Digital Workflow for Prosthetically Driven Implants Placement and Digital Cross Mounting: A Retrospective Case Series
Abstract
1. Introduction
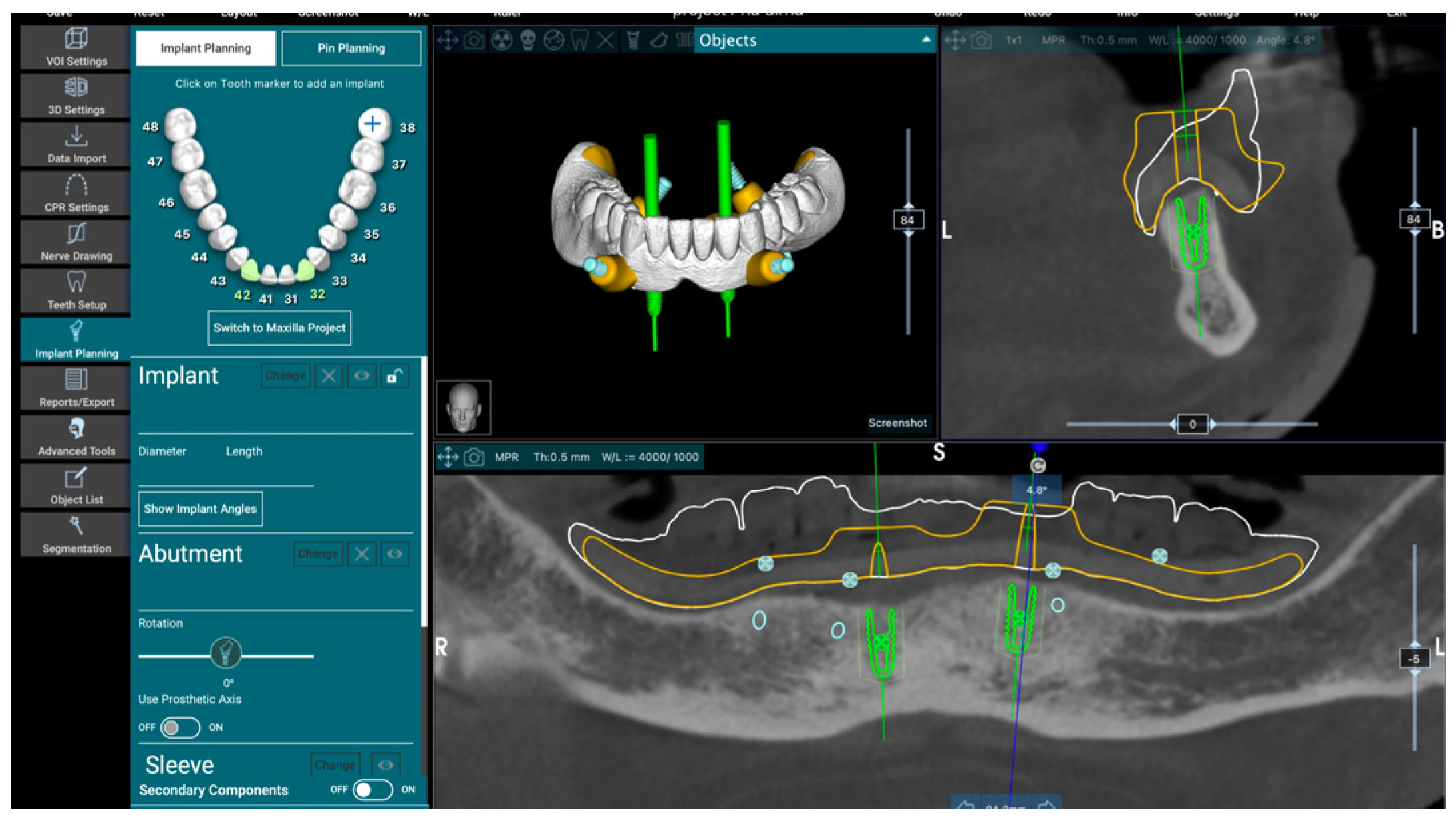
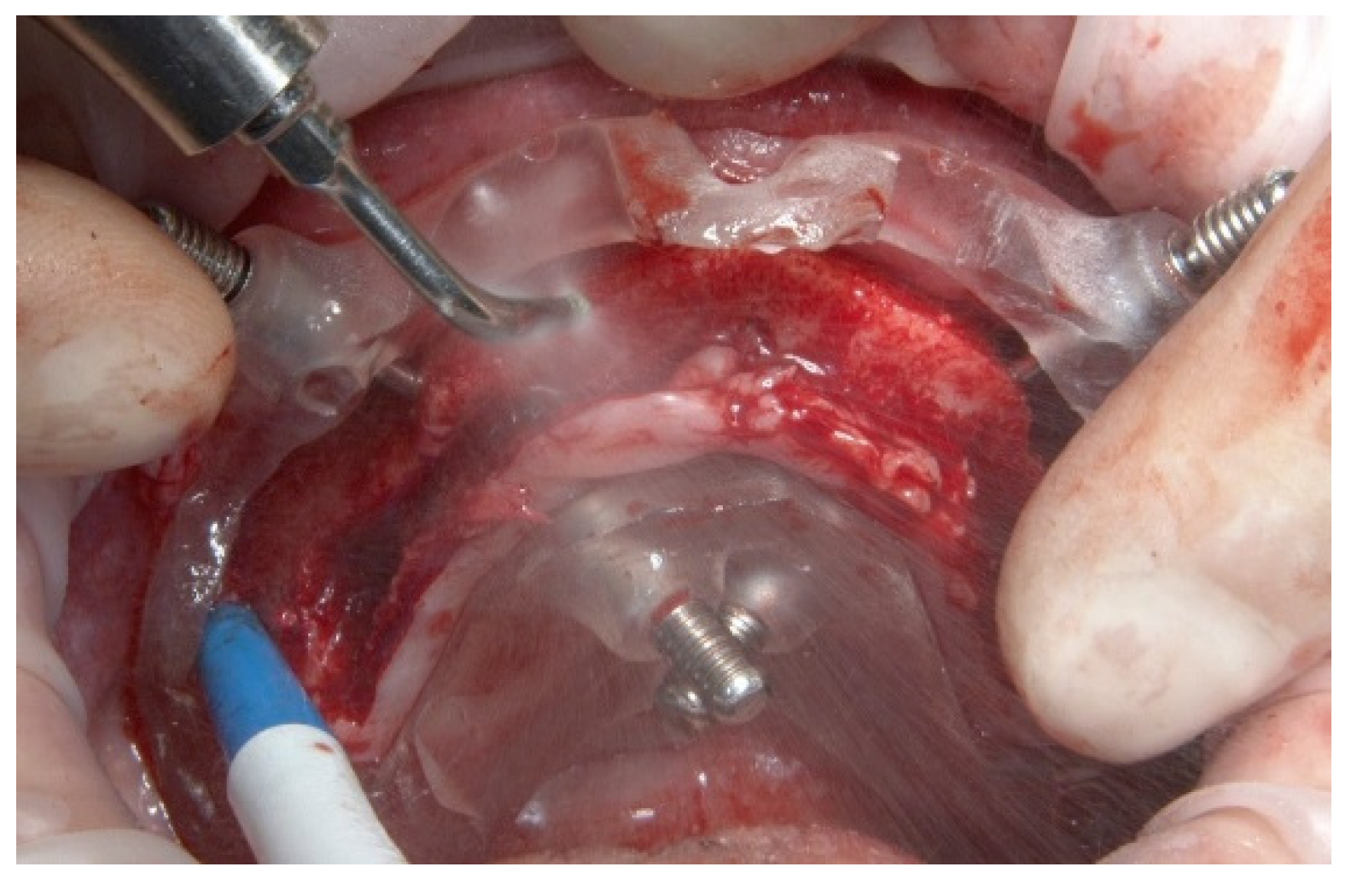
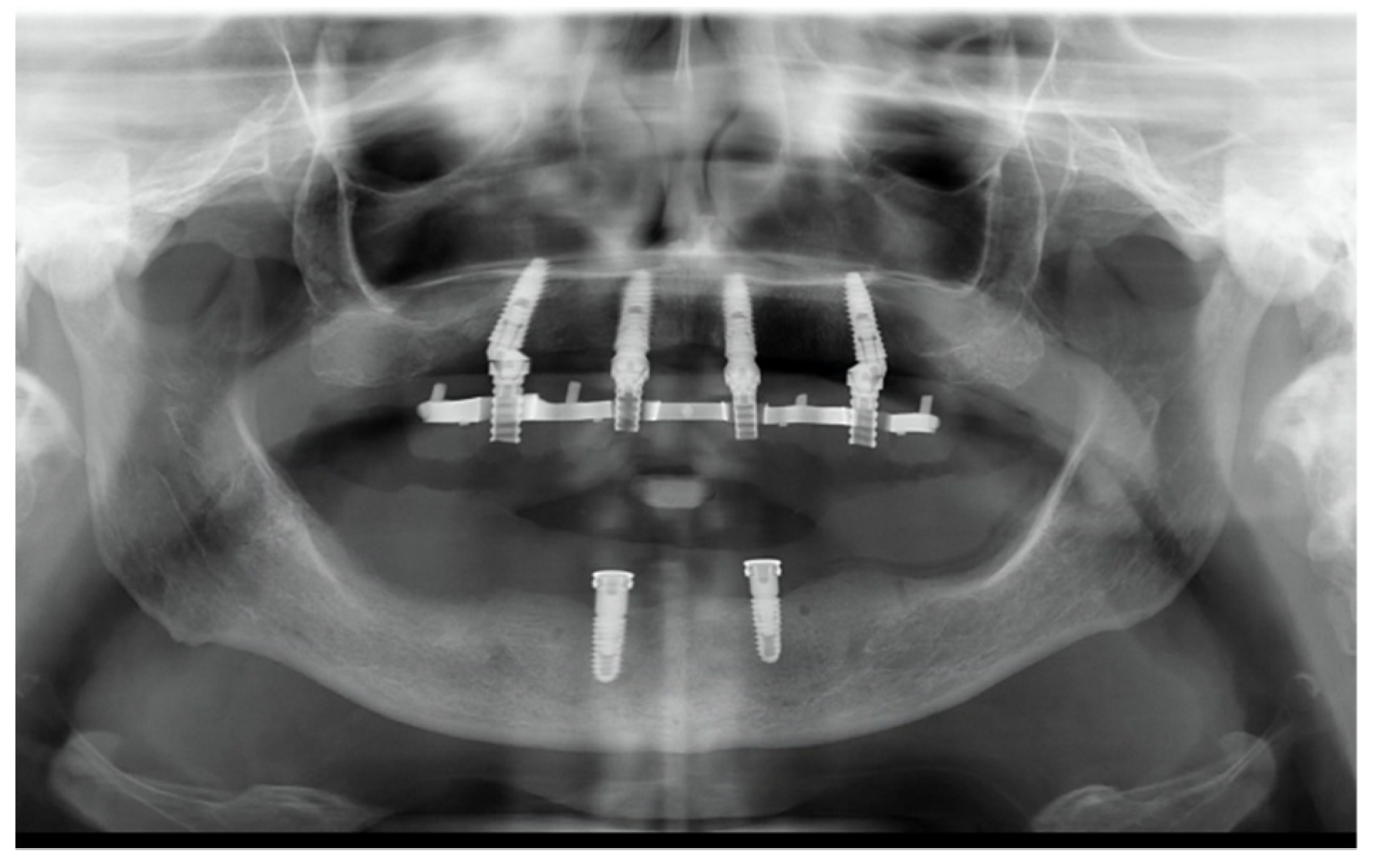
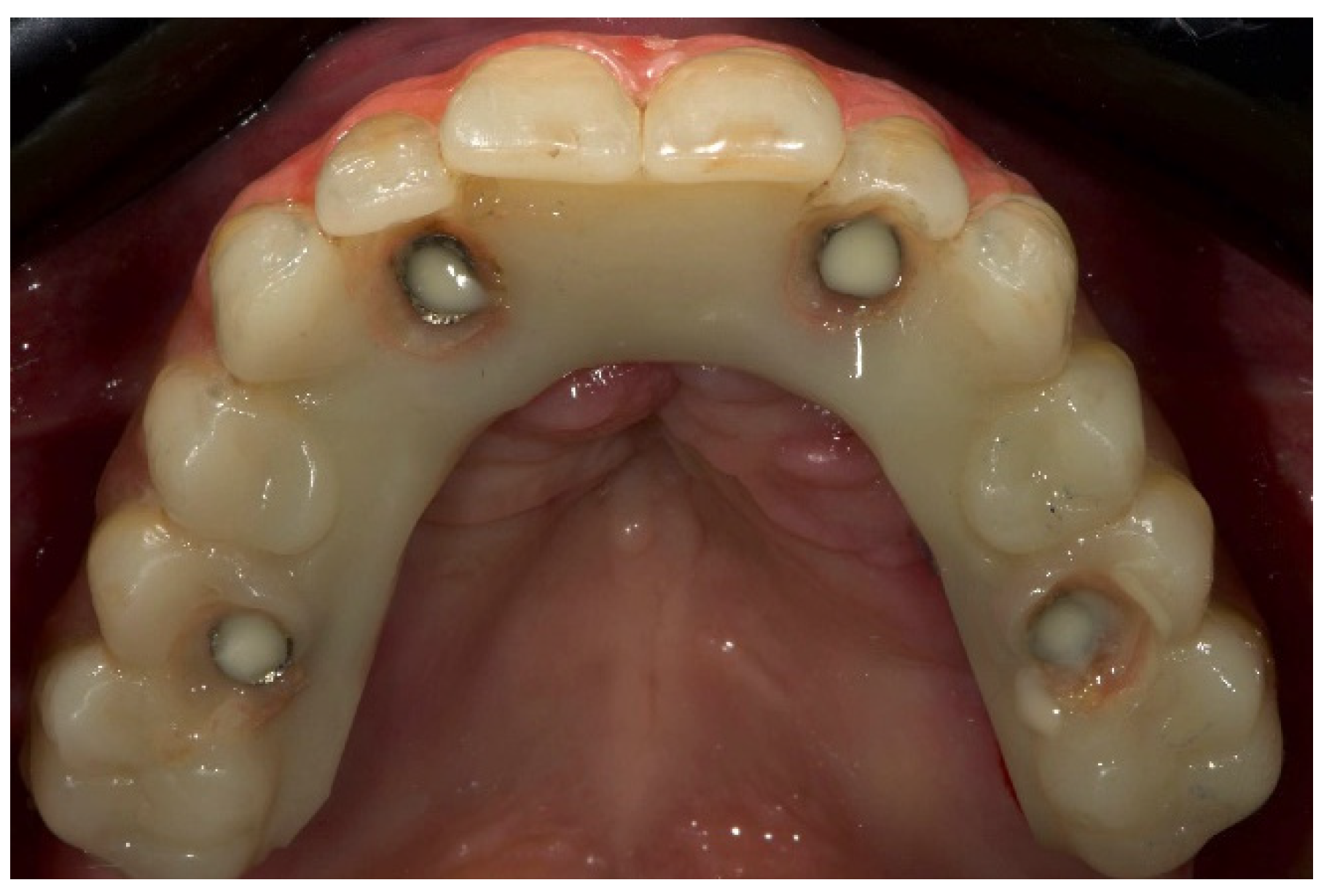
2. Material and Methods
- An implant was considered a failure if it presented with any mobility dictating its removal, assessed by tapping or rocking the implant head with the metallic handles of two instruments; progressive marginal bone loss or infection; and any mechanical complications rendering the implant unusable, although still mechanically stable in the bone. A prosthesis was considered a failure if, in any case, it needed to be performed again. The same operator (MT) evaluated failures;
- Any biological (pain, swelling, suppuration, etc.) and/or mechanical (screw loosening, fracture of the prosthesis, etc.) complications were evaluated and recorded by the same operator (MT);
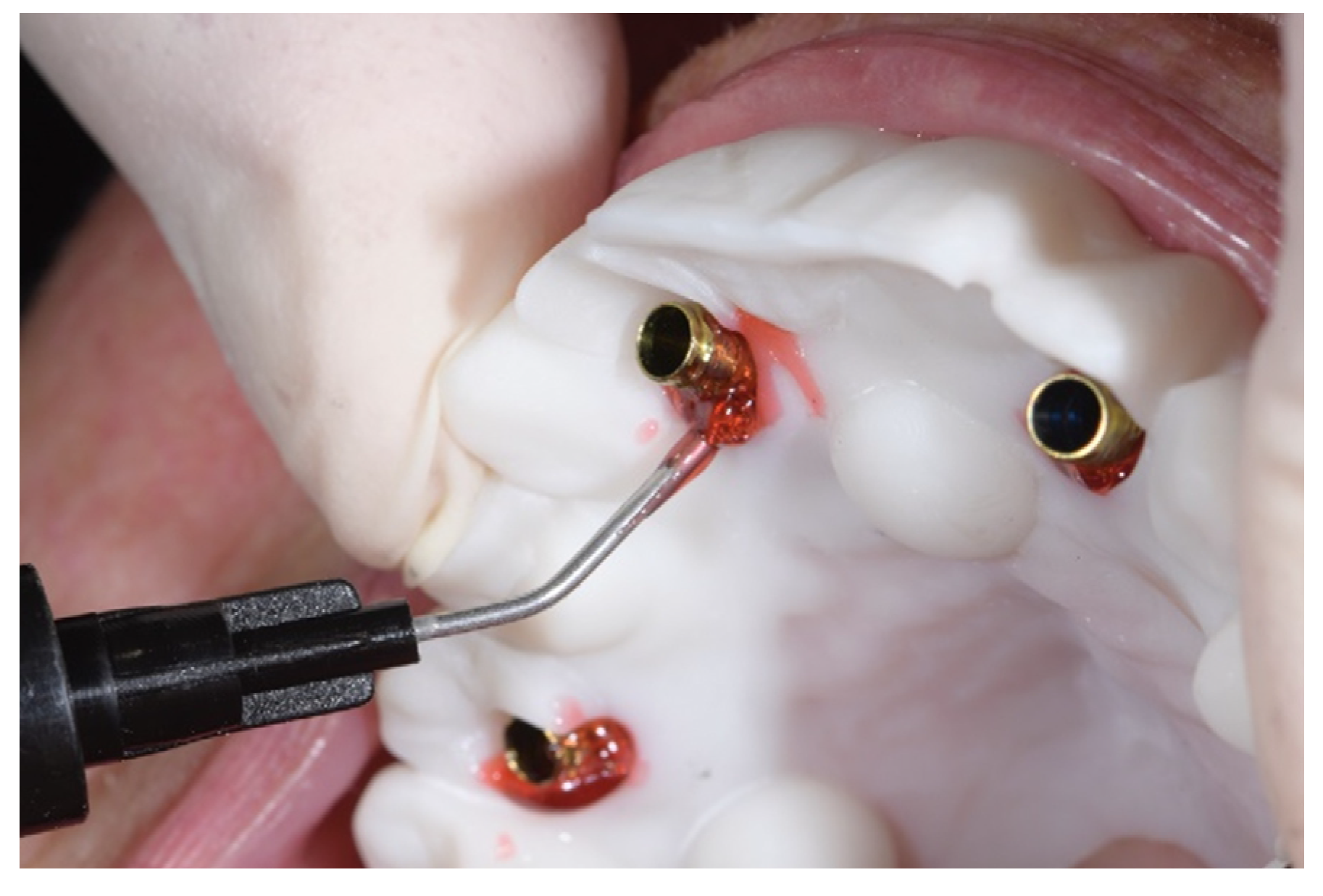
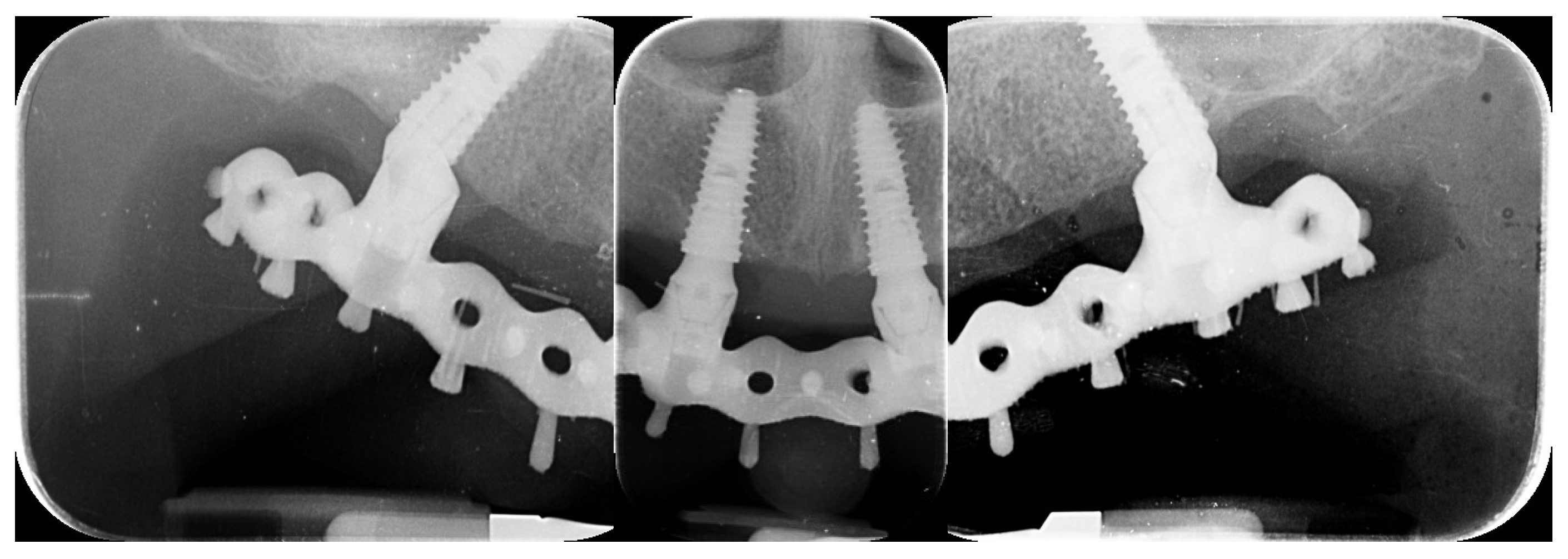
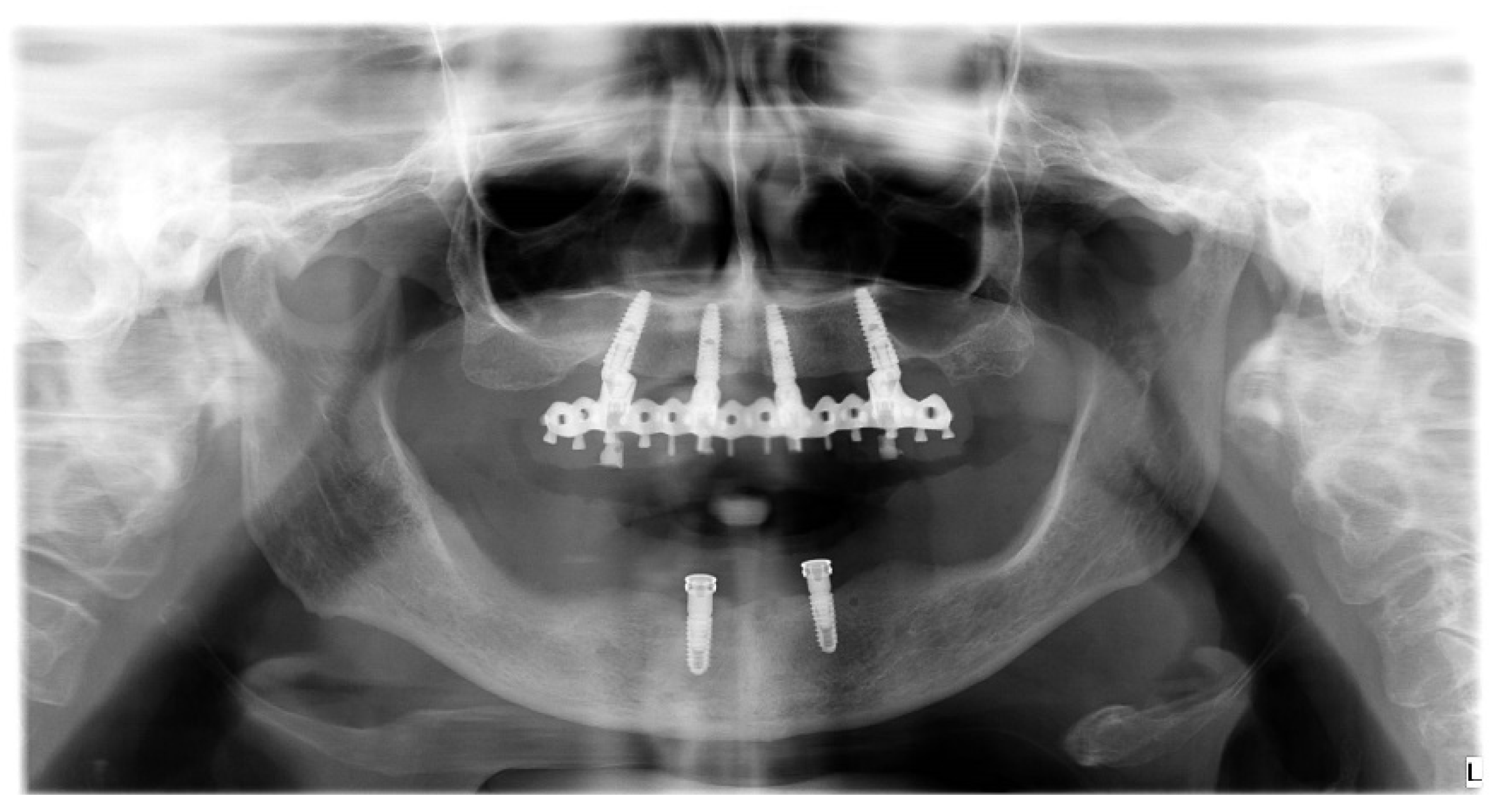
- Accuracy was tested by means of direct vision and tactile sensation, performed by applying alternately pressure on the aluminum try-in, and then the definitive metal framework (Alternate Pressure Technique), secured without screws, to determine if any movement occurs. In addition, the one-screw test proposed by Jemt and co-workers was performed in case of doubts occurred [11]. No discrepancy of the radiopaque, aluminum try-in, secured with only one screw tightened, was observed [11]. Peri-apical radiographs were taken if needed. The same operator (MT) performed both tests using a microscope magnification (10× to 16×);
