 2023).
- Chatterjee, S.; Chanda, A. Development of a Tribofidelic Human Heel Surrogate for Barefoot Slip Testing. J. Bionic Eng. 2022, 192, 429–439. [Google Scholar] [CrossRef]
- Chhikara, K.; Gupta, S.; Chanda, A. Development of a novel foot orthosis for plantar pain reduction. Mater. Today Proc. 2022, 62, 3532–3537. [Google Scholar] [CrossRef]
- Yick, K.L.; Tse, C.Y. Textiles and other materials for orthopaedic footwear insoles. In Handbook of Footwear Design and Manufacture; Woodhead Publishing: Sawston, UK, 2013; pp. 341–371. [Google Scholar] [CrossRef]
- Mulligan, E. Lower Leg, Ankle, and Foot Rehabilitation. Phys. Rehabil. Inj. Athl. 2012, 4, 426–463. [Google Scholar] [CrossRef]
- Nicolopoulos, C.S.; Black, J.; Anderson, E.G. Foot orthoses materials. Foot 2000, 10, 1–3. [Google Scholar] [CrossRef]
- Brückner, K.; Odenwald, S.; Schwanitz, S.; Heidenfelder, J.; Milani, T. Polyurethane-foam midsoles in running shoes-impact energy and damping. Procedia Eng. 2010, 2, 2789–2793. [Google Scholar] [CrossRef]
- Gerrard, J.M.; Bonanno, D.R.; Bonanno, D.R.; Whittaker, G.A.; Landorf, K.B. Effect of different orthotic materials on plantar pressures: A systematic review. J. Foot Ankle Res. 2020, 13, 1–11. [Google Scholar] [CrossRef]
- Akambase, J.A.; Kokoreva, T.V.; Gurova, O.A.; Akambase, J.A. The effect of body positions on foot types: Considering body weight. Transl. Res. Anat. 2019, 16, 100048. [Google Scholar] [CrossRef]
- Fähndrich, E.; Linden, M. Reliability and validity of the Visual Analogue Scale (VAS). Pharmacopsychiatria 1982, 15, 90–94. [Google Scholar] [CrossRef]
- Martin, R.L.; Irrgang, J.J.; Burdett, R.G.; Conti, S.F.; Van Swearingen, J.M. Evidence of Validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005, 26, 968–983. [Google Scholar] [CrossRef]
- Karami, E.; Kashani, R.V.; Bani, M.A.; Daryabor, A. Effect of Prefabricated Insole with Shock Absorb Canal and Custom-Molded Insole on Pain and Function in Subjects with Plantar Fasciitis: A Pilot Study. J. Clin. Physiother. Res. 2020, 5, e25. [Google Scholar] [CrossRef]
- Chung, C.L.; Paquette, M.R.; DiAngelo, D.J. Impact of a dynamic ankle orthosis on acute pain and function in patients with mechanical foot and ankle pain. Clin. Biomech. 2021, 83, 105281. [Google Scholar] [CrossRef]




| Group | Number of Subjects | Mean | Standard Deviation | Standard Error Mean | |
|---|---|---|---|---|---|
| Age * | 1 | 18 | 26.66 | 4.22 | 0.99 |
| 2 | 18 | 26.16 | 4.24 | 1.00 | |
| Height * | 1 | 18 | 156.83 | 10.28 | 2.42 |
| 2 | 18 | 156.33 | 5.25 | 1.23 | |
| Weight * | 1 | 18 | 59.00 | 10.14 | 2.39 |
| 2 | 18 | 58.22 | 12.99 | 3.06 | |
| BMI * | 1 | 18 | 21.62 | 2.28 | 0.88 |
| 2 | 18 | 21.73 | 1.43 | 0.23 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chhikara, K.; Sidhu, S.S.; Gupta, S.; Saharawat, S.; Kataria, C.; Chanda, A. Development and Effectiveness Testing of a Novel 3D-Printed Multi-Material Orthosis in Nurses with Plantar Foot Pain. Prosthesis 2023, 5, 73-87. https://doi.org/10.3390/prosthesis5010006
Chhikara K, Sidhu SS, Gupta S, Saharawat S, Kataria C, Chanda A. Development and Effectiveness Testing of a Novel 3D-Printed Multi-Material Orthosis in Nurses with Plantar Foot Pain. Prosthesis. 2023; 5(1):73-87. https://doi.org/10.3390/prosthesis5010006
Chicago/Turabian StyleChhikara, Komal, Sarabjeet Singh Sidhu, Shubham Gupta, Sakshi Saharawat, Chitra Kataria, and Arnab Chanda. 2023. "Development and Effectiveness Testing of a Novel 3D-Printed Multi-Material Orthosis in Nurses with Plantar Foot Pain" Prosthesis 5, no. 1: 73-87. https://doi.org/10.3390/prosthesis5010006
APA StyleChhikara, K., Sidhu, S. S., Gupta, S., Saharawat, S., Kataria, C., & Chanda, A. (2023). Development and Effectiveness Testing of a Novel 3D-Printed Multi-Material Orthosis in Nurses with Plantar Foot Pain. Prosthesis, 5(1), 73-87. https://doi.org/10.3390/prosthesis5010006