- Patients’ satisfaction was measured by means of a questionnaire delivered four months after prosthesis delivery by an independent outcome assessor. The following questions were asked: Are you satisfied with the function of your implant-supported prosthesis?; Are you satisfied with the aesthetic outcome of your implant supported prosthesis?; Would you undergo the same therapy again? Possible answers: yes absolutely; yes partly; not sure; not really; absolutely not. An operator not previously involved in the treatment of the patient filled out the questionnaire.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tallarico, M.; Scrascia, R.; Annucci, M.; Meloni, S.M.; Lumbau, A.I.; Koshovari, A.; Xhanari, E.; Martinolli, M. Errors in Implant Positioning Due to Lack of Planning: A Clinical Case Report of New Prosthetic Materials and Solutions. Materials 2020, 13, 1883. [Google Scholar] [CrossRef]
- Tallarico, M.; Meloni, S.M. Retrospective Analysis on Survival Rate, Template-Related Complications, and Prevalence of Pe-ri-implantitis of 694 Anodized Implants Placed Using Computer-Guided Surgery: Results Between 1 and 10 Years of Follow-Up. Int. J. Oral Maxillofac. Implant. 2017, 32, 1162–1171. [Google Scholar] [CrossRef]
- D’Haese, J.; Ackhurst, J.; Wismeijer, D.; De Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontol. 2000 2017, 73, 121–133. [Google Scholar] [CrossRef]
- Cicciù, M.; Tallarico, M. Dental Implant Materials: Current State and Future Perspectives. Materials 2021, 14, 371. [Google Scholar] [CrossRef]
- Tallarico, M.; Esposito, M.; Xhanari, E.; Caneva, M.; Meloni, S.M. Computer-guided vs freehand placement of immediately loaded dental implants: 5-year postloading results of a randomised controlled trial. Eur. J. Oral Implant. 2018, 11, 203–213. [Google Scholar]
- Tallarico, M.; Xhanari, E.; Kim, Y.J.; Cocchi, F.; Martinolli, M.; Alushi, A.; Baldoni, E.E.; Meloni, S.M. Accuracy of comput-er-assisted template-based implant placement using conventional impression and scan model or intraoral digital impression: A randomised controlled trial with 1 year of follow-up. Int. J. Oral Implant. 2019, 12, 197–206. [Google Scholar]
- Venezia, P.; Torsello, F.; Santomauro, V.; Dibello, V.; Cavalcanti, R. Full Digital Workflow for the Treatment of an Edentulous Patient with Guided Surgery, Immediate Loading and 3D-Printed Hybrid Prosthesis: The BARI Technique 2.0. A Case Report. Int. J. Environ. Res. Public Health 2019, 16, 5160. [Google Scholar] [CrossRef]
- Tallarico, M.; Schiappa, D.; Schipani, F.; Cocchi, F.; Annucci, M.; Xhanari, E. Improved fully digital workflow to rehabilitate edentulous patient with an implant overdenture in 4 appointments: A case report. J. Oral Sci. Rehabil. 2017, 3, 38–46. [Google Scholar]
- Baruffaldi, A.; Maiorana, C.; Poli, P.P.; Baruffaldi, A.; Baruffaldi, M. A suggested protocol to increase the accuracy of prosthetic phases in case of full-arch model-free fully guided computer-aided implant placement and immediate loading. Oral Maxillofac. Surg. 2020, 24, 343–351. [Google Scholar] [CrossRef]
- Tallarico, M.; Czajkowska, M.; Cicciù, M.; Giardina, F.; Minciarelli, A.; Zadrożny, Ł.; Park, C.-J.; Meloni, S.M. Accuracy of surgical templates with and without metallic sleeves in case of partial arch restorations: A systematic review. J. Dent. 2021, 115, 103852. [Google Scholar] [CrossRef]
- Jemt, T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in eden-tulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int. J. Oral Maxillofac. Implant. 1991, 6, 270–276. [Google Scholar]
- Menini, M.; Conserva, E.; Tealdo, T.; Bevilacqua, M.; Pera, F.; Signori, A.; Pera, P. Shock Absorption Capacity of Restorative Materials for Dental Implant Prostheses: An In Vitro Study. Int. J. Prosthodont. 2013, 26, 549–556. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tallarico, M.; Martinolli, M.; Kim, Y.-J.; Cocchi, F.; Meloni, S.M.; Alushi, A.; Xhanari, E. Accuracy of Computer-Assisted Template-Based Implant Placement Using Two Different Surgical Templates Designed with or without Metallic Sleeves: A Randomized Controlled Trial. Dent. J. 2019, 7, 41. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Kim, Y.-J.; Cocchi, F.; Martinolli, M.; Meloni, S.M. Accuracy of newly developed sleeve-designed templates for insertion of dental implants: A prospective multicenters clinical trial. Clin. Implant Dent. Relat. Res. 2018, 21, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Polizzi, G.; Cantoni, T. Five-Year Follow-Up of Immediate Fixed Restorations of Maxillary Implants Inserted in Both Fresh Extraction and Healed Sites Using the N obel G uide™ System. Clin. Implant Dent. Relat. Res. 2015, 17, 221–233. [Google Scholar] [CrossRef]
- Cantoni, T.; Polizzi, G. Implant treatment planning in fresh extraction sockets: Use of a novel radiographic guide and CAD/CAM technology. Quintessence Int. 2009, 40, 773–781. [Google Scholar]
- Tallarico, M.; Lumbau, A.I.; Park, C.J.; Puddu, A.; Sanseverino, F.; Amarena, R.; Meloni, S.M. In vitro evaluation of bioburden, three-dimensional stability, and accuracy of surgical templates without metallic sleeves after routinely infection control activ-ities. Clin. Implant Dent. Relat. Res. 2021, 23, 380–387. [Google Scholar] [CrossRef]
- Tallarico, M.; Xhanari, E.; Martinolli, M.; Baldoni, E.; Meloni, S. Extraoral chairside digitalization: Clinical reports on a new digital protocol for surgical and prosthetic treatment of completely edentulous patients. J. Oral Sci. Rehabil. 2018, 4, 16–20. [Google Scholar]
- Tallarico, M.; Lumbau, A.I.; Scrascia, R.; Demelas, G.; Sanseverino, F.; Amarena, R.; Meloni, S.M. Feasibility of Using a Pros-thetic-Based Impression Template to Improve the Trueness and Precision of a Complete Arch Digital Impression on Four and Six Implants: An In Vitro Study. Materials 2020, 13, 3543. [Google Scholar] [CrossRef]
- Venezia, P.; Lacasella, P.; Cordaro, L.; Torsello, F.; Cavalcanti, R. The BARI technique: A new approach to immediate loading. Int. J. Esthet. Dent. 2015, 10, 428–443. [Google Scholar]
- Ender, A.; Zimmermann, M.; Mehl, A. Accuracy of complete- and partial-arch impressions of actual intraoral scanning systems in vitro. Int. J. Comput. Dent. 2019, 22, 11–19. [Google Scholar] [PubMed]
- Gedrimiene, A.; Adaskevicius, R.; Rutkunas, V. Accuracy of digital and conventional dental implant impressions for fixed partial dentures: A comparative clinical study. J. Adv. Prosthodont. 2019, 11, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Imburgia, M.; Logozzo, S.; Hauschild, U.; Veronesi, G.; Mangano, C.; Mangano, F.G. Accuracy of four intraoral scanners in oral implantology: A comparative in vitro study. BMC Oral Health 2017, 17, 92. [Google Scholar] [CrossRef]
- Mangano, F.G.; Veronesi, G.; Hauschild, U.; Mijiritsky, E.; Mangano, C. Trueness and Precision of Four Intraoral Scanners in Oral Implantology: A Comparative in Vitro Study. PLoS ONE 2016, 11, e0163107. [Google Scholar] [CrossRef]
- Róth, I.; Czigola, A.; Joós-Kovács, G.L.; Dalos, M.; Hermann, P.; Borbély, J. Learning curve of digital intraoral scanning—An in vivo study. BMC Oral Health 2020, 20, 1–7. [Google Scholar] [CrossRef]
- Lee, S.J.; Kim, S.-W.; Lee, J.J.; Cheong, C.W. Comparison of Intraoral and Extraoral Digital Scanners: Evaluation of Surface Topography and Precision. Dent. J. 2020, 8, 52. [Google Scholar] [CrossRef]
- Tallarico, M.; Ceruso, F.M.; Muzzi, L.; Meloni, S.M.; Kim, Y.-J.; Gargari, M.; Martinolli, M. Effect of Simultaneous Immediate Implant Placement and Guided Bone Reconstruction with Ultra-Fine Titanium Mesh Membranes on Radiographic and Clinical Parameters after 18 Months of Loading. Materials 2019, 12, 1710. [Google Scholar] [CrossRef]
- Zadrożny, Ł.; Czajkowska, M.; Tallarico, M.; Wagner, L.; Markowski, J.; Mijiritsky, E.; Cicciù, M. Prosthetic Surgical Templates and Dental Implant Site Time Preparation: An In Vitro Study. Prosthesis 2022, 4, 25–37. [Google Scholar] [CrossRef]
- Tallarico, M.; Meloni, S.M.; Park, C.-J.; Zadrożny, Ł.; Scrascia, R.; Cicciù, M. Implant Fracture: A Narrative Literature Review. Prosthesis 2021, 3, 267–279. [Google Scholar] [CrossRef]
- Tallarico, M.; Canullo, L.; Pisano, M.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M.; Meloni, S.M. An up to 7-Year Retrospective Analysis of Biologic and Technical Complication With the All-on-4 Concept. J. Oral Implant. 2016, 42, 265–271. [Google Scholar] [CrossRef]














| Exclusion Criteria |
|---|
| ASA 3 and 4 classification; American Society of Anesthesiologists, https://www.asahq.org (accessed on 10 July 2022) |
| Pregnant or nursing |
| Intravenous bisphosphonate therapy |
| Alcohol or drug abuse |
| Heavy smoking (≥20 cigarettes/day) |
| Radiation therapy to the head or neck region within the last five years |
| History of parafunction |
| Untreated periodontitis |
| Psychiatric therapy or unrealistic expectations |
| Immunosuppressed or immunocompromised |
| Lack of opposite occluding dentition/prosthesis |
| Acute infection in the area intended for implant placement |
| Need for bone augmentation |
| Full mouth bleeding on probing [BoP] and full mouth plaque index [PI] higher than 25% |
| Allergy or adverse reactions to the restorative materials |
| Advantages | Disadvantage |
|---|---|
| All the treatments will be free of charge | Costs for travel and medicines at her own |
| All the surgical and prosthetic procedure will be performed by the same expert clinician (M.T.) | Availability of time for the trying sessions and live surgeries |
| General rules of Good Medical Practice will be respected | Availability for follow-ups |
| Management of possible complications, including remakes will be free of charge for at least 5 years after delivery | Signed informed consent for facial pictures and video shooting |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tallarico, M.; Galiffi, D.; Scrascia, R.; Gualandri, M.; Zadrożny, Ł.; Czajkowska, M.; Catapano, S.; Grande, F.; Baldoni, E.; Lumbau, A.I.; et al. Digital Workflow for Prosthetically Driven Implants Placement and Digital Cross Mounting: A Retrospective Case Series. Prosthesis 2022, 4, 353-368. https://doi.org/10.3390/prosthesis4030029
Tallarico M, Galiffi D, Scrascia R, Gualandri M, Zadrożny Ł, Czajkowska M, Catapano S, Grande F, Baldoni E, Lumbau AI, et al. Digital Workflow for Prosthetically Driven Implants Placement and Digital Cross Mounting: A Retrospective Case Series. Prosthesis. 2022; 4(3):353-368. https://doi.org/10.3390/prosthesis4030029
Chicago/Turabian StyleTallarico, Marco, Davide Galiffi, Roberto Scrascia, Maurizio Gualandri, Łukasz Zadrożny, Marta Czajkowska, Santo Catapano, Francesco Grande, Edoardo Baldoni, Aurea Immacolata Lumbau, and et al. 2022. "Digital Workflow for Prosthetically Driven Implants Placement and Digital Cross Mounting: A Retrospective Case Series" Prosthesis 4, no. 3: 353-368. https://doi.org/10.3390/prosthesis4030029
APA StyleTallarico, M., Galiffi, D., Scrascia, R., Gualandri, M., Zadrożny, Ł., Czajkowska, M., Catapano, S., Grande, F., Baldoni, E., Lumbau, A. I., Meloni, S. M., & Pisano, M. (2022). Digital Workflow for Prosthetically Driven Implants Placement and Digital Cross Mounting: A Retrospective Case Series. Prosthesis, 4(3), 353-368. https://doi.org/10.3390/prosthesis4030029











